Abstract
Purpose
Bee sting injuries to the eye and surrounding tissue are an infrequent occurrence. Here we present an interesting Case of a 64 year old bee keeper who was stung in the left upper eyelid.
Observations
After the injury, she developed pain and inflammation of the eyelid though a few days after the injury noted increased eye pain. On initial ophthalmic assessment, no retained foreign body was noted. Six days after the incident, her lid edema had improved and a retained foreign body – the bee stinger - had been found on eversion of the eyelid. We propose that as the inflammation resolved, the stinger extruded from the inner eyelid tissue, causing a corneal abrasion, which was the source of her acute increase in pain.
Conclusion and Importance
In cases of bee injuries, it is paramount to consider the possibility of retained foreign bodies and to perform a thorough ophthalmic examination and assessment.
Keywords: Corneal abrasion, Bee sting, Foreign body, Superficial laceration, Cornea, Eyelid
1. Introduction
Ocular foreign bodies and traumatic injury are commonplace in ophthalmology. Rarer are ocular foreign bodies due to insect attack. There are multiple reports in the literature of bee stings causing ocular injury from the trauma of the attack and inflammation due to the toxin in the stinger.1, 2, 3, 4 Here we present a unique Case of a retained eyelid bee stinger, initially masked by lid edema, causing a secondary corneal abrasion after resolution of lid inflammation.
2. Case report
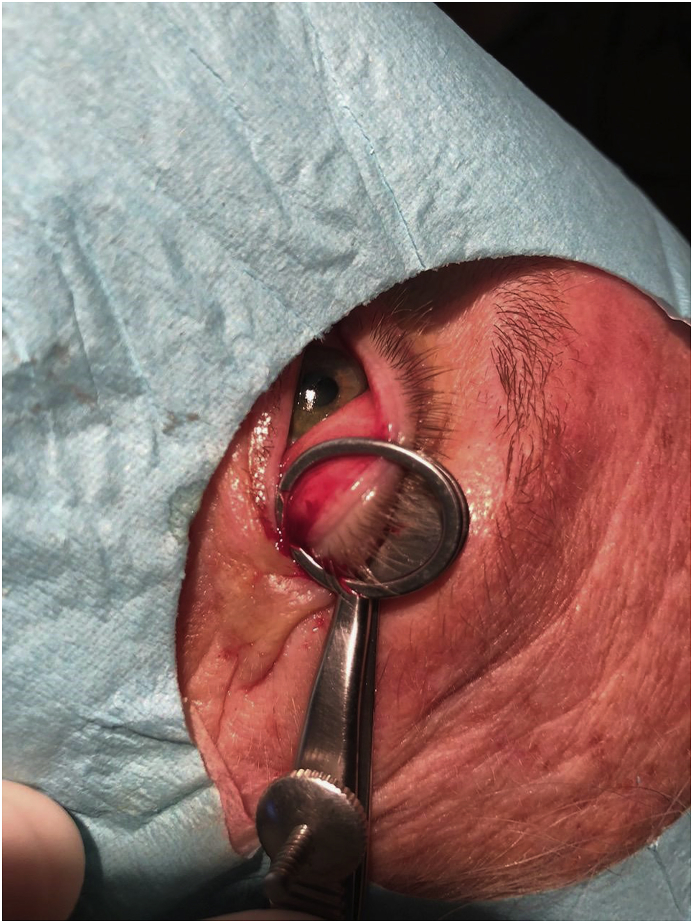
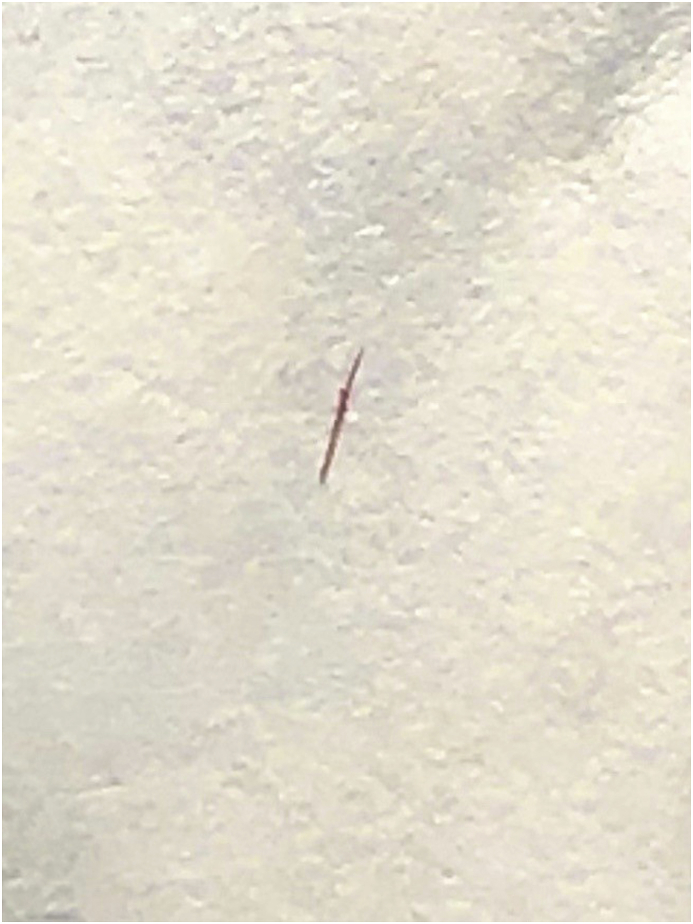
64-year-old otherwise healthy female beekeeper and with a history of Hashimoto's Disease presented to the optometrist five days status post bee sting to the left upper eyelid. She experienced eyelid pain and swelling in the days immediately following the bee sting, but she did not have significant eye pain. On presentation to the optometrist, she noted increasing eye pain. She described the pain as an irritating, scratchy feeling. On exam by the optometrist, swelling was noted of the left periorbital tissues. The patient was referred to ophthalmology for further evaluation with concern that the stinger may have been lodged in the eye. In the interim, the patient was started on oflaxacin eyedrops three times per day and prednisolone drops four times per day for pain and inflammation. The next day (now 6 days after the original injury), the patient presented for ophthalmology evaluation. Vision was 20/20 with correction in both eyes. Pupils were equal and reactive to light. Ocular motility exam was normal. Examination of the right eye was normal. Examination of the left eye showed no swelling of the left upper eyelid. The conjunctiva was not injected and a nasal pinguecula was noted. Linear staining with Fluorescein was evident in the temporal third of the cornea, suggestive of an upper eyelid foreign body (Fig. 1). On lid eversion at the slit lamp, there initially appeared to be no retained foreign body. However, on closer inspection a very small black dot was identified on the superior tarsal conjunctiva. A cornea spud was used in an attempt to remove the presumed foreign body which looked like a small grain of sand. However, instead of gently sliding off of the tarsal conjunctiva, the object seemed to be firmly embedded in the tarsal conjunctiva. By pushing aside a small amount of surrounding tissue, the object's sharp tip became more identifiable. The remainder of the exam was unremarkable. After informed consent was obtained from the patient, the left upper eyelid was everted with a chalazion clamp, and a 15° blade was used to dissect around the foreign body. The long slender shape of the object began to become identifiable as a bee stinger (Fig. 2). The stinger was then removed with jeweler's forceps and erythromycin ointment was placed in the eye (Fig. 3). The patient was continued on ofloxacin three times a day in the left eye for five days, and the prednisolone was stopped. The patient was asked to follow up with her original optometrist and to follow up with ophthalmology as needed. In phone consultation the following day, the patient expressed complete resolution of her symptoms.
Fig. 1.
Corneal abrasion secondary to the bee stinger.
Fig. 2.
Upper eyelid eversion, exposing the affected lid.
Fig. 3.
Bee stinger removed from the patient's eyelid.
3. Discussion
A PubMed search was done with the key words “bee sting” and “eye” as part of the review of literature for this Case report.
Bee sting injury to the eye is a relatively rare occurrence and not often studied. Our PubMed search returned less than 50 articles - most of which were Case reports with a few small studies. Case reports have documented a range of injuries secondary to bee stings including but not limited to toxic endophthalmitis, toxic optic neuropathy, vision loss, anterior uveitis, vitritis, cilio-choroidal detachment, corneal injury, retained corneal foreign body, cataract, conjunctivitis, and hyphema.1, 2, 3 A similar case to the one above described a retained subconjunctival honey bee stinger causing multiple corneal abrasions.4 The present case is unique in that the initial foreign body embedded in the lid initially caused no symptoms of corneal injury because the tip of the stinger did not extrude through the tarsal conjunctiva while the eyelid was edematous. It was only until the edema resolved that the stinger was able to extrude through the now thinner eyelid, causing the large corneal abrasion. In addition, this case demonstrates the importance of considering a retained foreign body involving the tarsal conjunctiva after a bee sting injury to the skin surface of the eyelid. The staining with fluorescein showing the corneal abrasion was the pathognomonic finding leading to the diagnosis of a retained foreign body of the upper lid. Also, this case highlights the importance of eyelid eversion to aid in the search for retained foreign bodies as they may be otherwise missed.
4. Conclusions
Although serious injury from bee stings to the eye and periorbital are not common, when injury occurs it is important to consider the possibility of a retained stinger in the eye or periorbital tissue and to assess the patient with eyelid eversion.
Patient consent
Consent to publish the Case report was obtained from the patient. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
OD, AN, and JD have no disclosures or conflicts of interest.
Acknowledgements
The authors acknowledge Kathryn Fallon, OD for her initial assistance with the patient.
References
- 1.Rishi E., Rishi P. Intraocular inflammation in a Case of bee sting injury. GMS Ophthalmol Cases. 2018;8:1–5. doi: 10.3205/oc000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed M., Lee C.S., McMillan B. Predicting visual function after an ocular bee sting. Int Ophthalmol. 2019;39(7):1621–1626. doi: 10.1007/s10792-018-0978-z. [DOI] [PubMed] [Google Scholar]
- 3.Gudiseva H., Uddaraju M., Pradhan S. Ocular manifestations of isolated corneal bee sting injury, management strategies, and clinical outcomes. Indian J Ophthalmol. 2018;66(2):262–268. doi: 10.4103/ijo.IJO_600_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhalerao S.A., Singh P., Rani P.K., Rathi V. The sting of a honey bee: an unusual subconjunctival foreign body. Indian J Ophthalmol. 2017;65(11):1226–1228. doi: 10.4103/ijo.IJO_533_17. [DOI] [PMC free article] [PubMed] [Google Scholar]