Abstract
Background
The importance of teaching the skills and practice of evidence-based medicine (EBM) for medical professionals has steadily grown in recent years. Alongside this growth is a need to evaluate the effectiveness of EBM curriculum as assessed by competency in the five ‘A’s’: asking, acquiring, appraising, applying and assessing (impact and performance). EBM educators in medical education will benefit from a compendium of existing assessment tools for assessing EBM competencies in their settings. The purpose of this review is to provide a systematic review and taxonomy of validated tools that evaluate EBM teaching in medical education.
Methods
We searched MEDLINE, EMBASE, Cochrane library, Educational Resources Information Centre (ERIC), Best Evidence Medical Education (BEME) databases and references of retrieved articles published between January 2005 and March 2019. We have presented the identified tools along with their psychometric properties including validity, reliability and relevance to the five domains of EBM practice and dimensions of EBM learning. We also assessed the quality of the tools to identify high quality tools as those supported by established interrater reliability (if applicable), objective (non-self-reported) outcome measures and achieved ≥ 3 types of established validity evidence. We have reported our study in accordance with the PRISMA guidelines.
Results
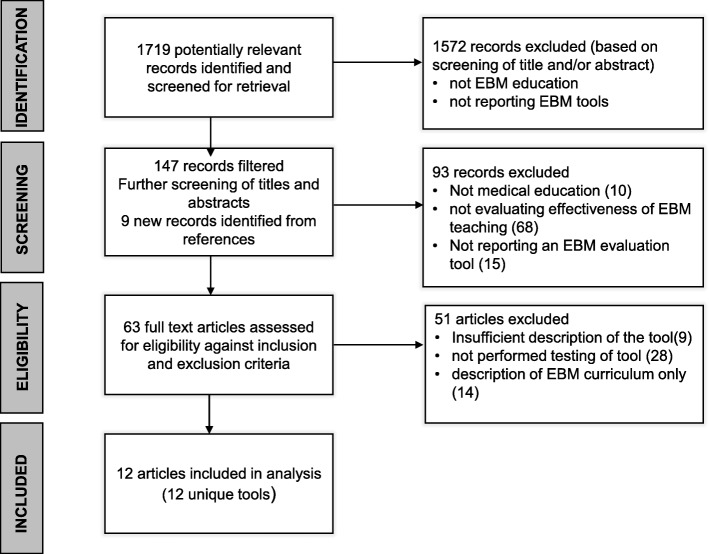
We identified 1719 potentially relevant articles of which 63 full text articles were assessed for eligibility against inclusion and exclusion criteria. Twelve articles each with a unique and newly identified tool were included in the final analysis. Of the twelve tools, all of them assessed the third step of EBM practice (appraise) and four assessed just that one step. None of the twelve tools assessed the last step of EBM practice (assess). Of the seven domains of EBM learning, ten tools assessed knowledge gain, nine assessed skills and-one assessed attitude. None addressed reaction to EBM teaching, self-efficacy, behaviours or patient benefit. Of the twelve tools identified, six were high quality. We have also provided a taxonomy of tools using the CREATE framework, for EBM teachers in medical education.
Conclusions
Six tools of reasonable validity are available for evaluating most steps of EBM and some domains of EBM learning. Further development and validation of tools that evaluate all the steps in EBM and all educational outcome domains are needed.
Systematic review registration
PROSPERO CRD42018116203.
Keywords: Evidence-based medicine, Competency, Medical education, Assessment
Background
Evidence-based medicine (EBM) is the skill of bringing together clinical judgement, the best available evidence from health research along with patient preferences and values in making clinical decisions [1]. EBM involves five steps—asking, acquiring, appraising, applying evidence in clinical decisions and assessing impact and performance [2]. To ensure future medical professionals are better equipped with lifelong skills for evidence-based medicine, we need to ensure that EBM teaching is integrated into undergraduate and postgraduate medical curriculum. In the UK, the General Medical Council recommends that ‘Newly qualified doctors must be able to apply scientific method and approaches to medical research and integrate these with a range of sources of information used to make decisions for care’ (https://www.gmc-uk.org/-/media/documents/dc11326-outcomes-for-graduates-2018_pdf-75040796.pdf).
Researchers have emphasised on the need to shift EBM teaching from the classroom to application of skills in clinical practice to achieve improvement in outcomes [3]. EBM teaching should focus on implementing multifaceted, clinically integrated approaches with assessments of knowledge, skills and behaviour in the medium to long term using validated assessment tools [4]. This highlights the need for validated tools to evaluate the impact of EBM teaching and assessment of medical trainees’ competency.
A systematic review of EBP education evaluation tools in 2006 [5] identified 104 unique instruments for evaluating evidence-based practice (EBP) teaching, though the authors identified only two of them—Fresno [6] and Berlin [7] as high-quality instruments which evaluate knowledge and skills across the EBP steps. The authors defined high-quality instruments as those with established interrater reliability (if applicable), objective outcome measures (non-self-reported) and multiple (≥ 3) types of established validity evidence. They found that among EBP skills, instruments acquiring evidence and appraising evidence were most commonly evaluated, with some newer instruments measuring asking and applying skills. Since the 2006 review, new assessment tools have been developed which assess EBM attitudes and behaviours [8–10].
Despite the availability of tools to evaluate EBM teaching, most evidence-based practice educational interventions still do not use high quality tools to measure outcomes [8]. EBM educators in medical education will benefit by the availability of a compendium of such tools which are classified by their suitability of assessing the five steps of EBM and the various educational outcome domains. Ensuring longitudinal evaluation of EBM teaching using validated assessment tools will provide educators information on the medium to long-term impact of their teaching.
In 2011, a guidance was developed for classification of tools to assess EBP learning, which also recommended a common taxonomy and proposed a framework—CREATE (Classification Rubric for Evidence Based Practice Assessment Tools in Education) for classifying such tools [11]. The purpose of the framework was to help EBP educators identify the best available assessment tool, provide direction for developers of new EBP learning assessment tools and a framework for classifying the tools. To that end, we designed this systematic review to incorporate these updates since the 2006 systematic review to assess and summarise published assessment tools for the evaluation of EBM teaching and learning in medical education.
The primary objective of this review was to summarise and describe currently available tools to evaluate EBM teaching in medical education. We compare, contrast and discuss the tools with consideration given to their psychometric properties and relevance to EBM domains and dimensions of EBM learning. The review aimed to differentiate tools into different subcategories according to type, extent, methods and results of psychometric testing and suitability for different evaluation purposes. The second objective of this review is to produce a taxonomy of tools based on the CREATE framework for medical educators to aid in the evaluation of EBM teaching.
Methods
Identification of studies
A scoping search was performed to validate the developed search strategy and justify the importance of conducting a review on the topic as defined by our research question and objectives. This search identified the most recent systematic review on this topic with a search end date of April 2006 [5]. We carried out an initial database search for relevant studies published between Jan 2005 and December 2018 with an update in March 2019.
Eligibility criteria
We included studies that reported a quantitative and/or qualitative description of at least one tool used to evaluate EBM in medical education which (a) assessed the dimension(s) of EBM learning, namely reaction to educational experience, attitudes, self-efficacy, knowledge, skills, behaviours and benefits to patients and (b) assessed different step(s) of EBM and (c) presented results of the psychometric performance of the tool. In addition to the above criteria, only tools which used objective outcome measures (non-self-reported) were included. We excluded tools which were explicitly designed for use in evaluating EBM teaching for other healthcare professionals (e.g. nurses or dentists). However, if such a tool was later validated for use in medical education, they were included in this review. We only included English language studies. Qualitative studies discussing perceptions of EBM curriculum and did not satisfy the inclusion criteria, conference abstracts, short notes, comments, editorials and study protocols were excluded.
Search strategy
The following electronic bibliographic databases of published studies were searched: MEDLINE, EMBASE, ERIC, BEME guidelines, Allied and complementary medicine, Cochrane Database of Systematic Reviews (CDSR) and Centre for Reviews and Dissemination (CRD) Databases (Database of Abstracts of Reviews of Effects (DARE). We also searched reference lists of retrieved articles.
Search terms
Search terms included: ‘Evidence Based Medicine’ or ‘EBM’ or ‘Evidence Based Practice’ or ‘Evidence Based Healthcare’ or ‘Evidence based Health Care’; ‘Educational Measurement’ or ‘assessment tool’; ‘Medical students’; ‘Medical education’; Clinical competence. MeSH terms were supplemented with keywords. Terms were then compared with the indexing terms applied to key journal articles which had previously been identified. An information specialist applied a preliminary search strategy, which was based on medical subject headings (MeSH) terms and text words of key papers that were identified beforehand (see Additional file 1).
Study selection
The first investigator (BK) carried out initial screening and excluded studies which did not meet the inclusion criteria. This included screening of titles and abstracts to assess their eligibility based on participant characteristics, descriptions of tools, assessment against the five EBM steps and seven educational domains and reporting of psychometric properties of the tools. BK and JHH subsequently screened full text articles against the inclusion and exclusion criteria and any discrepancies were resolved by consensus. When multiple studies presented the evaluation of the same tool, only the first study which evaluated the psychometric properties of the tool in medical education was included in this review, subsequent studies were considered as duplicates.
Data extraction and analysis
Data extraction was conducted using a standardised data extraction form. Information extracted included type of evaluation tool—description and development of the tool; number, level of expertise in EBM, training level of participants; the EBM steps evaluated; relevance of the tool to the dimensions of EBM learning, namely reaction to educational experience, attitudes, self-efficacy, knowledge, skills, behaviours and benefits to patients and psychometric properties of the tool.
BK and JHH independently reviewed and extracted data, and a third reviewer (LJ) also independently verified the findings of BK and JHH. Results were compared to achieve consensus. Disagreements during data extraction were resolved by consensus. Reviewers were not blinded to any portion of the articles.
BK, JHH and LJ evaluated the quality of each tool using the method from a previous systematic review [5]. Quality was assessed using guidance published by Shaneyfelt et al: (i) established interrater reliability (if applicable), (ii) type of outcome measure and (iii) validity [5]. A tool was rated high quality when supported by established (interrater reliability (if applicable), use of objective (non-self-reported) outcome measure(s) and when it also demonstrated multiple (≥ 3) types of established validity evidence (including evidence of discriminative validity)). Results of quality assessments were compared, and any discrepancies were resolved by consensus.
We first classified included tools and instruments according to the steps of EBM practice and educational outcome domains evaluated. To provide a taxonomy which can help medical educators decide on the most appropriate tool(s) available to evaluate their EBM teaching, we reviewed only those tools identified as high quality against the CREATE framework [11]. The framework helps in characterising the assessments with regards to the 5-step EBP model, types and level of educational assessment specific to EBP, audience characteristics and assessment aims. The framework is meant to help developers of new tools to identify and where possible address the current gaps. Educators can assess different elements of EBM learning, and the authors of CREATE have used the work by Freeth et al. for categorising assessment of EBM educational outcomes [12].
Results
Of the 1791 articles retrieved, 1572 were excluded and 147 articles were screened for eligibility. Of these 147; 93 were excluded and 63 full text articles were identified for further screening (Fig. 1 shows the PRISMA flowchart). After assessing the 63 full text articles for eligibility against inclusion and exclusion criteria, twelve were included in the final analysis.
Fig. 1.
PRISMA flowchart of the systematic review
Uploaded separately
The completed PRISMA checklist [13] has been attached as Additional file 2.
Classification of tools according to the assessment of EBM practice
We categorised the twelve tools according to their relevance to the five steps of EBM. EBM step 3—‘appraise’ was the most frequently assessed using a validated tool—all twelve tools (100%) identified assessed ‘appraise’. Three evaluated the first four steps of EBM, namely ask, acquire, appraise and apply. Seven (58%) evaluated ‘ask’, seven (58%) evaluated ‘acquire’ and 4 (33%) evaluated ‘apply’. None of the seven identified evaluated the last step—‘assess’ (Table 1).
Table 1.
Classification of tools against EBM steps evaluated
| Tool | EBM steps | ||||
|---|---|---|---|---|---|
| Ask | Acquire | Appraise | Apply | Assess | |
| Taylor’s questionnaire [14] | Yes | Yes | |||
| Berlin [7] | Yes | ||||
| Fresno [6] | Yes | Yes | Yes | ||
| ACE [15] | Yes | Yes | Yes | Yes | |
| Utrecht questionnaire U-CEP [16] | Yes | Yes | Yes | ||
| MacRae examination [17] | Yes | ||||
| EBM test [18] | Yes | Yes | Yes | ||
| Educational prescription [19] | Yes | Yes | Yes | Yes | |
| Mendiola-mcq [20] | Yes | ||||
| Tudiver OSCE [21] | Yes | Yes | Yes | ||
| Frohna’s OSCE [22] | Yes | Yes | Yes | Yes | |
| BACES [23] | Yes | ||||
Classification of tools according to the educational outcome domains measured
We have also differentiated tools according to their relevance to the seven dimensions of EBM learning, namely reaction to educational experience, attitudes, self-efficacy, knowledge, skills, behaviours and benefits to patients. Of the twelve tools, ten (83%) evaluated knowledge gain, nine (75%) EBM skills and one (8%) evaluated attitude. None addressed reactions to EBM teaching, self-efficacy, change in behaviours or patient benefit (Table 2).
Table 2.
Classification of tools against the seven educational outcome domains
| Outcome domains assessed by the twelve EBM instruments | |||||||
|---|---|---|---|---|---|---|---|
| Reaction to EBM teaching | Attitude | Self-efficacy | Knowledge | Skills | Behaviours | Patient benefit | |
| Taylor’s questionnaire | Yes | Yes | |||||
| Berlin | Yes | Yes | |||||
| Fresno | Yes | Yes | |||||
| ACE | Yes | Yes | |||||
| Utrecht questionnaire U-CEP | Yes | ||||||
| MacRae examination | Yes | Yes | |||||
| EBM test | Yes | Yes | |||||
| Educational prescription | Yes | Yes | |||||
| Mendiola | Yes | ||||||
| Tudiver OSCE | Yes | ||||||
| Frohna’s OSCE | Yes | ||||||
| BACES | Yes | Yes | |||||
Quality of EBM tools and taxonomy
Quality assessment ratings are presented in Table 3. Of the twelve tools included, six (50%) were judged to be of high quality supported by established (interrater reliability (if applicable), use of objective (non-self-reported) outcome measure(s) and demonstrated multiple (≥ 3) types of established validity evidence (including evidence of discriminative validity)).
Table 3.
High quality tools with ≥ 3 types of established validity
| Tool | Reported psychometric properties | |||||||
|---|---|---|---|---|---|---|---|---|
| Content validity | Interrater reliability | Internal validity | Responsive validity | Discriminative validity | Construct Validity | Internal reliability (ITC) | External validity | |
| Taylor’s questionnaire [14] | Yes | Yes | Yes | Yes | ||||
| Berlin [7] | Yes | Yes | Yes | Yes | ||||
| Fresno [6] | Yes | Yes | Yes | Yes | ||||
| ACE [15] | Yes | Yes | Yes | Yes | Yes | |||
| Utrecht questionnaire [16] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| MacRae [17] | Yes | Yes | Yes | Yes | Yes | |||
The validity assessments of the six high-quality tools used in evaluating EBM teaching in medical education are presented in Table 3. Evaluations of psychometric test properties of these tools are presented in Table 4, and their classification against the CREATE framework is presented in Table 5. The Taylor’s questionnaire [14] has a set of multiple-choice questions which assesses knowledge and attitudes and was initially validated in four groups of healthcare professionals with varying degrees of expertise (UK). It has since been assessed in a medical student cohort (Mexico). The Berlin questionnaire [7] measures basic knowledge about interpreting evidence from healthcare research and is built around clinical scenarios and have two separate sets of questions focusing on epidemiological knowledge and skills. It was initially evaluated in EBM experts, medical students and participants in EBP course (USA). The Fresno test [6] assesses medical professionals’ knowledge and skills and consists of two clinical scenarios with 12 open-ended questions. It was initially evaluated in family practice residents and faculty members (USA).
Table 4.
Details of studies where the high-quality tools (n = 6) were validated for use in evaluating EBM teaching in medical education
| Source instrument name and date | Instrument development-number of participants, level of expertise | EBM learning domains | Instrument description | EBM steps | Psychometric properties with results of validity and reliability assessment |
|---|---|---|---|---|---|
| Berlin questionnaire-Fritsche [7] | 266 participants—43 experts in evidence-based medicine, 20 controls (medical students) and 203 participants in evidence-based medicine course (USA) | Knowledge and skills | Berlin questionnaire was developed to measure basic knowledge about interpreting evidence from healthcare research, skills to relate a clinical problem to a clinical question, the best design to answer it and the ability to use quantitative information from published research to solve specific patient problems. The questions were built around clinical scenarios and has two separate sets of 15 multiple-choice questions mainly focusing on epidemiological knowledge and skills (scores range from 0 to 15) | Appraise |
Content validity Internal validity Responsive validity Discriminative validity The two sets of questionnaires were psychometrically equivalent: interclass correlation coefficient for students and experts 0.96 (95% confidence interval 0.92 to 0.98, p < 0.001). Cronbach’s alpha 0.75 for set 1 and 0.82 for set 2. Ability to discriminate between groups with different levels of knowledge by comparing the three groups with varying expertise: The mean score of controls (4.2 (2.2)), course participants (6.3 (2.9)) and experts (11.9 (1.6)) were significantly different (analysis of variance, p < 0.001) |
| Fresno test-Ramos et al. [6] | Family practice residents and faculty member (n = 43); volunteers self-identified as experts in EBM ( n = 53); family practice teachers (n = 19) (USA) | Knowledge and skills | Fresno test was developed and validated to assess medical professionals’ knowledge and skills. It consists of two clinical scenarios with 12 open-ended questions which are scored with standardised grading rubrics. Calculation skills were assessed by fill in the blank questions. | Ask, acquire and appraise |
Content validity Interrater reliability Internal validity Discriminative validity Expert opinion Interrater correlations ranged from 0.76 to 0.98 for individual items Cronbach’s alpha was 0.88. ITC ranged 0.47–0.75. Item difficulties ranged from moderate (73%) to difficult (24%). Item discrimination ranged from 0.41 to 0.86. Construct validity, on the 212 point test, the novice mean was 95.6 and the expert mean was 147.5 (p< 0.001) |
| MacRae [17] | Residents in University of Toronto General Surgery Program (n = 44) (Canada) | Knowledge and skills | Examination consisted of three articles each followed by a series of short-answer questions and 7-point rating scales to assess study quality. | Appraise |
Content validity Interrater reliability Internal validity Discriminative validity Construct validity Cronbach’s alpha 0.77 Interrater reliability—Pearson product moment correlation coefficient between clinical epidemiologist and non-epidemiologist-0.91 between clinical epidemiologist and nurse 0.78.Construct validity was assessed by comparing scores of those who attended the journal club versus those who did not and by postgraduate year of training (p= 0.02) |
|
Taylor [14] Bradley et al. [24] |
4 groups of healthcare professionals (n = 152 ) with varying degrees of expertise of EBP (UK) Group 1—with no or little prior EBP education 2—undertaken CASP workshop within last 4 weeks; 3—undertaken CASP workshop in the last 12 months; 4—academics currently teaching EBP and attended 1997 Oxford CEBM workshop Later, Bradley et al. tried with 175 medical students in RCT of self-directed vs workshop-based EBP curricula (Norway) |
Knowledge and attitudes |
Questionnaire 11mcqs -true, false, do not know Correct responses given 1 Incorrect responses scored 1 Do not know 0 |
Acquire and appraise |
Content validity Internal validity Responsive validity Discriminative validity Cronbach’s alpha (0.72 for knowledge and 0.64 for attitude questions) Spearman’s correlation (internal consistency), total knowledge and attitudes scores ranged from 0.12 to 0.66, discriminative validity (novice and expert) Responsiveness (instrument able to detect change) |
| ACE tool- Dragan Ilic [15] | 342 medical students—98 EBM-novice, 108 EBM-intermediate and 136 EBM-advanced participants (Australia) | Knowledge and skills | Assessing Competency in EBM (ACE )tool was developed and validated to evaluate medical trainees’ competency in EBM across knowledge, skills and attitudes—15 items, dochotomous outcome measure; items 1 and 2, asking the answerable question; items 3 and 4, searching literature; items 5–11 critical appraisal; items 12–15 relate to step 4 applying evidence to the patient scenario. | Ask, acquire, appraise and apply |
Content validity Interrater reliability Internal validity Responsive validity Discriminative validity Construct validity—statistically significant linear trend for sequentially improved mean score corresponding to the level of training (p< 0.0001) Item difficulty ranged from 36 to 84%, internal reliability ranged from 0.14 to 0.20, item discrimination ranged from 0.37 to 0.84, Cronbach’s alpha coefficient for internal consistency was 0.69 |
| Kortekaas-Utrecht questionnaire [16] (original questionnaire in Dutch, English version now available) | Postgraduate GP trainees (n=219), hospital trainees (n = 20), GP supervisors (n=20) academic GPs or clinical epidemiologists (n = 8) (Netherlands) | Knowledge | Utrecht questionnaire on knowledge on clinical epidemiology (U-CEP): two sets of 25 questions and a combined set of 50 | Ask, appraise and apply |
Content validity Internal validity Responsive validity Discriminative validity Content validity—expert opinion and survey Construct validity—significant difference in mean score between experts, trainees and supervisors Internal consistency—Cronbach alpha 0.79 for set A, 0.80 for set B and 0.89 for combined Responsive validity—significantly higher mean scores after EBM training than before EBM training Internal reliability—ITC using Pearson product, median 0.22 for set A, 0.26 for set B and 0.24 for combined Item Discrimination ability—median-0.35 for set A, 0.43 for set B and 0.37 for combined |
ITC item total correlation, RCT randomised controlled trial, CASP critical appraisal skills program, UCEP Utrecht questionnaire on knowledge on clinical epidemiology for evidence-based practice
Table 5.
Classification of the six high quality tools according to CREATE framework
| Assessment category | Type of assessment | Steps of EBM | |||||
|---|---|---|---|---|---|---|---|
| 7 | Benefits to patients | Patient-oriented outcomes | |||||
| 6 | Behaviours | Activity monitoring | |||||
| 5 | Skills | Performance assessment |
Fresno ACE |
Fresno ACE |
Berlin’s Fresno ACE MacRae |
ACE | |
| 4 | Knowledge | Cognitive testing |
Fresno ACE U-CEP |
Fresno ACE Taylor's |
Taylor’s Berlins Fresno ACE UCEP MacRae |
ACE UCEP |
|
| 3 | Self-efficacy | Self-report/opinion | |||||
| 2 | Attitudes | Taylor's | Taylor’s | ||||
| 1 | Reaction to the educational experience | ||||||
| Ask | Search | Appraise | Integrate | Evaluate | |||
Audience characteristic: students and trainees in medical education.
Assessment aims: formative
The ACE tool [15] evaluates medical trainees’ competency in EBM across knowledge, skills and attitudes and has 15 questions with dichotomous outcome measure. It was initially evaluated with medical students and professionals with different levels of EBM expertise (Australia). The Utrecht questionnaire has two sets of twenty-five questions testing knowledge on clinical epidemiology and was initially evaluated with postgraduate GP trainees, hospital trainees, GP supervisors, academic GPs or clinical epidemiologists (Netherlands). The MacRae examination consists of three articles each followed by a series of short-answer questions testing knowledge and skills which was evaluated in surgery residents (Canada).
Details of the remaining six tools identified in this review, which did not meet the criteria for ‘high-quality’ tools are presented in Table 6. These tools have been used to evaluate EBM in medical education and assess (a) the dimension(s) of EBM learning, namely reaction to educational experience, attitudes, self-efficacy, knowledge, skills, behaviours and benefits to patients; (b) different step(s) of EBM and (c) presented results of the psychometric performance of the tool. However, they have not demonstrated multiple (≥ 3) types of established validity evidence (including evidence of discriminative validity).
Table 6.
Details of studies which have used and validated six other tools identified as lower quality by this review for use in evaluating EBM teaching in medical education
| Source instrument name and date | Instrument development, number of participants, level of expertise | EBM learning domains | Instrument description | EBM steps | Psychometric properties with results of validity and reliability assessment |
|---|---|---|---|---|---|
| Educational Prescription-David Feldstein [19] | 20 residents | Knowledge and skills | Educat academic GPs or clinical ional prescription (EP)—web-based tool that guides learners through the four As of EBM. Learners use the EP to define a clinical question, document a search strategy, appraise the evidence, report the results and apply evidence to the particular patient | Asking, acquiring, appraising, applying |
Predictive validity Interrater reliability Interrater reliability on the 20 EPs showed fair agreement for question formation (k= 0.22); moderate agreement for overall competence (k = 0.57) and evaluation of evidence (k= 0.44). and substantial agreement for searching (k = 0.70) and application of evidence (k = 0.72) |
| BACES-Barlow [23] |
Yes postgraduate medical trainees/residents—150 residents |
Knowledge, skills | BACES-Biostatistics and Clinical Epidemiology Skills (BACES) assessment for medical residents-30 multiple-choice questions were written to focus on interpreting clinical epidemiological and statistical methods | Appraisal—interpreting clinical epidemiology and statistical methods |
Content validity was assessed through a four person expert review Item Response Theory (IRT) makes it flexible to use subsets of questions for other cohorts of residents (novice, intermediate and advanced). 26 items fit into a two parameter logistic IRT model and correlated well with their comparable CTT (classical test theory) values |
| David Feldstein-EBM test [18] | 48 internal medicine residents | Knowledge and skills | EBM test—25 mcqs-covering seven EBM focus areas: (a) asking clinical questions, (b) searching, (c) EBM resources, (d) critical appraisal of therapeutic and diagnostic evidence, (e) calculating ARR, NNT and RRR, (f) interpreting diagnostic test results and (g) interpreting confidence intervals |
Asking, acquiring and appraising Asking clinical questions, searching, EBM resources, critical appraisal, calculations of ARR, NNT, RRR, interpreting diagnostic test results and interpreting confidence intervals. |
Construct validity Responsive validity EBM experts scored significantly higher EBM test scores compared to PGY-1 residents (p < 0.001), who in turn scored higher than 1st year students (p < 0.004). Responsiveness of the test was also demonstrated with 16 practising clinicians—mean difference in fellows’ pre-test to post-test EBM scores was 5.8 points (95% CI 4.2, 7.4) |
| Frohna-OSCE [22] | Medical students (n-26) who tried the paper-based test during the pilot phase. A web-based station was then developed for full implementation (n = 140). | Skills | A web-based 20-min OSCE-specific case scenario where students asked a structural clinical question, generated effective MEDLINE search terms and elected the most appropriate of 3 abstracts | Ask, acquire, appraise and apply |
Face validity Interrater reliability Literature review and expert consensus Between three scorers, there was good interrater reliability with 84, 94 and 96% agreement (k = 0.64, 0.82 and 0.91) |
| Tudiver-OSCE [21] | Residents—first year and second year | Skills | OSCE stations | Ask, acquire, appraise and apply |
Content validity Construct validity p= 0.43 Criterion validity p < 0.001 Interrater reliability ICC 0.96 Internal reliability Cronbach’s alpha 0.58 |
| Mendiola-mcq [20] | Fifth year medical students | Knowledge | MCQ (100 questions) | Appraise |
Reliability of the mcq = Cronbach’s alpha 0.72 in M5 and 0.83 in M6 group Effect size in Cohen’s d for the knowledge score main outcome comparison of M5 EBM vs M5 non-EBM was 3.54 |
mcq multiple choice question, OSCE objective structured clinical examination, ICC intraclass correlation, NNT number needed to treat, ARR attributable risk ratio, RRR relative risk ratio
Assessment aims: formative
Discussion
This systematic review has identified twelve validated tools which can help evaluate EBM teaching in medical education. This review has focused on tools which used objective outcome measures, provided enough description of the tool, the EBM educational domains assessed, EBM steps assessed, and details of the psychometric tests carried out. Of the twelve tools identified, six were high-quality tools as supported by established (interrater reliability (if applicable), use of objective (non-self-reported) outcome measure(s) and demonstrated multiple (≥ 3) types of established validity evidence (including evidence of discriminative validity).
Of the five steps of EBM, ‘appraise’ was the most commonly evaluated step, followed by ‘ask’, ‘acquire’ and ‘apply’ steps. None of the tools identified evaluated the last step—‘assess’. Conducting an audit of clinical processes and outcomes and using activity diaries to document activities directly related to EBP have been suggested as possible methods of assessing EBP process [25]. Most tools evaluated knowledge and skills domains of the seven outcome domains. Few evaluated changes in attitude and behaviours. No tools were identified which could evaluate reaction to EBM teaching or the impact on patient benefit. Challenges in measuring the impact of patient benefit might be because the impact is often latent and distant and the difficulty in isolating the effect of EBM from the role of the overarching team and healthcare system on patient outcomes [8].
This is the first systematic review which has provided EBM educators in medical education a compendium of currently available high-quality tools to evaluate teaching of EBM. We have also categorised the six high quality tools identified by this review according to the CREATE framework [11] to provide a taxonomy which can help medical educators decide on the most appropriate tool(s) available to evaluate their EBM teaching. The taxonomy has categorised tools against the EBM steps and the EBM educational domains, to help developers of new tools to identify and where possible address the current gaps.
Shaneyfelt et al. [5] identified 104 unique assessment strategies in 2006, which could be used to evaluate EBP (evidence-based practice) and found that most evaluated EBM skills. In line with the present review, they also noted that of the EBP skills, acquiring evidence and appraising evidence were most commonly evaluated. Of the 104 tools identified, they categorised seven as level 1, they were supported by established interrater reliability (if applicable), objective (non-self-reported) outcome measures, and multiple (≥ 3) types of established validity evidence (including evidence of discriminative validity) [5]. The authors specifically identified the Fresno [6] and Berlin [7] as the only high quality instruments for evaluating knowledge and skills of individual trainees across the EBP steps. The 2006 review [5], however, did not categorise the level 1 tools according to the EBM educational domains assessed.
Since the 2006 review, two new tools have been identified for use in medical education with similar quality as the initial level 1 tools—ACE and Utrecht questionnaire [15, 16]. There have been more recent reviews which have included these tools—a recent review in 2013 carried out by Oude Rengerink et al [9] identified 160 different tools that assessed EBP behaviour amongst all healthcare professionals. However, the authors found that most of them subjectively evaluated a single step of EBP behaviours without established psychometric properties. They did not find any tool with established validity and reliability which evaluated all five EBP steps.
Leung et al. [26] in their 2014 review of tools for measuring nurses’ knowledge, skills and attitudes for evidence-based practice identified 24 tools, of which only one had adequate validity—the evidence-based practice questionnaire [27]. However, the authors note that the evidence-based practice questionnaire relies entirely on self-report rather than direct measurement of competence. Thomas et al. in their 2015 systematic review of evidence-based medicine tests for family physician residents found that only the Fresno test had been evaluated with more than one group of family medicine residents and had the best documentation of validity and reliability [10].
The specific focus of this review on tools used in medical education (excluding other healthcare professionals) offers unique insight and information of use to medical educators. In addition to presenting details of the identified tools, we have provided a taxonomy of tools which have been categorised according to the EBM steps evaluated and the educational outcome domains measured. We have used the qualities of level 1 category tools suggested by Shaneyfelt et al. to provide a current list of six high-quality tools and have classified them according to CREATE framework. We found that while earlier tools evaluated fewer steps of EBM and educational outcome domains, there is an increasing focus on developing more comprehensive tools which can evaluate all steps of EBM and all educational outcome domains. While most of the tools identified in this review had some validation, recent tools have had more psychometric tests performed and reported. The most recent of the tools, the Utrecht questionnaire has specifically undergone rigorous validation. The authors have carried out tests of internal consistency, internal reliability (item-total correlation), item discrimination index, item difficulty, content validity, construct validity, responsiveness, test-retest reliability, feasibility and external validation.
Similar to previous reviews [8, 10, 26], while categorising the high-quality tools against the five EBM steps, we found that the majority of validated tools focus on ‘appraise’, and fewer tools have focused on the other steps ‘ask’, ‘acquire’ and ‘apply’. There is also a need for tools which can address the last step of EBM—‘assess’. Translating research findings into clinical decisions is an important lifelong skill for healthcare professionals. EBM is not just about the ability to ask the right question, followed by searching and appraising the quality of evidence. It is bringing together clinical expertise, patient values and current best evidence into clinical decision making [1]. Multifaceted clinically integrated teaching methods along with evaluation of EBM knowledge, skills, attitudes and behaviour using validated tools can help in enhancing EBM competencies [4].
This review has identified some gaps in tools available for EBM teaching. There is a need for tools which can address all aspects of EBM steps- in particular, ‘apply’ and ‘assess’. Evidence suggests that medical education often focuses on teaching and assessing students on the first three steps of EBM—ask, acquire and appraise [8, 28]. Medical trainees should be taught how to bring together the evidence, patients’ preferences and clinical expertise in clinical decisions. As assessment drives learning, trainees should then be assessed on this step of EBM to encourage them to be lifelong learners. Secondly, within educational domains, most tools evaluate knowledge and skills with very few evaluating attitudes and behaviour. Researchers in medical education need to explore new tools which can evaluate all steps of EBM and educational outcome domains. Researchers also need to publish information on the feasibility of implementing the tools—time taken to complete and grade along with any other resource implications. This can help medical educators in making decisions about the feasibility of using these tools in assessing the effectiveness of EBM teaching. In our review, we found that while five tools had details on the feasibility of administering them, seven did not have any specific details.
This systematic review may have some limitations. We may have missed some tools, especially the ones which might have been published in grey literature. However, we searched multiple databases using a robust search strategy and screened citations from retrieved articles. Another limitation is that there may be some inaccuracies in reporting the tools against the educational outcome domains, EBM steps and validity tests. We tried to address this by having two independent reviewers extract data against the agreed checklist from the final list of articles; which was then verified by a third reviewer. Lastly our review was limited to tools used in medical education. Though literature suggests that several of these tools have also been used in other healthcare professions like nursing, dentistry and allied health professionals.
In summary, this review has helped to develop a taxonomy of the available tools based on their psychometric properties such as reliability and validity; relevance to the five EBM domains and the seven dimensions of EBM learning suggested by the CREATE framework. This will assist EBM educators in medical education in selecting the most appropriate and psychometrically validated measures to evaluate EBM teaching.
Supplementary information
Acknowledgements
None
Authors’ contributions
BK, JH, RP and DN led the development of the study. DN, JH, LJ and RP provided methodological input. BK and JH independently searched, screened the papers and extracted the data; LJ independently extracted data and confirmed findings with BK and JH. BK drafted the manuscript. JH, LJ, RP, DN and CJS read and approved the final manuscript.
Authors’ information
BK is a senior clinical lecturer and a PhD student in the University of Buckingham Medical School. DN is the Director of the Post Graduate Certificate in Teaching Evidence-Based Health Care and senior research fellow at the Centre for Evidence Based Medicine, Oxford. JH is a lecturer in the Department of Psychology, Manchester Metropolitan University. LJ is a biomedical lecturer in the University of Birmingham City. RP is a librarian in the University of Buckingham. CJS is a senior lecturer in the University of Buckingham Medical School.
Funding
There is no funding documentation relevant to this study. This article represents an independent research project funded by an internal University of Buckingham Medical School PhD studentship and the systematic review forms part of that PhD project. The views expressed in this protocol are those of the authors.
Availability of data and materials
The data are available to all interested researchers upon request. Please contact the corresponding author.
Ethics approval and consent to participate
This review did not require ethical approval as it only summarised published studies with non-identifiable data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bharathy Kumaravel, Email: Bharathy.Kumaravel@buckingham.ac.uk.
Jasmine Heath Hearn, Email: j.hearn@mmu.ac.uk.
Leila Jahangiri, Email: Leila.Jahangiri@bcu.ac.uk.
Rachel Pollard, Email: rachel.pollard@buckingham.ac.uk.
Claire J. Stocker, Email: Claire.stocker@buckingham.ac.uk
David Nunan, Email: david.nunan@phc.ox.ac.uk.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13643-020-01311-y.
References
- 1.Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence-based medicine: how to practice and teach EBM. 2019. [Google Scholar]
- 3.Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ. 2004;329(7473):1017. doi: 10.1136/bmj.329.7473.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young T, Rohwer A, Volmink J, Clarke M. What Are the Effects of Teaching Evidence-Based Health Care (EBHC)? Overview of Systematic Reviews. PLoS One. 2014;9(1):e86706. doi: 10.1371/journal.pone.0086706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaneyfelt T, Baum KD, Bell D, Feldstein D, Houston TK, Kaatz S, et al. Instruments for Evaluating Education in Evidence-Based Practice: A Systematic Review. JAMA. 2006;296(9):1116. doi: 10.1001/jama.296.9.1116. [DOI] [PubMed] [Google Scholar]
- 6.Ramos KD. Validation of the Fresno test of competence in evidence based medicine. BMJ. 2003;326(7384):319–321. doi: 10.1136/bmj.326.7384.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fritsche L, Greenhalgh T, Falck-Ytter Y, Neumayer H-H, Kunz R. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325(7376):1338–1341. doi: 10.1136/bmj.325.7376.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albarqouni L, Hoffmann T, Glasziou P. Evidence-based practice educational intervention studies: a systematic review of what is taught and how it is measured. BMC Med Educ. 2018;18(1) Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-018-1284-1. Cited 2018 Nov 27. [DOI] [PMC free article] [PubMed]
- 9.Oude Rengerink K, Zwolsman SE, Ubbink DT, Mol BWJ, van Dijk N, Vermeulen H. Tools to assess Evidence-Based Practice behaviour among healthcare professionals. Evid Based Med. 2013;18(4):129–138. doi: 10.1136/eb-2012-100969. [DOI] [PubMed] [Google Scholar]
- 10.Thomas RE, Kreptul D. Systematic review of evidence-based medicine tests for family physician residents. Fam Med. 2015;47(2):101–117. [PubMed] [Google Scholar]
- 11.Tilson JK, Kaplan SL, Harris JL, Hutchinson A, Ilic D, Niederman R, et al. Sicily statement on classification and development of evidence-based practice learning assessment tools. BMC Med Educ. 2011;11(1) Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-11-78. Cited 2019 Feb 16. [DOI] [PMC free article] [PubMed]
- 12.Freeth D. Learning and Teaching Support Network. A critical review of evaluations of interprofessional education. London: LTSN-Centre for Health Sciences and Practice; 2002. [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(jul21 1):b2535–b2535. [PMC free article] [PubMed]
- 14.Taylor R, Reeves B, Mears R, Keast J, Binns S, Ewings P, et al. Development and validation of a questionnaire to evaluate the effectiveness of evidence-based practice teaching. Med Educ. 2001;35(6):544–547. doi: 10.1046/j.1365-2923.2001.00916.x. [DOI] [PubMed] [Google Scholar]
- 15.Ilic D, Nordin RB, Glasziou P, Tilson JK, Villanueva E, et al. BMC Med Educ. 2014;14(1) Available from: http://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-14-114. Cited 2018 Nov 28. [DOI] [PMC free article] [PubMed]
- 16.Kortekaas MF, Bartelink M-LEL, de Groot E, Korving H, de Wit NJ, Grobbee DE, et al. The Utrecht questionnaire (U-CEP) measuring knowledge on clinical epidemiology proved to be valid. J Clin Epidemiol. 2017;82:119–127. doi: 10.1016/j.jclinepi.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 17.MacRae HM, Regehr G, Brenneman F, McKenzie M, McLeod RS. Assessment of critical appraisal skills. Am J Surg. 2004;187(1):120–123. doi: 10.1016/j.amjsurg.2002.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Feldstein DA, Maenner MJ, Srisurichan R, Roach MA, Vogelman BS. Evidence-based medicine training during residency: a randomized controlled trial of efficacy. 2010;10(1) Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-10-59. Cited 2019 Sep 13. [DOI] [PMC free article] [PubMed]
- 19.Feldstein DA, Mead S, Manwell LB. Feasibility of an evidence-based medicine educational prescription. Med Educ. 2009;43(11):1105–1106. doi: 10.1111/j.1365-2923.2009.03492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sánchez-Mendiola M, Kieffer-Escobar LF, Marín-Beltrán S, Downing SM, Schwartz A. Teaching of evidence-based medicine to medical students in Mexico: a randomized controlled trial. BMC Med Educ. 2012;12(1) Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-12-107. Cited 2019 Sep 13. [DOI] [PMC free article] [PubMed]
- 21.Tudiver F, Rose D, Banks B, Pfortmiller D. Reliability and validity testing of an evidence-based medicine OSCE station. Fam Med. 2009;41(2):89–91. [PubMed] [Google Scholar]
- 22.Frohna JG, Gruppen LD, Fliegel JE, Mangrulkar RS. Development of an Evaluation of Medical Student Competence in Evidence-Based Medicine Using a Computer-Based OSCE Station. Teach Learn Med. 2006;18(3):267–272. doi: 10.1207/s15328015tlm1803_13. [DOI] [PubMed] [Google Scholar]
- 23.Barlow PB, Skolits G, Heidel RE, Metheny W, Smith TL. Development of the Biostatistics and Clinical Epidemiology Skills (BACES) assessment for medical residents. Postgrad Med J. 2015;91(1078):423–430. doi: 10.1136/postgradmedj-2014-133197. [DOI] [PubMed] [Google Scholar]
- 24.Bradley P, Oterholt C, Herrin J, Nordheim L, Bjorndal A. Comparison of directed and self-directed learning in evidence-based medicine: a randomised controlled trial. Med Educ. 2005;39(10):1027–35. doi: 10.1111/j.1365-2929.2005.02268.x. [DOI] [PubMed] [Google Scholar]
- 25.Ilic D. Assessing competency in Evidence Based Practice: strengths and limitations of current tools in practice. BMC Med Educ. 2009;9(1) Available from: https://bmcmededuc.biomedcentral.com/articles/10.1186/1472-6920-9-53. Cited 2020 Jan 12. [DOI] [PMC free article] [PubMed]
- 26.Leung K, Trevena L, Waters D. Systematic review of instruments for measuring nurses’ knowledge, skills and attitudes for evidence-based practice. J Adv Nurs. 2014;70(10):2181–2195. doi: 10.1111/jan.12454. [DOI] [PubMed] [Google Scholar]
- 27.Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. J Adv Nurs. 2006;53(4):454–458. doi: 10.1111/j.1365-2648.2006.03739.x. [DOI] [PubMed] [Google Scholar]
- 28.Meats E, Heneghan C, Crilly M, Glasziou P. Evidence-based medicine teaching in UK medical schools. Med Teach. 2009;31(4):332–337. doi: 10.1080/01421590802572791. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available to all interested researchers upon request. Please contact the corresponding author.