Abstract
A 69-year-old man had experienced right chest pain for several months. Chest computed tomography (CT) showed a right upper lobe lung tumor and swelling of multiple mediastinal and right hilar lymph node. Three punctures to 4R lymph nodes and two punctures to 11i lymph nodes were performed, using endobronchial ultrasonography. Thirty days after punctures, he was admitted with appetite loss and general fatigue. Chest CT supposed the evidence of mediastinitis and pericarditis. Despite the antibiotics, cardiac tamponade developed on the third hospital day. Pericardial fenestration and pericardial drainage were performed. Gram-positive cocci were identified and Gemella sanguinis was eventually identified as the microbial identification system. Like the former reports, the necessity of surgical procedure for late onset of mediastinitis and pericarditis. caused by EBUS-TBNA was suggested.
1. Introduction
Evaluation of the hilar and mediastinal lymph nodes is particularly important for therapeutic decision-making when treating lung cancer; compared to mediastinoscopy, endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive technique for investigating mediastinal and hilar lymph nodes [1]. According to a systematic review and meta-analysis, the rate of major complications with EBUS-TBNA is 0.07% [2]. In a Japanese study, complications were reported in 17 of 3689 (0.46%) bronchoscopies [3]. EBUS-TBNA is generally a safe intervention; however, the possibility of severe side effects remains, and most occur early in the post-operative period. Here, we report a case with late onset infectious complications of EBUS-TBNA.
2. Case
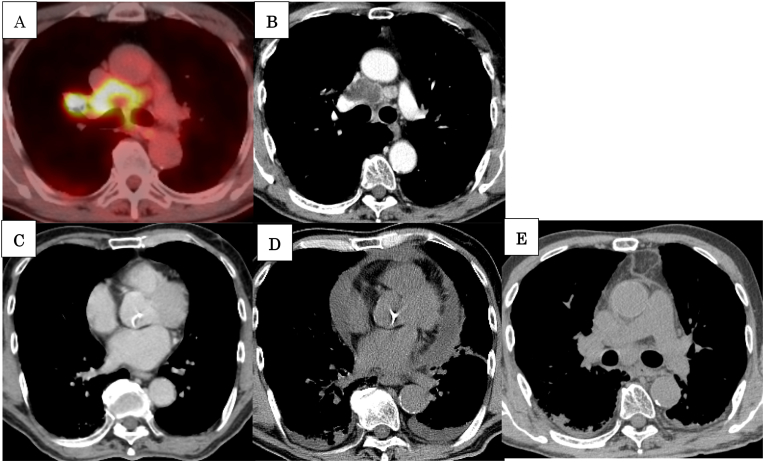
A 69-year-old man with preexisting hypertension and severe emphysema had experienced right-sided chest pain for several months. He had smoked a pack of cigarettes per day for 44 years. Chest computed tomography (CT) showed a tumor in the upper lobe of the right lung, and enlargement of multiple mediastinal and right hilar lymph nodes (Fig. 1A and B). Endobronchial lung biopsy was performed under ultrasonographic guidance, using a guide sheath; no malignant cells were found using rapid on-site cytologic evaluation. EBUS-TBNA was performed using the UC260FW (Olympus, Tokyo, Japan) bronchoscope to obtain tissue. A single-use 22-G needle was used for needle aspiration. The needle aspirate was obtained using the stylet push out method. The lung tumor and mediastinal lymph nodes were found to be necrotic (Fig. 1B); the necrotic areas were avoided under ultrasonographic guidance during aspiration. Three and two needle aspirates were obtained from the 4R and 11i lymph nodes, respectively. The histologic diagnosis was that of non-small cell lung cancer with neuroendocrine differentiation and considerable necrosis. Microbiological examination of the samples revealed no clinically significant bacteria.
Fig. 1.
18-F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) showing uptake of FDG at the right hilar and mediastinal lymph nodes (A). Chest enhanced CT showing the low-density area inside the mediastinal lymph node, indicative of necrosis (B). The CT at 24 days after EBUS-TBNA showing no evidence of enlargement of mediastinal nodes or cardiac effusion (C). Chest CT obtained 30 days after EBUS-TBNA showing pericardial effusion (D), and enlargement of mediastinal lymph nodes with increased fat tissue concentration (E).
Thirty days after the procedure, the patient was admitted to our hospital with loss of appetite and general fatigue, without fever. The chest CT scan revealed further enlargement of the lymph nodes with pericardial effusion (Fig. 1D and E). Six days before admission, a CT scan for planning radiation therapy revealed no complications from EBUS-TBNA (Fig. 1C). Although tazobactam/piperacillin was empirically administered to treat the mediastinitis and pericarditis, cardiac tamponade developed on the third hospital day. Pericardial fenestration and drainage were accordingly performed. The pericardial fluid obtained appeared yellow and turbid; Gram-positive cocci were identified on examination. We therefore diagnosed an infection in the mediastinal lymph nodes and pericardium, consequent to EBUS-TBNA. Intravenous vancomycin was added to the tazobactam/piperacillin regimen. Five days after pericardial fenestration, the antibiotic regimen was de-escalated to intravenous ampicillin/sulbactam; at 28 days after pericardial fenestration, the antibiotic regimen was de-escalated to oral amoxicillin hydrate for 4 weeks. Chemoradiation therapy for lung cancer was initiated 25 days after pericardial fenestration, without further complications. On anaerobic culture, the pericardial effusion demonstrated the growth of colonies, which were identified on subculture. Gemella sanguinis was eventually identified using the MALDI biotyper@ ver.3.1 (Bruker Daltonics) microbial identification system.
3. Discussion
Infections such as mediastinitis, pericarditis, and abscesses are reportedly caused by EBUS-TBNA [4,5]. Most infections caused by EBUS-TBNA have been reported to occur within one month; in two reported cases, infectious mediastinitis developed over 30 days after the procedure [5,6]. In these cases, Streptococcus spp was the causative bacterium [7]. Ishimoto et al. suggested the necessity of surgery for late-onset endocarditis caused by EBUS-TBNA. Similar to the findings in these reports, cardiac tamponade developed in our case despite antibiotic treatment, necessitating pericardial fenestration. The strategy for treating pericarditis caused by EBUS-TBNA may be planned depending on the surgical procedure. Gemella sanguinis, the causative organism in our case, is a slow-growing bacterium similar to auxotrophic streptococci. Since prophylactic antibiotics were administered after EBUS-TBNA, the infection was of late-onset. We should recognize that infections caused by EBUS-TBNA may develop over one month after the procedure.
In humans, Gemella sanguinis is found on mucus membranes, including the oropharynx, gastrointestinal tract, and genitourinary tract. The risk factors for infections with Gemella spp. include underlying dental and heart disease. In our case, the patient had no heart disease; however, he had poor oral hygiene, and had full dentures.
The bacteria invade by contamination of the airway from the bronchoscopic fibers from the oral cavity, and while removing the needle aspirate needle from the channel. In this case, internal necrosis was confirmed by enhanced CT; infection should therefore be carefully prevented. Although the examination was performed by avoiding the necrotic tissue, the number of needle aspirates obtained should have been reduced. The importance of oral care before bronchoscopy has been emphasized, and our hospital has initiated efforts to improve dental hygiene before investigation. This case highlights the need to consider the possibility of late-onset pericarditis caused by EBUS-TBNA.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Takako Inoue, Email: okuyama-ta@mc.pref.osaka.jp.
Tatsuya Nishikawa, Email: nishikawa-ta@mc.pref.osaka.jp.
Kei Kunimasa, Email: kunimasa-ke@mc.pref.osaka.jp.
Motohiro Tamiya, Email: moto19781205@yahoo.co.jp.
Hanako Kuhara, Email: kuhara-ha@mc.pref.osaka.jp.
Kazumi Nishino, Email: nisino-ka@mc.pref.osaka.jp.
Mamoru Fujiwara, Email: fujiwaram@opho.jp.
Masashi Fujita, Email: masashi.fujita@oici.jp.
Fumio Imamura, Email: imamura-fu@mc.pref.osaka.jp.
Toru Kumagai, Email: kumagai-to@mc.pref.osaka.jp.
References
- 1.Yasufuku K., Chhajed P.N., Sekine Y., Nakajima T., Chiyo M., Iyoda A., Yoshida S., Otsuji M., Shibuya K., Iizasa T., Saitoh Y., Fujisawa T. Endobronchial ultrasound using a new convex probe: a preliminary study on surgically resected specimens. Oncol. Rep. 2004;11:293–296. [PubMed] [Google Scholar]
- 2.Gu P., Zhao Y.Z., Jiang L.Y., Zhang W., Xin Y., Han B.H. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur. J. Canc. 2009;45:1389–1396. doi: 10.1016/j.ejca.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 3.Asano F., Aoe M., Ohsaki Y., Okada Y., Sasada S., Sato S., Suzuki E., Senba H., Fujino S., Ohmori K. Deaths and complications associated with respiratory endoscopy: a survey by the Japan Society for Respiratory Endoscopy in 2010. Respirology. 2012;17:478–485. doi: 10.1111/j.1440-1843.2011.02123.x. [DOI] [PubMed] [Google Scholar]
- 4.Haas A.R. Infectious complications from full extension endobronchial ultrasound transbronchial needle aspiration. Eur. Respir. J. 2009;33:935–938. doi: 10.1183/09031936.00025708. [DOI] [PubMed] [Google Scholar]
- 5.Huang C.T., Chen C.Y., Ho C.C., Yu C.J. A rare constellation of empyema, lung abscess, and mediastinal abscess as a complication of endobronchial ultrasound-guided transbronchial needle aspiration. Eur. J. Cardio. Thorac. Surg. 2011;40:264–265. doi: 10.1016/j.ejcts.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 6.Kouskov O.S., Almeida F.A., Eapen G.A., Uzbeck M., Deffebach M. Mediastinal infection after ultrasound-guided needle aspiration. J Bronchology Interv Pulmonol. 2010;17:338–341. doi: 10.1097/LBR.0b013e3181f30d74. [DOI] [PubMed] [Google Scholar]
- 7.Ishimoto H., Yatera K., Uchimura K., Oda K., Takenaka M., Kawanami T., Tanaka F., Mukae H. A serious mediastinum abscess induced by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA): a case report and review of the literature. Intern. Med. 2015;54:2647–2650. doi: 10.2169/internalmedicine.54.4465. [DOI] [PubMed] [Google Scholar]