Abstract
Objective
To estimate correlates of early intervention (EI) service dosage and gains in children’s functional capabilities from EI entry and discharge.
Design
Retrospective cohort study
Setting
Secondary analyses of a subset of data (n=1,005) collected from an EI administrative database on children discharged from a large, urban EI program between 10/1/2014 and 9/30/16.
Participants
Children who were EI eligible due to developmental delay, had received an EI care plan and at least 1 billable EI service, and had outcomes data at EI entry and exit.
Measured child characteristics included age (49.0% 12–24 months [n=492]), sex (36.0% female [n=362]), number of developmental delays (76.1% had one developmental delay [n=765]), and number of EI services received (78.5% received multiple [n=789]).
Intervention
N/A
Main Outcome Measures
Outcomes were EI service intensity (hours per month) and change in functional capabilities as measured via the state-mandated Child Outcomes Summary (COS). Adjusted quantile median regression estimated EI intensity. Adjusted linear regression estimated change in function for social-emotional, cognitive, and adaptive domains of the COS. Measures of children’s developmental delay severity, age at EI entry, race and ethnicity, sex, and language.
Results
Children older than 24 months old experienced significantly higher EI service intensity (b=0.40, 95% CI: 0.18, 0.63). Child age and EI service intensity were significantly linked to gains in social and cognitive COS score changes from EI entry to exit.
Conclusion(s)
Older children receive a higher intensity of EI services. EI service intensity and age were linked with positive changes in functional gains.
Keywords: early intervention, activities of daily living, cognition, social skills
Early intervention (EI) is a system that provides access to rehabilitation services for approximately 2–3% of infants and young children with developmental needs nationally.1 EI emphasizes family-centered, coordinated care often delivered using a transdisciplinary team approach and within the child’s natural learning environments (e.g., home, community)2–4, because a primary goal of EI is to help children optimally function in their homes and communities. Disparities in EI service access and intensity are related to children’s social (e.g., child age) and clinical (e.g., developmental delay) characteristics.5,6 Yet, there is limited evidence about how child characteristics and EI services relate to outcomes.
A results-driven accountability system provides unprecedented opportunity to examine the adequacy of EI services relative to outcomes. EI now calls for states to report on child functional outcomes at service entry and exit7. Most states choose to use the child outcomes summary (COS) to report on a child’s activity competence according to their social-emotional, cognitive, and adaptive capabilities at EI entry and exit. Since COS outcomes are aligned with contemporary pediatric rehabilitation frameworks that emphasize children’s activity competence as a key rehabilitation outcome, COS data can be used to build evidence about rehabilitation relevant outcomes for EI populations.8–10
While activity competence is a commonly quantified outcome in pediatric rehabilitation, few studies have examined the association between EI service use and gains in activity competencies.11 A number of large sample studies have established the significant role of young children’s activity competence on their participation in valued home and community activities.12,13 Even among preschoolers who received EI, children’s activity competencies were negatively associated with participation difficulty across most community activities.14 While these studies have not been conducted longitudinally, they suggest longer- term consequences of poor activity competence at EI discharge. Therefore, there is need to examine factors associated with children’s activity competence while accounting for EI service use.
As compared to efficacy studies carried out in controlled research conditions, COS data can be paired with other rehabilitation relevant data elements routinely collected by EI programs to estimate the role of EI service use on activity competence. When COS data are paired with data on social and clinical characteristics of EI eligible children and families, and the type and amount of EI services rendered, it becomes possible to estimate the relative impact of EI services on children’s functional progress. However, to our knowledge, only one study has used these data in combination to estimate child functional progress as a function of EI service use, conditional on select child and family characteristics. In this study, Noyes- Grosser and colleagues7 established children with Autism Spectrum Disorder received higher intensity EI and made functional gains in one or more COS domains at EI exit. Since nearly two-thirds of children receiving EI services present with developmental delay (no diagnosis)15, there is critical need to understand EI service use and functional outcomes among the majority of children who receive EI.
The purpose of this study was to estimate child and family characteristics associated with EI service intensity (aim 1), and to examine the impact of child and family characteristics and EI service intensity on changes in children’s activity competence by EI discharge (aim 2). We hypothesized child age at EI entry, functional abilities, and higher EI intensity will be associated with change in social-emotional, adaptive, and cognitive functioning by EI exit.
Methods
Setting and Participants
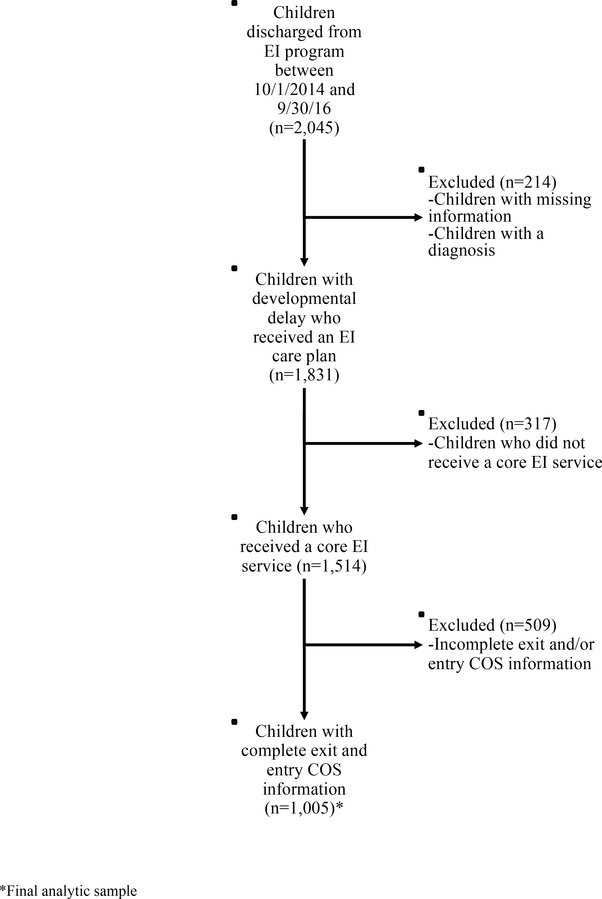
Multi-site institutional ethics approval was obtained prior to data extraction. The study sample was ascertained from electronic administrative data at a large EI program in Colorado that enrolls approximately 1,000 families annually.16 Data were originally extracted from records of children who were discharged between 10/1/2014 and 9/30/16, following the adoption of an expanded electronic data capture system by the EI program (n=2,045). As shown in Figure 1, this study leverages a subset of data (n=1,005, 66%) on children who were EI eligible due to developmental delay (i.e., sample children did not have a concomitant developmental disability), had received an EI care plan and at least 1 billable EI service, and had COS data at EI entry and exit. In Colorado, developmental delay is defined as 25% or greater delay in one or more areas of development based on standardized evelopmental assessments administered by the EI team17
Figure.
Enrollment diagram
COS = Child Outcomes Summary; EI= early intervention
Measures and Framework
The choice of measures was primarily informed by existing participation related constructs in a contemporary conceptual framework highlighting children’s cognitive, physical, and social-emotional skills and independence when executing discrete tasks according to an expected standard (i.e., their activity competence).9,18,19 As a participation-related construct, a child’s activity competence can be measured according to their use of skills and abilities in a daily environment and is influenced by extrinsic factors to the child, like the EI service context that includes rehabilitation and developmental therapies that focus on function.8,20,21 For this study, we considered how changes in children’s activity competence from EI entry to exit were influenced by child and family characteristics and EI service intensity.
Change in Activity Competence
Change in a child’s activity competence (i.e., their functional capabilities) was measured as the difference in COS scores22 generated at EI entry and exit for three domains: 1) social-emotional (“positive social emotional skills, including social relationships”), 2) cognitive (“acquisition and use of knowledge and skills, including early language/communication and early literacy”), and 3) adaptive (“use of appropriate behaviors to meet their needs”). The three COS scores are endorsed by the Office of Special Education Programs and are used to develop a functional profile of the child that is monitored from EI entry to EI exit. Each of the three COS scores is derived from a team consensus rating process in which caregiver and EI practitioner observations of a child’s functional capabilities, as well as a child’s assessment results inform the team’s rating of the child’s functional capabilities. Each score is on a 7-point scale, from 1=very early skills (i.e., child does not use any immediate foundational skills related to this outcome) to 7=all skills expected (i.e., there are no concerns about the child’s function in this area). A 13-point scale (ranging from −6 to 6) was used to represent change in functional capabilities for each domain as the exit COS score minus the entry COS score.
EI Service Intensity
EI service intensity was operationalized as total hours per month of core EI services (i.e., occupational therapy [OT], physical therapy [PT], speech therapy [ST] and developmental intervention [DI]) divided by EI enrollment length (in months), to estimate total EI service hours per month. To increase interpretability in the final models estimating the association between EI service intensity (i.e., service dosage) and change in activity competence, we created categories of EI service intensity (i.e., less than 2 hours per month, from 2 and up to 3 hours per month, from 3 and up to 4 hours per month, and 4 or more hours per month). Generally, service intensity did not change over time for individual children (J. Litfin, personal communication).
Child Characteristics
We included select child and family characteristics as informed by prior studies on social disparities in EI access23–26, service utilization5, and functional outcomes.14,15 Predisposing characteristics27, which are social factors that increase the likelihood of EI access, included the child’s ethnicity, age at EI entry, sex, and language. Child ethnicity was categorized as white, non-Hispanic (WNH); black, non-Hispanic (BNH); Hispanic; and other, non-Hispanic (ONH; includes Asian, Pacific Islander and children reporting more than one ethnicity). Age at EI entry was grouped into infants (under 12 months), 1-year-olds (12–23 months), and 2-year-olds (24–36 months). We also included a measure of child sex (male, female), and primary language spoken at home (English versus a language other than English). For this study, the enabling characteristic27, which is a factor associated with means to accessing EI services, was health insurance type, categorized as private versus public (Medicaid or CHP+). To describe service need, the number of developmental delays (e.g., gross and fine motor delay) was included as a proxy for condition severity [1, 2, 3 or more].
Statistical Analysis
Analyses were conducted in Stata 14.2. Descriptive statistics were used to summarize sample characteristics and EI service use according to service dosage and number of core EI services. For continuous variables, sample means, medians, and standard deviations were calculated. Due to skewed distribution, inter-quartile ranges (IQR) were used to describe EI service utilization. Sample proportions were calculated for categorical variables.
To estimate the association between child and family characteristics and EI service intensity (aim 1), we fit an adjusted median quantile regression model, which estimates the median rather than the mean, and accounts for the skewed distribution of the outcomes data on EI service utilization. For these models, we report the beta coefficient and the 95% confidence interval (CI). These coefficients are interpreted as the association between an additional hour per month of EI service intensity and each child characteristic, relative to the reference group.
To estimate the association between EI service use intensity and change in activity competency (aim 2), we fit an adjusted linear regression model. Specifically, we estimated the association between the difference in COS scores from EI entry to exit and EI service intensity and child and family characteristics. For these models, we report the beta coefficient and the 95% CI. These coefficients are interpreted as the association between a one-unit change (i.e., an additional COS score point) in function for each category of service intensity and each child characteristic, relative to the reference group.
Results
Sample Characteristics
As shown in Table 1, over half of the sampled children were from an ethnic minority group or publicly insured. A total of 388 children (38.6%) were Hispanic, 94 children (9.4%) BNH, and 362 children (36.0%) were female. Most children (76.1%) had a developmental delay in 1 of 5 areas of standardized assessment, while 12.4% had a delay in three or more developmental areas. In 789 households (78.5%), English was the primary language.
Table 1.
Child predisposing and clinical characteristics and service need
|
n (%) |
|
|---|---|
| Number of Delay Conditions | |
| 1 | 765 (76.1) |
| 2 | 115 (11.4) |
| 3 or more | 125 (12.4) |
| Child’s Age (months) | |
| < 12 | 199 (19.8) |
| 12–24 | 492 (49.0) |
| >24 Months | 314 (31.2) |
| Ethnicity | |
| White, non-Hispanic | 458 (45.6) |
| Black, non-Hispanic | 94 (9.4) |
| Hispanic | 388 (38.6) |
| Other, non-Hispanic | 65 (6.5) |
| Primary Language, English | 789 (78.5) |
| Child Sex, Female | 362 (36.0) |
| Mean (SD) |
|
| Entry COS | |
| Positive Social-Emotional Skills | 5.07 (1.65) |
| Acquiring and Using Knowledge and Skills | 3.96 (1.53) |
| Taking Appropriate Action to Meet Needs | 4.58 (1.65) |
| Exit COS | |
| Positive Social-Emotional Skills | 4.62 (2.77) |
| Acquiring and Using Knowledge and Skills | 4.29 (2.66) |
| Taking Appropriate Action to Meet Needs | 4.55 (2.73) |
| Difference in COS (Exit COS - Entry COS) | |
| Positive Social-Emotional Skills | −0.45 (2.90) |
| Acquiring and Using Knowledge and Skills | 0.33 (2.87) |
| Taking Appropriate Action to Meet Needs | −0.04 (2.84) |
COS = Child Outcomes Summary.
Average COS scores at EI entry were highest for social-emotional (M=5.07, SD=1.65) and lowest for cognitive (M=3.96, SD=1.53). In comparison, average COS scores at exit were similar for the three areas at EI exit: 1) social-emotional (M=4.62, SD=2.77); 2) cognitive (M=4.29, SD=2.66); and 3) adaptive (M=4.55, SD=2.73).
As shown in Table 2, 78.5% of the children sampled received multiple EI services. ST was the most common core EI service and was accessed by 80.7% of children sampled. Median [IQR] per child total dosage (i.e., hours) of EI services was 10.76 [6.47, 18.58]. Median [IQR] per child intensity (hours per month) of EI services was 2.30 [1.70, 3.23].
Table 2.
Early intervention service use
| Characteristic | n (%) | |
|---|---|---|
| Type of EI Services Received | ||
| PT | 241 (24.0) | |
| OT | 191 (19.0) | |
| ST | 811 (80.7) | |
| DI | 450 (44.8) | |
| Number of EI Services Received | ||
| 1 | 216 (21.5) | |
| 2 | 313 (31.1) | |
| 3 or more | 476 (47.4) | |
| EI Service Use Intensity (hours per month) | ||
| < 2 | 171 (17.0) | |
| 2–3 | 430 (42.8) | |
| 3–4 | 192 (19.1) | |
| 4 or more | 212 (21.1) | |
| Mean (SD) | Median [IQR] | |
| EI Child Service Use, Conditional on Any Use | ||
| Total Per Child Hours of EI Services | 11.92 (6.47) | 10.76 [6.47, 18.58] |
| Total Per Child EI Service Intensity | 2.42 (1.02) | 2.30 [1.70, 3.23] |
| Length of EI Services (Days) | 149.50 (74.29) | 164.50 [151.00, 179.00] |
EI = early intervention; PT = physical therapy; OT = occupational therapy; ST = speech and language therapy; DI = developmental intervention
EI Service Intensity (Aim 1)
As compared to infants, 2-year-olds received more intensive EI (b=0.404 [0.178, 0.631]). Also, as compared to WNH children, children from an ethnicity categorized as other, non-Hispanic received more intensive EI (b=0.656 [0.180, 1.132]) (see Table 3). However, these results on ethnic differences in EI service intensity should be interpreted with caution, as children from an ethnicity categorized as other, non-Hispanic represent only 6.5% of the study sample.
Table 3.
Adjusted per child intensity of early intervention services
| Independent Variables | Total EI Service Intensity |
|---|---|
| Number of Delay Conditions | |
| 1 | ref |
| 2 | −0.459 [−1.184, 0.267] |
| 3 or more | −0.491 [−1.219, 0.238] |
| Child Age (months) | |
| < 12 | ref |
| 12–24 | 0.644 [−0.182, 1.469] |
| > 24 | 0.404***[0.178, 0.631] |
| Ethnicity | |
| White, non-Hispanic | ref |
| Black, non-Hispanic | −0.331 [−0.748, 0.086] |
| Hispanic | 0.706 [−0.534, 1.946] |
| Other, non-Hispanic | 0.656**[0.180, 1.132] |
| Primary Language, English | 0.565 [−0.932, 2.063] |
| Child’s Sex, Female | 0.489 [−0.487, 1.466] |
| Insurance Type, Medicaid and CHP+ | 0.485 [−0.285, 1.255] |
CHP+ = Child Health Plan Plus; EI = early intervention
p<0.001
p<0.01
p<0.05
Change in Activity Competence (Aim 2)
There were significant associations between EI service intensity and change in children’s activity competence (i.e., their functional capabilities) for two of the three domains assessed (see Table 4).
Table 4.
Change in children’s functional capabilities as a function of child and family characteristics and early intervention service use intensity
| Child Outcomes Summary (COS)
Domains | |||
|---|---|---|---|
| Independent Variables | Social-Emotional(1) | Cognitive(2) | Adaptive(3) |
| EI Service Intensity (hours per month) | |||
| < 2 | ref | ref | ref |
| 2–3 | 0.767**[0.226, 1.309] | 0.621* [0.077, 1.165] | 0.487 [−0.061, 1.036] |
| 3–4 | 0.653* [0.046, 1.260] | 0.694* [0.080, 1.308] | 0.425 [−0.193, 1.044] |
| 4 or more | 0.645* [0.022, 1.269] | 0.413 [−0.211, 1.037] | 0.261 [−0.368, 0.891] |
| Number of Delay Conditions | |||
| 1 | ref | ref | ref |
| 2 | 0.071 [−0.507, 0.648] | −0.051 [−0.596, 0.495] | −0.154 [−0.721, 0.414] |
| 3 or more | 0.448 [−0.052, 0.948] | −0.063 [−0.512, 0.386] | 0.057 [−0.448, 0.562] |
| Child Age (months) | |||
| <12 | ref | ref | ref |
| 12–24 | 0.590* [0.074, 1.106] | 1.175***[0.653, 1.697] | −0.221 [−0.736, 0.294] |
| > 24 | 0.847**[0.311, 1.382] | 1.383***[0.851, 1.914] | −0.242 [−0.780, 0.296] |
| Ethnicity | |||
| White, non-Hispanic | ref | ref | ref |
| Black, non-Hispanic | −0.020 [−0.675, 0.636] | −0.123 [−0.803, 0.558] | −0.207 [−0.872, 0.458] |
| Hispanic | −0.168 [−0.633, 0.297] | −0.423 [−0.877, 0.032] | −0.315 [−0.787, 0.158] |
| Other, non-Hispanic | 0.556 [−0.132, 1.244] | 0.373 [−0.371, 1.117] | 0.406 [−0.288, 1.100] |
| Primary Language, English | −0.124 [−0.628, 0.380] | 0.182 [−0.293, 0.656] | 0.014 [−0.498, 0.525] |
| Child Sex, Female | −0.121 [−0.496, 0.254] | −0.210 [−0.581, 0.160] | 0.197 [−0.171, 0.566] |
p<0.001
p<0.01
p<0.05
Difference in Positive Social-Emotional Skills (PSE) (Exit PSE Score - Entry PSE Score)
Difference in Acquiring and Using Knowledge and Skills (AUK) (Exit AUK Score - Entry AUK Score)
Difference in Taking Appropriate Action to Meet Needs (TAAM) (Exit TAAM Score - Entry TAAM Score)
Social-Emotional
Compared to children who received less than 2 hours of EI services per month, those who received 2–3 hours per month (b=0.767 [0.226, 1.309]), 3–4 hours per month (b=0.653 [0.046, 1.260]), and greater than 4 hours per month (b=0.645 [0.022, 1.269]) demonstrated greater gain in social-emotional capabilities by EI discharge. As compared to infants, 1-year-olds (b=0.590 [0.074, 1.106]) and 2-year-olds (b=0.847 [0.311, 1.382]) demonstrated greater gain in social-emotional capabilities by EI exit.
Cognitive
Compared to children who received less than 2 hours of EI services per month, those who received 2–3 hours per month (b=0.621 [0.077, 1.165]), or 3–4 hours per month (b=0.694 [0.080, 1.308]) demonstrated greater cognitive gains at EI discharge. Compared to infants, 1-year-olds (b=1.175 [0.653, 1.697]) and 2-year-olds (b=1.383 [0.851, 1.914]) demonstrated greater gain in cognitive capabilities by EI exit.
Adaptive
There were no differences in the amount of change in adaptive capabilities by EI service intensity or across predisposing and enabling child characteristics.
Discussion
This single-site study examined the relationship between EI service utilization and changes in children’s capabilities to perform functional tasks of everyday life. Study results partially support study hypotheses, mainly that child age at EI entry and EI service intensity were linked to gains in children’s capabilities. Results provide rationale and framework for conducting scale-up studies of EI effectiveness, with an eye toward improving rehabilitation care quality within EI.
Previous studies have reported on a range of EI service intensity from less than 2 hours per month15 to over 8 hours per month7. There are many factors that influence service intensity, including state variability in programming (e.g., primary service provider model implementation), sample or population, and individual child characteristics. The sample in this study was found to be on the lower end of the established range, receiving an average of 2.3 hours per month of EI services. This finding might be reflective of the transition to a primary service provider approach to EI service provision.28
Similar to previous research5,6,29, child age at EI entry was significantly correlated with EI service intensity, whereby 2-year-olds experienced a significantly higher intensity of EI services. One possible explanation for this finding is 2-year-olds are closer to transitioning out of EI, as children are no longer eligible to receive services through EI once they turn 3- years-old. As compared to infants, 2-year-olds may require a broader scope of service delivery. Thus, a child’s care team may recommend a higher intensity of service provision to enable the child to meet developmental milestones and family goals prior to transitioning out of EI services.
This study extends knowledge about the role of child age at EI entry and EI service intensity on functional outcomes. Prior studies have shown child age at EI entry is associated with social-emotional functioning 30, both cross-sectionally and from the parent perspective.31 Prior studies have also shown EI service use is associated with cognitive COS scores.7 However, this is the first study to show that children who are older and those receiving a higher intensity of EI services experience significant gains in their activity competence from EI entry to exit, for all but one domain assessed (i.e., adaptive). It is possible child age at EI entry and EI intensity were linked to social-emotional and cognitive gains because of the types of EI services received. ST was the most common EI service received, which typically emphasizes social communication and cognition as compared to adaptive behavior. Alternatively, these findings may be related to challenges of generating a valid COS score for adaptive capabilities. Relative to the other two COS domains, the adaptive domain contains fewer items and is broader in scope, including motor items such as mobility (e.g. crawling). The scope could result in greater discrepancy when generating a COS score by EI team consensus. In subsequent work using data collected prospectively, testing associations between COS scores and scores from the Pediatric Evaluation of Disability Inventory Computer Adaptive Test30 will help further validate COS scores, particularly within the adaptive domain.
It remains unclear if these findings on EI service use and outcomes will replicate in studies that capture EI service use quality. Rehabilitation services, particularly during early childhood, are commonly rendered in the child’s natural environment (e.g., home) and should be family-centered2,32 to foster gains in the child’s cognitive, social-emotional, and adaptive capabilities. However, in this study, we were limited to estimates of EI service intensity rather than EI service quality, such as the extent to which services are family-centered and thereby responsive to family priorities. Future studies could benefit from data drawn from valid measures of service quality, such as the Measure of Processes of Care (MPOC)32, which has been scaled for implementation across Ontario33, or the New York Impact on Child Scale34 and National Center for Special Education Accountability Monitoring Family Centered Services Scale35 that have been scaled for statewide implementation.4 The MPOC in particular was developed within pediatric rehabilitation and affords for both parent and provider perspectives of EI service quality.32 EI programs that do not administer service quality measures could alternatively leverage their programmatic data on collaboration time to capture EI service quality, since most children receive multiple EI services and need collaborative service provision.
Study Limitations
There are several study limitations related to sampling and timing of data collection. First, data were drawn from a large but single EI program; therefore, results warrant replication within and across states that vary in terms of EI eligibility and approaches to service delivery.21 Despite limits to generalizability, most states use COS to report on child outcomes nationally, so this study provides a scalable framework to further leverage these data for outcomes research to drive quality improvement at a more local level, such as regional or county level comparisons. Second, this study leveraged data on a subsample of children with COS data (~70% of the total sample). This is higher than prior studies7, but nevertheless is a subsample. We tested for differences between the subsample with and without complete COS scores, and found no significant differences on measured child characteristics (those shown in Table 1) between these groups. However, results could vary by unmeasured factors related to child outcomes, such as intensity of other non-EI services received, or level of family engagement during care planning when COS ratings are generated. Finally, data in this study were drawn prior to the implementation of GO4IT, a statewide quality improvement initiative to help providers to systematically synthesize multiple sources of assessment data to design and monitor function-focused care, which often includes generating COS scores to estimate a child’s functional status. Therefore, replication of this study in programs where GO4IT is being implemented may benefit from more precise COS estimates.
Conclusions
This study leveraged data on children discharged from a large, urban EI program with complete outcomes data, to estimate factors related to EI service use and gains in functional outcomes between service entry and exit. Child age at EI entry was significantly linked with EI service use intensity, and both child age at EI entry and EI service intensity were significantly linked to gains in the COS social-emotional and cognitive capabilities by EI discharge. The study framework can be used across EI programs to harmonize administrative data capture, conduct research on EI service use and outcomes, and apply results to improve EI care quality and value.
Acknowledgements
Research reported in this publication was supported by funding from the National Institutes of Health (1R03HD084909-01A1 and P2CHD065702) and the Comprehensive Opportunities in Rehabilitation Research Training program (K12 HD05593). We thank Vera Kaelin and Andrea Gurga from the Children’s Participation in Environment Research Lab for helping to interpret main results and provide critical feedback on earlier versions of this manuscript as well as assist with manuscript preparation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. We thank members of the High Value Early Intervention Research Group for their critical review of this manuscript.
List of abbreviations
- EI
early intervention
- COS
child outcomes summary
- OT
occupational therapy
- PT
physical therapy
- ST
speech therapy
- DI
developmental intervention
- WNH
white, non-Hispanic
- BNH
black, non-Hispanic
- ONH
Other, non-Hispanic
- IQR
inter-quartile ranges
- CI
confidence interval
- MPOC
Measure of Processes of Care
Footnotes
Conflict of Interest: The authors of this study have no conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.IDEA Infant and Toddlers Coordinators Association. Percentage of all children (including at risk) under three receiving services. 2008–2012 child count data. IDEA Infant & Toddler Coordinators Association website; http://ideainfanttoddler.org/association-reports.php. Updated 2018. Accessed January 31, 2019. [Google Scholar]
- 2.Bruder MB. Early childhood intervention: a promise to children and families for their future. Except Child. 2010;76(3):339–355. doi: 10.1177/001440291007600306. [DOI] [Google Scholar]
- 3.Whipple W Key principles of early intervention and effective practices: a crosswalk with statements from discipline specific literature. https://dese.mo.gov/sites/default/files/se-fs-first-steps-key-principles-crossalk-disciplines.pdf. Updated December 2014. Accessed January 31, 2019. [Google Scholar]
- 4.Bruder MB, Dunst CJ. Factors related to the scope of early intervention service coordinator practices. Infants Young Child. 2008;21(3):176–185. doi: 10.1097/01.IYC.0000324547.54693.18. [DOI] [Google Scholar]
- 5.Khetani MA, Richardson Z, McManus BM. Social disparities in early intervention service use and provider-reported outcomes. JDevBehavPediatr. 2017;38(7):501–509. doi: 10.1097/DBP.0000000000000474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McManus BM, Rapport MJ, Richardson Z, Lindrooth R. Therapy use for children with developmental conditions: analysis of Colorado Medicaid data. Pediatr Phys Ther. 2017;29(3):192–198. doi: 10.1097/PEP.0000000000000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noyes-Grosser DM, Elbaum B, Wu Y, et al. Early intervention outcomes for toddlers with autism spectrum disorder and their families. Infants Young Child. 2018;31(3): 177–199. doi: 10.1097/IYC.0000000000000121. [DOI] [Google Scholar]
- 8.The World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 9.Miller AR, Rosenbaum P. Perspectives on “disease” and “disability” in dhild health: the case of childhood neurodisability. Front Public Heal. 2016;4(226):1–13. doi: 10.3389/fpubh.2016.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imms C, Granlund M, Wilson PH, Steenbergen B, Rosenbaum PL, Gordon AM. Participation, both a means and an end: a conceptual analysis of processes and outcomes in childhood disability. Dev Med Child Neurol. 2017;59(1):16–25. doi: 10.1111/dmcn.13237. [DOI] [PubMed] [Google Scholar]
- 11.Msall ME, Rogers BT, Ripstein H, Lyon N, Wilczenski F. Measurements of functional outcomes in children with cerebral palsy. Ment Retard Dev Disabil Res Rev. 1997;3(2): 194–203. doi:. [DOI] [Google Scholar]
- 12.Di Marino E, Tremblay S, Khetani M, Anaby D. The effect of child, family and environmental factors on the participation of young children with disabilities. Disabil Health J. 2018;11(1):36–42. doi: 10.1016/j.dhjo.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Albrecht EC, Khetani MA. Environmental impact on young children’s participation in home-based activities. Dev Med Child Neurol. 2017;59(4):388–394. doi: 10.1111/dmcn.13360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khetani M, Graham JE, Alvord C. Community participation patterns among preschool-aged children who have received Part C early intervention services. Child Care Health Dev. 2013. doi: 10.1111/cch.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hebbeler K, Spiker D, Bailey D, et al. Early intervention for infants & toddlers with disabilities and their families: participants, services, and outcomes. Final report of the National Early Intervention Longitudinal Study (NEILS) https://www.sri.com/sites/default/files/publications/neils_finalreport_200702.pdf. Updated January 2007. Accessed January 31, 2019. [Google Scholar]
- 16.McManus BM, Richardson Z, Scully EA, Dooling-Litfin JK, Graham JE, Khetani MA. (2018). “Early Intervention Colorado (EI-CO) participant characteristics, service use, and outcomes, Colorado, 2014–2016”. Ann Arbor, Michigan: Inter-university consortium for political and social research; 10.3886/ICPSR37131.v1 [DOI] [Google Scholar]
- 17.COLO. CODE REGS. § 2509–10 12 (2015)
- 18.Imms C, Adair B, Keen D, Ullenhag A, Rosenbaum P, Granlund M. “Participation”: a systematic review of language, definitions, and constructs used in intervention research with children with disabilities. Dev Med Child Neurol. 2016;58(1):29–38. doi: 10.1111/dmcn.12932. [DOI] [PubMed] [Google Scholar]
- 19.Adair B, Ullenhag A, Rosenbaum P, Granlund M, Keen D, Imms C. Measures used to quantify participation in childhood disability and their alignment with the family of participation-related constructs: a systematic review. Dev Med Child Neurol. 2018. doi: 10.1111/dmcn.13959. [DOI] [PubMed] [Google Scholar]
- 20.Dunst CJ, Hamby D, Trivette CM, Raab M, Bruder MB. Young children’s participation in everyday family and community activity. Psychol Rep. 2002;91(3):875–897. doi: 10.2466/pr0.2002.91.3.875. [DOI] [PubMed] [Google Scholar]
- 21.Bruder MB. Service coordination and integration in a developmental systems approach to early intervention In: Guralnick MJ, ed. The developmental systems approach to early intervention. Baltimore, MD: Brookes; 2005:29–58. [Google Scholar]
- 22.Early Childhood Technical Assistance Center. Child outcome summary (COS) process. Early Childhood Technical Assistance Center website; http://ectacenter.org/eco/pages/cos.asp. Accessed January 31, 2019. [Google Scholar]
- 23.Twardzik E, Cotto-Negron C, MacDonald M. Factors related to early intervention Part C enrollment: a systematic review. DisabilHealth J. 2017;10(4):467–474. doi: 10.1016/j.dhjo.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Barfield WD, Clements KM, Lee KG, Kotelchuck M, Wilber N, Wise PH. Using linked data to assess patterns of early intervention (EI) referral among very low birth weight infants. Matern Child Health J. 2008;12(1):24–33. doi: 10.1007/s10995-007-0227-y. [DOI] [PubMed] [Google Scholar]
- 25.Feinberg E, Silverstein M, Donahue S, Bliss R. The impact of race on participation in Part C early intervention services. J Dev Behav Pediatr. 2011;32(4):284–291. doi: 10.1097/DBP.0b013e3182142fbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McManus BM, Robert S, Albanese A, Sadek-Badawi M, Palta M. Predictors of receiving therapy among very low birth weight 2-year olds eligible for Part C early intervention in Wisconsin. BioMed Cent Pediatr. 2013; 13(106): 1–9. doi: 10.1186/1471-2431-13-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9(3):208–220. doi: 10.1080/08912963.2016.1278444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kingsley K, Mailloux Z. Evidence for the effectiveness of different service delivery models in early intervention services. Am JOccup Ther. 2013;67(4):431–436. doi: 10.5014/ajot.2013.006171. [DOI] [PubMed] [Google Scholar]
- 29.Richardson Z, Khetani MA, Scully EA, Dooling-Litfin JK, McManus BM . Social and functional characteristics of receipt and service use intensity of core early intervention services. Acad Pediatr. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dumas HM, Fragala-Pinkham MA, Haley SM, et al. Computer adaptive test performance in children with and without disabilities: prospective field study of the PEDI-CAT. DisabilRehabil. 2012;34(5):393–401. doi: 10.3109/09638288.2011.607217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khetani MA, McManus BM, Arestad K, et al. Technology-based functional assessment in early intervention: a pilot study. BioMed Cent Pilot Feasibility Stud. 2018;4(65):1–9. doi: 10.1186/s40814-018-0260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cunningham BJ, Rosenbaum PL. Measure of processes of care: a review of 20 years of research. Dev Med Child Neurol. 2014;56(5):445–452. doi: 10.1111/dmcn.12347. [DOI] [PubMed] [Google Scholar]
- 33.Gorter JW, Rosenbaum PL, Teplicky R, Williams U. Giving parents a voice: a systematic program evaluation of familyDcentred service delivery. Paper presented at: European Academy of Childhood Disability Conference; May 17–20, 2017; Amsterdam, The Netherlands https://onlinelibrary.wiley.com/doi/full/10.1111/dmcn.13455. Accessed January 31, 2019. [Google Scholar]
- 34.Noyes-Grosser D, Elbaum B. Measuring the impact of early intervention services on children and families: a model approach to family-centered program evaluation and quality improvement. Paper presented at: Third Conference of the International Society on Early Intervention; May 2–5, 2011; New York, NY http://depts.washington.edu/isei/conf_materials/2011_ISEI_Conference_Program.pdf. Accessed January 31, 2019. [Google Scholar]
- 35.Fisher WPJ, Elbaum B, Coulter WA. Construction and validation of two parent-report scales for the evaluation of early intervention programs. JApplMeas. 2012; 13(1):57–76. [PubMed] [Google Scholar]