We read with interest an article on coronavirus disease 2019 (COVID-19) recently published in the journal by Sun et al. (1). In this letter, we would like to report a patient who showed a similar occurrence of pneumomediastinum with COVID-19 pneumonia, likely as a rare complication.
On February 5, 2020, a 36-year-old woman was admitted to the fever clinic of Union Hospital (Tongji Medical College, Wuhan, Hubei) due to a low-grade fever (37.3℃), cough, and bloody sputum that lasted for 12 days and chest tightness and shortness of breath that developed a day ago. Except for a history of mastitis, she had no history of other specific diseases such as hypertension, diabetes, or any heart diseases nor had any traumatic injuries. The patient exhibited a clear consciousness, with the blood pressure of 107/60 mm Hg, and a pulse rate of 60 beats/min. Her oxygen saturation was only 72%, even after applying an oxygen mask. An immediate noninvasive ventilator was applied with other symptom-directed treatments.
Laboratory studies showed leukopenia (white blood cell count 4050/µL) and lymphocytosis (lymphocyte cell count 1600/µL). The white blood cell differential count showed neutrophils (2300/µL, 50.2%), eosinophils (70/µL, 1.6%), lymphocytes (1400/µL, 32.4%), and monocytes (480/µL, 11.3%). There were elevated blood levels for C-reactive protein (23 mg/L; normal range, 0–10 mg/L), erythrocyte sedimentation rate (42 mg/L; normal range, < 20 mm/h), and D-dimer (5.77 mg/L; normal range, < 0.5 mg/L), IL-6 (4.58 pg/mL; normal range, 0.10–2.90 pg/mL), aspartate aminotransferase (198 U/L; normal range, 8–40 U/L), and alanine aminotransferase (259 U/L; normal range, 5–40 U/L).
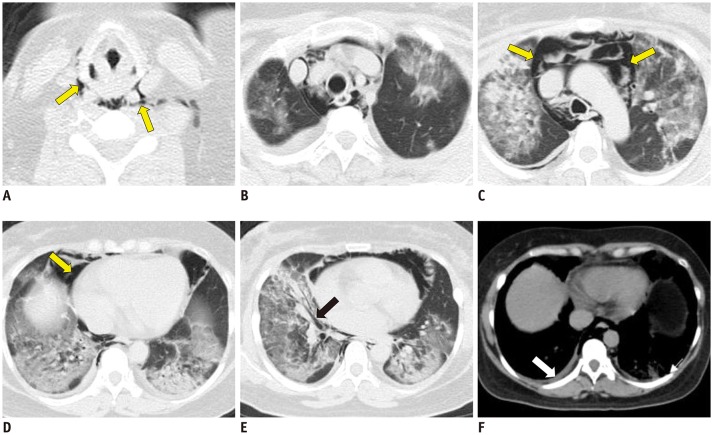
Chest CT showed multiple diffuse patchy consolidation areas and ground-glass opacities in both lungs (Fig. 1). There was interlobular septal thickening with pleural effusion and bronchiectasis. The adjacent pleura showed reactive thickening, without mediastinal lymphadenopathy. According to a scoring method published in the literature (2), the total lung severity score of the patient was 19 out of 20. Besides, we found pneumatosis extending from the mediastinal pericardium to the bilateral cervical soft tissue space (Fig. 1A–D). The patient was considered to have spontaneous pneumomediastinum because no other sources of mediastinal air could be identified. Spontaneous pneumomediastinum is uncommon in virus pneumonia. It was reported in cases with severe acute respiratory syndrome (SARS)-associated coronavirus pneumonia (3). Once it appears, the patient's condition could be serious with worse prognosis. Real-time fluorescence polymerase chain reaction of the patient's sputum was positive for the COVID-19 nucleic acid. Despite combined antiviral drugs, anti-inflammatory drugs, and supportive care, unfortunately, the patient succumbed to illness two days later due to respiratory failure and acute respiratory distress syndrome.
Fig. 1. Chest CT of 36-year-old woman with COVID-19 pneumonia obtained 12 days after onset of symptoms.
A–D. Pneumatosis extends from mediastinal pericardium to bilateral cervical soft tissue space (yellow arrows; A, C, D). B–E. Images show multifocal diffuse bilateral ground-glass opacities and consolidation with air bronchogram in middle lobe of right lung (black arrow; E). F. There are small pleural effusion and reactive thickening of pleura (white arrow).
References
- 1.Sun R, Liu H, Wang X. Mediastinal emphysema, giant bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020;21:541–544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsiao CH, Wu MZ, Hsieh SW, Chien LC, Hwang KC, Su IJ. Clinicopathology of severe acute respiratory syndrome: an autopsy case report. J Formos Med Assoc. 2004;103:787–792. [PubMed] [Google Scholar]