Abstract
Recently, some global cases of 2019 novel coronavirus (COVID-19) pneumonia have been caused by second- or third-generation transmission of the viral infection, resulting in no traceable epidemiological history. Owing to the complications of COVID-19 pneumonia, the first symptom and imaging features of patients can be very atypical and early diagnosis of COVID-19 infections remains a challenge. It would aid radiologists and clinicians to be aware of the early atypical symptom and imaging features of the disease and contribute to the prevention of infected patients being missed.
Keywords: COVID-19, Hemoptysis, Atypical symptoms, Atypical imaging features, 2019 novel coronavirus
INTRODUCTION
After the outbreak of the novel coronavirus in December of last year in China, the virus has spread widely in countries such as South Korea, Italy, and Iran. Increasing numbers of researchers fear that the virus will become a worldwide pandemic, which will cause fatal consequences. The most common signs and symptoms of the 2019 novel coronavirus (COVID-19; temporarily termed as 2019-nCoV) at onset are fever, a dry cough, shortness of breath, myalgia or fatigue, and dyspnea. Owing to the complexity of COVID-19, some patients may present with atypical manifestations such as hemoptysis or atypical CT findings, and this presents a substantial challenge for the control of the epidemic situation.
CASE REPORT
A 57-year-old man, without history of respiratory disease, presented to the emergency department with a 3-hour history of hemoptysis in Hunan, China. He denied recent travel to Wuhan City, Hubei Province, or any exposure to 2019-nCoV. No supportive results were found in laboratory tests upon admission. A unenhanced CT scan of the chest showed a localized area of ground-glass opacity (GGO) in the apicoposterior segment of the left upper lobe (Fig. 1). This patient was admitted to the hospital with a suspicion of pulmonary infection or tuberculosis. Three days after admission, a small amount of pleural effusion was seen. No affirmative results were found in the drainage of pleural effusion. Hemoptysis was unable to be controlled after symptomatic treatments including hemostasis and anti-infection therapy. Eight days later, a follow-up chest CT scan showed that the GGO in the left upper lobe had evolved into consolidation (Fig. 2). The GGO appeared on the superior segment of the left lower lobe. Bleeding was confirmed in the apicoposterior segment of the left upper lobe by using a fiber bronchoscope on the 10th day after admission. Fever occurred on the 11th day and the patient reached their highest body temperature of 39℃. Dyspnea was present on 14th day and gradually increased. On day 18 post admission, the GGOs and consolidation in the medial aspect of the left upper lobe decreased, while diffuse GGO and consolidation increased in the remaining areas of the lungs. The patient showed diffuse haziness in both lungs, batwing appearance, crazy-paving appearance, and the air-bronchogram sign. GGO was also distributed along the peripheral or subpleural regions (Fig. 3). The COVID-19 infection was eventually confirmed by a real time reverse-transcription-polymerase chain-reaction assay. The hemoptysis gradually decreased and the dyspnea was relieved with symptomatic treatment and antiviral therapy according to the Guidelines and Management for COVID-19. A chest CT scan showed that the consolidation in both lungs were obviously absorbed; the GGO region enlarged but the GGO density decreased on day 24 (Fig. 4A, B). On day 29 post admission, GGO and a small patch of consolidation continued to be absorbed. Initial GGO on the first CT scan and the initial GGO and consolidation on the second CT scan in the apicoposterior segment of the left upper lobe were obviously absorbed (Fig. 4C, D). This study was approved by the ethics board of Hunan province Hospital, and the informed consent for present study was waived.
Fig. 1. CT findings on day of admission.
A. Unenhanced chest CT showed area of localized GGO in apicoposterior segment of left upper lobe (yellow arrow). Distribution of lesions was mainly located in medial lung. B. No lesions were observed in other regions of lungs. GGO = ground-glass opacity
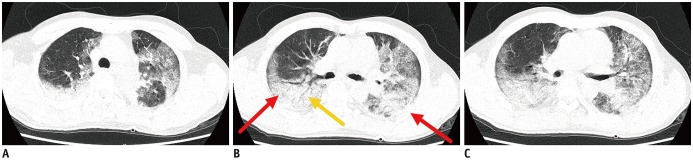
Fig. 2. CT findings on 8th day after admission.
A. Chest CT showed that GGO in left upper lobe had evolved into consolidation (yellow arrow). B. Newly presented GGO in superior lingual segment of left upper lobe and superior segment of left lower lobe were distributed along subpleural regions (yellow arrows).
Fig. 3. CT findings on 18th day after admission.
A–C. Initial GGOs and consolidation in medial aspect of left upper lobe zone decreased on 18th day, while diffuse GGO and consolidation increased in remaining areas of lungs with appearance of diffuse haziness in both lungs and batwing sign (red arrows). Crazy-paving and air-bronchogram sign (yellow arrow) were visible. Some GGO was also distributed along peripheral or subpleural regions.
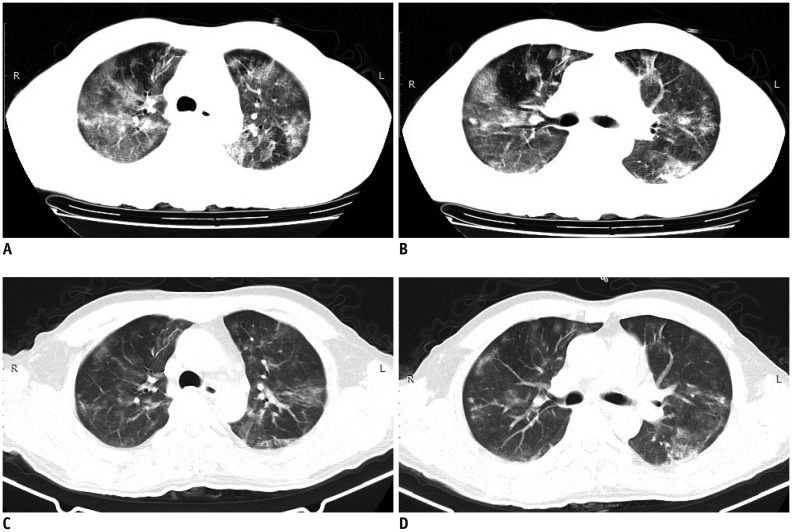
Fig. 4. CT findings on 24th and 29th day post-admission.
A, B. On day 24, consolidation was clearly absorbed. GGO regions were enlarged but GGO density had decreased. Some GGO was mixed with small patch consolidation. C, D. On day 29, GGO and small patch consolidation continued to absorb. Initial GGO on first CT scan and initial GGO and consolidation on second CT scan in apicoposterior segment of left upper lobe were clearly absorbed.
DISCUSSION
Early diagnosis of COVID-19 infections remains an enormous challenge (1,2). The most common signs and symptoms of COVID-19 infection at onset of illness have been reported to include fever, a dry cough, shortness of breath, myalgia or fatigue, and dyspnea (3,4,5). However, hemoptysis was the only clinical symptom in this patient during the first ten days of the disease course, combined with the slow progression of lung lesions. Hemoptysis has been rarely reported in patients with COVID-19 infections to date (3,6), and thus, it has not been included in the Guidelines and Management of COVID-19, constituted by the National Health Commission of China. Hence, it is difficult to diagnose COVID-19 infections especially without obvious epidemiological exposure. After the onset of fever and dyspnea, combined with typical CT findings, the patient was rapidly diagnosed with COVID-19 pneumonia by physicians. This case indicates the complexity of the pathogenesis of pneumonia caused by COVID-19 infection. Typical CT findings include GGO, mixed GGO, or crazy-paving patterns and consolidation of the peripheral or subpleural regions with bilateral lower lung involvements (7,8,9). An area of localized GGO in the apicoposterior segment of the left upper lobe of this patient was not a typical CT finding of COVID-19 pneumonia. It is a challenge to diagnose COVID-19 infections from GGO with a unilateral, isolated, or non-peripheral distribution with the only symptom of hemoptysis, but without epidemiological exposure. The first consideration was blood in the alveoli or an atypical manifestation of tuberculosis upon admission. The typical manifestations of the COVID-2019 pneumonia appeared on the 18th day after admission. The two final CT findings corresponded to the absorption stage, in which the clinical symptoms improved after adequate treatment according to the Guidelines and Management of COVID-19. Moreover, initial GGO on the first and second CT scans in the apicoposterior segment of the left upper lobe was clearly absorbed, which was consistent with the gradual improvement of hemoptysis.
In summary, the present case of COVID-19 pneumonia was likely caused by a second- or third-generation transmission of the viral infection, resulting in no traceable epidemiological history. Moreover, owing to the complexity of the COVID-19 pneumonia pathogenesis shown in this case, the initial symptom and imaging features of COVID-19 pneumonia could also be atypical. Importantly, COVID-19 pneumonia may present with atypical manifestations, such as hemoptysis and focal GGO with non-peripheral distribution, on initial CT scans.
Footnotes
This study was funded by the Novel Coronavirus Pneumonia Emergency Project of Hunan Provincial Science and Technology Department (2020SK3018).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.National Health Commission of the People's Republic of China. Diagnosis and treatment protocols of pneumonia caused by a novel coronavirus (trial version 3) [Accessed January 26, 2020]. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202001/f492c9153ea9437bb587ce2ffcbee1fa/files/39e7578d85964dbe81117736dd789d8f.pdf.
- 2.National Health Commission of the People's Republic of China. Diagnosis and treatment protocols of pneumonia caused by new coronavirus (trial version 5, revised edition) [Accessed February 10, 2020]. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202002/d4b895337e19445f8d728fcaf1e3e13a/files/ab6bec7f93e64e7f998d802991203cd6.pdf.
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 07; doi: 10.1001/jama.2020.1585. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 2020 Feb 04; doi: 10.1148/radiol.2020200241. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020 Feb 04; doi: 10.1148/radiol.2020200230. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 Feb 13; doi: 10.1148/radiol.2020200370. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]