Abstract
The 2019 novel coronavirus (2019-nCoV) outbreak in Wuhan, Hubei Province, China in 2019 led to large numbers of people being infected and developing atypical pneumonia (coronavirus disease 2019, COVID-19). Typical imaging manifestations of patients infected with 2019-nCoV has been reported, but we encountered an atypical radiological manifestation on baseline computed tomography (CT) images in three patients from Wuhan, China infected with the 2019-nCoV. Surprisingly, the only similar CT finding was a solitary sub-centimeter ground-glass nodule adjacent to bronchovascular bundles, which could be easily overlooked. In addition, the follow-up images in these patients showed how COVID-19 pneumonia evolved from these small nodules. The radiologic manifestation of the three cases will expand contemporary understanding of COVID-19.
Keywords: COVID-19; Solitary pulmonary nodule; Ground-glass; Pneumonia, viral; Tomography, X-ray computed
INTRODUCTION
A new dangerous coronavirus (2019 novel coronavirus, 2019-nCoV), leading to an outbreak of atypical pneumonia (coronavirus disease 2019, COVID-19), emerged in Wuhan, Hubei province, China at the end of December 2019 (1). As of March 3, 2020, more than 90000 people have been confirmed to have COVID-19 and more than 3000 people have died from the disease worldwide. Without any suitable therapeutic drugs, early detection and timely isolation are the best methods of preventing the disease from progressing and spreading. The role of high-resolution computed tomography (CT) has been crucial in the diagnosis of COVID-19 pneumonia and typical radiologic findings of COVID-19 pneumonia were included in the diagnostic criteria in China (2). Moreover, initial chest CT had a higher sensitivity than reverse transcription-polymerase chain reaction (RT-PCR) for 2019-nCoV (3). The typical CT findings of COVID-19 pneumonia include bilateral multiple ground-glass opacities and consolidative lesions in peripheral lung fields (4,5). However, we treated three patients with COVID-19 pneumonia initially manifesting as a solitary sub-centimeter nodule on baseline CT imaging in hospital. The purpose of the study is to share our experience of atypical manifestations of COVID-19 on CT with the aim of achieving a comprehensive radiological understanding of COVID-19.
CASE REPORT
Case 1
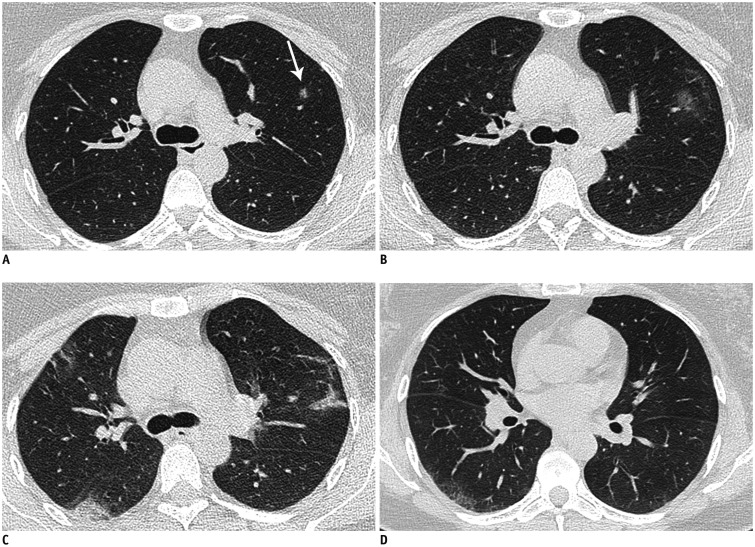
A 44-year-old woman was admitted to the hospital due to fever. She had a history of exposure to a patient with unexplained fever 3 days previously. The patient developed fever (37.8℃), accompanied by myalgia one day after contact with the patient. Initial laboratory investigation revealed the following: decreased leukocyte count (3.74 × 109/L), normal neutrophil ratio (46.2%), and increased monocyte ratio (21.9%). Chest CT images showed a small solitary ground-glass nodule on January 24 (Fig. 1A). Soon the patient's sputum tested positive for 2019-nCoV nucleic acid. On January 29, the nodule had enlarged with ground-glass opacities on follow-up CT images (Fig. 1B). The initial nodules showed absorption changes and the typical radiological manifestation of COVID-19 infection began to appear in the whole lung on February 1 (Fig. 1C). With the progression of infection, the patient showed abnormal results in laboratory investigations on February 8; the neutrophil ratio was increased (77.8%), the lymphocyte ratio was decreased (12.4%), the monocytes ratio was decreased (9.8%), and the lymphocyte count was decreased (0.68 × 109/L). After antiviral and symptomatic treatment, most of the lesions had been absorbed and some residues still existed in the peripheral lung on the latest follow-up CT images (Fig. 1D). She has since been cured, testing negative for viral nucleic acid.
Fig. 1. Chest CT images of 44-year-old woman with COVID-19 pneumonia.
Day 2, baseline CT image (A) shows solitary sub-centimeter ground-glass nodule 8 mm in size (arrow) in left upper lobe. Day 7 follow-up CT image (B) shows initial nodule enlarged with ground-glass opacities. Day 9 follow-up CT image (C) shows initial nodule presenting with absorption change and typical radiological manifestation of COVID-19 infection began to appear in whole lung. Day 27 latest follow-up CT image (D) shows most of lesions are absorbed and some residues still exist in peripheral lung. COVID-19 = coronavirus disease 2019
Case 2
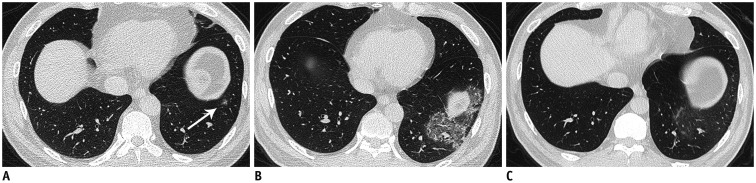
A 51-year-old man had a history of contact with a patient with confirmed COVID-19. He initially denied any clinical symptoms on January 23. Because of his history of exposure to a confirmed patient, he was asked to stay in isolation at home. However, on baseline chest CT images, a small ill-defined ground-glass nodule was suspected in his left lower lobe (Fig. 2A). On January 30, he began to have a fever (37.8℃) with chest pain and his C-reactive protein level was slightly increased (8.7 mg/L); therefore, he underwent a further chest CT scan. A confluent crazy-paving appearance presented in the same location as the nodule on chest CT images (Fig. 2B). Because of medical resource pressures from the COVID-19 outbreak, the patient was treated at home with antiviral agents. The latest follow-up chest CT images showed that the lesioned area had become smaller and the density had begun to decrease on February 13 (Fig. 2C). The patient remains under close observation although the clinical symptoms have disappeared.
Fig. 2. Chest CT images of 51-year-old man with COVID-19 pneumonia.
A. Baseline chest CT image (7 days before onset of symptoms) shows solitary ill-defined ground-glass nodule 7 mm in size (arrow) in left lower lobe. Day 2, patient presented with fever and chest pain day earlier; follow-up CT image (B) shows confluent crazy-paving pattern and consolidation opacities appear in same location. Day 15 follow-up CT image (C) shows area of lesion has become smaller and density has begun to decrease.
Case 3
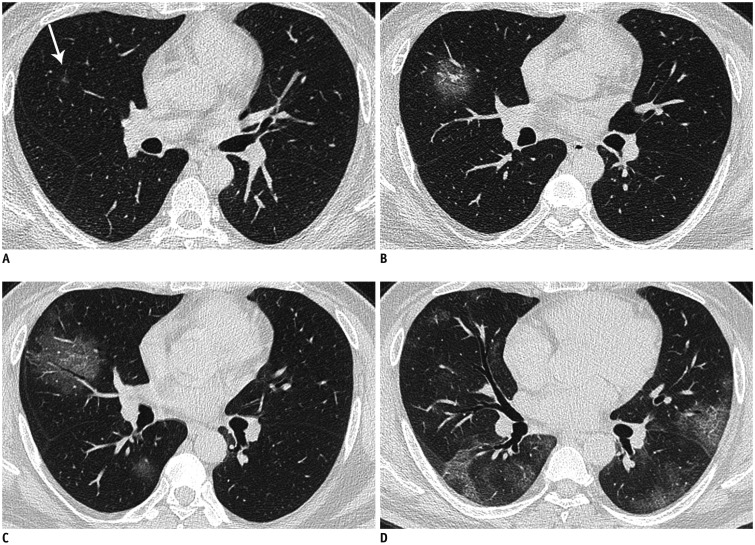
A 48-year-old man was admitted to hospital due to fever (38.3℃) and myalgia with a history of exposure to a patient with COVID-19 infection 6 days previously. Initial laboratory investigation revealed an increased C-reactive protein level (37.58 mg/L); all other indicators were normal. On baseline chest CT images, there was a sub-centimeter ground-glass nodule with an ill-defined margin in the right middle lobe during a period when the patient did not present with any symptoms (Fig. 3A). On subsequent chest CT images, the initial nodules had become larger. Grid-like vessels passing through the lesion were thickened and an air bronchogram appeared in the lesion (Fig. 3B). Ground-glass opacities began to appear in both lower lobes (Fig. 3C). On admission, his body temperature peaked (39.0℃). The RT-PCR of the patient's sputum tested positive for 2019-nCoV nucleic acid on February 17. The latest chest CT images showed diffuse parenchymal abnormalities in the periphery of the whole lungs (Fig. 3D).
Fig. 3. Chest CT images of 48-year-old man with COVID-19 pneumonia.
A. Baseline CT image (2 days before onset of symptoms) shows suspicious solitary sub-centimeter ground-glass nodule 5 mm in size (arrow) in right middle lobe. Day 2 follow-up CT image (B) shows that vessels passing through lesion are thickened and air bronchogram also appears in lesion. Day 4 follow-up CT image (C) shows area of lesion is further enlarged. Moreover, similar ground-glass opacities also appear around initial lesion and in right lower lobe. Day 27 follow-up CT image (D) shows diffuse parenchymal abnormalities in periphery of whole lungs.
DISCUSSION
In December 2019, 2019-nCoV broke out in Wuhan, China and the outbreak quickly spread across the country and abroad. According to Wu et al. (6), the basic reproduction number of COVID-19 was estimated to be 2.68 (95% confidence interval, 2.47–2.86), which means the 2019-nCoV has great transmission capacity. The aim of this study was to alert radiologists that some patients with COVID-19 infection could have only a sub-centimeter ground-glass nodule on baseline chest CT images. These patients will be prone to misdiagnosis in the clinic if the radiologists disregard the possibility of COVID-19 in the radiology report. In addition, we recorded the evolution of chest CT findings in COVID-19 pneumonia. RT-PCR analysis is the gold standard for diagnosing 2019-nCoV infection, but in the context of limited medical resources with an overwhelming outbreak, the role of chest CT is particularly important.
These three patients with COVID-19 had a similar feature on CT, a history of exposure to a suspected or confirmed patient with 2019-nCoV. All patients developed a fever in a short period after the exposure, but two patients presented with symptoms after the CT abnormalities were first seen. According to recent studies, abnormal CT findings can be found even in asymptomatic patients (7,8). All patients had abnormal laboratory investigation findings; one had a decreased lymphocyte count and the others had an increase in C-reactive protein, which both indicate viral infection. Some laboratory tests could provide clues suggestive of COVID-19, such as leukocytopenia, lymphopenia, and elevated C-reactive protein in the recent report (9).
We reviewed the serial CT images of patients with COVID-19. All patients recovered and we obtained all imaging data from onset to recovery. Based on the observations of previous studies (5,10,11), COVID-19 pneumonia is mainly characterized by multiple lesions that are preferentially distributed in the posterior or peripheral areas of both lungs. Furthermore, radiologic findings were associated with disease severity (8). In our study, the initial lesion was a solitary sub-centimeter ground-glass nodule distributed in the boundary between the outer one-third and inner two-thirds of pulmonary lobes, along with adjacent bronchovascular bundles (Figs. 1A, 2A, 3A). The small ground-glass nodule can easily be misdiagnosed as a benign nodule or early lung adenocarcinoma, or even not detected due to a lack of experience.
Furthermore, the reported imaging features in COVID-19 are variable and nonspecific (12). The radiological features of the patients as the disease progressed are shown below. The disease progressed over a period of 2–3 days, presenting as an enlarged nodule with a blurred margin on CT. Interestingly, the small ground-glass nodules were initially separate from the pleura; however, as the nodule evolved, the shape of the lesions became patchy to confluent and were predominantly found in subpleural areas. Multiple solid and ground-glass opacities always began to appear in the local lobe. Soon after, crazy-paving pattern, diffuse bilateral pulmonary ground-glass opacities with segmental consolidation appeared in the peripheral areas of the lung during the peak stage of the disease (approximately 10 days after onset of initial symptoms). The above imaging findings were associated with the death of a large number of epithelium and foam cells in the alveoli, inflammatory exudate filling the alveolar cavity, and pulmonary tissue necrosis (13). After the peak of COVID-19, the lesion was gradually absorbed and there was residual fibrosis in the original location.
In summary, we suspect that a solitary sub-centimeter nodule reflects an incipient stage of COVID-19 when it just begins to involve the lower respiratory tract. More remarkably, chest CT images can depict minute incipient lesions before the onset of symptoms. The Fleischner guideline is a commonly used guideline when a small ground-glass nodule is incidentally encountered on CT. The guideline recommends no routine follow-up or 6–12 months follow-up based on whether the nodule was 6 mm in size (14). In the endemic areas of COVID-19, such follow-up strategies may miss incipient COVID-19 pneumonia. Accordingly, short-interval follow-up CT scan is required, particularly for suspected cases with a history of exposure to 2019-nCoV, considering its rapid progression. A few patients lack symptoms in the early stages of infection but also exhibit positive CT findings according to Ai et al. (3). Moreover, we revealed the evolution of disease as seen on chest CT and these findings are nearly consistent with a recent report (10,11,15). Thus, chest CT is of great significance in the diagnosis of COVID-19 infection in areas where COVID-19 infection prevails. Accurate diagnosis requires an in-depth understanding of COVID-19 with a combination of the patient's symptoms, epidemic history, and other medical examination findings at the same time.
Acknowledgments
The authors would like to express appreciation for all of the people for their efforts to combat the COVID-19 outbreak.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diagnosis and treatment of nCoV pneumonia (trial version 6) National Health Commission of the People's Republic of China Web site. 2020. Feb 19, [Accessed February 19, 2020]. http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.shtml.
- 3.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 Feb 26; doi: 10.1148/radiol.2020200642. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W. CT manifestations of two cases of 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:208–209. doi: 10.1148/radiol.2020200280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020 Feb 13; doi: 10.1007/s00330-020-06731-x. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. [Google Scholar]
- 7.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020 Feb 24; doi: 10.1016/S1473-3099(20)30086-4. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from the front line. J Infect. 2020;80:373–377. doi: 10.1016/j.jinf.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295:202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 Feb 13; doi: 10.1148/radiol.2020200370. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. AJR Am J Roentgenol. 2020 Feb 28; doi: 10.2214/AJR.20.22969. [Epub] [DOI] [PubMed] [Google Scholar]
- 13.Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–739. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 14.MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017;284:228–243. doi: 10.1148/radiol.2017161659. [DOI] [PubMed] [Google Scholar]
- 15.Xu YH, Dong JH, An WM, Lv XY, Yin XP, Zhang JZ, et al. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect. 2020;80:394–400. doi: 10.1016/j.jinf.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]