Abstract
PURPOSE
The aim of this study was to investigate the shear bond strength of luting cements used with implant retained restorations on to titanium specimens after different surface treatments.
MATERIALS AND METHODS
One hundred twenty disc shaped specimens were used. They were divided into three groups considering the surface treatments (no treatment, sandblasting, and oxygen plasma treatment). Water contact angle of specimens were determined. The specimens were further divided into four subgroups (n=10) according to applied cement types: polycarboxylate cement (Adhesor Carbofine-AC), temporary zinc oxide free cement (Temporary Cement-ZOC), non eugenol provisional cement for implant retained prosthesis (Premier Implant Cement-PI), and non eugenol acrylic-urethane polymer based provisional cement for implant luting (Cem Implant Cement-CI). Shear bond strength values were evaluated. Two-way ANOVA test and Regression analysis were used to statistical analyze the results.
RESULTS
Overall shear bond strength values of luting cements defined in sandblasting groups were considerably higher than other surfaces (P<.05). The cements can be ranked as AC > CI > PI > ZOC according to shear bond strength values for all surface treatment groups (P<.05). Water contact angles of surface treatments (control, sandblasting, and plasma treatment group) were 76.17° ± 3.99, 110.45° ± 1.41, and 73.80° ± 4.79, respectively. Regression analysis revealed that correlation between the contact angle of different surfaces and shear bond strength was not strong (P>.05).
CONCLUSION
The retentive strength findings of all luting cements were higher in sandblasting and oxygen plasma groups than in control groups. Oxygen plasma treatment can improve the adhesion ability of titanium surfaces without any mechanical damage to titanium structure.
Keywords: Titanium, Plasma surface modification, Sandblasting, Contact angle, Dental implant
INTRODUCTION
Fixed implant-supported restorations provide widely accepted and predictable rehabilitation for individuals who are missing natural teeth.1 Prostheses and implants may be connected in one of two ways: cementation with a luting cement, or retention with a fastening screw. The type of connection used may vary depending upon the clinical situation, and the advantages and disadvantages of both methods have been well documented,2,3 with neither type of connection demonstrating clear superiority over the other.4 Studies have suggested that in comparison to screw retention, cement retention results in lower complication rates, better passive fit with multiple implants, greater fracture resistance of the ceramic structure, good aesthetic appearance without occlusal gaps, easier application, and lower costs.5,6 The bonding ability of a luting cement needs to be sufficiently strong to ensure retention of the prosthesis during functional movement as well as patient comfort.6 At the same time, the prosthesis may require removal for a number of reasons, including loosening of screws located below the prosthesis, abutment fracture, and peri-implant treatment requirements.7 Moreover, if recementation is required, residual cement on the bonding surfaces may contribute to bond failure.8
Zinc oxide-based, polycarboxylate, and glass-ionomer cements, while designed mainly for prostheses retained with natural teeth, may also be used as luting agents for implant supported prostheses.9 However, these cements were formulated with dental hard tissue in mind and may have adverse effects on titanium surfaces as well as peri-implant tissue. For instance, polycarboxylate cement can produce corrosion and trigger color changes in titanium alloys,10 and resin-modified glass ionomer cements can induce toxic activity, apoptosis, and inflammation of peri implant tissue11. Recently, special luting cements that are compatible with titanium have been introduced for use with implantsupported restorations.12 The bond strengths of these cements have been evaluated by several studies,4,9,13 the results of which suggest they be classified as semi-permanent cements, with bond strengths somewhere between those of zinc oxide-based and polycarboxylate cements. While there is no consensus regarding how an ideal balance between retention and retrievability of a prosthesis can be achieved through cementation,4 these new cements may be presumed to provide a more appropriate balance between prosthesis retention and retrievability.
In addition to the strength of the cement, retention is also affected by factors such as abutment length, tapering, and surface characteristics. Abutment surface properties and various surface modification methods have been investigated in a number of recent studies.9,14 According to one study, modification techniques that alter the surface energy of titanium may represent the greatest potential for improvement in prosthesis retention15 and secure an optimal balance between luting-cement bond strength and prosthesis retrievability. Methods such as sandblasting, airborne-particle abrasion, acid-etching, and the use of a diamond rotary to create circumferential grooves have all been reported to modify titanium surfaces and thus improve luting-cement bond strengths.11,16,17 For example, Al Hamad et al. found that sandblasting of abutment surfaces had a greater effect on luting-cement bond strength than increases in abutment length.18
Another new method that has been introduced to improve the surface energy of titanium is non-thermal plasma (NTP) treatment,9 which involves the application of various gases, such as oxygen plasma, under atmospheric pressure in order to increase titanium wettability.19,20 NTP has been shown to achieve changes in surface chemistry without any cytotoxic effects.19 Previous studies have investigated different NTP protocols,21,22 mainly in order to assess cell response and gain a better understanding of the effects of altered implant surfaces on osseointegration. However, there is limited knowledge about the effect of shear forces on the luting cement applied on the titanium surfaces altered by NTP treatment.
In view of this information, the present study intended to comparatively assess the shear bond strength and failure modes of two temporary implant luting cements and two conventional cements following two methods for modifying titanium surfaces - sandblasting and oxygen plasma treatment. The null hypotheses of the study were as follows: (1) the modification of titanium surfaces by either sandblasting or oxygen plasma treatment has no impact on the shear bond strength of luting cements; and (2) surface treatment has no effect on the failure modes of different luting cements.
MATERIALS AND METHODS
This study was conducted with 120 discs (6.6 mm dia. × 4 mm h.) produced from Grade-5 titanium (Ti-6Al-4V) (Bioinfinity Dental Implant, Pre-milled abutment, Istanbul, Turkey) and embedded in 20 mm dia. × 20 mm h. acrylic resin (Meliodent, Kulzer, Hanau, Germany). Bonding surfaces of the titanium specimens were polished with 600 SiC paper using an automatic polishing device under water.23,24 Specimens were then ultrasonically cleaned (Transsonic T700, Elma, Singen, Germany) for 10 minutes and dried by air. Specimens were separated equally into 3 groups considering applied surface pre-treatment (n = 40), as follows:
Group CNT: No treatment (control group)
Group SAB: Sandblasting with 50 µ Al2O3(S). Surfaces were sandblasted with 50 µ Al2O3 particles (Cobra, Renfert, Hilzingen, Germany) applied perpendicularly from a distance of 10 mm at 0.4 MPa for 10 seconds. Following sandblasting, the specimens were cleaned by ultrasonic machine with distilled water for 10 minutes and they were dried by air spray.
Group OPT: Oxygen plasma treatment. Non-thermal plasma (Plazmatek, Isparta, Turkey) was applied with oxygen pressure at 7 × 10−1 torr and a discharge current of 30 mA for 5 minutes21. (Ultrasonic cleaning was not performed so as not to disrupt the activated surfaces.)
Following the surface treatments, water contact angle analysis was performed (Kruss Drop Shape Analyzer, Hamburg, Germany) using 2 µL distilled water per specimen. Next, 1 representative sample per group was coated with 15-nm gold-alloy nano particles and examined at ×500 magnification under a scanning electron microscope (Vega, Tescan, Brno, Czech Republic). Then, energy-dispersive x-ray (EDX) (Vega, Tescan, Brno, Czech Republic) elemental analysis was performed.
After surface analysis was completed, considering the luting cement types applied, each group of specimens was also divided into four subgroups (n = 10), as follows: AC: polycarboxylate cement (Adhesor Carbofine, Pentron Clinical, Orange, CA, USA); ZOC: temporary zinc-oxidefree cement (Temporary Cement, Cavex, Haarlem, Netherlands); PI: non-eugenol provisional cement for implant-retained prosthesis (Premier Implant Cement, Premier Dental, Plymouth Meeting, PA, USA); and CI: noneugenol acrylic-urethane polymer-based provisional cement for implant luting (Cem Implant Cement, BJM Laboratories Silmet Ltd, Or-Yehuda, Israel) (Table 1).
Table 1. Cement used in the study (including manufacturers and lot numbers).
| Cement | Abbrevations | Cement type | Manufacturer | Lot No. |
|---|---|---|---|---|
| Adhesor Carbofine | AC | Zinc polycarboxylate cement for fixed partial prosthesis | Pentron | 5956753-2 |
| Zinc Oxide Free Cement | ZOC | Zinc oxide non-eugenol provisional cement | Cavex | 180604 |
| Premier Implant Cement | PI | Non-eugenol temporary cement for implant retained prosthesis | Premier Dental Products, Plymouth Meeting, PA | 4288CI |
| Cem Implant Cement | CI | Non-eugenol acrylic-urethane polymer based temporary cement for implant luting | BJM Laboratories Silmet Ltd, Or-Yehuda, Israel | 4296CITR |
Cements were prepared in accordance with the manufacturers' instructions using the cement's own syringe tips and/or auto-mixing or dispenser syringe tips. Specimens were clamped to an Ultradent bonding jig (Ultradent Product Inc., South Jordan, UT, USA). Luting cement was applied to the titanium surfaces using an Ultradent Teflon mold (Ultradent Product, Inc.) with an inner diameter of 2.3 mm and a height of 3 mm.25 After allowing the cement to set for 10 minutes, specimens were carefully dislodged from the acrylic molds and stored in a covered box containing distilled water until bond strength testing to prevent any stress to the cement material.23
A universal testing machine (Bisco Bond Tester, Bisco, Schamburg, IL, USA) was used to test shear bond strength. Specimens were placed in the specimen holder with the cement sample parallel to the loading piston, and a load with a cross-head speed of 0.5 mm/min was performed. Maximum load at failure was recorded in Newton (N) and the load at failure was divided by the bond area (mm2) to calculate shear-bond strength values in MPa. Failure types were identified with a stereomicroscope (M3B, Wild, Heerbrugg, Switzerland) and classified as either adhesive, cohesive, or mixed failure. In addition, a representative specimen per group was selected and examined under an SEM at × 500 magnification.
Statistical analysis was carried out using SPSS for Windows, Version 11.0 (SPSS Inc., Chicago, IL, USA) with the level of significance set at 0.05. Following normality testing (Shapiro-Wilk test: p = 0.122; P > .05), the influence of cement type and surface treatment method on shearbond strength was analyzed using Two-way ANOVA. Tukey's multiple comparison test was performed to figure out the interaction of cement and surface treatment among the groups. Regression analysis was performed to evaluate correlations between contact angle and shear bond strength values. Fisher's Exact test was used to analyze the distribution of failure modes (adhesive, cohesive, mixed) in the different surface-treatment groups.
RESULTS
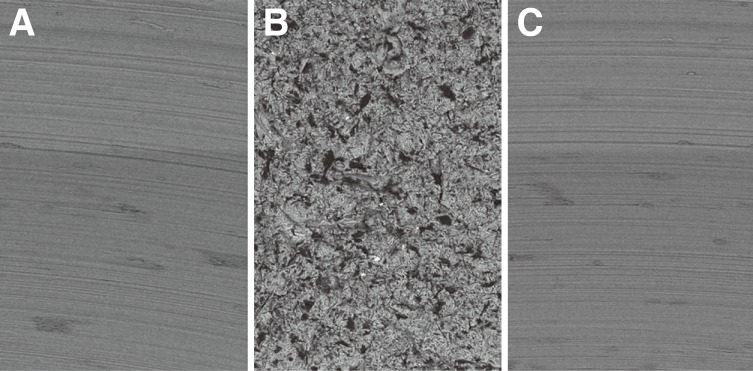
SEM analysis performed prior to cementation showed no changes in the morphological characteristics of the titanium surfaces in either the CNT or OPT group, whereas the specimen surface of the SAB group was visibly rougher than both the CNT and OP groups (Fig. 1). EDX analysis of elemental atomic concentrations (%) also showed variations among groups (Fig. 2), with higher levels of O2 and lower levels of carbon in the OPT group (O2: 10.6; Carbon: 6.81) and higher levels of both elements (O2: 29.48; Carbon: 10.32) in the SAB group as compared to the CNT group (O2: 0.11; Carbon: 7.82).
Fig. 1. SEM images of the titanium surfaces (Ti-6Al-4V) at ×500 magnification: Control (CNT) group (A), Sandblasting (SAB) group (B), and Oxygen plasma treatment (OPT) group (C).
Fig. 2. EDX analysis of titanium surfaces: Control (CNT) group (A), Sandblasting (SAB) group (B), Oxygen plasma treatment (OPT) group (C).
The results of two-way ANOVA indicated shear bond strength outcomes to be crucially affected by both cement type (P < .05) and surface treatment method (P < .05), as well as by the interaction between cement and surface treatment (P < .05) (Table 2). Mean shear bond strengths and standard deviations for all groups are presented in Table 3. For all surface treatment groups, the shear bond strength of the AC subgroup was notably higher (P < .05) and that of the ZOC subgroup was remarkably lower than the other cement subgroups (P < .05). Tukey test results indicated significant differences in the shear bond strength values of the cement types, with the highest shear bond strength observed in the AC subgroup, followed by the CI, PI, and ZOC subgroups for all surface-treatment groups (Table 3).
Table 2. The results of two-way ANOVA on the shear bond strength (MPa).
| Source | SS | df | MS | F | Sig. | P |
|---|---|---|---|---|---|---|
| Surface Treatment (ST) | 13.490 | 2 | 6.745 | 89.369 | 0.000 | .623 |
| Cement (Ce) | 139.447 | 3 | 46.482 | 615.851 | 0.000 | .945 |
| ST x Ce | 2.935 | 6 | 0.489 | 6.480 | 0.000 | .265 |
| Error | 8.151 | 108 | 0.075 | |||
| Total | 1086.545 | 120 |
SS: Sum of square, df: Degree of freedom,MS: Meansquare, ST x Ce: Effect of the interaction between surface treatment and cement material.
Table 3. Shear bond strength values (MPa); means and standard deviations (two-way ANOVA Test).
| Cement | CNT | SAB | OPT |
|---|---|---|---|
| AC | 3.48 ± 0.34aA | 4.90 ± 0.37bA | 4.52 ± 0.31cA |
| ZOC | 0.95 ± 0.19aB | 1.59 ± 0.22bB | 1.34 ± 0.17cB |
| PI | 2.15 ± 0.96aC | 2.78 ± 0.20bC | 2.52 ± 0.33cC |
| CI | 2.72 ± 0.17aD | 3.27 ± 0.31bD | 2.99 ± 0.30cD |
Uppercase letters indicate significant differences in values in the same column. Lower-case letters show significant differences in values in the same row.
Water contact angle testing of titanium surfaces is presented in Figure 3. Water contact angles (means + standard deviations) were as follows: Group CNT, 76.17° ± 3.99; Group SAB, 110.45° ± 1.41; Group OPT, 73.80° ± 4.79. Regression analysis revealed a weak negative correlation between shear bond strength and surface water contact angle (For CNT group %0 r = 0.00; p = 0.959 P > .05, for SAB group %0.04 r = 0.004; p = 0.711 P > .05, for OPT group %0.4 r = 0.047; p = 0.177 P > .05).
Fig. 3. Water contact shapes: Control (CNT) group (A), Sandblasting (SAB) group (B), Oxygen plasma treatment (OPT) group (C).
Adhesive, cohesive, and mixed failure types of the luting cements and different surface treatment methods were shown in Table 4. Also, SEM images of representative specimens are shown in Fig. 4. Failure mode distribution analyzed by Fisher's Exact test. In CNT group, higher adhesive failure rates were detected in the PI and CI cement subgroups than AC and ZOC subgroups (P < .05), whereas cohesive and mixed failure occurred at higher rates in the ZOC and AC subgroups as compared to the PI and CI subgroups (P < .05). In SAB group, mixed and cohesive failure modes were predominated, with adhesive failure rates higher in the PI and CI subgroups (P < .05) compared to the ZOC and AC subgroups and cohesive failure rates higher in the ZOC and AC subgroups compared to the PI and CI subgroups (P < .05). In OPT group, cohesive failure rates were significantly higher in the ZOC and AC subgroups compared to the PI and CI subgroups (P < .05).
Table 4. Distribution of failure modes per surface treatment group and luting cement.
| Luting cement | AC | ZOC | PI | CI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group\Failure mode | A | Co | M | A | Co | M | A | Co | M | A | Co | M | Total |
| CNT | 1 | 7 | 2 | 1 | 6 | 3 | 10 | 0 | 0 | 10 | 0 | 0 | 40 |
| SAB | 1 | 6 | 3 | 0 | 7 | 3 | 4 | 4 | 2 | 3 | 5 | 2 | 40 |
| OPT | 6 | 4 | 0 | 6 | 3 | 1 | 10 | 0 | 0 | 10 | 0 | 0 | 40 |
A: Adhesive, Co: Cohesive, M: Mixed
Fig. 4. SEM images of cements after shear bond testing (×500 magnification). (A) Mix failure for ZOC (sandblasting surface), (B) cohesive failure for AC (oxygen plasma surface), (C) cohesive failure for CI (sandblasting surface), (D) cohesive failure for PI (control group). T: Titanium Surface, L: Luting Cement.
DISCUSSION
The retention and retrievability of implant-supported prostheses can alter by the type of luting cement used and the surface properties of the abutments. This study examined and compared the shear bond strength values of four different luting cements to titanium surfaces treated using two different techniques as well as to untreated controls.
Bonding procedures used in the cementation of titanium discs were performed according to Seker et al.25 However, in contrast to their study, plasma treatment in this study was applied for 5 minutes, since previous studies have stated that the level of energy stabilizes after the initial energy bombardment that occurs during the first 5 minutes of application.21,26 Most plasma studies have evaluated surface changes using atomic force microscope and profilometer21,22; however, considering that these studies reported changes of less than 1 nm, this study evaluated water contact angle instead.
The first null hypothesis of the study that modification of titanium surfaces by surface treatments would have no impact on the shear bond strength of luting cements was not accepted. Sandblasting indicated significantly higher bond strength values than other groups in all the cement groups. Also, control group was shown to lower shear bond strength values than sandblasting and oxygen plasma treatment groups. Furthermore, the second null hypothesis that surface treatment would have no impact on failure modes of different luting cements to titanium was also rejected, as oxygen plasma treatment surfaces had higher rates of adhesive failure.
Although polycarboxylate cement and zinc oxide noneugenol provisional cement are widely used as permanent and temporary cements for tooth-supported prosthesis, respectively, these cements were designed to provide adhesion to tooth tissue via chelation, and the effects of these cements on titanium surfaces has not been thoroughly explored.27 Non-eugenol provisional cements can facilitate prosthesis retrievability, but their low tensile strength and high solubility make for poor retention.3 Moreover, the chemical composition and polymerization of cements can produce changes in the surface characteristics of titanium; for example, as Wadhwani and Chung have noted, polycarboxylate cements that contain stannous fluoride can caused pit-shaped corrosion of titanium surfaces.9 To avoid these problems, new types of luting cements have been introduced to the market specifically for use with implant-retained prostheses. These include the eugenol-free, resin-based Premier Implant (PI) cement, as well as a resilient, urethane oligomer-based cement, Cem Implant (CI). Based on previous studies, these cements can be classified as “semi-permanent cements,”3 whose tensile strengths fall somewhere between those of non-eugenol temporary cements and polycarboxylate cement and which have been shown to improve retention.4
The study found the shear bond strength of both CI and PI to be lower than AC and higher than ZOC. More soluble characteristic of conventional temporary cement than resin based temporary cements can be a reason for lower shear bond strength values for ZOC. Inversely, the highest shear bond strength values were found for AC and this result may be attributed to chemical chelation ability1 of the cement and a greater film thickness, which is stated as 25 µm by the manufacturer. Furthermore, the shear bond strength value of CI was found to be higher than that of PI. This may be attributed to the excellent mechanical properties of TiO2.28 According to manufacturer, CI cement contains TiO2, unlike PI. TiO2 may act as a filler between the particules of cement29 and enhance the shear bond strength of CI. Whereas the low bond strength of ZOC can be attributed to its greater solubility and minimal film thickness, the higher bond strengths of CI and PI as compared to ZOC can be attributed to the greater film thicknesses of resin-based cements.30,31 According to the manufacturers, ZOC has a film thickness of less than 10 µm, whereas the resin-based PI and CI cements have film thicknesses in the range of 10 – 15 µm.
Friction between the abutment surface and the inner surface of the prosthetic framework occurring under vertical forces may affect the bond strength of luting cement. In tensile bond strength studies, forces are implemented vertically to the luting cement between the abutment surface and the inner surface of the implant-retained prosthesis framework12; however, under clinical conditions, mastication forces are not always applied on a vertical axis.32 Unlike previous studies,3,33,34 this research examined the influence of shear forces on the bond strength of luting cements, a subject that has not been thoroughly explored.32 Interestingly, the shear bond strength results found in this research were lower than the tensile bond strengths reported in previous studies.6,9,13
Some previous studies1,6,34 have stated that the relatively high bond strengths of polycarboxylate cement to titanium are most likely due to the cement's chemical chelation of metallic ions from the titanium surface, while a previous study that recommended ZOC cement for luting implant-retained prostheses attributed to the chemical bond between ZOC cement and titanium to organic acids (ethoxy benzoic acid) contained in the cement formula.35 In line with this information, this study found higher rates of cohesive failure in the AC and ZOC cement groups, which may be attributed to the creation of a strong bond between titanium and cement by chemical chelation, whereas the higher rates of adhesive failure in the PI and CI cement groups may be due to the comparatively stronger molecular bonding occurring within these resin-based cements.
The surface properties of titanium may also play a role in the retention and failure patterns of luting cements. Previous studies have investigated various procedures such as sandblasting, circumferential roughening, and acid etching13,36,37 that can change the surface energy of titanium14. Another method that can alter the surface energy of titanium is oxygen plasma treatment, a non-invasive procedure in which an oxide layer is formed on the titanium surface without the creation of areas of micro-retention. By increasing the amount of O2 and decreasing the amount of C on the titanium surface, surface energy is increased.37 Oxygen plasma treatment can be performed under different atmospheric pressure conditions and with various types of electrically neutral ionized gas as well as using homogenous dielectric barrier discharge, and it has a wide range of applications from industry to medicine.25,38 Studies examining the effects of oxygen plasma treatment application to titanium material on cell movement and osseointegration21,22 have reported increases in surface concentrations of reactive species (O2) and hydrophilicity that optimized cell growth. However, few studies25,33 have looked at the effects of oxygen plasma treatment on bonding ability between titanium surfaces and luting cements. Moreover, comparing results among studies is difficult due to differences in materials, gas type, and amount and duration of applied pressure.
In the present study, oxygen-plasma treatment increased the bond strength between cement and titanium when compared to non-treated controls. In line with El-Helbawy et al.'s33 report of increases in increased O2 levels following oxygen-plasma treatment, the relatively higher bond strength achieved through oxygen plasma treatment found in the present study may be due to improvements in the chemical adhesion between titanium and cement achieved through higher levels of O2 on the cleaned titanium surfaces.39,40
Sandblasting was also found to improve bond strength values. Sandblasting of surfaces creates areas of micro-retention that can improve adhesion of luting cements through mechanical interlocking. This would also explain the higher rates of cohesive failure in the sandblasting group in the current study, which is in line with prior reports.13,27,33,39
In contrast to previous studies comparing bond strengths of untreated, sandblasted, and oxygen plasma treated surfaces,25,40 the present study found lower bond strength values for the OPT group than the SAB group. The differences in study findings may be due to differences in amounts of applied power, discharge voltage, and treatment duration.
The results of contact angle analysis showing a lower contact angle in the plasma-treated group in comparison to controls verified this study's findings regarding surface energy are in line with both Henningsen et al.22 and Matthes et al..41 However, due to confounding factors such as hydrophilicity, wettability and surface energy,42 it is not possible to identify a direct relationship between luting cement bond strength and water contact angle.
This study had a number of limitations that should be noted. First, only one type of titanium was used in the study. Second, only one oxygen plasma treatment protocol was examined. Future studies should be conducted with different oxygen plasma treatment protocols in order to gain a better understanding of how different plasma treatment parameters affect bonding performance of luting cements under clinical conditions.
CONCLUSION
Concerning the findings of this study, both sandblasting and oxygen plasma treatment of titanium surfaces may improve the bond strength of luting cements; however, as a non-invasive procedure, oxygen plasma treatment may be preferable to sandblasting, an invasive method that may have an adverse effect on the physical structure of titanium. Also, PI and CI cements are more easily removed from abutment surfaces than conventional cements designed for adhesion to natural teeth and may help avoid cementation failure caused by residual cement on abutment surfaces in clinical practice.
References
- 1.Worni A, Gholami H, Marchand L, Katsoulis J, Mericske-Stern R, Enkling N. Retrievability of implant-supported crowns when using three different cements: a controlled clinical trial. Int J Prosthodont. 2015;28:22–29. doi: 10.11607/ijp.4119. [DOI] [PubMed] [Google Scholar]
- 2.Vigolo P, Givani A, Majzoub Z, Cordioli G. Cemented versus screw-retained implant-supported single-tooth crowns: a 4-year prospective clinical study. Int J Oral Maxillofac Implants. 2004;19:260–265. [PubMed] [Google Scholar]
- 3.Mehl C, Harder S, Wolfart M, Kern M, Wolfart S. Retrievability of implant-retained crowns following cementation. Clin Oral Implants Res. 2008;19:1304–1311. doi: 10.1111/j.1600-0501.2008.01587.x. [DOI] [PubMed] [Google Scholar]
- 4.Gultekin P, Gultekin BA, Aydin M, Yalcin S. Cement selection for implant-supported crowns fabricated with different luting space settings. J Prosthodont. 2013;22:112–119. doi: 10.1111/j.1532-849X.2012.00912.x. [DOI] [PubMed] [Google Scholar]
- 5.Canullo L, Cocchetto R, Marinotti F, Oltra DP, Diago MP, Loi I. Clinical evaluation of an improved cementation technique for implant-supported restorations: a randomized controlled trial. Clin Oral Implants Res. 2016;27:1492–1499. doi: 10.1111/clr.12589. [DOI] [PubMed] [Google Scholar]
- 6.Garg P, Pujari M, Prithviraj DR, Khare S. Retentiveness of various luting agents used with implant-supported prosthesis: an in vitro study. J Oral Implantol. 2014;40:649–654. doi: 10.1563/AAID-JOI-D-12-00008. [DOI] [PubMed] [Google Scholar]
- 7.Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003;18:719–728. [PubMed] [Google Scholar]
- 8.Kim Y, Yamashita J, Shotwell JL, Chong KH, Wang HL. The comparison of provisional luting agents and abutment surface roughness on the retention of provisional implant-supported crowns. J Prosthet Dent. 2006;95:450–455. doi: 10.1016/j.prosdent.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Wadhwani C, Chung KH. Bond strength and interactions of machined titanium-based alloy with dental cements. J Prosthet Dent. 2015;114:660–665. doi: 10.1016/j.prosdent.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues DC, Valderrama P, Wilson TG, Palmer K, Thomas A, Sridhar S, Adapalli A, Burbano M, Wadhwani C. Titanium corrosion mechanisms in the oral environment: A retrieval study. Materials (Basel) 2013;6:5258–5274. doi: 10.3390/ma6115258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicholson JW, Czarnecka B. The biocompatibility of resinmodified glass-ionomer cements for dentistry. Dent Mater. 2008;24:1702–1708. doi: 10.1016/j.dental.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Nematollahi F, Beyabanaki E, Alikhasi M. Cement selection for cement-retained implant-supported prostheses: A literature review. J Prosthodont. 2016;25:599–606. doi: 10.1111/jopr.12361. [DOI] [PubMed] [Google Scholar]
- 13.Jugdev J, Borzabadi-Farahani A, Lynch E. The effect of air abrasion of metal implant abutments on the tensile bond strength of three luting agents used to cement implant superstructures: an in vitro study. Int J Oral Maxillofac Implants. 2014;29:784–790. doi: 10.11607/jomi.3167. [DOI] [PubMed] [Google Scholar]
- 14.Ajay R, Suma K, Ali SA, Kumar Sivakumar JS, Rakshagan V, Devaki V, Divya K. Effect of surface modifications on the retention of cement-retained implant crowns under fatigue loads: An in vitro study. J Pharm Bioallied Sci. 2017;9:S154–S160. doi: 10.4103/jpbs.JPBS_146_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elsaka SE. Effect of surface pretreatments on the bonding strength and durability of self-adhesive resin cements to machined titanium. J Prosthet Dent. 2013;109:113–120. doi: 10.1016/S0022-3913(13)60026-8. [DOI] [PubMed] [Google Scholar]
- 16.Cano-Batalla J, Soliva-Garriga J, Campillo-Funollet M, Munoz-Viveros CA, Giner-Tarrida L. Influence of abutment height and surface roughness on in vitro retention of three luting agents. Int J Oral Maxillofac Implants. 2012;27:36–41. [PubMed] [Google Scholar]
- 17.Lewinstein I, Block L, Lehr Z, Ormianer Z, Matalon S. An in vitro assessment of circumferential grooves on the retention of cement-retained implant-supported crowns. J Prosthet Dent. 2011;106:367–372. doi: 10.1016/S0022-3913(11)60149-2. [DOI] [PubMed] [Google Scholar]
- 18.Al Hamad KQ, Al Rashdan BA, Abu-Sitta EH. The effects of height and surface roughness of abutments and the type of cement on bond strength of cement-retained implant restorations. Clin Oral Implants Res. 2011;22:638–644. doi: 10.1111/j.1600-0501.2010.02011.x. [DOI] [PubMed] [Google Scholar]
- 19.Larsson Wexell C, Thomsen P, Aronsson BO, Tengvall P, Rodahl M, Lausmaa J, Kasemo B, Ericson LE. Bone response to surface-modified titanium implants: studies on the early tissue response to implants with different surface characteristics. Int J Biomater. 2013;2013:412482. doi: 10.1155/2013/412482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duske K, Koban I, Kindel E, Schröder K, Nebe B, Holtfreter B, Jablonowski L, Weltmann KD, Kocher T. Atmospheric plasma enhances wettability and cell spreading on dental implant metals. J Clin Periodontol. 2012;39:400–407. doi: 10.1111/j.1600-051X.2012.01853.x. [DOI] [PubMed] [Google Scholar]
- 21.Tseng WY, Hsu SH, Huang CH, Tu YC, Tseng SC, Chen HL, Chen MH, Su WF, Lin LD. Low pressure radio-frequency oxygen plasma induced oxidation of titanium--surface characteristics and biological effects. PLoS One. 2013;8:e84898. doi: 10.1371/journal.pone.0084898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Henningsen A, Smeets R, Hartjen P, Heinrich O, Heuberger R, Heiland M, Precht C, Cacaci C. Photofunctionalization and non-thermal plasma activation of titanium surfaces. Clin Oral Investig. 2018;22:1045–1054. doi: 10.1007/s00784-017-2186-z. [DOI] [PubMed] [Google Scholar]
- 23.Ozer F, Pak-Tunc E, Esen Dagli N, Ramachandran D, Sen D, Blatz MB. Shear bond strength of luting cements to fixed superstructure metal surfaces under various seating forces. J Adv Prosthodont. 2018;10:340–346. doi: 10.4047/jap.2018.10.5.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Özcan M, Matinlinna J. Surface conditioning protocol for the adhesion of resin-based cements to base and noble alloys: How to condition and why? J Adhes Dent. 2015;17:372–373. doi: 10.3290/j.jad.a34787. [DOI] [PubMed] [Google Scholar]
- 25.Seker E, Kilicarslan MA, Deniz ST, Mumcu E, Ozkan P. Effect of atmospheric plasma versus conventional surface treatments on the adhesion capability between self-adhesive resin cement and titanium surface. J Adv Prosthodont. 2015;7:249–256. doi: 10.4047/jap.2015.7.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vogelsang A, Ohl A, Steffen H, Foest R, Schröder K, Weltmann KD. Locally resolved analysis of polymer surface functionalization by an atmospheric pressure argon microplasma jet with air entrainment. Plasma Process Polym. 2010;7:16–24. [Google Scholar]
- 27.Wadhwani CP, Piñeyro AF. Implant cementation: clinical problems and solutions. Dent Today. 2012;31:56, 58, 60–62. quiz 63, 54. [PubMed] [Google Scholar]
- 28.Reddy AK, Kambalyal PB, Patil SR, Vankhre M, Khan MY, Kumar TR. Comparative evaluation and influence on shear bond strength of incorporating silver, zinc oxide, and titanium dioxide nanoparticles in orthodontic adhesive. J Orthod Sci. 2016;5:127–131. doi: 10.4103/2278-0203.192115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun J, Forster AM, Johnson PM, Eidelman N, Quinn G, Schumacher G, Zhang X, Wu WL. Improving performance of dental resins by adding titanium dioxide nanoparticles. Dent Mater. 2011;27:972–982. doi: 10.1016/j.dental.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 30.Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL. Tensile bond strengths of provisional luting agents used with an implant system. J Prosthet Dent. 1999;81:510–514. doi: 10.1016/s0022-3913(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 31.Gumus HO, Kurtulus IL, Kuru E. Evaluation and comparison of the film thicknesses of six temporary cements before and after thermal cycling. Niger J Clin Pract. 2018;21:1656–1661. doi: 10.4103/njcp.njcp_382_17. [DOI] [PubMed] [Google Scholar]
- 32.Naumova EA, Roth F, Geis B, Baulig C, Arnold WH, Piwowarczyk A. Influence of luting materials on the retention of cemented implant-supported crowns: An in vitro study. Materials (Basel) 2018;11:E1853. doi: 10.3390/ma11101853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Helbawy NG, El-Hatery AA, Ahmed MH. Comparison of Oxygen Plasma Treatment and Sandblasting of Titanium Implant-Abutment Surface on Bond Strength and Surface Topography. Int J Oral Maxillofac Implants. 2016;31:555–562. doi: 10.11607/jomi.4355. [DOI] [PubMed] [Google Scholar]
- 34.Mansour A, Ercoli C, Graser G, Tallents R, Moss M. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin Oral Implants Res. 2002;13:343–348. doi: 10.1034/j.1600-0501.2002.130401.x. [DOI] [PubMed] [Google Scholar]
- 35.Hagaman EW, Chen B, Jiao J, Parsons W. Solid-state 17O NMR study of benzoic acid adsorption on metal oxide surfaces. Solid State Nucl Magn Reson. 2012;41:60–67. doi: 10.1016/j.ssnmr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Michalakis K, Pissiotis AL, Kang K, Hirayama H, Garefis PD, Petridis H. The effect of thermal cycling and air abrasion on cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants. 2007;22:569–574. [PubMed] [Google Scholar]
- 37.Labriaga W, Song SY, Park JH, Ryu JJ, Lee JY, Shin SW. Effect of non-thermal plasma on the shear bond strength of resin cements to polyetherketoneketone (PEKK) J Adv Prosthodont. 2018;10:408–414. doi: 10.4047/jap.2018.10.6.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.do Prado M, da Silva EM, Marques JDN, Gonzalez CB, Simão RA. The effects of non-thermal plasma and conventional treatments on the bond strength of fiber posts to resin cement. Restor Dent Endod. 2017;42:125–133. doi: 10.5395/rde.2017.42.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al Jabbari YS, Zinelis S, Eliades G. Effect of sandblasting conditions on alumina retention in representative dental alloys. Dent Mater J. 2012;31:249–255. doi: 10.4012/dmj.2011-210. [DOI] [PubMed] [Google Scholar]
- 40.Lümkemann N, Eichberger M, Stawarczyk B. Different surface modifications combined with universal adhesives: the impact on the bonding properties of zirconia to composite resin cement. Clin Oral Investig. 2019;23:3941–3950. doi: 10.1007/s00784-019-02825-z. [DOI] [PubMed] [Google Scholar]
- 41.Matthes R, Jablonowski L, Holtfreter B, Gerling T, von Woedtke T, Kocher T. Fibroblast growth on zirconia ceramic and titanium disks after application with cold atmospheric pressure plasma devices or with antiseptics. Int J Oral Maxillofac Implants. 2019;34:809–818. doi: 10.11607/jomi.7285. [DOI] [PubMed] [Google Scholar]
- 42.Elias AB, Simão RA, Prado M, Cesar PF, Botelho Dos Santos G, Moreira da Silva E. Effect of different times of nonthermal argon plasma treatment on the microtensile bond strength of self-adhesive resin cement to yttria-stabilized tetragonal zirconia polycrystal ceramic. J Prosthet Dent. 2019;121:485–491. doi: 10.1016/j.prosdent.2018.03.025. [DOI] [PubMed] [Google Scholar]