Abstract
Rationale & Objective
Women with end stage kidney disease (ESKD) have decreased fertility and are at increased risk for pregnancy complications. This study examined secular trends and outcomes of obstetric deliveries in a US cohort of women with ESKD.
Study Design
Retrospective cohort study
Setting & Participants
Women aged 18–44 years with ESKD and registered in the United States Renal Data System (USRDS) from 2002 – 2015.
Exposure
ESKD modality (hemodialysis, peritoneal dialysis, transplant)
Outcomes
Infant delivery, pre-term delivery, cesarean delivery
Analytical Approach
Unadjusted delivery rates were expressed as the number of delivering women per 1000 patient-years among women 18–44 within each year over the study period, stratified by ESKD modality. Logistic regression models were used to evaluate associations of delivery, pre-term delivery, and cesarean delivery, with patient characteristics.
Results
The delivery rate in women undergoing HD and in women with a kidney transplant increased from 2.1 to 3.6 and 3.1 to 4.6 per 1000 patient-years, respectively (p<0.001 for each). The delivery rate in patients undergoing peritoneal dialysis was lower and did not increase significantly (p = 0.9). Women with a transplant were less likely to deliver preterm compared to women undergoing HD (OR, 0.92; 95% CI, 0.84–1.00), though more likely have a cesarean delivery (OR, 1.18; 95% CI, 1.06–1.31). For deliveries occurring in the 2012–2015 time period, 75% of women treated with HD were prescribed <=4 outpatient HD treatments per week and 25% were prescribed 5+ treatments per week in the 30 days prior to delivery.
Limitations
Ascertainment of outcomes and comorbidities using administrative claims data.
Conclusions
The delivery rate in women of reproductive age with ESKD increased from 2002 to 2015 amongst those treated with transplantation or hemodialysis. Women with a functioning transplant were less likely to deliver preterm, but more likely to have a cesarean delivery. Prescriptions for outpatient intensified hemodialysis for pregnant women with ESKD were infrequent in 2012–2015.
Keywords: end-stage kidney disease (ESKD), USRDS (US Renal Data System), pregnancy, obstetrics, delivery, preterm delivery, cesarean delivery, maternal outcomes, fetal morbidity, hemodialysis (HD), peritoneal dialysis (PD), transplantation, preeclampsia, childbirth, kidney failure, kidney replacement therapy, KRT modality
Introduction
Pregnancy in women with end stage kidney disease (ESKD) is a relatively rare and challenging clinical scenario. Women with ESKD have reduced fertility, owing in part to dysregulation of the hypothalamic-pituitary-gonadal axis and hyperprolactinemia resulting in anovulation1,2, as well as high rates of sexual dysfunction3–5. Women with ESKD whose treatment modality is dialysis also have a higher risk of maternal and fetal morbidities including blood transfusions6, severe hypertension, preeclampsia,7 and fetal demise8,9. Although kidney transplantation improves the biologic mechanisms of infertility in patients with ESKD10, transplant recipients still experience pregnancy complications including preeclampsia, cesarean delivery, and preterm delivery more frequently than the general population6,11,12.
Despite the challenges women with ESKD face conceiving, carrying, and delivering offspring, reports of successful pregnancies on hemodialysis (HD) are rising.13 The Australian and New Zealand Dialysis and Transplant Registry (ANZDATA) showed an increasing rate of pregnancy for women on dialysis from 1976–2008, from 0.67 pregnancies per 1000 person-years in 1986–1995 to 3.3 per 1000 person-years in 1996–200814 There is limited information on a national level in the US about childbirth in women with ESKD, particularly amongst those treated with dialysis.
The objectives of this study were to describe secular trends in obstetric deliveries amongst US women with ESKD and investigate the associations of treatment modality (HD, peritoneal dialysis, and transplant) and other clinical characteristics with delivery outcomes including preterm delivery and cesarean delivery. We hypothesized that shorter kidney replacement therapy (KRT) vintage (time since ESKD designation) would be associated with higher likelihood of delivery. Furthermore, in a subset of delivering women receiving HD from 2012–2015, we sought to use dialysis clinical data available from Consolidated Renal Operations in a Web-enabled Network (CROWNWeb) to examine the association between preterm delivery and intensity of HD prescribed. We hypothesized that fewer hours of dialysis weekly and higher pre-HD SUN would be associated with higher likelihood of preterm delivery.
Methods
Study population
We performed a retrospective cohort study of all female ESKD patients age 18–44 years between January 1, 2002 and September 30, 2015 using data from the US Renal Data System (USRDS). The USRDS is the national registry of persons undergoing maintenance dialysis or having received a kidney transplant. We restricted analyses to persons with Medicare as their primary payer to facilitate complete capture of administrative claims data. Multiple observations were included for each woman, one for each year observed in USRDS over the study period. For each year in the study period, prevalent women with ESKD were followed for the proportion of time in that year they had data available (for example, if a woman was declared to have ESKD on July 1, 2008 and died on June 30, 2010 she was ascribed 0.5 years of follow up in 2008, 1 year of follow up in 2009, and 0.5 years of follow up in 2010). For women delivering between 2012–2015, additional clinical data elements were available monthly from CROWNWeb, a web-based data-collection system that was implemented across all Medicare-certified dialysis facilities from May 2012 onward15. This study was performed under the USRDS Coordinating Center contract with the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); research as part of the contract was approved by the University of Michigan Institutional Review Board (HUM00086162). Because data for the USRDS components are collected by federal mandate, there are no individual patient consent requirements.
Outcome Ascertainment
Obstetric delivery was the primary outcome of interest as identified by International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes from previously described, validated methods (Table S1)16 Given the comorbidity burden in the ESKD population, we assumed that few deliveries would occur outside of a hospitalization (e.g., at home). Because first trimester pregnancy losses are common17, may not require medical attention, and thus may be incompletely captured by inpatient or outpatient claims, conception or pregnancy were not used as outcomes of interest. Secondary outcomes included preterm delivery and cesarean delivery. Preterm delivery at less than 37 weeks was identified by ICD-9-CM code 644.21. Cesarean delivery was identified by ICD-9-CM codes 740.x, 741.x, 742.x, 744.x, 749.9. All ICD-9-CM codes were derived from Medicare inpatient claims.
Exposures of interest
Treatment modality (HD, peritoneal dialysis, or transplant) and KRT vintage (time since ESKD declaration) at time of each delivery was determined from USRDS treatment history files. Modality assignment for non-delivering women was updated each year, as necessary, and defined as last modality reported for every year in which they were available from 2002 to 2015.
Covariates
Patient demographic characteristics, including age, race, ethnicity, assigned ‘primary cause’ of kidney failure and date of ESKD onset, were obtained from the Centers for Medicare & Medicaid Services (CMS) End Stage Renal Disease Medical Evidence Report (Form CMS-2728-U3)18 recorded at time of ESKD registration. Age and vintage for each woman were updated each year based on time since 2728 filing. For delivering women, age and vintage (years since ESKD onset) in the year of each delivery was also calculated. Comorbid conditions, such as diabetes mellitus, hypertension, heart failure, cardiovascular disease, cerebrovascular disease, peripheral vascular disease, chronic obstructive pulmonary disease, and cancer, were ascertained from institutional or physician/supplier claims. To establish presence of a comorbidity, either one inpatient claim or two outpatient claims over the entire study period were required.
Statistical Analyses
We described characteristics among all women 18–44 by modality (HD, peritoneal dialysis, transplant, unknown) and delivery status (delivered vs. not delivered), using mean and standard deviation or median and interquartile range for continuous variables and count and percent for categorical variables. To simplify these characteristics, rather than report descriptive values per woman per year in the data set, age, vintage, and comorbidities were averaged within each woman, using values only at delivery for delivering women. P-values were calculated from t-test for continuous variables and chi-squared test for categorical variables, with 3 degrees of freedom for race and 8 degrees of freedom for primary cause of ESKD. Unadjusted delivery rates were expressed as number of delivering women per 1000 patient-years among women 18–44 within each year over the study period, stratified by modality. As a sensitivity analysis, proportions were estimated and little difference was seen between the two measures.
Association between modality and delivery outcomes
Logistic regression models were used to evaluate associations between patient characteristics and delivery, pre-term delivery, and cesarean delivery. Due to the repeated measures nature of the data (one observation per woman per year with ESKD), we employed generalized estimating equations using an unstructured working correlation matrix, to account for multiple observations for individuals. The final multivariable logistic regression model included modality, age, race, vintage, cause of kidney failure, calendar year and comorbidities. Models assessing delivery were examined among the full sample of women aged 18–44 years, while models assessing pre-term delivery and cesarean section were examined only among women with deliveries.
Association between HD prescription and delivery outcomes
A subgroup analysis was performed using women who delivered between 2012 and 2015 and had available data in CROWNWeb. There were no women with repeated deliveries in this subgroup analysis. Amongst delivering women treated with HD between 2012 and 2015 with complete records at 30 days prior to delivery (n=132) and for 9 consecutive months prior to delivery in CROWNWeb (n=48) descriptive statistics were used to summarize HD treatment variables, including number of sessions per week, prescribed and delivered HD time, Kt/V, ultrafiltration rate (UFR), and pre-HD serum urea nitrogen (SUN), using mean and standard deviation or median and interquartile range for continuous variables and count and percent for categorical variables. Logistic regression models were used to evaluate the association of preterm delivery and cesarean delivery with prescribed minutes of HD and pre-HD SUN 30 days prior to delivery. Covariates were limited to baseline demographics, vintage, and kidney failure cause given the smaller sample size. The final multivariable logistic regression model included minutes of HD, pre-HD SUN, age, race, vintage, cause of kidney failure. Thirty days prior to delivery was chosen as the representative time period because date of conception and exact gestational age at delivery are not able to be determined from USRDS. Time points 25–40 weeks prior to delivery may capture pre-conception HD prescriptions (if women delivered preterm) or HD prescriptions prior to a pregnancy being known to the patient and her nephrologist.
All analyses were conducted using SAS, version 9.4 (SAS Institute Inc., Cary NC). Due to the large sample size in the primary analysis, statistical significance level was defined as p=0.005.
Results
Study Population
Among 121,581 Medicare-insured women aged 18–44 with ESKD between January 1, 2002 and September 30, 2015, there were 1807 deliveries were identified in 1607 women. Patient characteristics by modality and delivery status are described in Table 1. The group of delivering women receiving home HD was too small to report separately (<10 women per year). Amongst all women 18–44 with ESKD from 2002–2015, the majority were non-Hispanic white. Glomerulonephritis was listed as the most common cause for ESKD in this population regardless of delivery status. Delivering women were of shorter KRT vintage across all modalities. The average age at delivery rose over the study period from 29.1 years in 2002 to 31.9 years in 2015. Amongst the women who delivered in the study period, the average age at ESKD incidence was 24.5 years, whereas amongst non-delivering women, the average age at incidence was 32.3 years (p <0.001). Of delivering women, 81.8% were treated with hemodialysis as their first modality, 12% were treated with peritoneal dialysis as their first modality, 5.9% were transplanted first, and in the remaining 0.3% first modality was unknown. At the time of delivery, 41% of women were being treated with hemodialysis, 2.8% peritoneal dialysis, 42.8% transplant, and in 13% modality was unknown.
Table 1.
Patient characteristics among women with ESKD of childbearing age, by delivery status and modality of kidney replacement therapy, 2002–2015
| Hemodialysis | Peritoneal Dialysis | Transplant | Unknown1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No Delivery (n= 11,718) | 1+ Delivery (n= 664) | p-value2 | No Delivery (n= 3,225) | 1+ Delivery (n= 47) | p-value2 | No Delivery (n= 25,446) | 1+ Delivery (n= 670) | p-value2 | No Delivery (n= 79585) | 1+ Delivery (n=226) | p-value2 | |
| Age, y | 37.5 | 30.6 | <0.001 | 36.1 | 30.1 | <0.001 | 35.5 | 30.5 | <0.001 | 36.4 | 29.9 | <0.001 |
| Race (%) | <0.0013 | 0.033 | <0.0013 | <0.0013 | ||||||||
| White | 46.8% | 38.6% | 59.4% | 40% | 76.6% | 71.2% | 53.0% | 38.3% | ||||
| Black | 46.1% | 52.6% | 30.8% | 48% | 13.5% | 20.5% | 39.0% | 54.2% | ||||
| Asian | 3.2% | 3.1% | 6.4% | 10% | 4.5% | 4.9% | 3.1% | 1.9% | ||||
| Other | 3.8% | 5.7% | 3.5% | 2% | 5.4% | 3.4% | 4.7% | 5.6% | ||||
| Hispanic | 15.6% | 24.5% | <0.001 | 17.0% | 28% | 0.06 | 16.6% | 27.2% | <0.001 | 17.9% | 17.0% | 0.7 |
| KRT Vintage (y) | 7.1 | 4.4 | <0.001 | 2.5 | 7 | <0.001 | 9.6 | 8.2 | <0.001 | 1.7 | 1.9 | .2 |
| Cause of kidney failure (%) | <0.0014 | <0.0014 | <0.0014 | <0.0014 | ||||||||
| DM | 30.0% | 12.5% | 24.4% | 6% | 18.9% | 9.6% | 31.1% | 15.4% | ||||
| HTN | 19.8% | 22.9% | 15.2% | 17% | 6.9% | 7.5% | 17.5% | 16.8% | ||||
| GN | 30.1% | 47.1% | 39.6% | 52% | 37.1% | 55.1% | 21.5% | 39.3% | ||||
| Cystic Kidney | 2.6% | 2.2% | 4.5% | 0% | 5.7% | 4.0% | 3.2% | 2.3% | ||||
| Other Urologic | 2.1% | 1.9% | 2.5% | 0% | 4.0% | 4.7% | 1.2% | 0.9% | ||||
| Other | 10.3% | 6.7% | 9.4% | 10% | 16.0% | 13.2% | 16.4% | 19.6% | ||||
| Unknown | 3.9% | 5.7% | 4% | 15% | 6.0% | 5.0% | 4.7% | 4.2% | ||||
| Missing | 0.5% | 1.0% | 0.5% | 0% | 5.5% | 0.9% | 4.1% | 1.4% | ||||
| Comorbidities | ||||||||||||
| ASHD | 23.0% | 16.3% | <0.001 | 21.9% | 11% | 0.02 | 8.0% | 4.6% | <0.001 | 13.0% | 15.0% | .4 |
| CHF | 31.3% | 32.7% | 0.4 | 38.9% | 22% | 0.2 | 8.4% | 8.7% | 0.8 | 18.0% | 25.2% | 0.01 |
| CVA | 13.6% | 8.6% | <0.001 | 13.2% | 6% | 0.06 | 4.2% | 3.1% | 0.08 | 7.8% | 8.5% | .7 |
| PVD | 33.4% | 30.8% | .2 | 29.3% | 21% | 0.09 | 11.6% | 11.8% | 0.8 | 18.8% | 18.0% | .8 |
| Other CVD | 40.4% | 50.5% | <0.001 | 40.0% | 45% | 0.5 | 14.9% | 21.7% | <0.001 | 22.7% | 35.6% | <0.001 |
| Anemia | 73.7% | 96.5% | <0.001 | 79.5% | 96% | <0.001 | 33.6% | 68.3% | <0.001 | 51.4% | 79.8% | <0.001 |
Data is presented by woman across all years of the study period.
Unknown refers to “uncertain dialysis” or “missing” modality.
p-values from chi-squared test for categorical variables and t-test for continuous variables.
p-value for race (degrees of freedom = 3).
p-value for cause (degrees of freedom = 8).
GN: Glomerulonephritis. ASHD: Atherosclerotic heart disease. CHF: Congestive heart failure. CVA: Cerebrovascular accident. PVD: Peripheral vascular disease. CVD: Cardiovascular disease; KRT, kidney replacement therapy; HTN, hypertension; DM, diabetes mellitus.
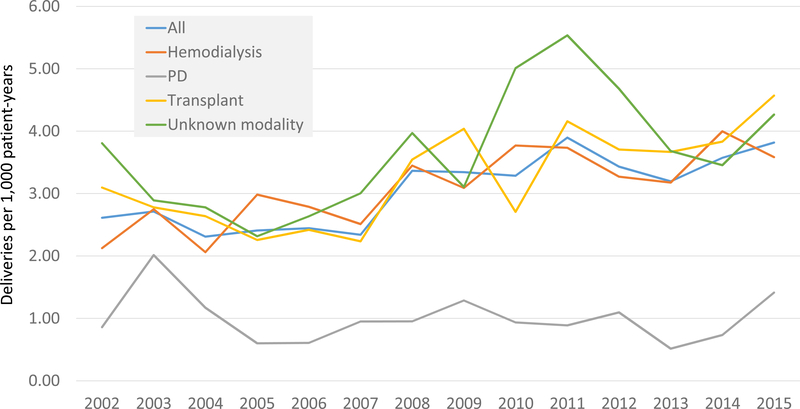
Delivery rates
The unadjusted delivery rate amongst all women 18–44 with ESKD increased from 2.6 to 3.8 per 1000 patient-years from 2002 to 2015 (p < 0.001) (Figure 1). The delivery rate in patients undergoing HD increased from 2.1 to 3.6 per 1000 patient-years (p < 0.001). The delivery rate in patients with a functioning kidney transplant increased from 3.1 to 4.6 per 1000 patient-years (p < 0.001). The delivery rate in patients undergoing peritoneal dialysis did not increase significantly (p = 0.9), ranging 0.5–1.4 deliveries per 1000 patient-years over the study period, and was lower than those receiving HD or a kidney transplant.
Figure 1. Deliveries per 1,000 patient-years in women age 18–44 with ESKD.
Unadjusted delivery rates per 1000 patient-years among women 18–44 within each year over the study period, stratified by modality.
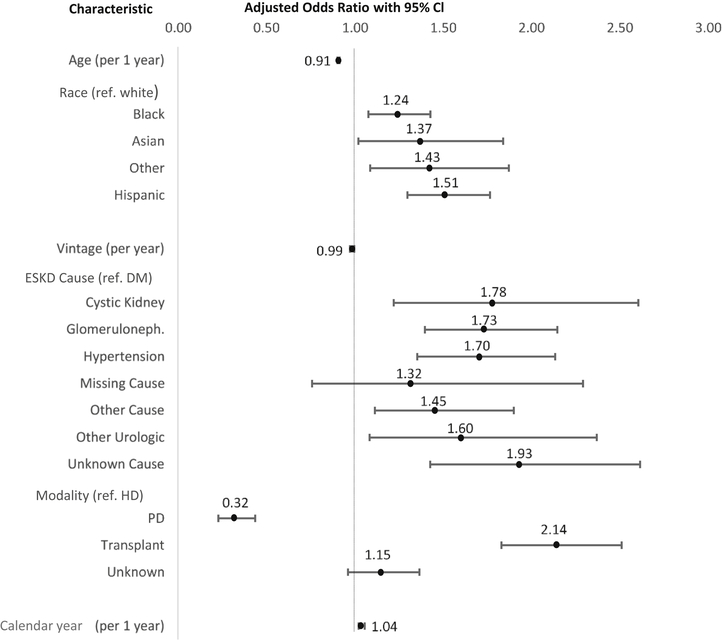
Association of modality and vintage with delivery
Women with a functioning kidney transplant had higher odds of delivery compared to women undergoing HD (OR, 2.14; 95% CI, 1.83–2.51) and those undergoing peritoneal dialysis had a lower odds of delivery (OR, 0.32; 95% CI, 0.23–0.44) (Figure 2). For each additional year after ESKD diagnosis, the odds of delivery were lower by 1% (OR, 0.99; 95% CI, 0.97–1.00). Older age was also associated with lower odds of delivery (OR for each additional year, 0.91; 95% CI, 0.90–0.91). Black and Hispanic women (compared to White) were more likely to deliver (ORs of 1.24 [95% CI, 1.08–1.44 and 1.52 [95% CI, 1.30–1.77], respectively), as were women whose primary cause of kidney failure was glomerulonephritis (OR, 1.73; 95% CI, 1.40–2.15) or hypertension (OR, 1.7; 95% CI, 1.35–2.13), when compared to diabetes.
Figure 2. Relationships between clinical characteristics and odds of delivery.
Forest plot showing multivariable association between clinical characteristics and odds of delivery (with 95% confidence intervals) using logistic generalized estimating equations accounting for multiple deliveries in a single individual and adjusted for comorbidities.
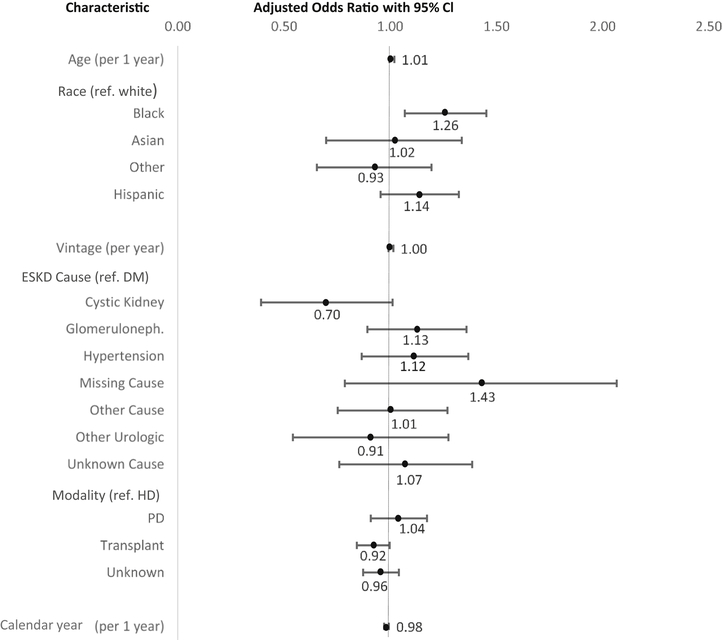
Association of modality with preterm delivery and cesarean delivery
Amongst delivering women with ESKD from 2002–2015, preterm delivery was observed in 41%, 41%, and 33% of HD, peritoneal dialysis (PD), and functioning kidney transplant patients, respectively. The overall odds of preterm delivery over the study period decreased by 2% per year (OR per each additional year, 0.98; 95% CI, 0.97–0.99) (Figure 3). Women with a kidney transplant were less likely to deliver preterm compared to women undergoing HD (OR, 0.92; 95% CI, 0.84–1.00). Black women were more likely to deliver preterm when compared to white (OR, 1.26; 95% CI, 1.07–1.49); however, there was no difference in preterm delivery between women who identified as Asian (OR, 1.02; 95% CI, 0.70–1.48) or Hispanic (OR, 0.93; 95% CI, 0.96–1.36) compared to white women.
Figure 3. Relationships between clinical characteristics and preterm delivery.
Forest plot showing multivariable association between clinical characteristics and odds of preterm delivery (with 95% confidence intervals) using logistic generalized estimating equations accounting for multiple deliveries in a single individual and adjusted for comorbidities.
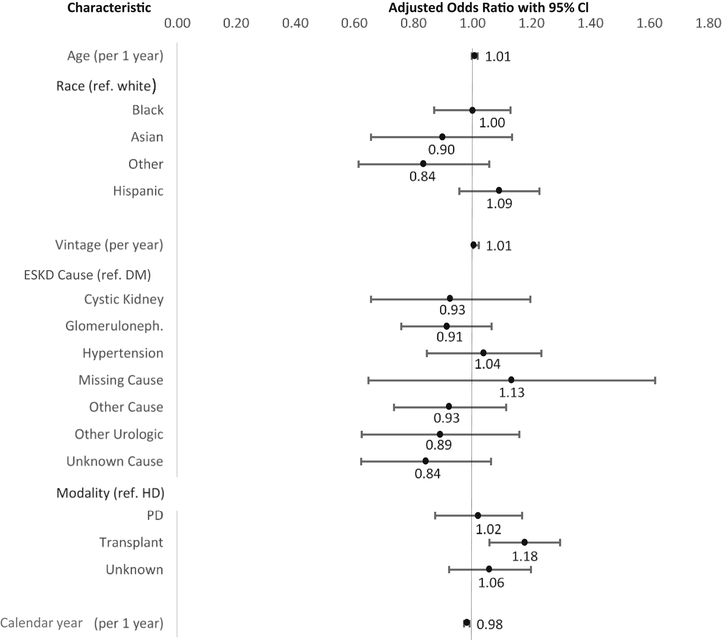
Amongst delivering women with ESKD from 2002 to 2015, cesarean delivery was observed in 39% of delivering women treated with HD, 41% treated with peritoneal dialysis, and 50.6% with a functioning kidney transplant. Women with a kidney transplant were more likely to deliver via cesarean (OR, 1.18; 95% CI, 1.06–1.31) (Figure 4) when compared to women receiving HD. Older women and women with longer KRT vintage were more likely to deliver via cesarean each year (OR for each group of 1.01 [95% CI, 1.00–1.02]).
Figure 4. Relationships between clinical characteristics and cesarean delivery.
Forest plot showing multivariable association between clinical characteristics and odds of cesarean delivery (with 95% confidence intervals) using logistic generalized estimating equations accounting for multiple deliveries in a single individual and adjusted for comorbidities.
Association of HD treatment characteristics with preterm delivery and cesarean section
A total of 199 women treated with HD between 2012 and 2015 had one delivery; 132 women had CROWNWeb data 30 days prior to delivery. Of these 132 delivering women, 69%, 5.3%, 7.6%, 15.2%, and 2.3% were prescribed 3, 4, 5, 6, and 7 sessions per week, respectively, at 30 days prior to their delivery. One individual was prescribed one session per week. A total of 48 women had 9 complete months of CROWNWeb data prior to delivery; over those 9 months, the proportion of women with a SUN < 50 mg/dL increased from 41.3% to 65.8% and the mean number of prescribed minutes per week increased from 678 minutes to 746 minutes (Figures S1a–d). There was no individual characteristic (age, race/ethnicity, vintage, cause of kidney failure, post-HD weight) that significantly predicted receipt of 5 or more dialysis treatments per week 30 days prior to delivery (Table S2). In the multivariable logistic regression model, delivered HD minutes per week and pre-HD SUN at 30 days prior to delivery were not significantly associated with pre-term delivery or cesarean delivery (Tables 2 and 3)
Table 2.
Adjusted association of HD treatment characteristics with preterm delivery
| Characteristic | OR (95% CI) | ||
|---|---|---|---|
| Age, per 1-y older | 0.97 (0.916–1.034) | ||
| Racea | |||
| Black | 1.85 | 0.746 | 4.603 |
| Other | 2.22 | 0.422 | 11.630 |
| Hispanic | 1.95 | 0.749 | 5.080 |
| KRT vintage, per 1-y longer | 1.01 | 0.950 | 1.072 |
| ESKD causeb | |||
| GN | 1.22 | 0.420 | 3.561 |
| HTN | 1.48 | 0.472 | 4.638 |
| Other | 1.66 | 0.470 | 5.851 |
| Delivered HD per week, per 10 min greater | 0.99 | 0.996 | 1.002 |
| Pre-HD SUN, per 1 mg/dL greater | 1.00 | 0.997 | 1.006 |
Reference group: White
Reference group: Diabetes Mellitus
Results of multivariable logistic regression models evaluating the association of preterm delivery with prescribed minutes of HD and pre-HD SUN (n=132).
Table 3.
Adjusted association of HD treatment characteristics with cesarean delivery
| Characteristic | OR | 95% CI | |
|---|---|---|---|
| Age, per 1-y older | 0.98 | 0.928 | 1.043 |
| Racea | |||
| Black | 0.91 | 0.394 | 2.083 |
| Other | 0.38 | 0.049 | 2.991 |
| Hispanic | 1.10 | 0.446 | 2.699 |
| KRT vintage, per 1-y longer | 1.02 | 0.961 | 1.087 |
| ESKD causeb | |||
| GN | 1.21 | 0.459 | 3.201 |
| HTN | 1.13 | 0.381 | 3.375 |
| Other | 2.57 | 0.803 | 8.245 |
| Delivered HD per week, per 10 min greater | 1.01 | 0.983 | 1.028 |
| Pre-HD SUN, per 1 mg/dL greater | 1.00 | 0.995 | 1.004 |
Reference group: White.
Reference group: Diabetes Mellitus
Results of logistic regression models evaluating the association of cesarean delivery with prescribed minutes of HD and pre-HD SUN (n=132).
Discussion
Using a comprehensive national registry of persons with ESKD in the US, we examined trends in hospital deliveries amongst women of childbearing age by KRT modality, and further investigated associations between individual clinical characteristics and delivery outcomes. We found that the delivery rate among women of childbearing age with ESKD has increased over time, specifically amongst patients treated with kidney transplantation or HD, who in 2015 delivered at a rate of 4.6 per 1000 patient-years and 3.6 per 1000 patient-years, respectively. This represents a 71% increase in delivery rate among women of childbearing age undergoing HD during the study period.
Prior work has supported improvement in pregnancy outcomes9,13,19, and potentially fertility20, with intensified hemodialysis (20–36 hours per week) and frequent long hemodialysis is recommended as the standard of care for women who become pregnant while on maintenance hemodialysis21. Novel use of CROWNWeb, an additional data source in USRDS available from 2012–2015, allowed us to describe the outpatient HD prescriptions for delivering women in that period and observe the associations between prescribed minutes of HD per week and pre-HD SUN with preterm delivery. Interestingly, we found that while the average number of HD minutes prescribed rose slightly over the 9 months prior to delivery, only a minority of women were prescribed greater than 1200 minutes of HD per week in their outpatient hemodialysis units 30 days prior to delivery. Thus intensified hemodialysis seems like an unlikely sole explanation for the increased delivery rate among women treated with HD in the United States. We did not find any individual demographics that significantly associated with the receipt of intensified HD, nor did we find a significant association between minutes of HD prescribed or pre-HD SUN with preterm delivery or cesarean section. Notably, CROWNWeb only reports outpatient dialysis prescriptions. One potential explanation for our observations is that additional or longer dialysis treatments may be delivered in the inpatient setting in the US, which were not captured in our analyses. Additionally, if a significant proportion of women are hospitalized for intensive dialysis, analysis of HD prescriptions as an outpatient 30 days prior to delivery may have captured only the healthiest of pregnant women on HD. In our sample, 65 women had at least one non-delivery hospitalization in the 9 months prior to their delivery. Hemodialysis adequacy guidelines published in 2015 recommended intensified HD20, however this may be challenging from an individual patient and HD unit perspective. Future study of individual, dialysis unit, and systems level facilitators and barriers to longer or more frequent HD, as well as standardized reporting and monitoring of pregnancy outcomes, are warranted to determine how to best provide patient-centered, cost-effective, high-quality HD care during pregnancy.
In our study period, patients treated with PD were significantly less likely to deliver and the rate of delivery in this group of patients remained low and static, with approximately 1 delivery per 1,000 patient-years in women of childbearing age. Our findings are similar to what was reported from a smaller US case-series22 and ANZDATA, where a pregnancy rate of 1.06 pregnancies per 1000 patient-years was observed for women on PD14. Mechanical or inflammatory effects of hypertonic intraperitoneal dialysate and/or prior episodes of peritonitis are two proposed physiologic mechanisms for lower fertility in women undergoing peritoneal dialysis, though these hypotheses have not been vigorously tested. While our data source cannot account for differences in pregnancy and motherhood desires between ESKD patients by modality, the observed differences across all of these studies suggest that women with ESKD seeking advice regarding dialysis modality and potential for conception, should be advised that the likelihood is lower with peritoneal dialysis compared to HD, and greater after transplantation.
While Gill et al.23 examined the birth rate amongst kidney transplant recipients between 1990 and 2003, the present study evaluates delivery rates from 2002 to 2015. In contrast to Gill et al., who found decreasing birth rates amongst transplant recipients from 1990 to 200323, our study has found rising delivery rates from 2002 to 2015 amongst women within three years of a kidney transplant. Though administrative data cannot fully elucidate the reasons for such a trend reversal, it is notable that Gill’s earlier study period coincided with the advent of a known teratogen, mycophenolate mofetil (MMF), as standard of care in immunosuppression for transplant recipients beginning in 1995. This novel agent may have influenced contemporary nephrologists’ counseling patterns to encourage MMF in conjunction with contraception, in parallel with national initiatives to improve contraception use amongst women with kidney transplants at that time. In 2005, the American Society of Transplantation published guidelines on reproduction and transplantation that acknowledged that prior recommendations on timing of conception may have been overly restrictive24 and azathioprine is the preferred alternative to MMF in pregnancy. This too may have played a role in the trend reversal during our study period. Furthermore, several qualitative studies examining women’s perspectives on pregnancy in light of their kidney disease have been published over our study period, as summarized by Tong et al.25 Such studies may have also brought attention to the need for more patient-centered approaches to care in this group of patients over the last decade.
Our study observed the overall odds of preterm delivery decreased by 2% per year. Preterm delivery occurred in 33% of women with a functioning kidney transplant, and 41% of women treated with HD or peritoneal dialysis. Within a similar study period, ANZDATA reported 46.6% of babies to mothers on dialysis were born preterm14 and Piccoli et al. reported preterm delivery in 90.5% of mothers on dialysis in Italy25,26. The variation in findings may be due to differences in methodology; while ANZDATA is a national registry of ESKD patients and collects specific information regarding pregnancy outcomes14, the Italian group used surveys of public dialysis centers and follow up with patients and caregivers to ascertain information regarding live birth outcomes26 which may have been susceptible to reporting bias. A major strength of our study was use of a national registry of persons with ESKD, linked to claims data for identification of hospital deliveries. In the US, we observed Black women with ESKD were significantly more likely to deliver preterm when compared to white women. This echoes concerning national data from the US: preterm delivery is more common amongst all delivering Black women27 and this includes women with ESKD.
Our study also observed that 50.6% of transplant recipients gave birth via cesarean delivery, and transplant recipients were at higher odds of cesarean delivery compared to women treated with dialysis. Similarly, in a systematic review and meta-analysis, Deshpande et al. reported cesarean deliveries in 53% of live births amongst kidney transplant recipients in North America. Deshpande’s work also observed an increased rate of gestational diabetes amongst transplant recipients.11 Risk factors for cesarean delivery include maternal obesity, excessive maternal weight gain,28 and gestational diabetes.29 Steroid use amongst transplant recipients may increase the likelihood of excessive gestational weight gain and gestational diabetes, subsequently increasing the risk for cesarean delivery. Weight and prior cesarean delivery, another significant risk factor for a subsequent cesarean delivery, were unable to be controlled for in our analyses of outcomes amongst transplant recipients.
Our findings should be interpreted in light of certain limitations. This analysis examines women with Medicare as their primary insurer. While this constitutes approximately 80% of prevalent ESKD patients, Medicare coverage is provided to transplant recipients only for the first 3 years following transplant. We may have disproportionately missed younger patients with private insurance who are more likely to deliver. These policies have not changed over the study period and are unlikely to affect observed trends, though absolute delivery rates reported herein are likely conservative. Additionally, we have relied on established ICD-9-CM codes for identification of hospital deliveries of live-born infants as well as preterm and cesarean deliveries16,30; however we may have missed the most severe adverse events of early perinatal and very preterm delivery, particularly in our analyses of outpatient HD treatment characteristics 30 days prior to delivery. Finally, while residual kidney function is suspected to play a significant role in fertility and pregnancy outcomes, we were unable to control for this in our analyses due to incomplete reporting in CROWNWeb. However, given that delivery was associated with shorter KRT vintage, and vintage is inversely correlated with residual kidney function31, this suggests that higher residual kidney function may play a role in successful conception and delivery.
In conclusion, obstetric delivery rates in women with ESKD rose by nearly 50% between 2002 and 2015, most notably for women on HD or with a functioning kidney transplant. These women are at high risk of pre-term delivery, particularly amongst Black women with ESKD. Future work should explore facilitators and barriers to implementation of outpatient intensified HD as well as alternative settings for antenatal HD for this high risk population, to understand best practices for improved outcomes in the US. Addressing family planning preferences of women of childbearing age with ESKD is an imperative for nephrologists and ESKD management teams, as this challenging clinical scenario becomes more common over time.
Supplementary Material
Figures S1. Descriptive statistics of HD parameters for 9 months prior to delivery.
Table S1. List of ICD-9-CM codes defining delivery.
Table S2. Associations of clinical characteristics with 5 or more HD sessions prescribed per week in 30 days prior to delivery.
Acknowledgements
We acknowledge the Co-Deputy Directors of the USRDS Coordinating Center when it was based in Ann Arbor, Vahakn Shahinian, MD, University of Michigan, and Bruce Robinson, MD, Vice President, Arbor Research Collaborative for Health, as well as the NIDDK Project Officers, Kevin C. Abbott, MD, MPH and Lawrence Y.C. Agodoa, MD.
Support: The USRDS is funded by NIDDK, through NIH contract HHSN276201400001C. The USRDS Coordinating Center was located at the Kidney Epidemiology and Cost Center, University of Michigan, in partnership with Arbor Research Collaborative for Health, Ann Arbor, Michigan, from 2014–2019; Dr Saran served as Director. Andrea L. Oliverio was supported by NIH-NIDDK 5T32DK007378–37. The funders had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
Disclaimer: The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the U.S. government.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Palmer BF, Clegg DJ. Gonadal dysfunction in chronic kidney disease. Rev Endocr Metab Disord 2017;18:117–30. [DOI] [PubMed] [Google Scholar]
- 2.Holley JL, Schmidt RJ. Changes in fertility and hormone replacement therapy in kidney disease. Adv Chronic Kidney Dis 2013;20:240–5. [DOI] [PubMed] [Google Scholar]
- 3.Strippoli GF, Collaborative D, Sexual Dysfunction in Hemodialysis Working G, et al. Sexual dysfunction in women with ESRD requiring hemodialysis. Clin J Am Soc Nephrol 2012;7:974–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtulus FO, Salman MY, Fazlioglu A, Fazlioglu B. Effects of Renal Transplantation on Female Sexual Dysfunction: Comparative Study With Hemodialysis and a Control Group. Transplant Proc 2017;49:2099–104. [DOI] [PubMed] [Google Scholar]
- 5.Basok EK, Atsu N, Rifaioglu MM, Kantarci G, Yildirim A, Tokuc R. Assessment of female sexual function and quality of life in predialysis, peritoneal dialysis, hemodialysis, and renal transplant patients. Int Urol Nephrol 2009;41:473–81. [DOI] [PubMed] [Google Scholar]
- 6.Oliverio AL AL, Mariani LH, Winkelman TNA, Dalton VK. Health Outcomes and Health Care Utilization Among Obstetric Deliveries With Concurrent CKD in the United States. Am J Kidney Dis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tangren J, Nadel M, Hladunewich MA. Pregnancy and End-Stage Renal Disease. Blood Purif 2018;45:194–200. [DOI] [PubMed] [Google Scholar]
- 8.Hou SH. Frequency and outcome of pregnancy in women on dialysis. Am J Kidney Dis 1994;23:60–3. [DOI] [PubMed] [Google Scholar]
- 9.Luders C, Castro MC, Titan SM, et al. Obstetric outcome in pregnant women on long-term dialysis: a case series. Am J Kidney Dis 2010;56:77–85. [DOI] [PubMed] [Google Scholar]
- 10.Wang GC, Zheng JH, Xu LG, et al. Measurements of serum pituitary-gonadal hormones and investigation of sexual and reproductive functions in kidney transplant recipients. Int J Nephrol 2010;2010:612126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deshpande NA, James NT, Kucirka LM, et al. Pregnancy outcomes in kidney transplant recipients: a systematic review and meta-analysis. Am J Transplant 2011;11:2388–404. [DOI] [PubMed] [Google Scholar]
- 12.Shah S, Venkatesan RL, Gupta A, et al. Pregnancy outcomes in women with kidney transplant: Meta-analysis and systematic review. BMC Nephrol 2019;20:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piccoli GB, Minelli F, Versino E, et al. Pregnancy in dialysis patients in the new millennium: a systematic review and meta-regression analysis correlating dialysis schedules and pregnancy outcomes. Nephrol Dial Transplant 2016;31:1915–34. [DOI] [PubMed] [Google Scholar]
- 14.Shahir AK, Briggs N, Katsoulis J, Levidiotis V. An observational outcomes study from 1966–2008, examining pregnancy and neonatal outcomes from dialysed women using data from the ANZDATA Registry. Nephrology (Carlton) 2013;18:276–84. [DOI] [PubMed] [Google Scholar]
- 15.About CROWNWeb. (Accessed April 24, 2019, at mycrownweb.org.)
- 16.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J 2008;12:469–77. [DOI] [PubMed] [Google Scholar]
- 17.Wilcox AJ, Weinberg CR, O’Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med 1988;319:189–94. [DOI] [PubMed] [Google Scholar]
- 18.End stage renal disease medical evidence report Department of Health and Human Services, Center for Medicare and Medicaid Services (Accessed Oct 9, 2018, at https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms2728.pdf.)
- 19.Hladunewich MA, Hou S, Odutayo A, et al. Intensive hemodialysis associates with improved pregnancy outcomes: a Canadian and United States cohort comparison. J Am Soc Nephrol 2014;25:1103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barua M, Hladunewich M, Keunen J, et al. Successful pregnancies on nocturnal home hemodialysis. Clin J Am Soc Nephrol 2008;3:392–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Kidney F KDOQI Clinical Practice Guideline for Hemodialysis Adequacy: 2015 update. Am J Kidney Dis 2015;66:884–930. [DOI] [PubMed] [Google Scholar]
- 22.Okundaye I, Abrinko P, Hou S. Registry of pregnancy in dialysis patients. Am J Kidney Dis 1998;31:766–73. [DOI] [PubMed] [Google Scholar]
- 23.Gill JS, Zalunardo N, Rose C, Tonelli M. The pregnancy rate and live birth rate in kidney transplant recipients. Am J Transplant 2009;9:1541–9. [DOI] [PubMed] [Google Scholar]
- 24.McKay DB, Josephson MA, Armenti VT, et al. Reproduction and transplantation: report on the AST Consensus Conference on Reproductive Issues and Transplantation. Am J Transplant 2005;5:1592–9. [DOI] [PubMed] [Google Scholar]
- 25.Tong A, Jesudason S, Craig JC, Winkelmayer WC. Perspectives on pregnancy in women with chronic kidney disease: systematic review of qualitative studies. Nephrol Dial Transplant 2015;30:652–61. [DOI] [PubMed] [Google Scholar]
- 26.Piccoli GB, Cabiddu G, Daidone G, et al. The children of dialysis: live-born babies from on-dialysis mothers in Italy--an epidemiological perspective comparing dialysis, kidney transplantation and the overall population. Nephrol Dial Transplant 2014;29:1578–86. [DOI] [PubMed] [Google Scholar]
- 27.Describing the Increase in Preterm Births in the United States, 2014–2016. (Accessed April 25, 2019, at https://www.cdc.gov/nchs/products/databriefs/db312.htm.)
- 28.Young TK, Woodmansee B. Factors that are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol 2002;187:312–8; discussion 8–20. [DOI] [PubMed] [Google Scholar]
- 29.Gorgal R, Goncalves E, Barros M, et al. Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J Obstet Gynaecol Res 2012;38:154–9. [DOI] [PubMed] [Google Scholar]
- 30.Admon LK, Winkelman TNA, Moniz MH, Davis MM, Heisler M, Dalton VK. Disparities in Chronic Conditions Among Women Hospitalized for Delivery in the United States, 2005–2014. Obstet Gynecol 2017;130:1319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daugirdas JT, Greene T, Rocco MV, et al. Effect of frequent hemodialysis on residual kidney function. Kidney Int 2013;83:949–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figures S1. Descriptive statistics of HD parameters for 9 months prior to delivery.
Table S1. List of ICD-9-CM codes defining delivery.
Table S2. Associations of clinical characteristics with 5 or more HD sessions prescribed per week in 30 days prior to delivery.