Abstract
Purpose:
To investigate associations between sleep disturbances and mental health in adolescents.
Method:
Data are from a national sample of 11,670 US participants (5594 female, aged 9-10 years, 63.5% White) in the Adolescent Brain Cognitive Development (ABCD) study. Initial longitudinal analyses were conducted for a subset of the sample (n=4951). Measures of youth sleep disturbance (disorders of initiating and maintaining sleep [DIMS], sleep-wake transition disorders [SWTD] and disorders of excessive somnolence [DOES]) and ‘typical’ total sleep time (TST) (number of hours slept on most nights in the past six months) were obtained from the parent-report Sleep Disturbance Scale (Data Release 2.0). Parent-report measures of youth mental health (depression, internalizing and externalizing behaviors) from the Child Behavior Checklist and typical screen-time were included.
Results:
At baseline, greater sleep disturbance and shorter TST were associated with greater internalizing, externalizing and depression scores. After controlling for baseline mental health symptoms, baseline sleep disturbance significantly predicted depression, internalizing and externalizing scores at one-year follow-up. A significant interaction with sex indicated that the association between DOES and depression one year later was steeper for girls, compared to boys (p<0.001, 95% CI 1.04-3.45).
Conclusion:
Sleep disturbances predicted future mental health, particularly depression in this young sample, highlighting the potential to harness sleep as a tool to mitigate the persistence of depression across early-adolescence and potentially prevent an adolescent onset of major depressive disorder.
Keywords: adolescent, children, sleep duration, minority, longitudinal, mental health
Introduction
The incidence of depression increases markedly during adolescence1, the phase of life stretching between childhood and adulthood (10-24 years)2. Depression is the most common psychiatric disorder in youth3, is ranked worldwide as the most burdensome condition in those under 254 and is a major risk factor for adolescent suicide5. An onset of major depressive disorder (MDD) during this time-period strongly predicts a lifetime trajectory of depressive episodes6. Thus, identifying positive modifiers of depression symptomology is key to developing preventative and treatment strategies that can be applied in early life, before an onset of MDD has occurred. Sleep is one potentially modifiable, behavior that undergoes considerable change across adolescence and is vital for brain plasticity. Improving sleep during adolescence may capitalize on ongoing neurodevelopmental processes to facilitate brain plasticity and lessen the impact of neural vulnerabilities to depression and reduce the risk of subsequent depressive episodes.
Sleep complaints are a key symptom of MDD in children and adolescents7 and reduced quantity of sleep increases the risk for MDD three-fold in adolescents8. Sleep disturbance is associated with an increased risk of suicide9. Specifically, adolescents who sleep less than 6 hours are three times as likely to consider suicide, compared to those who sleep for 8 hours10. Furthermore, sleep is a behavior that undergoes considerable change during mid-adolescence: adolescents frequently obtain insufficient sleep, driven by a normative delay in circadian phase and altered homeostatic dynamics11 and extracurricular activities, academic and social pressures which results in a preference for later bed times12. When these are combined with early school start times, insufficient sleep ensues. Recently, links between greater electronic device use and poor sleep have been identified13 and sleep loss may mediate relationships between media use and depressive symptoms14. However, while negative relationships between adolescent media use and mental health are commonly posited, recent studies utilizing large samples have identified marginal relationships15 and it remains to be seen whether such associations exist in early adolescence.
To date, longitudinal studies investigating associations between sleep and depression from early – late adolescence are sparse16, with most studies focusing on mid-older rather than young (< 11 years old) adolescent periods. Results from several prospective studies on mid-late adolescence, have suggested sleep disturbance is a precursor to depression17, however, large scale studies across early adolescence are required to further establish how poor sleep health may facilitate the onset of adolescent MDD. Here, we utilized data from The Adolescent Brain Cognitive Development (ABCD) study to assess how sleep disturbance and typical total sleep time are associated with depression symptoms at baseline and one-year follow-up in early-adolescents without a diagnosis of MDD. We hypothesized that sleep disturbances would predict depression one year later, particularly in girls, who are uniquely vulnerable during this developmental period18.
Method
Participants
11,875 participants, aged 9-10 years, were enrolled across the 21 ABCD data collection sites, which cover 17 states (https://abcdstudy.org/study-sites/). The ABCD study employed a rigorous epidemiologically informed school-based recruitment strategy, designed with consideration of the demographic composition of the 21 ABCD sites and the US as a whole19. Exclusionary criteria were minimal and are listed in supplementary material with the site list. Baseline analyses included 11,670 participants with complete data on sleep disturbances, mental health scales, parent-reported screen-time and relevant covariates: age, sex, race, ethnicity, and parental socioeconomic status (SES). Longitudinal analyses are on a subset of the sample (4,951 participants) who had completed their 1-year follow-up assessment by the time of the data release (ABCD 2.0 release: https://nda.nih.gov/study.html?id=634).
Procedure
All adult (parent/caregiver) participants provided written informed consent, and all youth provided written assent along with permission from a parent/legal guardian. Parents completed self-report measures in private via Redcap on an iPad. Youth worked separately with a research assistant to answer questionnaires, complete cognitive tasks and a Magnetic Resonance Imaging (MRI) session.
Measures
Demography
Parents answered a demographic questionnaire20. As multiple races could be selected per child, steps were taken to reduce the number of race categories to be used for statistical models, which resulted in six final race categories for statistical analyses: White, Black, Asian, Multiple, Other, Unsure. See supplementary material for procedures used for race category reduction. For all models, White was the reference category. Hispanic/Latino ethnicity was also assessed in all models, using non-Hispanic as the reference category. SES was estimated by identifying the maximum level of education across parents/guardians and categorized as follows: less than high school, high school/GED, some college, associate degree, Bachelor/professional degree and postgraduate degree. Bachelor/professional degree was the reference category. While household income is available, it is corelated with site, which is already controlled for in the model as random effects variable and thus we chose to include parental education only as an estimator of SES.
Family history of depression was also estimated from the parent-report item “Has ANY blood relative of your child ever suffered from depression, that is, have they felt so low for a period of at least two weeks that they hardly ate or slept or couldn’t work or do whatever they usually do?”. For this analysis, if the parent endorsed family history of depression for any relative, family history was recorded as ‘yes’. In all models, no-family history was the reference category.
Sleep
Sleep characteristics were assessed from the parent-report measure; Sleep Disturbance Scale for Children (SDSC)21, designed to categorize sleep disorders in children. The SDSC is a 27-item inventory rated on a 5-point Likert-type scale that provides scores on five subdomains, of which we focused on three: disorders of initiating and maintaining sleep, disorders of excessive somnolence and sleep-wake transition disorders that have been previously associated with mental health.
The individual item ‘How many hours of sleep does your child get on most nights?’ was used as the measure for typical TST (TST). Possible responses were: 1) 9-11 hours, 2) 8-9 hours, 3) 7-8 hours, 4) 5-7 hours, 5) Less than 5 hours. Given the small number of participants in the 5th category (n=34, 0.3% of sample) we combined categories 4 and 5. In all models that included TST, 9-11 hours was the reference category, since it is the recommended TST for this age group22.
Mental health
Mental health variables were derived from the Child Behavior Checklist (CBCL)23, a widely used, standardized measure for evaluating maladaptive behavioral and emotional problems in youth aged 4-18 years. Parents rate how true each item is now, or was within the past 6 months, using a 3- point Likert scale. The CBCL yields scores on internalizing (i.e., anxious, depressive, and overcontrolled), externalizing (i.e., aggressive, hyperactive, noncompliant, and under-controlled), and total problems and scores on DSM-oriented scales. All scores were standardized t-scores, based on national norms, scaled so that 50 is average for the youth’s age and gender, with a standard deviation of 10 points. Higher scores indicate greater problems. Of the 13 items within the DSM-depression scale, 4 related to sleep. Removing these items resulted in small changes to the scale’s raw-scores (9112 participants had zero change to their raw-score and the mean raw-score change was 1.2 [SD: 0.9]) and thus, in order to utilize the t-score measures, which were computed based on all items of the scales, we did not remove these items. For comparison we also assessed the CBCL withdrawn/depressed subscale, which did not comprise any items relating to sleep.
Youth and parents also completed the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS) clinical interview which were assessed to ensure that none of the participants included in the longitudinal analyses here met criteria for current MDD.
Screen time
Parents reported how much time their child spent using different types of electronic devices (computer, cell phone, tablet, iPod, other device), on a typical weekday (Monday-Friday) and weekend day (Saturday-Sunday). Parents were asked to not include time spent on school-related work but to include time spent watching TV or videos online, texting and chatting, playing games and visiting social networking sites. A measure of total daily screen-time for weekdays and weekends was then computed, which was time summed across the two reported times and used in the analysis.
Statistical procedure
Generalized additive mixed models (GAMMs) were used to investigate how sleep may be associated with mental health, using Stata software. The GAMM model is appropriate for both cross-sectional and longitudinal regression analyses and allows for an explicit modelling of aspects of the study design such as nesting of participants within sites and family. For each model, demographic factors (race, ethnicity, sex, parental education), site and twin/sibling status were included as covariates. For depression models, family history of depression (yes/no) was also included as a covariate. As sleep disturbance and screen-time measures were non-normally distributed, they were log-transformed prior to inclusion in the models.
For baseline analyses, separate GAMMs assessed each mental health measure (internalizing, externalizing, DSM-depression). As sleep measures were moderately-highly associated with each other, individual GAMMs assessed the relationship between each mental health and sleep variable separately (TST, disorders of excessive somnolence, disorders of initiating and maintaining sleep, sleep-wake transition disorders) and then model fit statistics were used to determine which sleep variable was best associated with each mental health variable.
For longitudinal analyses, similar GAMMs were run to assess mental health at follow-up. For each model, baseline sleep measures and covariates were included, as well as the baseline mental health measure (i.e. the GAMM assessing how baseline sleep disturbance predicts depression at follow-up included baseline depression as an additional covariate). The follow-up model for depression included sex interaction effects (sleep disturbance*sex, baseline depression*sex).
Results
Sample characteristics at baseline
At baseline, participants were aged 9-10.92 years, with a mean age of 9.9 years, and were typically pre-pubescent (See Table 1). The sample consisted of an almost equal distribution of the sexes (47.9% female) and a majority of non-Hispanic participants (79.5%). 63.5% of the participants were White and approximately 60% of the sample had parental education status which was a bachelors/professional degree or higher. On average, participant’s scores on the internalizing, externalizing and DSM-depression scales were in the normal range with 3% scoring within the ‘clinical range’ for the DSM depression scale, 9% for internalizing and 6% for externalizing scales.
Table 1:
Parent-reported demographic, mental health, sleep and screen-time use characteristics of the baseline ABCD sample. SD= standard deviation, CBCL= Child Behavior Check List, SDSC= Sleep Disturbance Scale for Children, DIMS= Disorders Initiating and Maintaining Sleep, DOES=Disorders of Excessive Somnolence, SWTD= Sleep-Wake Transition Disorders, PDS= puberty status from the Pubertal Development Scale40.
| Measure | Frequency | Percent | |
|---|---|---|---|
| Sex | |||
| Female | 5594 | 47.9 | |
| Male | 6076 | 52.1 | |
| PDS | |||
| Pre-puberty | 5833 | 49.1 | |
| Early-puberty | 2712 | 22.8 | |
| Mid-puberty | 2872 | 22.5 | |
| Late-puberty | 170 | 1.4 | |
| Post-puberty | 10 | 0.1 | |
| Ethnicity | |||
| Hispanic | 2391 | 20.5 | |
| Not-Hispanic | 9279 | 79.5 | |
| Race | |||
| White | 7411 | 63.5 | |
| Black | 2266 | 19.4 | |
| Asian | 604 | 5.2 | |
| Multiple | 292 | 2.5 | |
| Other | 937 | 8.0 | |
| Unsure | 160 | 1.4 | |
| Parental education | |||
| < High school | 574 | 4.9 | |
| High School/GED | 1104 | 9.5 | |
| Some college | 1485 | 12.7 | |
| Associate degree | 1550 | 13.3 | |
| Graduate/professional degree | 3547 | 30.4 | |
| Postgraduate degree | 3410 | 29.2 | |
| Total sleep time | |||
| 9-11 hours | 5543 | 47.5 | |
| 8-9 hours | 4349 | 37.3 | |
| 7-8 hours | 1384 | 11.9 | |
| <5 – 7 hours | 394 | 3.4 | |
| Measure | Mean or median | Range | SD |
| Age (months) | 119 | 108-131 | 7.5 |
| BMI | 17.7† | 10.1-45 | 4.2 |
| Internalizing (CBCL t-score) | 48.4† | 33-93 | 16.6 |
| Externalizing (CBCL t-score) | 44.0† | 33-84 | 10.3 |
| DSM5 Depression (CBCL t-score) | 50.0† | 50-89 | 5.7 |
| DIMS (SDSC) | 11† | 7-35 | 3.8 |
| DOES (SDSC) | 6† | 5-25 | 2.6 |
| SWTD (SDSC) | 7† | 6-30 | 2.4 |
| Weekday screen-time (hours) | 2 | 0-24 | 2.7 |
| Weekend screen-time (hours) | 3.5 | 0-24 | 2.6 |
Median is reported instead of the mean, because of the skewed distribution of the data.
Sleep disturbance scales from the SDSC indicated low levels of problems and average total sleep time (TST) was 9-11 hours.
Demographic differences in sleep and mental health at baseline
Multinomial logistic regression analyses identified age, race and parental education (p<.001) were significantly associated with TST; Black and multiple-race and older age were all associated with a greater likelihood of shorter TST. Bachelor’s and post-graduate parental education were associated with a greater likelihood of longer TST. Specifically, 55% of both White and Asian participants were reported to have the recommended 9-11 hours TST, compared to 25% of Black participants and 35% of Hispanic participants. Controlling for all other demographic variables, being Hispanic reduced the probability of being in category 9-11 (OR .706, 95% CI .626-.727) and increased the probability of being in category 7-8 (OR 1.34, 95% CI 1.13-1.59). Conversely, being multiple-race reduced the probability of being in category 9-11 (OR .626, 95% CI .474-.827) and increased the odds of being in category <5-7 (OR 3.29, 95% CI 1.96-5.56). Being Black reduced the probability of being in category 9-11 (OR .389, 95% CI .342-.443) and increased the probability of being in category <5-7 (OR 4.55, 95% CI 3.44-6.01). See Figure 1.
Figure 1:
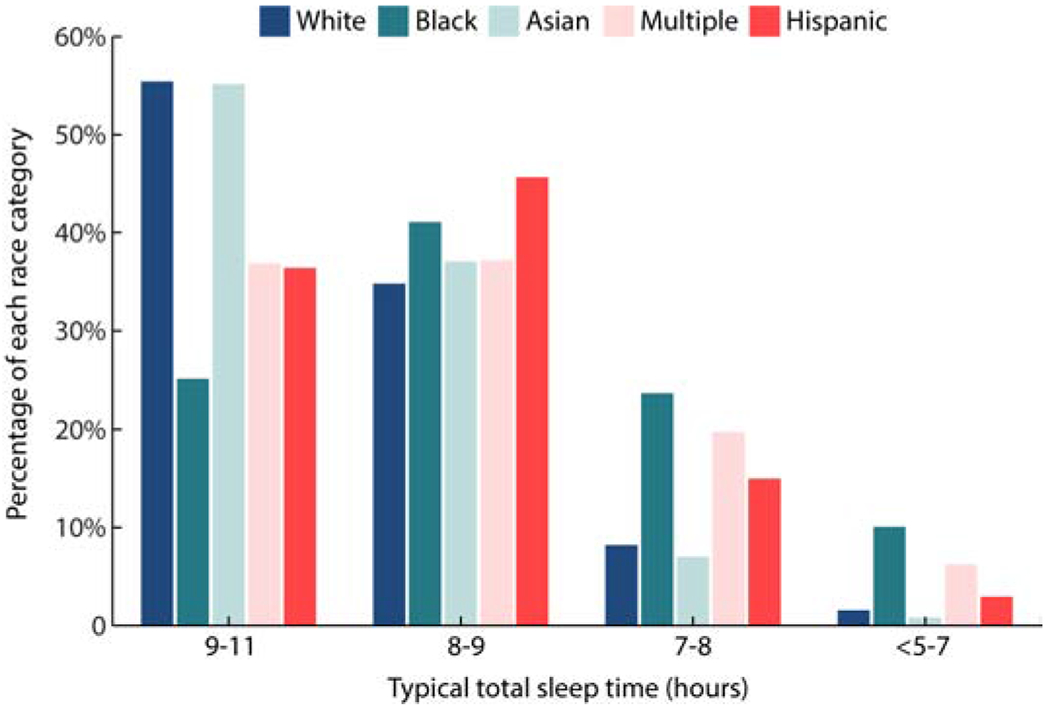
Proportion of each race category divided according to parent-reported total sleep time (TST) duration. After controlling for other demographic variables, Black and multiple race participants were significantly more likely to belong to the shortest TST categories compared to White participants.
Demographic variables alone accounted for a small proportion of variance in sleep disturbance variables (~1%), externalizing (3%), internalizing (2%) and depression (4%) measures and thus are not discussed further.
Baseline associations between TST, sleep disturbance and mental health
Sleep disturbance scores (disorders of excessive somnolence, disorders of initiating and maintaining sleep or sleep-wake transition disorders) accounted for 17 - 24% of the variance in internalizing (R2= 0.19), externalizing (R2= 0.17) and depression scores (DSM-scale: R2= 0.25, Withdrawn/depressed scale: R2=0.17), after adjusting for sociodemographic variables, site, and sibling/twin status. While all sleep disturbance measures were significantly associated with mental health, model fit statistics (BIC) indicated marginally better fits when using different sleep disturbance variables; internalizing symptoms were most associated with disorders of excessive somnolence, while externalizing symptoms and depression scores were most associated with disorders of initiating and maintaining sleep (Figure 2). See Table 2 for model statistics. In all cases, greater sleep disturbance was associated with poorer mental health (i.e. greater t-score).
Figure 2:
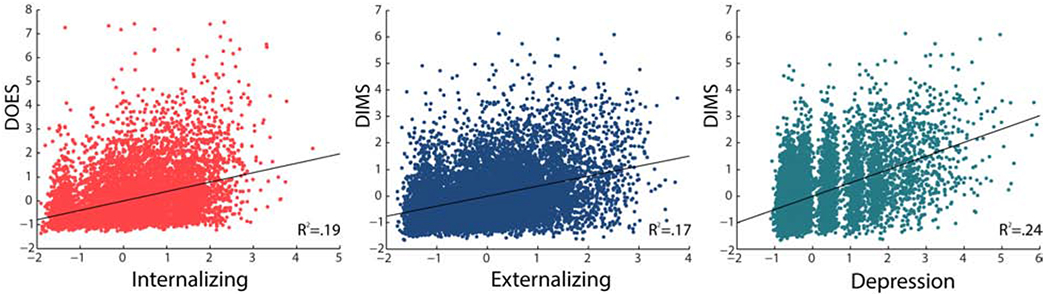
Associations between parent-reported sleep disturbance and mental health score in the ABCD sample at baseline. Child Behavior Checklist (CBCL) and Sleep Disturbance Scale for Children (SDSC) residuals are plotted after controlling for demographic variables (age, sex, race, ethnicity, parent education. Family history of depression was also included in the depression model), site and twin/sibling status. DIMS: Disorders Initiating and Maintaining Sleep; DOES: disorders of excessive somnolence. The sleep disturbance that was best associated with each mental health score is presented. R2 represents the full model (including all covariates above).
Table 2:
Outcomes for GAMM models assessing cross-sectional associations between baseline sleep and mental health in the ABCD sample. R2 is reported for the full model, BIC: Bayesian Information Criteria to assess model fit, β = standardized beta for the sleep variable in the model, CI = confidence interval for the sleep variable in the model. As TST was a categorical variable, β and CI are reported for two categories (7-8 hours and <5-7 hours), the longest TST category (9-11 hours, the recommended TST for 9-10-year olds20) was the reference category in the TST models. Models with the best fit for each mental health score are highlighted in bold. NS = not significant.
| Baseline model statistics | |||
|---|---|---|---|
| Covariates: age, sex, race, ethnicity, parent education, site and twin/sibling status. Family history of depression was also included in the depression models | |||
| Internalizing | Externalizing | Depression | |
| DIMS | BIC: 85982 | BIC: 85468 | BIC: 67757 |
| R2: 0.18 | R2: 0.17 | R2: 0.25 | |
| β: 0.41 | β: 0.39 | β: 0.46 | |
| CI: 31.51-34.33 | CI: 28.32-32.60 | CI:20.10-21.61 | |
| DOES | BIC: 85938 | BIC: 85514 | BIC: 68165 |
| R2: 0.19 | R2: 0.17 | R2: 0.22 | |
| β: 0.41 | β: 0.37 | β: 0.43 | |
| CI: 31.0-33.74 | CI: 27.256-29.95 | CI: 18.06-19.57 | |
| SWTD | BIC: 86243 | BIC: 85895 | BIC: 69208 |
| R2: 0.15 | R2: 0.12 | R2: 0.12 | |
| β: 0.36 | β: 0.31 | β: 0.30 | |
| CI: 28.73-31.73 | CI: 23.35-26.31 | CI:12.94-14.64 | |
| TST | BIC: 87729 | BIC: 86963 | BIC: 69773 |
| R2: 0.03 | R2: 0.04 | R2: 0.08 | |
| β (7-8 hrs): 0.08 | β (7-8 hrs): 0.08 | β (7-8 hrs): 0.15 | |
| CI: 1.86-3.18 | CI: 1,78-3.05 | CI: 2.30-3.0 | |
| β (<5-7 hrs): 0.12 | β (<5-7 hrs): 0.12 | β (<5-7 hrs): 0.21 | |
| CI: 5.54-7.75 | CI: 5.71-7.85 | CI: 6.15-7.35 | |
| Longitudinal model statistics | |||
| Covariates: baseline mental health score, age, sex, race, ethnicity, parent education, site and twin/sibling status. Family history of depression was also included in the depression models | |||
| Internalizing | Externalizing | Depression | |
| DIMS | BIC: 33708 | BIC: 32552 | BIC: 28882 |
| R2: 0.47 | R2: 0.54 | R2: 0.41 | |
| β: 0.07 | β: 0.05 | β: 0.11 | |
| CI: 4.45-8.33 | CI: 2.07-5.47 | CI: 4.41-6.75 | |
| DOES | BIC: 33578 | BIC: 32561 | BIC: 28859 |
| R2: 0.47 | R2: 0.54 | R2: 0.41 | |
| β: 0.07 | β: 0.05 | β: 0.13 | |
| CI: 3.89-7.74 | CI: 2.16-5.55 | CI: 4.79-7.15 | |
| SWTD | BIC: 33657 | BIC: 32507 | BIC: 28870 |
| R2: 0.47 | R2: 0.54 | R2: 0.40 | |
| β: 0.06 | β: 0.03 | β: 0.07 | |
| CI: 3.20-7.14 | CI: 0.96-4.41 | CI: 2.36-4.72 | |
| TST | BIC: 33766 | BIC: 32585 | BIC: 28974 |
| R2: 0.46 | R2: 0.54 | R2: 0.40 | |
| β (7-8 hrs): 0.01NS | β (7-8 hrs): 0.03 | β (7-8 hrs): 0.02NS | |
| CI: −0.29 – 1.28 | CI: 0.29-1.67 | CI: 0.04-1.0 | |
| β (<5-7 hrs): 0.001NS | β (<5-7 hrs): 0.03 | β (<5-7 hrs): 0.02NS | |
| CI: −1.42-1.57 | CI: 0.47-3.12 | CI: −0.08-1.77 | |
Models that included TST were significantly poorer fit compared to those that included sleep disturbance, accounting for 4-9% of the variance in mental health scores (Table 2). Within TST models, all TST categories were significant (p<0.001), indicating that, those sleeping less than 9-11 hours had significantly poorer mental health scores, compared to those sleeping 9-11 hours. Greatest effects were always identified for the shortest TST category (<5-7 hours), compared to the longest (9-11 hours).
In all models, although total screen time was significantly associated with mental health score, including it did not result in a significant increase in model fit and increased the variance explained by less than 1%. Additional models that replaced total screen time with weekday or weekend screen time resulted in almost identical outcomes. As such, screen time was not included in final models.
Longitudinal associations between sleep disturbance and mental health
For each model, after accounting for baseline mental health symptoms, baseline sleep disturbance significantly predicted mental health symptoms at one-year follow-up. In line with the results from the baseline analyses, models all performed similarly, with marginally better fits which indicated greater baseline disorders of excessive somnolence best predicted internalizing (β=.07, p<0.001) and depression (DSM-scale: β=.13, p<0.001, withdrawn/depressed scale: β=.08, p<0.001) scores at 1YFU and greater baseline disorders of initiating and maintaining sleep best predicted externalizing scores at 1YFU (β=.05, p<0.001). See Figure 3. For the depression model, a significant disorders of excessive somnolence*sex interaction identified that the association between disorders of excessive somnolence and 1YFU depression was steeper for girls, compared to boys (p<0.001, 95% CI 1.04-3.45), whilst holding all other variables constant. For each one unit increase in disorders of excessive somnolence, 1YFU depression increased by 3.7 units in boys and 8.2 units in girls (1YFU depression= 5.97 + 2.24*sex†, where boys are coded as −1 and girls as +1).
Figure 3:
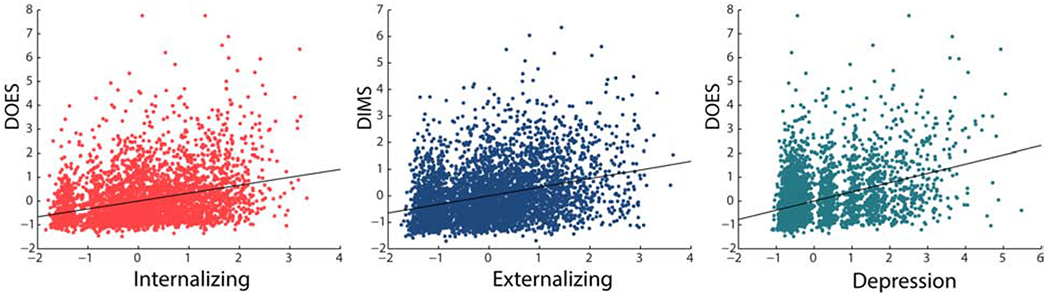
Associations between parent-reported sleep disturbance and mental health score in the ABCD sample at 1-year follow-up (1YFU). 1YFU Child Behavior Checklist (CBCL) and baseline Sleep Disturbance Scale residuals are plotted after controlling for demographic variables (age, sex, race, ethnicity, parent education. Family history of depression was also included in the depression model), site and twin/sibling status. DIMS: Disorders Initiating and Maintaining Sleep; DOES: disorders of excessive somnolence. The sleep disturbance that was best associated with each mental health score at follow-up is presented.
Short baseline TST (<5-7 hours) also significantly predicted externalizing symptoms at 1YFU (β=.03, p=0.003) after controlling for baseline externalizing score. Greater baseline mental health scores were strongly associated with greater scores at 1YFU (internalizing β= .57, depression β=.64, externalizing β=.70). See Figure 4. Adding baseline screen-time to the models did not significantly improve model fit.
For all analyses, models that replaced age with pubertal status, as assessed by the parental Pubertal Development Scale, performed almost identically, likely given the restricted range of pubertal development at this time point.
Discussion
Here we identified cross-sectional and longitudinal associations between sleep characteristics and mental health in a large sample of 9 and 10-year olds. Sleep disturbance was a better predictor of depression symptoms than typical sleep duration, which should be interpreted cautiously, given the limitations of the single total sleep time measure discussed below. We also found evidence that girls may be at greater risk of developing depression symptoms as a consequence of sleep disturbance, compared with boys.
Significant associations between sleep disturbance, depression, internalizing and externalizing behaviors were seen even within this sample of adolescents who are, on average, within the healthy range for these mental health scales. Identifying that sleep predicts depression symptomology one year later, in the absence of clinical disorder, is important and suggests a potential mechanism for future preventative tools. Preventing adolescent MDD is of particular importance because it is associated with a lifelong trajectory of future depression episodes 24 and multiple negative outcomes, including lower educational attainment 25 substance abuse 26 and suicide9.
Our results also show that those children with poorer mental health scores at baseline exhibited poorer scores at follow-up, which corresponds with the literature that early-emerging, sub-clinical symptoms of depression are stable and predictive of future depressive disorders, particularly in girls27. While we found little difference between boys and girls in internalizing or depression symptom scores at this young age, we identified sex differences in the relationship between sleep disturbance and depression. While sleep disturbance predicted follow-up depression symptoms in boys and girls, girls exhibited almost twice the sleep-disturbance associated increase in depression symptoms compared to boys, when controlling for baseline depression and all demographic variables. This sex-specific interaction between sleep disturbance and depression at this early age is an important finding, given that by the end of adolescence, girls are almost three times as likely to have experienced an onset of depression compared to boys 18, 28 While this sex difference in post-pubertal onset is often attributed to hormonal differences there is no conclusive evidence as to why girls are at higher risk of depression during this time. Likely, the reasons are multi-factorial and encompass social and biological domains, including direct or indirect effects on the brain of pubertal sex hormones29.
We found both types of sleep disorders, difficulties initiating and maintaining sleep, and excessive daytime somnolence, predicted future mental health symptoms. There were marginal differences between models, suggesting specific aspects of sleep disturbance may better predict depression (or other mental health disorders) in adolescence, which warrants further investigation. A large body of research has identified associations between excessive daytime somnolence and depression, largely in adults, and although the reason for this association remains unclear, it is possible that it may reflect disrupted circadian rhythm of sleep propensity30 Further research to establish whether excessive somnolence is a better predictor of adolescent depression onset, compared to sleep disturbance in general, is required. An important factor to consider when investigating sleep and depression is that given sleep issues and depression symptoms are commonly co-morbid, scales assessing depression symptomology often include sleep-related items. Thus, correlating sleep measures and depression scales may be subject to some bias. Here we found that sleep disturbance predicted two measures of depression symptomology, one that included some items related to sleep and one that did not. While disorders of excessive somnolence was the strongest predictor of follow-up depression, disorders of initiating and maintaining sleep (which overlap less with specific depressive symptoms, e.g. having a hard time getting out of bed in the morning) still predicted a similar proportion of the variance in depression symptoms, suggesting that sleep disruption plays some role in future depressive symptomology and that results are not driven by largely overlapping measures. These associations are likely complex and could reflect shared genes and/or environmental variables or could reflect parental tendencies to rather attribute emotional difficulties to over-tiredness31.
We did not find evidence to suggest that screen-time contributed to predictions of future mental health, supporting recent studies that did not find substantial negative associations between media use and well-being15 or depression 32 in older adolescents. While common public opinion is that excessive screen time has negative consequences on mental health or cognition, and some links have been identified by some14, the scientific field is relatively new and currently, findings are inconclusive. More research is required, utilizing more objective measures of screen-time, to ascertain exactly how specific aspects of screen-time behavior (e.g. social media v.s. gaming) may be related to a clinical manifestation of depression and whether it has greater consequences for those already at risk.
One major limitation of this work is the fact that youth behaviors and symptoms were ascertained from parent-report, which may be subject to shared method variance. Furthermore, the sleep disturbance and mental health measures were similar in format (health-valenced items on a Likert-type scale) which may have elicited reporter-specific response patterns that may inflate associations between measures. Reliance on parent-report is a common limitation of pediatric research and can result in either under- or over-reporting of the child’s behaviors and symptoms. Also, although analyses identified that TST was less of a predictor compared to sleep disturbance measures, several limitations exist with the current TST measure. Unlike the sleep disturbance measures, TST was estimated from a single question and was an ordinal variable that collapsed across multi-hour categories and did not distinguish between weekdays and weekends. Additional measures of sleep (both objective and more fine-grained continuous, subjective measures on weekdays and weekends), which have been added to the ABCD protocol, will be available for future analyses eliminating the need to rely solely on parent-report measures. These future annual waves of ABCD data will facilitate the exploration of how multiple measures of sleep may be differentially (or similarly) related to mental health outcomes, as discussed by others33 and will allow us to assess how short sleep and daytime somnolence could potentially share a common underlying construct such as inappropriate sleep schedules34. Finally, parent-report of family history of depression was not verified against clinical diagnosis and thus may not be entirely accurate. Despite these measurement limitations, the current work provides preliminary evidence that a modifiable behavior (sleep) predicts depression (and externalizing) symptomology early in development and prior to any clinical diagnoses, suggesting a potential preventative mechanism, which warrants future clinical investigation.
In this diverse sample, we identified race differences in TST, consistent with previous studies in children and adults: we identified that Black and multi-race children were significantly more likely to experience shorter TST, compared to White participants. Only 25% of Black participants and 35% of Hispanic participants in the sample were reported to typically achieve the recommended sleep duration for their age (9-11 hours). While one study in adults identified a genetic component to race differences in slow-wave sleep and slow-wave EEG power35, which may reflect genetic differences in brain structure, they did not find associations with sleep duration or quality. Instead, most studies that have identified poorer sleep in ethnic minorities have suggested that these differences are driven largely by health and environmental disparities between races36. While a small number of studies have reported similar disparities in children 37–39, longitudinal studies are required to establish whether differences identified in childhood are indicative of disparities than persist across the lifetime. Considering the vital role of sleep in maintaining brain plasticity, particularly during the adolescent period when vast brain developmental change occurs, and the links between poor quality sleep and negative outcomes (depression, suicide, substance use and poor academic achievement), early identification of adolescents at risk for short, or poor quality, sleep is vital. As we consider sleep as a potential tool to limit the trajectory of depression, we must also address underlying health disparities and psychosocial factors that further complicate, yet necessitate, the need to identify at-risk youth.
Furthermore, it should also be noted, that although the ABCD study is a large, nationwide study, its sample should not be considered entirely representative of US youth. While great efforts were taken to recruit typically under-represented race and socioeconomic groups and to minimize systematic sampling biases in recruitment at the school level, the sample is still skewed by several factors40. Nonetheless, the ABCD study consists of a population-based, demographically diverse sample which provides opportunities for scientific discovery that will be generalizable to a large majority of US youth. As the currently released longitudinal data does not include the full sample (n=4951 of 11,670 included for the baseline analyses) it is worth noting that that the longitudinal sample characteristics were largely consistent with the full, baseline sample (Supplementary Table 1), although there was a lower proportion of black participants and families with lower parental education. It is unlikely that these small demographic differences affected the longitudinal outcomes.
In summary, we identified cross-sectional and longitudinal relationships between sleep and mental health in a large sample of 9 and 10-year olds, in the early stages of adolescence. Although further research is required, findings suggest that sleep, as a modifiable behavior, could be targeted early in childhood to disrupt otherwise detrimental developmental trajectories that would result in an onset of depression during adolescence. The associated brain developmental processes during adolescence may offer a unique and critical window to target such interventions which warrants further investigation to address the burgeoning prevalence of adolescent depression in today’s world.
Supplementary Material
Implications and Contribution.
The incidence of depression increases markedly during adolescence, particularly for girls, and is associated with lifetime consequences. Sleep disturbance predicts depression symptoms in early adolescence, thus implicating sleep as a potential tool to limit the progression of depression and reduce the likelihood of an adolescent onset of major depressive disorder.
Acknowledgements
We thank all ABCD research assistants (specifically Maureen Gil, Leonardo Rosas, Yun Qi Lim, Vanessa Alschuler, Ellen Smith, Ingrid Durley, Teji Dulai, Quimby Lee and Rena Wang at SRI International) for their effort in collecting data for this project, and all of our research participants and their families for their continued support of the ABCD study.
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041025, U01DA041028, U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/nih-collaborators. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from https://dx.doi.org/10.15154/1503209.
Funding
This study was supported by the Adolescent Brain and Cognitive Development; grants: NIH U01DA041022-04 (SRI) and U01DA041028 (Pittsburgh). MdZ, FB, and IC have received research funding unrelated to this work from Ebb Therapeutics Inc., Fitbit Inc., and International Flavors & Fragrances Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Coefficient for the sex interaction only is reported for brevity, the full model included all covariates as listed in the methods
Conflicts of interest
None of the authors have potential conflicts of interest to be disclosed
References
- 1.Avenevoli S, et al. , Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry, 2015. 54(1): p. 37–44. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sawyer SM, et al. , The age of adolescence. Lancet Child Adolesc Health, 2018. 2(3): p. 223–228. [DOI] [PubMed] [Google Scholar]
- 3.Center for Behavioral Health Statistics and Quality, S.A.a.M.H.S.A.R.f.h.w.s.g.d., Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). 2017, Substance Abuse and Mental Health Services Administration: Rockville, MD. [Google Scholar]
- 4.Gore FM, et al. , Global burden of disease in young people aged 10-24 years: a systematic analysis. The Lancet, 2011. 377(9783): p. 2093–2102. [DOI] [PubMed] [Google Scholar]
- 5.Thapar A, et al. , Depression in adolescence. Lancet, 2012. 379(9820): p. 1056–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewinsohn PM, Rohde P, and Seeley JR, Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev, 1998. 18(7): p. 765–94. [DOI] [PubMed] [Google Scholar]
- 7.Wesselhoeft R, et al. , Major depressive disorder and subthreshold depression in prepubertal children from the Danish National Birth Cohort. Compr Psychiatry, 2016. 70: p. 65–76. [DOI] [PubMed] [Google Scholar]
- 8.Roberts RE and Duong HT, The prospective association between sleep deprivation and depression among adolescents. Sleep, 2014. 37(2): p. 239–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldstein TR, Bridge JA, and Brent DA, Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol, 2008. 76(1): p. 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weaver MD, et al. , Dose-dependent associations between sleep duration and unsafe behaviors among us high school students. JAMA Pediatrics, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knutson KL and Lauderdale DS, Sociodemographic and behavioral predictors of bed time and wake time among US adolescents aged 15 to 17 years. J Pediatr, 2009. 154(3): p. 426–30, 430.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colrain IM and Baker FC, Changes in sleep as a function of adolescent development. Neuropsychol Rev, 2011. 21(1): p. 5–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hysing M, et al. , Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open, 2015. 5(1): p. e006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lemola S, et al. , Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc, 2015. 44(2): p. 405–18. [DOI] [PubMed] [Google Scholar]
- 15.Orben A and Przybylski AK, Screens, Teens, and Psychological Well-Being: Evidence From Three Time-Use-Diary Studies. Psychol Sci, 2019. 30(5): p. 682–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gregory AM, et al. , The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep, 2009. 32(2): p. 189–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovato N and Gradisar M, A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev, 2014. 18(6): p. 521–9. [DOI] [PubMed] [Google Scholar]
- 18.Cyranowski JM, et al. , Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry, 2000. 57(1): p. 21–7. [DOI] [PubMed] [Google Scholar]
- 19.Garavan H, et al. , Recruiting the ABCD sample: Design considerations and procedures. Developmental Cognitive Neuroscience, 2018. 32: p. 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barch DM, et al. , Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Developmental Cognitive Neuroscience, 2018. 32: p. 55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bruni O, et al. , The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res, 1996. 5(4): p. 251–61. [DOI] [PubMed] [Google Scholar]
- 22.Paruthi S, et al. , Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med, 2016. 12(11): p. 1549–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Achenbach TM, Manual for the Child Behavior Checklist/4-18 and 1991 profile. University of Vermont, Department of Psychiatry, 1991. [Google Scholar]
- 24.Zisook S, et al. , Effect of age at onset on the course of major depressive disorder. Am J Psychiatry, 2007. 164(10): p. 1539–46. [DOI] [PubMed] [Google Scholar]
- 25.Franko DL, et al. , Psychosocial and health consequences of adolescent depression in Black and White young adult women. Health Psychol, 2005. 24(6): p. 586–93. [DOI] [PubMed] [Google Scholar]
- 26.Stice E, Presnell K, and Bearman SK, Relation of early menarche to depression, eating disorders, substance abuse, and comorbid psychopathology among adolescent girls. Dev Psychol, 2001. 37(5): p. 608–19. [DOI] [PubMed] [Google Scholar]
- 27.Keenan K, et al. , Subthreshold symptoms of depression in preadolescent girls are stable and predictive of depressive disorders. J Am Acad Child Adolesc Psychiatry, 2008. 47(12): p. 1433–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breslau J, et al. , Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Transl Psychiatry, 2017. 7(5): p. e1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Copeland WE, et al. , Early Pubertal Timing and Testosterone Associated With Higher Levels of Adolescent Depression in Girls. J Am Acad Child Adolesc Psychiatry, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chellappa SL, Schroder C, and Cajochen C, Chronobiology, excessive daytime sleepiness and depression: Is there a link? Sleep Med, 2009. 10(5): p. 505–14. [DOI] [PubMed] [Google Scholar]
- 31.Gregory AM, et al. , Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Arch Pediatr Adolesc Med, 2008. 162(4): p. 330–5. [DOI] [PubMed] [Google Scholar]
- 32.Heffer T and Willoughby T, The role of emotion dysregulation: A longitudinal investigation of the interpersonal theory of suicide. Psychiatry Res, 2018. 260: p. 379–383. [DOI] [PubMed] [Google Scholar]
- 33.Gregory AM and Sadeh A, Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev, 2012. 16(2): p. 129–36. [DOI] [PubMed] [Google Scholar]
- 34.Spruyt K, et al. , Odds, prevalence and predictors of sleep problems in school-age normal children. J Sleep Res, 2005. 14(2): p. 163–76. [DOI] [PubMed] [Google Scholar]
- 35.Halder I, et al. , African Genetic Ancestry is Associated with Sleep Depth in Older African Americans. Sleep, 2015. 38(8): p. 1185–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adenekan B, et al. , Sleep in America: role of racial/ethnic differences. Sleep medicine reviews, 2013. 17(4): p. 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith JP, et al. , Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health, 2019. 5(1): p. 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hale L, et al. , Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr, 2009. 30(5): p. 394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guglielmo D, et al. , Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health, 2018. 4(1): p. 68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Compton WM, Dowling G, and Garavan H, Ensuring the Best Use of Data: The Adolescent Brain Cognitive Development Study. JAMA Pediatrics, 2019. [In Press]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


