Abstract
BACKGROUND:
Fatal aortic rupture caused by esophageal foreign body (EFB), is associated with a high mortality, but can be prevented by thoracic endovascular aorta repair (TEVAR) that performed increasingly as technology improves. This study aims to investigate the cause, management and prognosis of suspected penetrating aortoesophageal foreign body injury.
METHODS:
Twelve cases who met the criteria were enrolled in this study. The demographic and clinical data were reviewed for evaluating the characteristics of EFB.
RESULTS:
Among 12 cases enrolled, 7 were males and 5 were females, with an age 27–86 years. The distance of EFB from aorta (DFA) of 7 cases were less than or equal to 0 mm, 5 cases were 0–2 mm. Eleven cases were managed with TEVAR, only one case was with open surgery standby but finally treated by flexible endoscopy (FE) successfully, without TEVAR. In group with TEVAR, EFB of 7 cases were successfully removed by rigid endoscopy (RE), and one of them was failed at the first RE treatment. EFB of 2 cases were successfully removed by open surgery with TEVAR, and other 9 cases were managed by endoscopies with TEVAR. The mean length of stay of hospitalization (LOS) and length of ICU stay of patients treated by open surgery with TEVAR (18.50±2.12 days and 5.50±0.71 days) was significantly longer than those of patients treated by endoscopy with TEVAR (7.00±2.74 days and 1.33±1.12 days, P<0.001 and P=0.001, respectively). Five cases had severe complications.
CONCLUSION:
Rational application of TEVAR can be a life-saving management for aortoesophageal foreign body injury, and jointed with endoscopy is safe and effective with a shorter length of ICU or total hospital stay.
Keywords: Aortoesophageal foreign body injury, Thoracic endovascular aorta repair
INTRODUCTION
Esophageal foreign body (EFB) impaction, which is an uncommon acquired cause of aortic injury, results in up to 1,500 deaths per year in the US.[1] Foreign bodies can be impacted, dislodged and migrated. The patients may experience serious hemorrhage at the time of esophageal perforation or at a later time in association with aortic pseudo-aneurysm (APA), aortoesophageal fistula (AEF), or even aortic dissection (AD) which are rare but life-threatening conditions.[2]
Thoracic endovascular aorta repair (TEVAR) was initially developed as a less invasive treatment for descending thoracic aortic aneurysms in patients who were unfit for conventional open surgery.[3] As improvements in endograft design and delivery devices, TEVAR was applied to other thoracic aortic pathologies, such as thoracoabdominal aortic aneurysms, or AD. Though TEVAR can greatly improve the survival rate of patients who have traumatic aortic injury by placing a stent-graft to seal the lesions and cover the fistulous track, little attention has been paid to EFB-induced aortic injury. Several reports have described successful endovascular repair of aortoesophageal foreign body injury, nevertheless, most of them are case reports.
As early as in 1967, Sloop and Thompson[4] reported an AEF case and reviewed that most of the aortic perforations occur 1 to 5 cm below the origin of the left subclavian artery, the area of closest approximation of the aorta and esophagus. Later in 1978, Nandi and Ong[5] reviewed 2,394 cases of EFB and found only two cases complicated with AEF. Unfortunately, the patients were both with rather poor prognosis. In 1985 and 1986, Bullaboy et al[6] and Schumacher et al[7] reported two children who ingested open safety pins and were found APA three and four months later but survived after open surgery, respectively. At the beginning of 21st centuries, Lam et al[8] reported a patient ingested a 3 cm fish bone and was showed arterial bleeding under flexible endoscopy (FE), but was still managed through open-surgery. Though, Zhang et al[9] pointed out that an aggressive surgical treatment without delay was still the only effective therapy for EFB-induced AEF, it was associated with high risk of morbidity and mortality; therefore, TEVAR is a much safer alternative to it.[10] Since 2005, when Chen et al[11] reported that an EFB-induced AEF case was successfully treated by TEVAR, the percentage of TEVAR has gone up in the management of aortic injury induced by EFB. Since EFB-induced aortic injury didn’t always occur at first and would be easily neglected at the initial admission, it often resulted in fatal outcome. Emergency TEVAR could protect the aorta and prevent acute rupture, which can bring more time and security for the foreign body to be removed safely.
In recent years, a joint management has been feasible and popular for suspected aortoesophageal foreign body injury including TEVAR at first to seal the aortic defect and endoscopy next to remove the EFB, depending on the advantages of less risk and more rapid recovery than open surgery. However, not all patients with suspected aortoesophgeal foreign body injury will be treated by TEVAR if the distance from the EFB to aorta (DFA) was not so close on CT scan, and those patients often had poor outcomes in the end. In this paper, we reviewed our experience during the last seven years and investigated the cause, management and prognosis of suspected penetrating aortoesophageal foreign body injury, to evaluate the critical importance of emergency TEVAR on suspected aortoesophageal foreign body injury.
METHODS
Study population
Between January 2013 and September 2019, 651 admissions due to EFB impaction were recorded in our hospital. Cases were identified by reviewing the consultation and hospitalization records with a diagnosis of EFB and confirmed by FE, rigid endoscopy (RE), or surgery. Suspected penetrating aortoesophageal foreign body injury was diagnosed when DFA was less than 2 mm between the foreign body and aortic wall seen on CT scan, or clinical symptoms and physical examination highly indicated even if DFA was more than 2 mm. After excluding 87 cases with insufficient records, 52 cases without detected EFBs under FE, RE, or surgery, 31 cases with discontinuation of treatment, 469 cases without suspected aortic injury, only 12 cases were enrolled for analysis.
Data extraction
The following records were reviewed for evaluating the characteristics of EFB, demographic and clinical data, including age, gender, basal diseases, clinical manifestations, physical examinations (PE), laboratory findings, the type, shape and size of EFB, distance of EFB from incisor (DFI), symptoms, duration of impaction (DOI), distance from the margin the EFB to aorta (DFA), managements, length of stay of intensive care unit (ICU), length of stay of hospitalization (LOS), complications and 30-day mortality. TEVAR procedures involves a stent graft system via the femoral artery and manipulated within the aorta under radiological guidance.[12] The patients were followed up at outpatient department (OPD) for six months after discharge.
Statistical analysis
Statistical analyses were performed using SPSS software (Version 21.0; IBM Corp., Armonk, NY, USA). Continuous variables were expressed as the mean±standard deviation (SD) for normally distributed and median for non-normally distributed. Statistical significance of differences was analyzed by one-way ANOVA. Categorical data were summarized as frequencies and percentages.
Ethics approval and informed consent
The study protocol was reviewed and approved by the Ethical Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University (Reference Number: 2018386). We obtained written informed content for all enrolled patients. The treatment protocols were carried out in accordance with the principles of the Helsinki Declaration.
RESULTS
Baseline parameters and their relationship
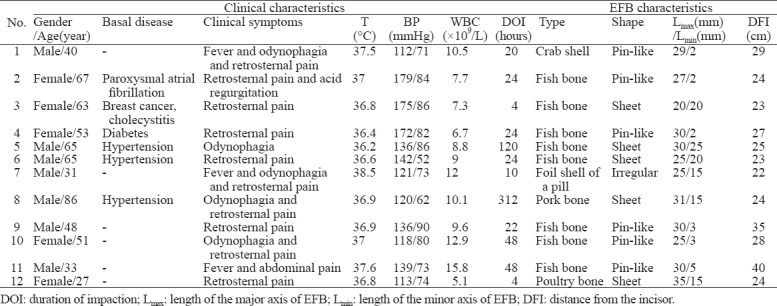
Among 12 cases enrolled, 7 were males and 5 females, with an age 27–86 years. Six patients had basal diseases. The clinical manifestations included retrosternal pain, odynophagia, fever, acid regurgitation, abdominal pain. Five cases were detected with high white blood cell (WBC) counts (≥10×109 cells). The median DOI was 24 hours (first to third quartiles: 12.5–48 hours). Five types and three shapes of EFB were included. The maximal length of EFB was 28.08±3.90 mm (range 20–35 mm). The mode and median DFI of EFB was 24 cm and 24.5 cm (first to third quartiles was 23.25–28.75 cm). Details were showed in Table 1.
Table 1.
Baseline characteristics
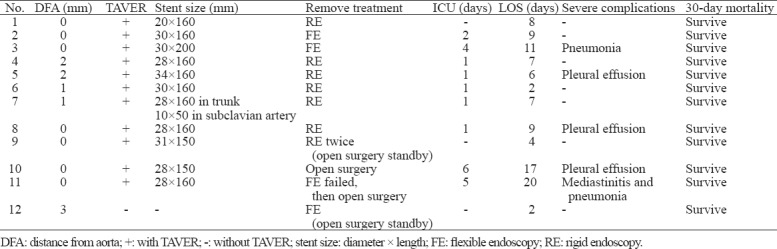
The association of EFB with aorta, management and prognosis
The DFA of 7 cases were less than or equal to 0 mm, 5 cases were 0–2 mm. Eleven cases were all managed with TEVAR, and only one case wasn’t given TEVAR (whose DFA was around 2 mm). All cases were treated by limiting oral intake and giving parenteral broad-spectrum antibiotics after the EFBs were removed. In group with TEVAR, EFBs of 7 cases were successfully removed by RE, and one of them was failed at the first RE treatment. EFB of 2 cases were successfully removed by open surgery, and one of them was failed at the first FE treatment. The one without TEVAR was treated by FE with open surgery standby. The median LOS was 7.5 days (first to third quartiles: 4.5–10.5 days). Nine cases were transported to SICU or EICU after management. The mean length of ICU stay were significantly longer in open surgery group (5.50±0.71 days) than endoscopy group (1.33±1.12 days, P=0.001). The one without TEVAR stayed only 2 days in hospital without transferred to ICU. The mean LOS of patients treated by open surgery with TEVAR (18.50±2.12 days) was significantly longer than that of patients treated by endoscopy with TEVAR (7.00±2.74 days, P<0.001). Five cases with severe complications were given strong and broad-spectrum antimicrobial therapy intravenously during the hospitalization, such as the third cephalosporin, carbapenems, and vancomucin, etc. The patients with TAVER were given oral antibiotics after discharge for at least one month to prevent infection. All patients survived with 30 days after effective treatment. Within six-month follow-up, only one patient was reexamined by CTA while other patients had regular CT or esophagram. No one got endograft infection after discharge depending on the clinical manifestations, physical examinations, lab examinations, and image examinations at OPD, and no one died during the period of six-month follow-up. Details were showed in Table 2.
Table 2.
The association of EFB with aorta, management and prognosis
Representative cases
In the following paragraphs, 2 representative cases with different etiologies, clinical manifestations, CT indications, management options, complications, will be described in details.
Case 1: TEVAR, RE, no severe complications, survive
The first case was a male patient, aged 48 years, who had no basal disease. The patient ingested a fish bone at dinner, then he swallowed a mass of steamed bun (which was seemed as a traditional way to treat EFB in the nation), making an attempt to push the fish bone into stomach, however he got retrosternal pain instantly. CT showed that a sharp foreign body perforated left wall of esophagus and penetrated the right side of aorta on the plane of the 7th thoracic vertebra (Figure 1A). TEVAR and RE with open surgery standby were planned. After emergency endovascular stent successfully placed within aorta, no obvious foreign body and no active hemorrhage were showed under RE at the first time. After repeated examination, a 30 mm ×3 mm fish bone was found at 35 cm of the esophagus from the incisor. He was discharged 4 days later with a stent in the right site of aorta (Figure 1B) and no severe complications. After 30-day and six-month follow-ups, he survived well.
Figure 1.
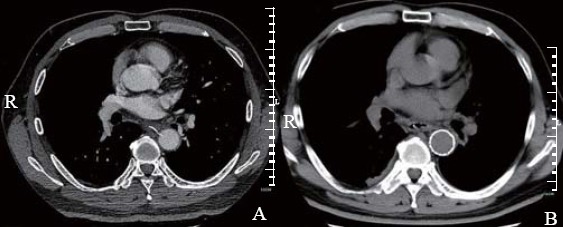
Computed tomographic images of case 1 before and after TEVAR. A: a sharp pin-like foreign body perforated left wall of esophagus and penetrated the right side of aorta on the plane of the 7th thoracic vertebra; B: a stent sealed the same site where the EFB had been.
Case 2: TEVAR, open surgery, mediastinitis and pneumonia, survive
The second case was a male patient, aged 33 years, who had no basal disease either. He felt epigastric pain right after he ate fish, and the pain intensified with fever the next day. He was then admitted by the local hospital. CT indicated that an EFB appeared in the esophagus 5 cm above the cardia of stomach, perforating the left-back wall of esophagus and penetrating the front of aortic wall. He was then transferred to our hospital, with emergency TEVAR and antibiotics therapy instantly. However, there was only a swelling area without EFB in the 40 cm of esophagus from the incisor explored by FE. Reexamined CT showed that the foreign body had pierced through the esophageal wall to the aorta. The consultation of multi-disciplinary team (MDT) prompted that the dangerous foreign body had perforated the esophagus and caused mediastinitis, aorta might rupture at any moment. Thanks to the occlusion of endovascular stent, there were still some probabilities to remove the EFB by open-surgery. Finally, it was successfully removed by surgeons and three tubes were left to drain the pus. The patient was then discharged 20 days later and survived after 30-day and six-month follow-ups.
DISCUSSION
Aortoesophageal was a catastrophic complication of EFB impaction. Since the esophagus lacks serosa and is surrounded by loose areolar connective tissue, it is vulnerable to spread of infection and erosion which would cause mediastinitis and aortic perforation easily. The ruptures of aorta rarely occur at the time of impaction, but a period of time later when AEF, APA or other fatal complications develop.[2,13]
Management selections rely on the type, size, location of EFB, extent of injury, age and comorbidities of the patients. The aims of treatment include elimination of further infection, prevention of fatal complications, restoration of esophageal continuity. Due to high morbidity and mortality rates by open surgical repair of aortic pathology,[3,14] minimally invasive approaches are increasingly used to mitigate the risk of repair, for example, TEVAR.[15] First published in 1994, TEVAR was a novel treatment modality. Recently, urgent endoscope combined with TEVAR is a valuable and popular approach to prevent severe complications and reduce the morality rate of penetrating aortoesophageal foreign body injury. However, outcomes of the technique have mixed results, it is less invasive but not widely available.[16]
Standards for TEVAR were first established in 1997.[17] According to the guideline, the complications of TEVAR can be divided into local vascular and remote systemic. Local complications are always due to the foreign body features of the graft itself, including bleeding, hematoma formation, wound or graft infection, graft thrombosis, intestinal ischemia, endoleak, graft migration, and aneurysm rupture. Remote systemic complications included myocardial infarction, organ failure, systemic infection, etc. Any death occurring within 30 days despite the cause was deemed as procedure related. Therefore, it is prudently to treat aortoesophageal foreign body by TEVAR for protection and prevention, especially when the EFB was several millimeters away from aorta on CT. Thus, a right application criteria of TEVAR was of vital importance. Nevertheless, few reports and no guidelines suggested the criteria for the use of TEVAR to treat aortoesophageal foreign body.
Wei et al[18] once put forward a classification to grade the injury of EFB-induced AEF, and the DFA was a great important index in the classification. When an EFB was visible on CT, DFA less than 2 mm suggested potential or definite AEF. In this research, DFA of all cases were less than 2 mm, 11 of them were treated with TEVAR timely, and all of them survived within 30 days. In addition, the only one case whose DFA was around 2 mm was managed by FE without TEVAR, despite open surgery stand by, and also survived. The results indicated that TEVAR was safe and effective in the cases with DFA less than 2 mm, and the value may be expected to be an indication for TEVAR at least.
Moreover, all cases in this study treated by TAVER had satisfactory short-term and long-term outcomes, which were associated not only with the rational use of antibiotics, but also with the optimal procedures to prevent fatal complications. In addition to the life-saving importance of TEVAR to prevent the threatening aortic rupture, other superiority was remarkable as well. TEVAR allowed EFB of more cases to be retrieved under endoscopy, not limited to be treated by open surgery. Grigorian et al[19] demonstrated in a study that using TEVAR had a shorter mean LOS than using open repair in blunt thoracic aortic injury. However, few study has compared the length of hospital or even ICU stay between TEVAR jointed with endoscopy and TEVAR jointed with open surgery. In the current study, the hybrid management of TEVAR and endoscopy significantly decreased the length of ICU and hospital stay compared with TAVER and open surgery. As a result, the patients could rapidly recover after minimally invasive procedures.
There were some limitations in the current study. Only 12 cases were enrolled in the final analysis, and the sample size was not large enough to increase the risk of bias. DFA of all cases were less or around 2 mm, so no conclusion could be made to the cases whose DFA were more than 2 mm.
CONCLUSION
The rational application of TEVAR can be a life-saving management for aortoesophageal foreign body injury, and jointed with endoscopy is safe and effective with a shorter length of ICU or total hospital stay. DFA less than 2 mm is an important parameter, which may be considered as a criteria for TEVAR application.
Footnotes
Funding: This work was supported by the Foundation of Key Discipline Construction of Zhejiang Province for Traditional Chinese Medicine (2017-XK-A36), and the Key Research and Development Program of Zhejiang Province (2019C03076).
Ethical approval: The study protocol was reviewed and approved by the Ethical Committee of the First Affiliated Hospital, School of Medicine, Zhejiang University (Reference Number: 2018386).
Conflicts of interest: They have no competing interests.
Contributors: YQL conceived the idea and designed experiments. WSYR collected and analyzed the data and drafted the manuscript. All authors reviewed the manuscript.
REFERENCES
- 1.Lai AT, Chow TL, Lee DT, Kwok SP. Risk factors predicting the development of complications after foreign body ingestion. Br J Surg. 2003;90(12):1531–5. doi: 10.1002/bjs.4356. [DOI] [PubMed] [Google Scholar]
- 2.Zhao XH, Lu YQ. Multiple embolisms resulted from a huge fishbone piercing the left atrium. Intensive Care Med. 2014;40(4):621–2. doi: 10.1007/s00134-014-3232-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicolaou G, Ismail M, Cheng D. Thoracic endovascular aortic repair:update on indications and guidelines. Anesthesiol Clin. 2013;31(2):451–78. doi: 10.1016/j.anclin.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Sloop RD, Thompson JC. Aorto-esophageal fistula:report of a case and review of literature. Gastroenterology. 1967;53(5):768–77. [PubMed] [Google Scholar]
- 5.Nandi P, Ong GB. Foreign body in the oesophagus:review of 2394 cases. Br J Surg. 1978;65(1):5–9. doi: 10.1002/bjs.1800650103. [DOI] [PubMed] [Google Scholar]
- 6.Bullaboy CA, Derkac WM, Johnson DH, Jennings RB Jr. False aneurysm of the aorta secondary to an esophageal foreign body. Ann Thorac Surg. 1985;39(3):275–6. doi: 10.1016/s0003-4975(10)62595-7. [DOI] [PubMed] [Google Scholar]
- 7.Schumacher KJ, Weaver DL, Knight MR, Presberg HJ. Aortic pseudoaneurysm due to ingested foreign body. South Med J. 1986;79(2):246–8. doi: 10.1097/00007611-198602000-00026. [DOI] [PubMed] [Google Scholar]
- 8.Lam EC, Brown JA, Whittaker JS. Esophageal foreign body causing direct aortic injury. Can J Gastroenterol. 2003;17(2):115–7. doi: 10.1155/2003/948232. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Liu J, Li J, Hu J, Yu F, Li S, et al. Diagnosis and treatment of 32 cases with aortoesophageal fistula due to esophageal foreign body. Laryngoscope. 2011;121(2):267–72. doi: 10.1002/lary.21366. [DOI] [PubMed] [Google Scholar]
- 10.Rawala MS, Badami V, Rizvi SB, Nanjundappa A. Aortoesophageal fistula:a fatal complication of thoracic endovascular aortic stent-graft placement. Am J Case Rep. 2018;19:1258–61. doi: 10.12659/AJCR.911441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen AP, Yu H, Li HM, Xiao XS, Liu SY. Aortoesophageal fistula and aortic pseudoaneurysm induced by swallowed fish bone:a report of two cases. Cardiovasc Intervent Radiol. 2011;34(Suppl 2):S17–9. doi: 10.1007/s00270-009-9764-7. [DOI] [PubMed] [Google Scholar]
- 12.Hanif MZ, Li D, Jabeen S, Fan Q. Endovascular repair in penetrating aortoesophageal foreign body injury. Ann Thorac Surg. 2013;96(4):1457–59. doi: 10.1016/j.athoracsur.2012.12.046. [DOI] [PubMed] [Google Scholar]
- 13.Ko SF, Lu HI, Ng SH, Kung CT. Fishbone penetration of the thoracic esophagus with prolonged asymptomatic impaction within the aorta. J Vasc Surg. 2013;57(2):518–20. doi: 10.1016/j.jvs.2012.08.067. [DOI] [PubMed] [Google Scholar]
- 14.Ouzounian M, LeMaire SA, Coselli JS. Open aortic arch repair:state-of-the-art and future perspectives. Semin Thorac Cardiovasc Surg. 2013;25(2):107–15. doi: 10.1053/j.semtcvs.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Younes HK, Davies MG, Bismuth J, Naoum JJ, Peden EK, Reardon MJ, et al. Hybrid thoracic endovascular aortic repair:pushing the envelope. J Vasc Surg. 2010;51(1):259–66. doi: 10.1016/j.jvs.2009.09.043. [DOI] [PubMed] [Google Scholar]
- 16.Hiraoka A, Chikazawa G, Tamura K, Totsugawa T, Sakaguchi T, Yoshitaka H. Clinical outcomes of different approaches to aortic arch disease. J Vasc Surg. 2015;61(1):88–95. doi: 10.1016/j.jvs.2014.06.121. [DOI] [PubMed] [Google Scholar]
- 17.Ahn SS, Rutherford RB, Johnston KW, May J, Veith FJ, Baker JD, et al. Reporting standards for infrarenal endovascular abdominal aortic aneurysm repair. Ad Hoc Committee for Standardized Reporting Practices in Vascular Surgery of The Society for Vascular Surgery/International Society for Cardiovascular Surgery. J Vasc Surg. 1997;25(2):405–10. doi: 10.1016/s0741-5214(97)70363-x. [DOI] [PubMed] [Google Scholar]
- 18.Wei Y, Chen L, Wang Y, Yu D, Peng J, Xu J. Proposed management protocol for ingested esophageal foreign body and aortoesophageal fistula:a single-center experience. Int J Clin Exp Med. 2015;8(1):607–15. [PMC free article] [PubMed] [Google Scholar]
- 19.Grigorian A, Spencer D, Donayre C, Nahmias J, Schubl S, Gabriel V, et al. National trends of thoracic endovascular aortic repair versus open repair in blunt thoracic aortic injury. Ann Vasc Surg. 2018;52:72–8. doi: 10.1016/j.avsg.2018.03.045. [DOI] [PubMed] [Google Scholar]


