Dear editor,
A recent study based on the use of experimental artificial intelligence (AI) tool showed 70%–80% accuracy in predicting development of severe disease in coronavirus disease 2019 (COVID-19) based on predictive parameters alanine aminotransferase (ALT), myalgia and hemoglobin, whilst only 5 of 53 patients developed acute respiratory distress syndrome (ARDS), 2 of whom reporting myalgia.[1] It is commonly advocated that myalgia may reflect generalized inflammation and cytokine response.[1] Multiple studies showed that myalgia is a common symptom at onset of COVID-19, seen in up to 36% of such patients.[2] Therefore, in this short article we aim to further assess whether myalgia may be a reliable predictor of severe COVID-19 disease.
A search in Medline (PubMed interface), Scopus, and Web of Science, utilizing the keywords “myalgia” AND “COVID-19” OR “Coronavirus 2019” OR “SARS-CoV-2” in all fields with no date or language restrictions was conducted. Search results were screened by title, abstract, and full text for those reporting data on prevalence of myalgia in patients developing severe or non-severe COVID-19 disease. Articles fitting the criteria with validated definition of “severe disease” (i.e., patient development of severe respiratory distress, requiring ICU admission, ventilatory support, or death) were incorporated into a pooled analysis. Computation of odds ratio (OR) and 95% confidence interval (CI) of myalgia in severe and non-severe COVID-19 disease was performed with MetaXL, software version 5.3 (EpiGear International Pty Ltd,. Sunrise Beach, Australia). Due to the limited number of studies, no risk of bias or publication bias assessment performed.
This digital search enabled the identification of 16 articles after removing duplicates, 13 of which were excluded after review of title, abstract, and full text due to being review articles (n=3), did not pertain to COVID-19 disease (n=1), did not report prevalence of myalgia (n=8), or did not specify difference in myalgia from fatigue (n=1). Six additional studies were selected using reference search. Final pooled analysis included 9 studies[3–11] with a total sample of 2,445 COVID-19 patients, 786 (32.1%) with severe disease. A total of 448 (18.3%) patients in the pooled sample presented with myalgias, 125 (19.3%) with severe COVID-19 disease and 296 (17.8%) without. Accordingly, myalgia was not found to be statistically associated with severe COVID-19 disease in any the nine individual studies, nor in our pooled analysis (OR 1.02; 95% CI 0.80–1.30; I2=12%, Cochran’s Q, P=0.33) (Figure 1).
Figure 1.
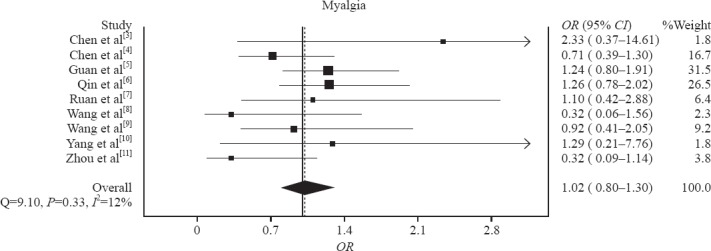
Association of myalgia with COVID-19 disease severity and mortality, odds ratio (OR) and 95% confidence interval (95% CI).
The results of this pooled analysis of the current scientific literature suggest that the presence of myalgias shall not be considered a prognostic factor for severe COVID-19 disease. It is hence unlikely that adding the efficiency of stratification models for COVID-19 may be substantially improved by adding the presence of myalgia.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: Authors have no conflicts of interest to declare.
Contributors: All authors have seen the manuscript and agreed to the content and data. All the authors played a significant role in the paper.
REFERENCES
- 1.Jiang X, Coffee M, Bari A, Wang J, Jiang X, Huang J, et al. Towards an artificial intelligence framework for data-driven prediction of coronavirus clinical severity. CMC-Computers, Materials &Continua. 2020;63(1):537–51. [Google Scholar]
- 2.Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients'clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020 Mar 12; doi: 10.1002/jmv.25757. DOI:10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunologic features in severe and moderate coronavirus disease 2019. J Clin Invest. 2020 Mar 27;:pii:137244. doi: 10.1172/JCI137244. DOI:10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019:retrospective study. BMJ. 2020 Mar 26;:368:m1091. doi: 10.1136/bmj.m1091. DOI:10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;0:null doi: 10.1056/NEJMoa2002032. Published online:February 28 2020. DOI:10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020 Mar 12;:pii:ciaa248. doi: 10.1093/cid/ciaa248. DOI:10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 Apr 6; doi: 10.1007/s00134-020-05991-x. DOI:10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020 Mar 16;:pii:ciaa272. doi: 10.1093/cid/ciaa272. DOI:10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7; doi: 10.1001/jama.2020.1585. DOI:10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China:a single-centered, retrospective, observational study. Lancet Respir Med. 2020 Feb 24; doi: 10.1016/S2213-2600(20)30079-5. pii:S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China:a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. DOI:10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


