INTRODUCTION
Identifying those at heightened risk of severe illness from novel coronavirus disease 2019 (COVID-19) is essential for modeling the disease, designing return-to-work criteria, allo-cating economic assistance, advancing health equity, and limiting morbidity and mortality. The U.S. Centers for Disease Control and Prevention has identified the criteria associated with the risk of severe complications from COVID-19 infection (Appendix Table 1, available online).1 Structural inequities have shaped racial, ethnic, and income disparities for the majority of these criteria. To date, there has been limited analysis of the proportion of the population that is at risk in the U.S. on the basis of these criteria, risk factors by race/ethnicity or income.2 Preliminary national data on cases by race/ethnicity suggest that disparities in hospitalization are already developing.3 Quantifying disparities in risk is important for allocating resources to prevent, identify, and treat COVID-19‒related severe illness and limit diverging outcomes for already vulnerable subgroups.
METHODS
The authors used data from the 2018 Behavioral Risk Factor Surveillance System, a nationally representative survey of >400,000 adults. This study estimated the proportion of adults that have at least one of the Centers for Disease Control and Prevention criteria for risk of severe illness from COVID-19 (referred to as higher risk for the remainder of this paper) (Appendix Table 1, available online) by age group, race/ethnicity, and household income (<$25,000 or not), accounting for comorbidities. In each age group, the proportion with more than 1 risk factor was also estimated, recognizing the potential for compounding risk. Prevalence ratios (PRs) and 95% CIs were estimated for race/ethnicity and income group using Poisson regression models with robust SEs. The authors excluded those who responded don't know/not sure or refused or had missing data for any risk factor except pregnancy (Appendix Tables 1 and 2, available online).
RESULTS
There were 387,304 respondents for the overall and race/ethnicity analyses and 336,861 respondents for the income analysis (Appendix Table 3, available online).
Approximately 97 million Americans (43% of adults) were at higher risk of illness from COVID-19. Among those aged <65 years, 28% were at higher risk, including 18% of the youngest age group (18–24 years).
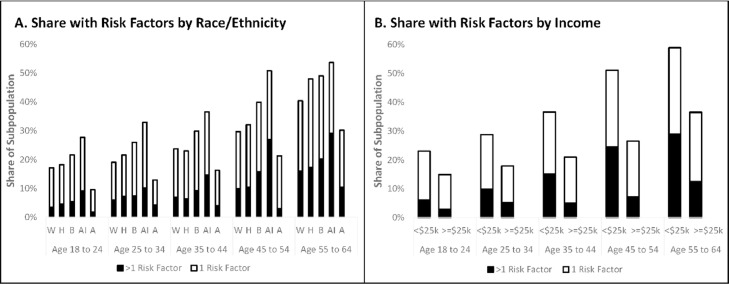
Racial/ethnic disparities in risk were found across age groups (Figure 1A ). Among those aged <65 years, 33% of black (PR=1.22, 95% CI=1.18, 1.26) and 42% of American Indian (PR=1.53, 95% CI=1.41, 1.66) adults were at higher risk relative to 27% of white adults (Appendix Table 4, available online).
Figure 1.
Disparities in prevalence of CDC risk factors for severe illness from COVID-19 by (A) race/ethnicity and (B) income.
A, Asian; AI, American Indian; B, black; CDC, Centers for Disease Control and Prevention; COVID-19, coronavirus disease 2019; H, Hispanic; W, white.
More than 40 million (18%) Americans had 2 or more risk factors. Among those aged <65 years, 11% of black (PR=1.27, 95% CI=1.19, 1.36) and 18% of American Indian (PR=2.15, 95% CI=1.84, 2.50) people had multiple risk factors relative to 8% of white people (Appendix Tables 5 and 8, available online). Among those aged ≥65 years, 69% of American Indian (PR=1.28, 95% CI=1.18, 1.38) and 61% of black (PR=1.12, 95% CI=1.08, 1.17) people had an additional risk factor(s) beyond age, relative to 54% of white adults (Appendix Table 6, available online).
At least 25 million Americans living in low-income households were at higher risk, and there were also disparities across age groups (Figure 1B). Among those aged <65 years, 40% of low-income people were at higher risk (PR=1.63, 95% CI=1.59, 1.67) relative to 24% of those with higher income (Appendix Table 7, available online). There were also income disparities in multiple risk factors among those aged <65 years (16% vs 6%, PR=2.51, 95% CI=2.38, 2.63) (Appendix Table 8, available online) and >65 years (63% vs 52%, PR=1.21, 95% CI=1.18, 1.24) (Appendix Table 9, available online).
DISCUSSION
People who are black, American Indian, or live in low-income households are more likely to have conditions associated with increased risk of illness from COVID-19 relative to those who are white or are living in higher-income households. These inequities in risk are compounded by structural disparities in access to medical insurance,4 wealth, and income volatility.5
Structural inequities also contribute to heightened exposure to COVID-19. Minorities and people living in low-income households are more likely to work in industries that have remained open during nonessential business closures.6 They are also more likely to live in crowded conditions7 and multigenerational households that may elevate exposure and limit options for quarantining family members.
It is vital that these race/ethnicity and income disparities in risk be considered in physical distancing policies and other protective measures, particularly for those who work in essential industries. Rationing resources based on comorbidities may exacerbate inequities, whereas prioritizing vaccine delivery on risks may reduce deaths and disparities.
Limitations
Data availability in the Behavioral Risk Factor Surveillance System is a limiting factor; the data do not include all risk criteria and only capture respondents who are aware of their conditions. These estimates represent a lower bound of adults at risk of severe illness. It is possible that the risk is not uniform and those with multiple factors may be at higher risk. This would be further evidence of race/ethnicity and income disparities.
ACKNOWLEDGMENTS
The authors acknowledge Professors Jonathan Levy and Patrick Kinney of the Department of Environmental Health at the Boston University School of Public Health and Lorraine Dean of the Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health for their review of the manuscript and guidance. They received no compensation for this role.
The research presented in this paper is that of the authors and does not reflect the official policy of the NIH.
This research was supported by training grant number 5T32ES014562-13 from the NIH National Institute of Environmental Health Sciences and grant number K01 MH116817 from the NIH National Institute of Mental Health.
Both authors contributed equally to all aspects of the manuscript.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2020.04.003.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.People who are at higher risk for severe illness. Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/specific-groups/people-at-higher-risk.html. Updated April 15, 2020. Accessed May 2, 2020.
- 2.Koma W, Neuman T, Claxton G, Rae M, Kates J, Michaud J. How many adults are at risk of serious illness if infected with coronavirus?San Francisco, CA: Kaiser Family Foundation.www.kff.org/global-health-policy/issue-brief/how-many-adults-are-at-risk-of-serious-illness-if-infected-with-coronavirus/. Published April 23, 2020. Accessed May 2, 2020.
- 3.Garg S, Kim L, Whitaker M. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Griffith K, Evans L, Bor J. The Affordable Care Act reduced socioeconomic disparities in health care access. Health Aff (Millwood) 2017;36(8):1503–1510. doi: 10.1377/hlthaff.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Pew Charitable Trusts . The Pew Charitable Trusts; Philadelphia, PA: 2017. How income volatility interacts with American families’ financial security. www.pewtrusts.org/-/media/assets/2017/03/incomevolatility_and_financialsecurity.pdf. Published March 2017. Accessed March 28, 2020. [Google Scholar]
- 6.BLS Reports: A profile of the working poor, 2016. U.S. Bureau of Labor Statistics.www.bls.gov/opub/reports/working-poor/2016/home.htm. Updated July 2018. Accessed March 31, 2020.
- 7.Adamkiewicz G, Zota AR, Fabian MP. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am J Public Health. 2011;101(suppl 1):S238–S245. doi: 10.2105/AJPH.2011.300119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.