Abstract
We describe a patient who presented with respiratory failure, chest pain, and fever. In the COVID-19 pandemic era, the focus was diverted to the coronavirus infection, and ST-segment elevation myocardial infarction was missed. Although we need to be vigilant in the diagnosis of COVID-19, we should not forget about the common disorders. (Level of Difficulty: Beginner.)
Key Words: acute coronary syndrome, cardiomyopathy, myocardial infarction
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; ECMO, extracorporeal membrane oxygenation; LAD, left anterior descending; LV, left ventricular; STEMI, ST-elevation myocardial infarction
Graphical abstract
We describe a patient who presented with respiratory failure, chest pain, and fever. In the COVID-19 pandemic era, the focus was diverted to the…
History of Presentation
A 56-year-old male patient presented with shortness of breath. His symptoms started 10 days before the admission. He had a virtual visit with his primary care doctor. At that visit, he described his symptoms as shortness of breath and cough associated with dull chest pain. He also reported fatigue, myalgia, and a recorded temperature of 102°F. On further questioning, he also mentioned similar episodes of chest pain in the past, with exertion. He was started on bronchodilators and antibiotics. Three days after the virtual visit with his primary care doctor, his symptoms continued to worsen, and he decided to call 911. On presentation to the hospital, he was found to be in respiratory distress.
Learning Objectives
-
•
In the COVID-19 era, vigilance for timely diagnosis, isolation, and treatment of COVID-19 patients is imperative.
-
•
However, fear should not deter us from recognizing common disorders.
Past Medical History
The patient had a history of hypertension and was taking lisinopril, 20 mg daily, and hydrochlorothiazide, 12.5 mg daily. He had a 40-pack-year smoking history. He worked in different restaurants and had exposure to a large number of people.
Differential Diagnosis
The differential diagnosis included the following: acute coronary syndrome; an infectious or inflammatory process, including coronavirus disease-2019 (COVID-19); acute respiratory distress syndrome; and pulmonary embolism.
Investigations
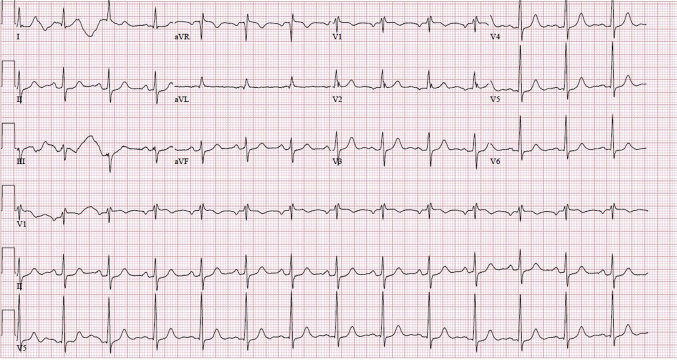
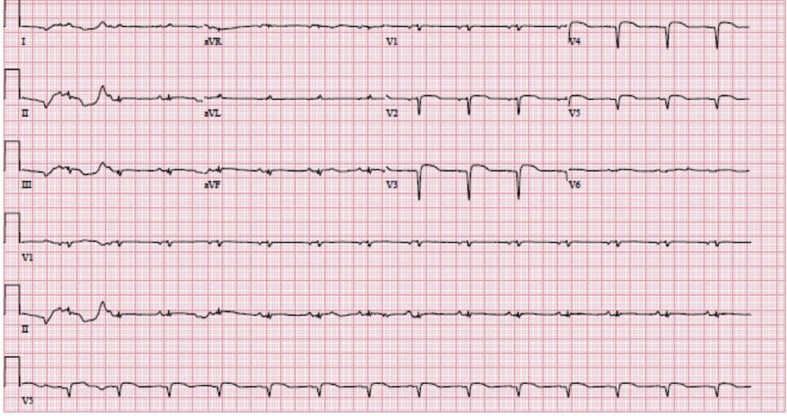
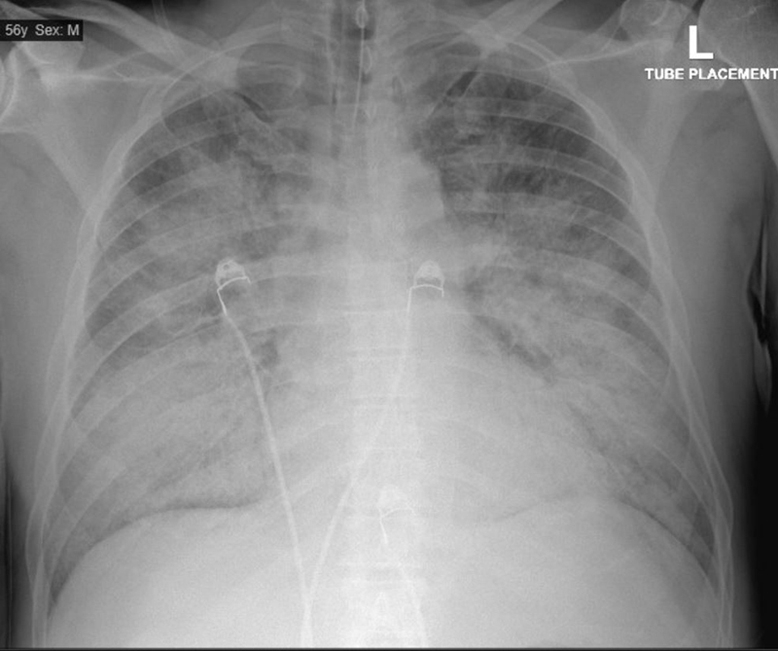
The chest radiograph showed diffuse patchy airspace opacities throughout the lungs (Figure 1). Arterial blood gas measurements on presentation showed the following: pH, 7.11; arterial partial pressure of carbon dioxide (Paco2), 66 mm Hg; arterial partial pressure of oxygen (Pao2), 50 mm Hg; and bicarbonate, 20.1 mmol/l. The patient was intubated. On 100% fraction of inspired oxygen (Fio2), arterial blood gas measurements were as follows: pH, 7.02; Paco2, 84 mm Hg; Pao2, 97 mm Hg; and bicarbonate, 21 mmol/l; with a Pao2/Fio2 ratio of 97 g. A COVID-19 polymerase chain reaction test was ordered. An electrocardiogram was done, which showed a new left bundle branch block (Figure 2), which was not present on an electrocardiogram from 2 months earlier (Figure 3). The troponin level was 56.82 ng/ml (normal range 0.00 to 0.04 ng/ml), and the B-type natriuretic peptide level was 2493 pg/ml (normal range 0 to 100 pg/ml). Echocardiography was performed, which showed severe left ventricular (LV) dysfunction with wall motion abnormalities (Figure 4, Video 1).
Figure 1.
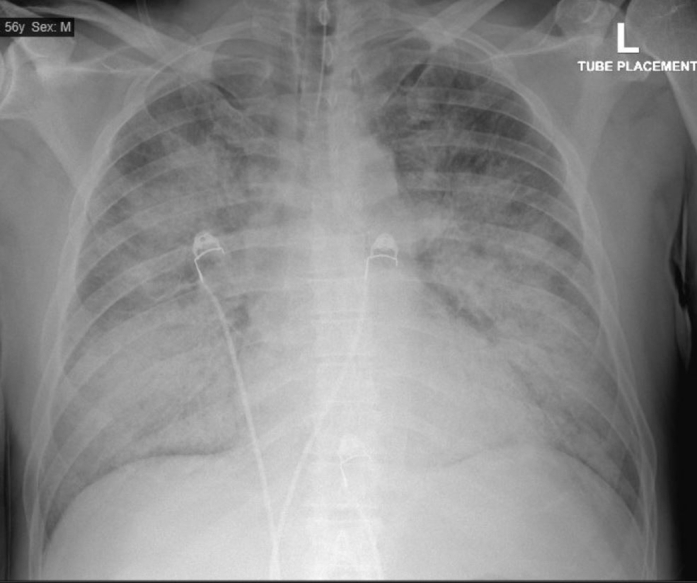
Chest Radiograph at Presentation
Chest radiograph shows diffuse patchy airspace opacities throughout the lungs, suggested as an infectious/inflammatory process such as multifocal pneumonia versus pulmonary edema or acute respiratory distress syndrome.
Figure 2.
Electrocardiogram at Presentation
The electrocardiogram at presentation shows sinus tachycardia and a left bundle branch block.
Figure 3.
Earlier Electrocardiogram
The previous electrocardiogram shows normal sinus rhythm and an incomplete right bundle branch block.
Figure 4.
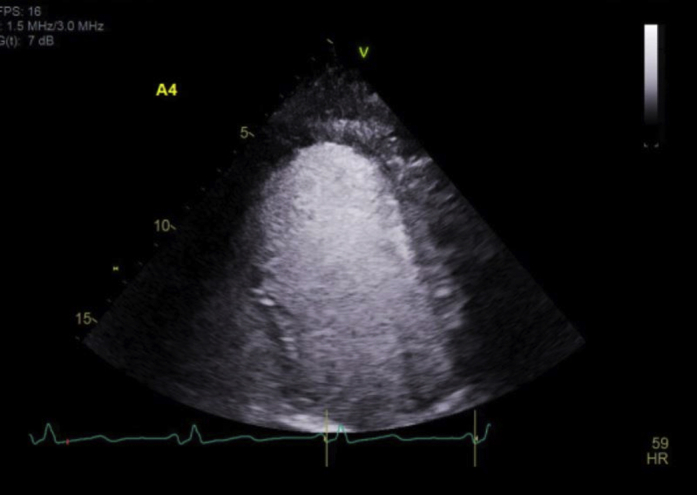
Echocardiography at Presentation
Echocardiographic still image of an apical 2-chamber view with contrast.
Online Video 1.
Echocardiography: LV Function
Echocardiographic apical 3 changer view shows severely depressed left ventricular (LV) function with wall motion abnormalities.
Management
On the basis of the patient’s symptoms on presentation and his history COVID-19 was suspected. The patient was intubated, but venovenous extracorporeal membrane oxygenation (ECMO) was soon considered on an emergency basis. The troponin elevation was considered a manifestation of myocarditis. Norepinephrine and vasopressin were started for hypotension. Venovenous ECMO placement was complicated by right ventricular rupture with worsening hypotension. Consequently, the patient underwent emergency placement of peripheral venoarterial ECMO followed by repair of the right ventricle and placement of a central LV vent to decompress the left ventricle. The patient was then transferred to our institution for a higher level of care. The COVID-19 polymerase chain reaction result was negative twice by this time. After arrival at our institution, he was taken to the cardiac catheterization laboratory. A coronary angiogram showed severe 99% stenosis of the mid–left anterior descending (LAD) artery with Thrombolysis In Myocardial Infarction (TIMI) flow grade 2, 60% long-segment stenosis in the proximal left circumflex artery, and a moderately diffusely diseased right coronary artery (Figures 5, 6, and 7, Videos 2, 3, and 4).
Figure 5.
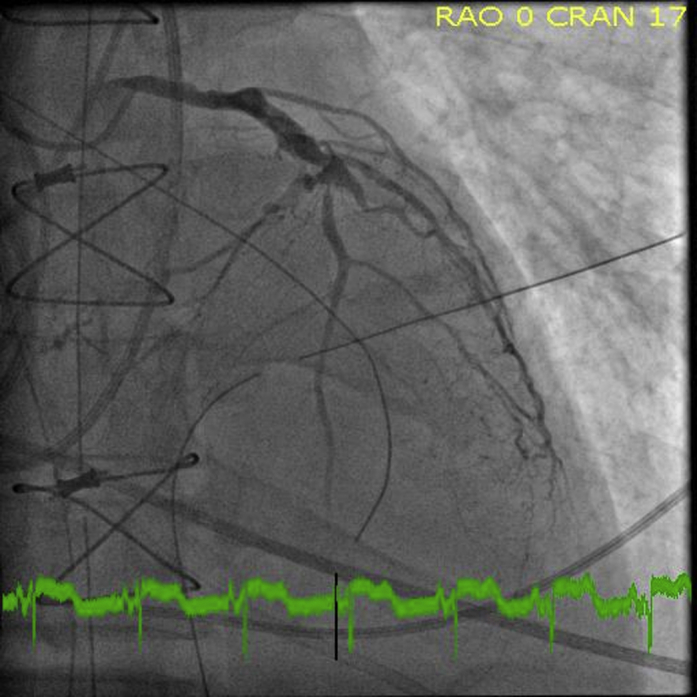
Angiography: LAD and LCX
Coronary angiogram right anterior oblique (RAO) 0, cranial (CRAN) 17 view, shows 99% stenosis of the mid–left anterior descending artery (LAD), 60% long segment stenosis in the proximal left circumflex artery (LCX) with the severe diffuse disease in the distal artery.
Figure 6.
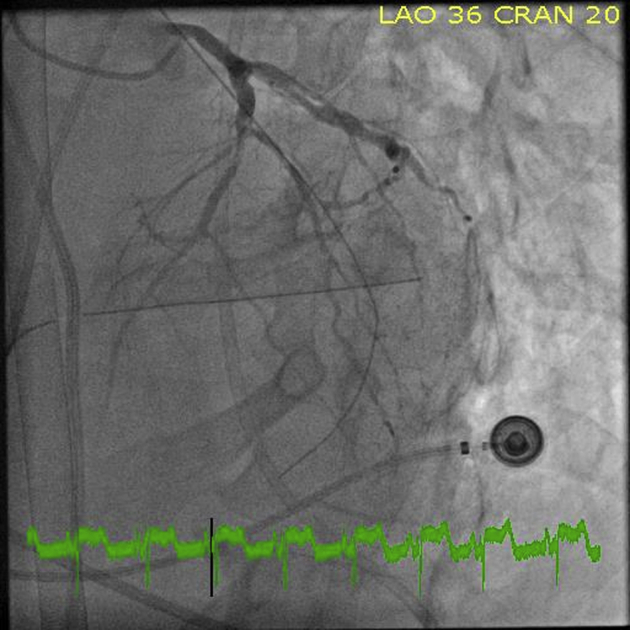
Angiography: LAD and LCX
Coronary angiogram left anterior oblique (LAO) 36, cranial (CRAN) 20 view, shows 99% stenosis of the mid–left anterior descending artery (LAD), 60% long segment stenosis in the proximal left circumflex artery (LCX) with the severe diffuse disease in the distal artery.
Figure 7.
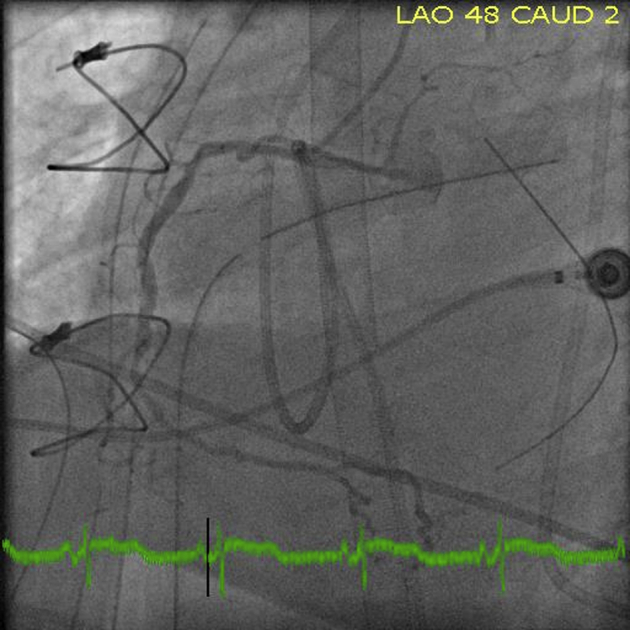
Angiography: RCA
Coronary angiogram left anterior oblique (LAO) 48, caudal (CAUD) 2 view shows moderately diffusely diseased right coronary artery (RCA).
Online Video 2.
Angiography: LAD and LCX
Coronary angiogram right anterior oblique 0, cranial 17 view, shows 99% stenosis of the mid–left anterior descending artery (LAD) with Thrombolysis In Myocardial Infarction 2 (TIMI2) flow, 60% long segment stenosis in the proximal left circumflex artery (LCX) with the severe diffuse disease in the distal artery, totally occluded third obtuse marginal artery.
Online Video 3.
Angiography: LAD and LCX
Coronary angiogram left anterior oblique 36, cranial 20 view, shows 99% stenosis of the mid–left anterior descending artery (LAD) with Thrombolysis In Myocardial Infarction 2 (TIMI2) flow, 60% long segment stenosis in the proximal left circumflex artery (LCX) with the severe diffuse disease in the distal artery, totally occluded third obtuse marginal artery.
Online Video 4.
Angiography: RCA
Coronary angiogram left anterior oblique 48, caudal 2 view shows moderately diffusely diseased right coronary artery (RCA).
Discussion
In December 2019, an outbreak of pneumonia caused by a novel coronavirus occurred in Wuhan, China (1). The virus was identified as severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), which leads to COVID-19 (2). Even though the primary manifestation of COVID-19 consists of respiratory symptoms, some patients have severe cardiovascular damage (3). Patients with cardiovascular disease have an increased risk of death. Cardiovascular manifestations of patients with COVID-19 include heart failure, myocarditis, arrhythmia, and elevated troponin, which can mimic STEMI or non–ST-segment elevation myocardial infarction. In Wuhan, out of 72,312 patients, 81% had mild symptoms, 13.9% had severe symptoms requiring oxygen, and 4.7% were critically ill needing care in the intensive care unit (4). In a case series from Zhongnan Hospital of Wuhan University, the manifestation of myocardial injury included 8.7% shock, 16.7% arrhythmia, and 7.2% acute cardiac injury (5). In another series (6), 6% of the COVID-19–positive patients presented with ventricular tachycardia or ventricular fibrillation, and 27.8% had myocardial injury ascertained by elevated troponin levels.
The COVID-19 pandemic has undoubtedly alerted the cardiology community to the cardiovascular manifestations of COVID (5). The vigilance and precautions needed for patients suspected of having COVID-19 in no way should be relaxed, but fear should not preclude us from delivering appropriate care. For example, in the case of the patient we presented, before the COVID-19 era, he most likely would have been referred for a further evaluation immediately. The patient has significant risk factors for coronary artery disease, with a history suggestive of chronic angina; therefore, further investigations were warranted. In the COVID-19 era, the hesitation of patients to go to the hospital to avoid exposure, the reservation of providers to send their patients to health care facilities, and the limitation of resources have created significant barriers for evaluation. Even in the case of patients who are already admitted to the hospital, when the suspicion of COVID-19 is raised, it can affect care either by distracting providers from other diagnoses or by delaying procedures to avoid exposure. For example, in this case, while the patient was being considered for ECMO, an angiogram should have been performed, with proper protection.
Recently, the neurology community released a plea to the public not to ignore symptoms of a stroke. We also send out a plea to the cardiology community to do the same and to be vigilant about the common cardiac-related diagnosis that we may mislabel in the COVID-19 era.
Follow-Up
Because the patient had completed the LAD artery infarct (Figure 8), the decision was made against LAD artery revascularization. The patient was taken to the operating room, an Impella 5.5 device (Abiomed, Danvers, Massachusetts) was placed through the axillary artery, and the patient was weaned from ECMO successfully. Currently, he remains in the intensive care unit and is recuperating from an arduous journey to be able to be considered for options of potential revascularization (after proven viability) or LV assist device placement (if he cannot be weaned from the Impella device) versus cardiac recovery (if he is able to be weaned from the Impella device successfully).
Figure 8.
Follow-Up Electrocardiogram
The follow-up electrocardiogram shows normal sinus rhythm and an anterior infarct.
Conclusions
We have presented the case of a 56-year-old man with risk factors for coronary artery disease who presented with STEMI. In the COIVD-19 era, the diagnosis was diverted toward COVID-19, and STEMI was missed. COVID-19 patients can present with cardiovascular manifestations. We have to be vigilant in diagnosing COVID-19 patients; however, we should not forget about the common diagnosis. The appropriate diagnostic tests and care should be delivered to patients who are suspected of having COVID-19, with the proper precautions taken.
Footnotes
Dr. Bhimaraj has reported consulting for Abbott and Abiomed. Dr. Yousefzai has reported that he has no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, or patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061-9. [DOI] [PMC free article] [PubMed]
- 2.Zhou P., Yang X.L., Wang X.G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CCA-ACC: Communication Conference of COVID-19-American College of Cardiology COVID 19 Conference, March 18, 2020, Part 2. Available at: https://www.acc.org/∼/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/Latest%20in%20Cardiology/COVID19-Hub/acc-cca-covid19-webinar-transcript-march-18-epidemiology-cvd-treatment-and-management.pdf. Accessed May 2020.
- 6.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcome of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1–8. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]