Abstract
Introduction: Primary leiomyosarcomas (LMS) of the mediastinum are extremely rare malignant mesenchymal tumors developing from soft tissues or great vessels. We present a case of a primary leiomyosarcoma of the middle mediastinum in which long-term survival was achieved.
Case Report: A 77-year-old man presented to us for examination with an extrapleural sign in his upper mediastinum on chest X-ray. Computed tomography (CT) revealed a well-circumscribed mass in the middle mediastinum. Thoracoscopic resection of the mediastinal tumor and immunohistological findings, which were positive for smooth muscle actin (SMA), HHF-35, vimentin, and desmin confirmed primary leiomyosarcoma. It recurred twice with solid right pulmonary metastases, which were resected. He was followed-up for a total of 9 years and 6 months from the first surgery with no signs of recurrence after his last surgery.
Conclusion: Surgical resection of both the primary tumor and pulmonary metastases remains the mainstay of treatment of primary leiomyosarcomas.
Keywords: mediastinal tumor, leiomyosarcoma, pulmonary metastasis
Introduction
Primary leiomyosarcomas (LMS) of the mediastinum are extremely rare malignant mesenchymal tumors, which may develop from soft tissues of the mediastinum or great vessels. Mediastinal sarcomas including LMS account for 1.4% of soft tissue sarcomas1) and about 3%–4% of mediastinal neoplasms.2,3) Moreover, LMS accounts for 6.5% of malignant soft tissue tumors4) with mediastinal LMS accounting for 0.15% of all mediastinal tumors and 11% of primary mediastinal sarcomas.1) In addition, mediastinal LMS have poor prognosis. To our knowledge, prior to this report, no cases of 5-year survival were reported in Japan. We present a rare case of LMS of the middle mediastinum in which long-term survival was achieved following three surgeries.
Case Report
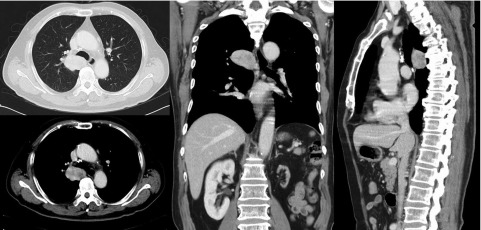
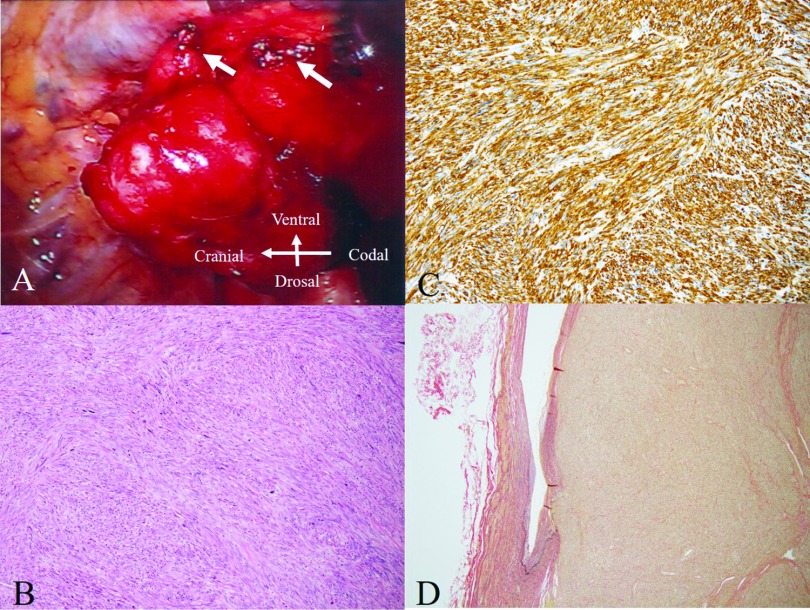
A 77-year-old man who presented to our division for medical examination had an extrapleural sign in his upper mediastinum on chest X-ray. He had a history of hypertension, dyslipidemia, and prostate cancer. He had no respiratory symptoms and physical examination was unremarkable. Laboratory tests for tumor markers including carcinoembryonic antigen, squamous cell carcinoma antigen, and pro-gastrin-releasing peptide were within the normal ranges. Computed tomography (CT) of the chest (Fig. 1) and magnetic resonance imaging (MRI) revealed a well-circumscribed mass measuring 4.8 × 2.9 cm with a relatively high contrast in the middle mediastinum that extended from the dorsal side of trachea to the right main bronchus and from the 5th to the 6th vertebral bodies. A whole body scan using 2-deoxy-2-[18F]-fluorodeoxyglucose-positron emission tomography (FDG-PET)/CT demonstrated a maximum standardized uptake value of 3.17 during the early phase and 3.11 during the late phase only by the mediastinal tumor. A bronchoscopy revealed that the respiratory tract was compressed from the dorsal side by the tumor, which seemed to be a benign tumor; however, we were unable to reach a definitive diagnosis. A thoracoscopic resection of the mediastinal tumor was performed afterward for diagnosis and treatment. The tumor surface was smooth and it sparsely adhered to the lung. Since we were unable to detect the origin of the tumor and the continuous code from the ventral side of the tumor to the dorsal side of the superior vena cava was observed, a complete resection was performed (Fig. 2A). A frozen section analysis revealed a spindle cell tumor. However, it was difficult to determine whether it was benign or malignant. Macroscopically, the tumor was white, well-defined, and solid. Histopathological findings revealed moderate to high atypia in the irregular fascicles of the spindle cells (Fig. 2B), partial hemorrhage, and necrosis. Mitosis was 3 to 5/high power field (HPF). LMS was confirmed based on the immunohistological findings, which were positive for smooth muscle actin (SMA) (Fig. 2C), HHF-35, vimentin, and desmin and negative for CD34, S-100, CAM5.2, and AE1/AE3. Since the tumor involved destroying a relatively thick vein, it was suspected to originate from blood vessels (Fig. 2D). After the initial surgery, LMS recurred with solid pulmonary metastasis twice after 3 years and 8 months and again after 4 years and 6 months from the initial surgery. Partial pulmonary resection and basal segmentectomy of the right lung was performed each time. The patient was followed-up for a total of 9 years and 6 months from the first surgery with no signs of recurrence from the last surgery.
Fig. 1. Radiologic findings. CT scan showing a well-circumscribed mass measuring 48 × 29 mm with a relatively high contrast in the middle mediastinum extending from the dorsal side of trachea to the right main bronchus and from the 5th to the 6th vertebral body. CT: computed tomography.
Fig. 2. Intra-operative findings and microscopic findings. (A) The tumor surface is smooth and the continuous code from the ventral side of the tumor to the dorsal side of the superior vena cava is observed (white arrows). (B) Histopathological findings show moderate to high atypia in the irregular fascicles of the spindle cells, partial hemorrhage, and necrosis. Hematoxylin and eosin staining. Magnification, × 10. (C) Tumor cells are positive for SMA. Immunohistochemical staining for SMA. Magnification, × 20. (D) The tumor involves destroying a relatively thick vein, suggesting that it originates from blood vessels. Verhoeff–Van Gieson elastic staining. Magnification, × 4. SMA: smooth muscle actin.
Discussion
LMS of the mediastinum is an extremely rare tumor with only 19 cases reported in Japan including our case (Table 1).5–12) The patients’ ages ranged from 34 to 84 years (mean: 63.4 years) of which 10 were females and 9 were males. Reports included three lesions in the anterior, four in the superior, seven in the middle, and five in the posterior mediastinum. The tumor sizes ranged from 4.0 to 21.0 cm (mean: 9.6 cm). Surgery was the primary treatment in 13 patients. In total, six patients were deemed inoperable. The tumors originated from great vessels including the superior vena cava in 4 patients, while the origin was unknown in the remaining 15 patients. A total of nine patients were treated by surgical resection alone with one patient receiving chemoradiation therapy in addition to surgery, two patients receiving radiotherapy either before or after surgery, and one receiving chemotherapy after surgery. Whereas four patients received chemotherapy and/or radiotherapy for their primary treatment and two patients opted for best supportive care following their diagnosis.
Table 1. Case reports of mediastinal leiomyosarcoma in Japan.
| No. | Age (years) | Sex | Site | Origin | Treatment for primary site | Size of tumor (cm) | Metastasis | Observation period (months) | Prognosis | Reference | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ope | CTx | RTx | ||||||||||
| 1 | 47 | F | A | Unknown | + | + | + | 7.0 | PUL | 6 | A | 5 |
| 2 | 63 | F | A | Unknown | − | + | − | 8.2 | PUL | 18 | A | 6 |
| 3 | 73 | F | S | Lt. BCV? | + | + | − | 5.0 | HEP, OTH | 28 | A | 5 |
| 4 | 62 | F | P | Unknown | + | + | − | 8.0 | − | 12 | A | 5 |
| 5 | 79 | F | P | Unknown | − | − | − | 12.0 | HEP, ADR, LYM | 3 | D | 7 |
| 6 | 69 | F | M | Unknown | + | − | − | 20.0 | n/a | n/a | n/a | 5 |
| 7 | 60 | F | M | Unknown | + | − | − | 11.9 | − | 8 | D | 8 |
| 8 | 74 | F | M | Unknown | − | − | + | 5.0 | BRA | 5 | D | 9 |
| 9 | 83 | F | M | Unknown | − | − | − | 6.0 | ADR | 2 | D | 10 |
| 10 | 66 | F | M | Unknown | + | − | − | 21.0 | − | 3 | A | 11 |
| 11 | 67 | M | A | Unknown | + | − | + | 10.0 | − | 12 | A | 5 |
| 12 | 66 | M | S | Unknown | + | − | + | 6.5 | − | 16 | A | 12 |
| 13 | 34 | M | S | SVC? | − | + | − | n/a | PUL, BRA | 42 | A | 5 |
| 14 | 72 | M | S | Unknown | + | − | − | 4.0 | − | 6 | A | 5 |
| 15 | 74 | M | P | ICA? | + | − | − | 12.0 | − | 6 | A | 5 |
| 16 | 34 | M | P | Unknown | + | − | − | 15.5 | PUL | 12 | D | 7 |
| 17 | 70 | M | P | Unknown | + | − | − | 6.5 | − | 13 | A | 7 |
| 18 | 35 | M | M | Unknown | − | + | + | n/a | − | 6 | D | 5 |
| 19 | 77 | M | M | Vein | + | − | − | 4.8 | PUL | 114 | A | Present case |
Ope: operation; CTx: chemotherapy; RTx: radiotherapy; PUL: pulmonary; BRA: brain; HEP: hepatic; ADR: adrenal; LYM: lymph node; OTH: other organ; A: anterior; M: middle; S: superior; P: posterior; Lt. BCV: left branchiocephaliv vein; SVC: superior vena cava; ICA: intracostal artery; n/a: not available; A: alive; D: dead
Although the prognosis of mediastinal LMS is unknown, an analysis by Burt and colleagues1) of 47 cases of patients with primary mediastinal sarcomas including five with LMS revealed a median survival of 13 months with a 5-year overall survival of 32%. In that series, the five patients with LMS were classified as having high-grade tumors was based on cellular differentiation, the degree of tumor cellularity and vascularity, amount of necrosis, and the number of mitoses. The 5-year survival rate among those was 27%. Complete resection was reported to be the most significant factor correlating with survival in patients with LMS.1,11–13) Additionally, a recent metaanalysis revealed the efficacy of adjuvant chemotherapy with doxorubicin and ifosfamide in those patients.14) In our case, we performed complete resection of the primary lesion; however, the patient did not receive adjuvant chemotherapy.
The lung is the most frequent site of metastasis from soft tissue sarcomas with complete surgical resection being the most consistent predictor of long-term survival in these patients.15) In Japan, out of 19 reported cases, 8 had metastases synchronous or metachronous to various organs with pulmonary metastases noted in 5 cases.
Chemotherapy should be considered in cases where complete resection cannot be performed. In metastatic cases, doxorubicin is the only drug with an established efficacy as a single agent.16) Recently, newly developed drugs including pazopanib,17,18) trabectedin,19) and eribulin20) have attracted attention for the treatment of soft tissue sarcomas. Although there are no reports on their use for the treatment of mediastinal sarcomas, similar outcomes are expected. Complete resection is important for treatment of both the primary lesion of the mediastinal LMS and lung metastasis. A better prognosis is expected with complete resection. Our case had a long-term survival of 9 years and 6 months despite the recurrence of solid lung metastases twice following the initial resection of the primary lesion. This suggests that long-term survival can be achieved with complete resection despite the recurrence of pulmonary metastases.
Conclusion
Mediastinal LMS is an extremely rare neoplasm. Complete surgical resection of the primary tumor is a significant prognostic factor. Despite limited data on the management of mediastinal LMS, surgical resection of solid pulmonary metastases remains the mainstay of treatment.
Consent
A written informed consent was provided by the patient for publication of this report.
Disclosure Statement
The authors report no conflicts of interest.
Acknowledgment
We would like to thank Dr. Yu Nishimura of Division of Pathology at Saitama Cancer Center for her valuable input.
References
- 1).Burt M, Ihde JK, Hajdu SI, et al. Primary sarcomas of the mediastinum: results of therapy. J Thorac Cardiovasc Surg 1998; 115: 671-80. [DOI] [PubMed] [Google Scholar]
- 2).Shields TW, Robinson PG. Mesenchymal tumors of the mediastinum. In: Shields TW, LoCiero J, Ponn RB, Rusch VW.eds.; General thoracic surgery. 7th ed Philadelphia: Lippincott Williams & Wilkins, 2009; pp 2473-97. [Google Scholar]
- 3).Silverman NA, Sabiston DC. Mediastinal masses. Surg Clin North Am 1980; 60: 757-77. [DOI] [PubMed] [Google Scholar]
- 4).Ogura K, Higashi T, Kawai A. Statistics of soft-tissue sarcoma in Japan: report from the bone and soft tissue tumor registry in Japan. J Orthop Sci 2017; 22: 755-64. [DOI] [PubMed] [Google Scholar]
- 5).Abe M, Okashiwa H, Takeoka T. A case of mediastinal leiomyosarcoma with recurrent metastases. J Jpn Surg Assoc 2001; 62: 2644-7. (in Japanese) [Google Scholar]
- 6).Ono K, Takeda T, Fujinami M, et al. A case of anterior mediastinal leiomyosarcoma with multiple lung metastases and bone metastasis treated by chemotherapy. AJRS 2013; 2: 742-5. (in Japanese) [Google Scholar]
- 7).Abiko T, Sato S, Futamata T, et al. A case of pleomorphic leiomyosarcoma of the posterior mediastinum. J Jpn Assoc Chest Surg 2005; 19: 819-22. (in Japanese) [Google Scholar]
- 8).Hirano H, Kizaki T, Sashikata T, et al. Leiomyosarcoma arising from soft tissue tumor of the mediastinum. Med Electron Microsc 2003; 36: 52-8. [DOI] [PubMed] [Google Scholar]
- 9).Shundo Y, Takahashi T, Itaya T, et al. [Leiomyosarcoma of the middle mediastinum; report of a case]. Kyobu Geka 2011; 64: 603-5. (in Japanese) [PubMed] [Google Scholar]
- 10).Yoshida M, Ando S, Naito Y, et al. Mediastinal leiomyosarcoma concurrent with intra-aortic thrombosis. BMJ Case Rep 2013; pii: bcr2012007527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Chen F, Muranishi Y, Minakata K, et al. Complete resection of a giant mediastinal leiomyosarcoma. Ann Thorac Surg 2015; 99: e69-71. [DOI] [PubMed] [Google Scholar]
- 12).Iwata T, Miura T, Inoue K, et al. Primary leiomyosarcoma of the anterior mediastinum encasing the aortic arch, left common carotid and left subclavian arteries. Ann Thorac Cardiovasc Surg 2012; 18: 140-3. [DOI] [PubMed] [Google Scholar]
- 13).Moran CA, Suster S, Perino G, et al. Malignant smooth muscle tumors presenting as mediastinal soft tissue masses. A clinicopathologic study of 10 cases. Cancer 1994; 74: 2251-60. [DOI] [PubMed] [Google Scholar]
- 14).Pervaiz N, Colterjohn N, Farrokhyar F, et al. A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer 2008; 113: 573-81. [DOI] [PubMed] [Google Scholar]
- 15).Billingsley KG, Burt ME, Jara E, et al. Pulmonary metastases from soft tissue sarcoma: analysis of patterns of diseases and postmetastasis survival. Ann Surg 1999; 229: 602-10; discussion 610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).van der Graaf WT, Blay JY, Chawla SP, et al. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet 2012; 379: 1879-86. [DOI] [PubMed] [Google Scholar]
- 17).Bramwell VH, Anderson D, Charette ML, et al. Doxorubicin-based chemotherapy for the palliative treatment of adult patients with locally advanced or metastatic soft tissue sarcoma. Cochrane Database Syst Rev 2003; CD003293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Nakamura T, Matsumine A, Kawai A, et al. The clinical outcome of pazopanib treatment in Japanese patients with relapsed soft tissue sarcoma: a Japanese musculoskeletal oncology group (JMOG) study. Cancer 2016; 122: 1408-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Demetri GD, von Mehren M, Jones RL, et al. Efficacy and safety of trabectedin or dacarbazine for metastatic liposarcoma or leiomyosarcoma after failure of conventional chemotherapy: results of a phase iii randomized multicenter clinical trial. J Clin Oncol 2016; 34: 786-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Schöffski P, Chawla S, Maki RG, et al. Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: a randomised, open-label, multicentre, phase 3 trial. Lancet 2016; 387: 1629-37. [DOI] [PubMed] [Google Scholar]