Abstract
Objective
The study evaluated the adherence to the guidelines for surgical antimicrobial prophylaxis in a Saudi tertiary care hospital.
Methods
The medical records of 707 patients from the surgical units over a selected 3-month period were selected. The data were reviewed and statistically analysed.
Results
Of the 707 respondents, 51.2% were women and most were older than 50 years. The most common surgical procedures involved orthopaedics (28.3%), followed by vascular surgery (15.1%). One hundred and thirty-eight (19.5%) patients received antibiotics according to the guidelines for surgical prophylaxis. More than half of the patients (399/56.4%) received antibiotics for more than 24 h and 129 (18.2%) received antibiotics for less than 24 h. Single dose antibiotic therapy was used in 179 (25.3%) patients. Two hundred and ninety-seven (42%) patients underwent clean surgery, 284 (40%) clean-contaminated and 128 (18%) contaminated surgery. A significant difference was evident between the antibiotics administered according to the recommended guidelines and the duration of antibiotic therapy (p = 0.001), duration (p = 0.001) and the type of surgical procedure (p = 0.00).
Conclusion
The findings of this study suggest that healthcare professionals do not strictly adhere to the guidelines for surgical antibiotic prophylaxis. Physicians are therefore encouraged to follow the recommendations appropriately and to regularly implement surgical antimicrobial prophylaxis for patient safety.
Keywords: Antimicrobial prophylaxis, Guidelines, KSA, Surgery, Orthopaedics
الملخص
أهداف البحث
تهدف هذه الدراسة لتقييم الالتزام بالقواعد الإرشادية في استخدام المضادات الحيوية الوقائية قبل العمليات الجراحية في أحد مستشفيات الرعاية المتقدمة (الثالثة) في المدينة المنورة بالمملكة العربية السعودية.
طرق البحث
تم في هذا الدراسة جمع بيانات جميع المرضى (٧٠٧ مريضا) الذين أجريت لهم عمليات جراحية مختلفة في أحد مستشفيات الرعاية الثالثة بالمدينة المنورة، وذلك خلال فترة الدراسة، التي استمرت لمدة ثلاثة أشهر.
النتائج
من بين ٧٠٧ مريضا شملتهم الدراسة، كان ٥١.٢٪ من الإناث ومعظمهم أكبر من ٥٠ سنة. كانت أكثر العمليات الجراحية شيوعا هي جراحات العظام (٢٨.٣٪)، وجراحات الأوعية الدموية (١٥.١٪). تلقى ١٣٨ (١٩.٥٪) من المرضى المضادات الحيوية وفقا للقواعد الإرشادية. فيما يتعلق بمدة استخدام المضادات الحيوية، تلقى أكثر من نصف المرضى (٣٩٩، ٥٦.٤٪) المضادات الحيوية لأكثر من ٢٤ ساعة. بالإضافة إلى ذلك، تلقى ١٧٩ (٢٥.٣ ٪) جرعة واحدة، في حين أن ١٢٩ (١٨.٢٪) فقط تلقى المضادات الحيوية لمدة تقل عن ٢٤ ساعة. فيما يتعلق بتصنيف الجروح الجراحية، خضع٢٩٧ مريض لعمليات جراحية نظيفة (٤٢٪)، و٢٨٤ مريضا (٤٠٪) لعمليات جراحية نظيفة-ملوثة، و١٢٨ (١٨٪) لعمليات جراحية ملوثة. وجد أن هناك اختلاف واضح بين استخدام المضادات الحيوية بناء على القواعد الإرشادية ومدة استخدام المضادات الحيوية، والإطار الزمني، ونوع العملية الجراحية.
الاستنتاجات
تشير نتائج الدراسة إلى أن ممارسي الرعاية الصحية أخفقوا في الالتزام الصارم بالسياسات الخاصة باستخدام المضادات الحيوية الوقائية في العمليات الجراحية. لذلك يلزم تشجيع الأطباء على اتباع التوصيات والحرص على الاستمرار في تطبيق القواعد الإرشادية عند استخدام المضادات الحيوية الوقائية في العمليات الجراحية.
كلمات المفتاحية: المضادات الوقائية, القواعد الإرشادية, المملكة العربية السعودية, الجراحة, جراحة العظام
Introduction
Healthcare-associated infections, such as surgical site infections (SSIs), are associated with increased morbidity and mortality globally.1 Surgical antimicrobial prophylaxis (SAP) refers to the practice of using antibiotics to stop infections at the surgical site. SAP is executed by providing a sufficient amount of the antibiotic to the tissues before surgery.2,3 The American Society of Health-System Pharmacists (ASHP) has published therapeutic guidelines designed to help reduce or control the incidences of morbidity and mortality associated with SSIs,4, 5, 6, 7, 8 with an emphasis on supporting suitable antibiotic selection and the timing and duration of SAP.
Previous reports revealed that failure to adhere to a medication schedule leads to substantial harm in patients and increases the incidence of antimicrobial resistance in special populations, such as patients who have had surgery.7, 8, 9, 10 SSIs have been linked to extended hospital stay following surgery and increased medical costs for the patient and in clinical settings.9,10
According to ASHP clinical practice guidelines regarding antimicrobial prophylaxis in surgery,9 the best time to administer preoperative antibiotic is within 60 min of surgical procedures, with the dose and selection of antibiotic made on the basis of body type (obese, normal or underweight) and observance of the recommended repeat doses during prolonged procedures.11, 12, 13 The guidelines also recommend shortened postoperative use of antibiotics, with a single dose or continuous use for less than 24 h.9 Adult and paediatric patients undergo a variety of surgical procedures that depend on the chronic disease conditions. These surgical procedures require antimicrobial prophylaxis to reduce SSI-related morbidity and mortality, and to decrease the duration and cost of health care. First- and second-generation cephalosporins are most commonly recommended for adult patients, while the use of vancomycin is strongly recommended for patients with allergies to beta (β)-lactam antibiotics,14,15 although penicillin and a β-lactamase inhibitor used in combination with cefazolin or vancomycin and gentamicin is preferred for paediatric patients.16,17 The recommendations for adult and paediatric patients are the same, except for dosing.9
A study focusing on developing countries reported the very low use of SAP, with only 51% of surgical residents being aware of the guidelines.18 Studies have also reported that the most common cause of non-adherence was lengthy postoperative prophylaxis.3,18,19 In KSA and some other countries, there are inconsistencies between ASHP guidelines for surgical prophylaxis and current clinical practice.20, 21, 22 Non-adherence to the SAP guidelines is increasing and has been examined in multiple studies.1,3,20, 21, 22 While there is a lack of data, the non-compliance among physicians might be due to a lack of adequate knowledge, absence of resources or guidelines, disagreements with the recommendations, and a misconception that prolonging the duration of SAP reduces the risk of SSI. Clearly, this heath care issue must be addressed. This study was performed to evaluate the adherence to SAP guidelines in a tertiary care hospital in Almadinah Almunawwarah, located in western KSA.
Material and Methods
Study design and setting
The cohort study was conducted from January to April 2018 in the Department of General Surgery, King Fahad Hospital, Almadinah Almunawwarah, KSA. All patients, irrespective of age, who underwent surgery were included. Patients who did not follow the guidelines, did not respond to the continuous follow-up, or who changed hospitals during the study period were excluded from the study. King Fahad Hospital is a 425-bed facility that provides acute as well as chronic medical and surgical services, and a variety of out-patient services. The hospital is the centre for the co-ordination of the delivery of health care services throughout the defined geographical areas in Almadinah Almunawwarah.
Data collection
The collected data that included information regarding patient characteristics (demographics) were retrieved through a review of the medical charts and data from the hospital information system. These data included the type of surgical procedure, number of surgical procedures, preferred antibiotic regimen, identity and dose of drugs, identity of the postoperative prophylactic antibiotic, duration of the postoperative prophylactic antibiotic (less than or greater than 24 h) and the use of a single dose. All collected data were recorded in Microsoft Excel.
Data analyses
The completed survey form was collected, and the data were analysed by SPSS Statistics version 25.0 (IBM Corporation, Armonk, NY) for descriptive analyses. Categorical data were calculated as frequencies and percentages. Chi-square test was also used to identify associations between categorical variables. A P-value < 0.05 was considered to indicate significant difference.
Results
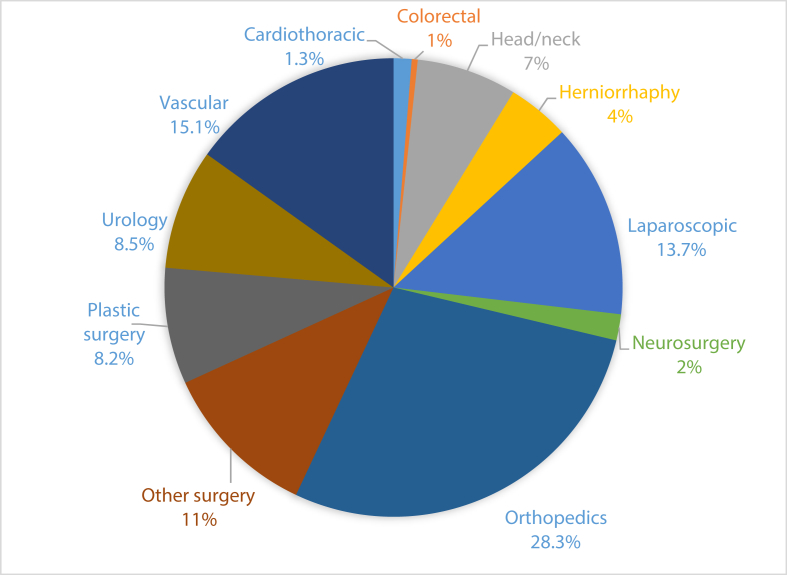
Half (51.2%) of the patients were female and most were older than 50 years of age (Table 1). Figure 1 shows the different surgical procedures performed during the study period. Majority of the procedures were orthopaedics (28.3%), vascular surgery (15.1%), laparoscopic procedures (13.7%), urology (8.5%) and plastic surgery (8.2%). One hundred and thirty-eight (19.5%) patients were administered antibiotics according to the guideline recommendations and 159 (22.5%) received antibiotics for the indicated times. More than half of the patients (n = 399, 56.4%) received antibiotics for >24 h and 129 (18.2%) for <24 h. Single dose therapy was used for 179 (25.3%) patients. Two hundred and ninety-seven (42%) patients had clean surgery, 284 (40%) had clean-contaminated surgery and 128 (18%) had contaminated surgery. Among the surgeries performed, SAP was administered <30 min prior to incision in 85 (12%) surgeries, 30–60 min prior to incision in 266 (37.6%) surgeries, 60–90 min prior to incision in 186 (26.3%) surgeries and >180 min prior to incision in 144 (20.4%) surgeries [Table 1].
Table 1.
Patient demographics and guidelines for SAP.
| Characteristics | Number | % |
|---|---|---|
| Gender | ||
| Male | 362 | 48.8 |
| Female | 345 | 51.2 |
| Age, years | ||
| 1–10 | 40 | 5.7 |
| 11–20 | 86 | 12.2 |
| 21–30 | 137 | 19.4 |
| 31–40 | 112 | 15.8 |
| 41–50 | 116 | 16.4 |
| >50 | 216 | 30.6 |
| Antibiotics given as per the recommendation of the guidelinea | ||
| Yes | 138 | 19.5 |
| No | 565 | 79.9 |
| Antibiotics given with a time frame | ||
| Yes | 159 | 22.5 |
| No | 548 | 77.5 |
| Duration of antibiotics | ||
| <24 h | 129 | 18.2 |
| >24 h | 399 | 56.4 |
| Single dose | 179 | 25.3 |
| Time of administration before surgical incision, mina | ||
| <30 | 85 | 12 |
| 30–60 | 266 | 37.6 |
| 90–120 | 91 | 12.9 |
| 120–150 | 70 | 9.9 |
| 150–180 | 50 | 7.1 |
| >180 | 144 | 20.4 |
Missing responses.
Figure 1.
The surgical procedures performed.
The most commonly prescribed antibiotics were ciprofloxacin alone (n = 20, 2.82%) or, in combination with metronidazole (n = 2, 0.3%) or ceftriaxone (n = 1, 0.1%), clindamycin (n = 8, 1.1%), cloxacillin (n = 1, 0.1%), gentamycin (n = 1, 0.1%), metronidazole (n = 5, 0.7%), piperacillin (16, 2.3%), piperacillin + moxifloxacin (n = 1, 0.1%) and vancomycin + gentamycin (n = 1, 0.1%). A single dose was used in 179 (25.3%) cases. Based on the strength of the antibiotic used, cefuroxime 1500 mg (n = 240, 33.9%) was the most common, followed by ceftriaxone 1 g (n = 203, 28.7%), cefazolin 1 g (n = 69, 9.7%), cefuroxime 750 mg (n = 19, 2.7%), clindamycin 900 mg (n = 23, 3.2%), clindamycin 600 mg (n = 13, 1.8%), ciprofloxacin 400 mg (n = 15, 2.1%) and piperacillin 4.5 g (n = 15, 2.1%).
Among the administered antibiotics, cephalosporin was the most frequently selected for use after a single dose (<or >24 h; n = 475, 67%), followed by cefuroxime (n = 215, 30.4%), ceftriaxone (n = 169, 23.9%), cephazolin (n = 47, 6.6%), ceftriaxone + metronidazole (n = 21, 3.0%), ceftazidime (n = 10, 1.4%) and cephalosporin in combination with different antibiotics (n = 13, 1.8%).
Table 2 summarises the significant differences between antibiotics administered according to the recommendation for the duration of antibiotic therapy in the guidelines (P = 0.001). Statistically significant differences were evident between antibiotics administered according to the time frame and those administered as recommended (P = 0.001). Table 3 summarises the significant differences between the type of surgical procedures performed and the antibiotics administered as recommended (P = 0.00).
Table 2.
Association between antibiotics administered as recommended and their duration.
| Variables |
<24 h |
>24 h |
Single dose |
P-value |
| Antibiotics given as recommended | ||||
| Yes | 22 (15.9%) | 60 (43.5%) | 56 (40.6%) | 0.001 |
| No |
107 (18.9%) |
336 (59.8%) |
122 (21.6%) |
|
| Antibiotics administered according to time frame |
||||
| No |
Yes |
Total |
P-value |
|
| Antibiotics given as recommended | ||||
| Yes | 86 | 52 | 138 | 0.000 |
| No | 460 | 105 | 565 | |
Table 3.
Types of surgical procedures performed and antibiotics administered as recommended.
| Surgical procedure | Antibiotics administered as recommended (%) |
P-value | |
|---|---|---|---|
| Yes | No | ||
| Cardiothoracic | – | 9 (1.6) | 0.000 |
| Colorectal | – | 3 (0.5) | |
| Head/neck | 40 (29) | 10 (1.8) | |
| Herniorrhaphy | 14 (10.1) | 17 (3.0) | |
| Laparoscopic | 20 (14.5) | 77 (13.6) | |
| Neurosurgery | 7 (5.1) | 6 (1.1) | |
| Orthopaedics | 1 (0.7) | 199 (35.2) | |
| Other surgery | 30 (21.7) | 48 (8.5) | |
| Plastic surgery | 10 (7.2) | 47 (8.3) | |
| Urology | 14 (10.1) | 44 (7.8) | |
| Vascular | 2 (1.4) | 105 (18.6) | |
Discussion
We surveyed the adherence to SAP guidelines at King Fahad Hospital to provide information that will be useful in formulating recommendations to improve health care practice. Most participants who underwent surgeries received antimicrobial prophylaxis pre- and/or post-operatively. The findings clearly demonstrated that adherence to SAP guidelines was not appropriate (19.5%) as only 22.5% of the SAP were administered according to the time frame stated in the ASHP guidelines. Furthermore, the practice of SAP observed in the present study did not conform to the recommended antimicrobial prophylaxis guidelines issued by ASHP.4, 5, 6, 7,9
Other studies20, 21, 22, 23 described similar findings. These findings may be the root cause for the overuse of antimicrobials for prophylaxis, besides the lack of an evidence-based protocol.
Many studies have established an adherence rate for the SAP guidelines, with the rate ranging widely from 0 to 70%.24,25 In the present study, overall adherence to the guidelines was 19.5%. This was very low compared to previously published studies. Surgeries were classified as clean-contaminated, contaminated, and dirty. The ASHP guidelines do not recommend antibiotics for clean procedures.3 Interestingly, in our study, among 707 patients who underwent surgery, four (0.5%) did not received antibiotics, as those surgeries were clean procedures, consistent with the ASHP guidelines. However, 42% of surgeries were performed as clean surgeries, a finding similar to that of another study conducted in Addis Ababa, which reported that 108 (54%) of the surgical wounds were clean, while 63 (31%) were clean-contaminated.19
The present study revealed discrepancies between the ASHP guidelines and the current practice at King Fahad Hospital. Similar discrepancies were found in other studies.20, 21, 22, 23 In the current study, only 18.2% of patients received SAP for an appropriate duration. This percentage was less than that reported in Mafraq Hospital, Abu Dhabi (30.5%), Iran (76.5%), India (89%), the Netherlands (92%) and Jordan (99.1%).23 The percentage of patients who received SAP within 1 h before skin incision was 37.6%. These results are inconsistent with reported rates of 40.3% in Abu Dhabi, 89% in India, 88.1% in Jordan, 76.5% in Iran and 50% in the Netherlands.23 However, another similar study performed in the capital of KSA reported that 40% of physicians followed the correct timing of administration as prescribed by the ASHP.20 This variation in antibiotic administration shows highlights the lack of knowledge of the ASHP guidelines and indicates that health care-associated infections may increase in health care settings.
The targeted duration of SAP should be initiated within 1 h prior to incision and discontinued within 24 h post-operatively for most procedures, and within 48 h for cardiac surgery.9,26 In operations lasting longer than 3 h a second dosage is recommended.9 A study compared the use of a single dose and 24-h administration, and described a similar efficacy for both approaches.27 Prolonged antibiotic prophylaxis is no more efficacious, may increase antibiotic resistance and unnecessarily increases hospital costs.28
Similar to other national and international studies,19,29, 30, 31, 32 cephalosporins including cefuroxime, ceftriaxone and cephazolin were the most frequently-used antimicrobial agents. Cefazolin and cefuroxime were also commonly used in prior studies.23,33 Another recent study published locally in KSA also reported similar findings. 20According to the guideline recommendations, narrow spectrum antimicrobials, first- or second-generation cephalosporins (such as cefazolin and cefuroxime) or clindamycin and vancomycin are recommended for patients with β-lactam allergy and for methicillin-resistant Staphylococcus aureus infection.4, 5, 6, 7,9 However, the ASHP SAP guidelines recommend cephazolin for surgical prophylaxis.9,33 Thus, the adherence to wide-spectrum antimicrobials in our study could be attributed to the absence of first- and second-generation cephalosporins, the low cost of ceftriaxone, absence of microbiologic data and lack of evidence-based protocols from the hospital.
A study34 described the major factors responsible for non-adherence to SAP guidelines. The authors included prescription for prophylactic antimicrobials by the surgeon, clean-contaminated surgery, trauma-related surgery and digestive tract, head, and neck-related surgeries. 34 However, the lack of adherence among healthcare professionals was mainly recognised due to the absence of comprehensive institutional guidelines, easy accessibility to several antibiotics that were not included in the guidelines and a lack of awareness about the SAP guidelines. Another major reason for non-compliance is the false belief that high-end/multiple antibiotics and prolonged therapy will be more effective in preventing SSIs as compared to short duration of narrow spectrum antibiotics.35 That being said, implementation of antibiotic stewardship is beneficial in controlling, prescribing and reducing inappropriate usage of antibiotics for therapeutic, empirical and prophylactic purposes.36
Limitations
Data were lacking, about the duration of surgery and the repeated dose of antibiotics although among the total surgeries performed, four patients did not receive antibiotics. These four were clean surgeries, implying that the guideline recommendation had been followed.
Conclusion
Most surgical procedures performed at King Fahad Hospital during a recent 3-month period involved SAP. However, the present findings indicate an inconsistency with the standard AHSP guidelines. Using the wrong antibiotic, administering a drug at the incorrect time, antimicrobial prophylaxis, and prolonged duration of postoperative antimicrobial prophylaxis were problems identified in the practice of SAP. These findings indicate the need for evidence-based guidelines for the practice of SAP in hospitals based on the antibiotic resistance pattern. Future studies focusing on adherence to SAP guidelines and improvement in health care settings are strongly recommended.
Recommendations
We recommend to implementation and adherence to the antibiotic stewardship programme for healthcare providers, who can play a significant role in reducing inappropriate usage of antibiotics in the healthcare setting. In addition, evaluating patients' medication profiles, providing specialist advice on optimal antibiotic therapy, reducing unnecessary antibiotic usage, writing evidence-based guidelines for antibiotic prescription and increasing the adherence to surgical prophylaxis antibiotic guidelines are all prudent actions. Adherence to surgical guidelines is crucial in every stage of health care practice by health care professionals. Therefore, a national assessment is needed.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
There is no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and complied with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Authors contributions
YMA, RA and AA participated in the study concepts, design of the study, development of the collection form and data acquisition and entry. OAA, FSA contributed to data analysis and statistical analysis of the data, participated in the intellectual content, reviewed and summarised the published literature and clinical studies and participated in outlining the result themes and manuscript preparation, editing and review. YMA takes responsibility for the integrity of the work as a whole. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Kim E.S., Park S.W., Lee C.S., Kwak Y.G., Moon C., Kim B.N. Impact of a national hospital evaluation program using clinical performance indicators on the use of surgical antibiotic prophylaxis in Korea. Int J Infect Dis. 2012;16(3):e187–e192. doi: 10.1016/j.ijid.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Ierano C., Nankervis J.M., James R., Rajkhowa A., Peel T., Thursky K. Surgical antimicrobial prophylaxis. Aust Prescr. 2017;40(6):225–229. doi: 10.18773/austprescr.2017.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwak Y.G. Appropriate use of surgical antibiotic prophylaxis. J Kor Med Sci. 2019;34(17):e136. doi: 10.3346/jkms.2019.34.e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bratzler D.W., Houck P.M., Surgical Infection Prevention Guideline Writers Workgroup Antimicrobial prophylaxis for surgery: an advisory statement from the national surgical infection prevention project. Am J Surg. 2005;189(4):395–404. doi: 10.1016/j.amjsurg.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Page C.P., Bohnen J.M., Fletcher J.R., McManus A.T., Solomkin J.S., Wittmann D.H. Antimicrobial prophylaxis for surgical wounds: guidelines for clinical care. Arch Surg. 1993;128(1):79–88. doi: 10.1001/archsurg.1993.01420130087014. [DOI] [PubMed] [Google Scholar]
- 6.Dellinger E.P., Gross P.A., Barrett T.L., Krause P.J., Martone W.J., McGowan J.E., Sweet R.L., Wenzel R.P. Quality standard for antimicrobial prophylaxis in surgical procedures. Infect Control Hosp Epidemiol. 1994;15(3):182–188. doi: 10.1086/646887. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Health-System Pharmacists ASHP therapeutic guidelines on antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 1999;56:1839–1888. doi: 10.1093/ajhp/56.18.1839. [DOI] [PubMed] [Google Scholar]
- 8.Mangram A.J., Horan T.C., Pearson M.L., Silver L.C., Jarvis W.R., Hospital Infection Control Practices Advisory Committee Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):247–280. doi: 10.1086/501620. [DOI] [PubMed] [Google Scholar]
- 9.Bratzler D.W., Dellinger E.P., Olsen K.M., Perl T.M., Auwaerter P.G., Bolon M.K., Fish D.N., Napolitano L.M., Sawyer R.G., Slain D., Steinberg J.P. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect. 2013 Feb 1;14(1):73–156. doi: 10.1089/sur.2013.9999. [DOI] [PubMed] [Google Scholar]
- 10.Olowo-Okere A., Ibrahim Y.K.E., Sani A.S., Olayinka B.O. Occurrence of surgical site infections at a tertiary healthcare facility in Abuja, Nigeria: a prospective observational study. Med Sci (Basel) 2018;6(3):60. doi: 10.3390/medsci6030060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edmiston C.E., Krepel C., Kelly H. Perioperative antibiotic prophylaxis in the gastric bypass patient: do we achieve therapeutic levels? Surgery. 2004;136:738–747. doi: 10.1016/j.surg.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 12.Claforan (cefotaxime sodium) for injection package insert. Sanofi Aventis; Bridgewater, NJ: 2009 Jul. [Google Scholar]
- 13.Pappas P.G., Silveira F.P. Candida in solid organ transplant recipients. Am J Transplant. 2009;9(suppl 4):S173–S179. doi: 10.1111/j.1600-6143.2009.02909.x. [DOI] [PubMed] [Google Scholar]
- 14.Alphonso N., Anagnostopoulos P.V., Scarpace S. Perioperative antibiotic prophylaxis in paediatric cardiac surgery. Cardiol Young. 2007;17:12–25. doi: 10.1017/S1047951107000066. [DOI] [PubMed] [Google Scholar]
- 15.Maher K.O., VanDerElzen K., Bove E.L. A retrospective review of three antibiotic prophylaxis regimens for pediatric cardiac surgical patients. Ann Thorac Surg. 2002;74:1195–1200. doi: 10.1016/s0003-4975(02)03893-6. [DOI] [PubMed] [Google Scholar]
- 16.Kato Y., Shime N., Hashimoto S. Effects of controlled perioperative antimicrobial prophylaxis on infectious outcomes in pediatric cardiac surgery. Crit Care Med. 2007;35:1763–1768. doi: 10.1097/01.CCM.0000269027.50834.FE. [DOI] [PubMed] [Google Scholar]
- 17.Vargas M.R., Danton M.H., Javaid S.M. Pharmacokinetics of intravenous flucloxacillin and amoxicillin in neonatal and infant cardiopulmonary bypass surgery. Eur J Cardio Thorac Surg. 2004;25:256–260. doi: 10.1016/j.ejcts.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Satti M.Z., Hamza M., Sajid Z., Asif O., Ahmed H., Zaidi S.M.J., Irshad U. Compliance rate of surgical antimicrobial prophylaxis and its association with knowledge of guidelines among surgical residents in a tertiary care public hospital of a developing country. Cureus. 2019;11(5) doi: 10.7759/cureus.4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Argaw N.A., Shumbash K.Z., Asfaw A.A., Hawaze S. Assessment of surgical antimicrobial prophylaxis in orthopaedics and traumatology surgical unit of a tertiary care teaching hospital in Addis Ababa. BMC Res Notes. 2017;10(1):160. doi: 10.1186/s13104-017-2475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jalil M.A., Al-Shdefat R.I., Tumah H.N. The practice of preoperative antibiotic prophylaxis and the adherence to guideline in Riyadh hospitals. Bull Env Pharmacol Life Sci. 2015;5:8–14. [Google Scholar]
- 21.Al-Azzam S.I., Alzoubi K.H., Mhaidat N.M., Haddadin R.D., Masadeh M.M., Tumah H.N., Magableh A., Maraqa N.K. Preoperative antibiotic prophylaxis practice and guideline adherence in Jordan: a multi-centre study in Jordanian hospitals. J Infect Dev Countr. 2012;6(10):715–720. doi: 10.3855/jidc.1676. [DOI] [PubMed] [Google Scholar]
- 22.Bennett N.J., Bull A.L., Dunt D.R., Russo P.L., Spelman D.W., Richards M.J. Surgical antibiotic prophylaxis in smaller hospitals. ANZ J Surg. 2006;76(8):676–678. doi: 10.1111/j.1445-2197.2006.03826.x. [DOI] [PubMed] [Google Scholar]
- 23.El Hassan M., Elnour A.A., Farah F.H., Shehab A., Al Kalbani N.M., Asim S., Shehab O.A., Abdulla R. Clinical pharmacists' review of surgical antimicrobial prophylaxis in a tertiary hospital in Abu Dhabi. Int J Clin Pharm. 2015;37(1):18–22. doi: 10.1007/s11096-014-0045-4. [DOI] [PubMed] [Google Scholar]
- 24.Tourmousoglou C.E., Yiannakopoulou E.C., Kalapothaki V., Bramis J., Papadopoulos J.S. Adherence to guidelines for antibiotic prophylaxis in general surgery: a critical appraisal. J Antimicrob Chemother. 2008;61(1):214–218. doi: 10.1093/jac/dkm406. [DOI] [PubMed] [Google Scholar]
- 25.Ruiz Tovar J., Badia J.M. Prevention of surgical site infection in abdominal surgery. A critical review of the evidence. Cir Esp. 2014;92(4):223–231. doi: 10.1016/j.ciresp.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Berrφos-Torres S.I., Umscheid C.A., Bratzler D.W., Healthcare Infection Control Practices Advisory Committee Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–791. doi: 10.1001/jamasurg.2017.0904. [DOI] [PubMed] [Google Scholar]
- 27.Fonseca S.N., Kunzle S.R., Junqueira M.J., Nascimento R.T., de Andrade J.I., Levin A.S. Implementing 1-dose antibiotic prophylaxis for prevention of surgical site infection. Arch Surg. 2006;141:1109–1114. doi: 10.1001/archsurg.141.11.1109. [DOI] [PubMed] [Google Scholar]
- 28.Harbarth S., Samore M., Lichtenberg D., Carmeli Y. Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation. 2000;101:2916–2921. doi: 10.1161/01.cir.101.25.2916. [DOI] [PubMed] [Google Scholar]
- 29.Vessal G., Namazi S., Davarpanah M.A., Foroughinia F. Evaluation of prophylactic antibiotic administration at the surgical ward of a major referral hospital, Islamic Republic of Iran. EMHJ. 2011;17(8):663–668. [PubMed] [Google Scholar]
- 30.Rehan H.S., Kakkar A.K., Goel S. Pattern of surgical antibiotic prophylaxis in a tertiary care teaching hospital in India. Int J Infect Control. 2010;6(2):34–39. [Google Scholar]
- 31.Radji M., Aini F., Fauziyah S. Evaluation of antibiotic prophylaxis administration at the orthopedic surgery clinic of tertiary hospital in Jakarta, Indonesia. Asian Pac J Trop Dis. 2014;4(3):190–193. [Google Scholar]
- 32.Kigera J.W.M., Gakuo L.N. Is there a role for prolonged post-operative antibiotic use in primary total hip arthroplasty in the African setting? SA Orthop J. 2013;12(4):38–40. [Google Scholar]
- 33.Abdel-Aziz A., El-Menyar A., Al-Thani H., Zarour A., Parchani A., Asim M., El-Enany R., Al-Tamimi H., Latifi R. Adherence of surgeons to antimicrobial prophylaxis guidelines in a tertiary general hospital in a rapidly developing country. Adv Pharmacol Sci. 2013;2013:842593. doi: 10.1155/2013/842593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simon A.M., Dzierzek A.C., Djossou F., Couppie P., Blaise N., Marie M., Mahamat A. Factors associated with non-compliance to surgical antimicrobial prophylaxis guidelines during a prospective audit. Ann Fr Anesth Reanim. 2012;31(2):126–131. doi: 10.1016/j.annfar.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 35.Parulekar L., Soman R., Singhal T., Rodrigues C., Dastur F.D., Mehta A. How good is compliance with surgical antibiotic prophylaxis guidelines in a tertiary care private hospital in India? A prospective study. Indian J Surg. 2009;71:15–18. doi: 10.1007/s12262-009-0004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aryee A., Price N. Antimicrobial stewardship—can we afford to do without it? Br J Clin Pharmacol. 2015;79(2):173–181. doi: 10.1111/bcp.12417. [DOI] [PMC free article] [PubMed] [Google Scholar]