The COVID-19 tsunami has reached our Catheterization laboratory (Cath lab) and will affect everyone in it, especially those labs (the majority) with direct access for patients for primary coronary intervention (PCI). It is essential to be prepared in advance. Awaiting the first COVID-19 patient’s arrival and then improvising corresponds to waiting for a disaster. Several instructions on how to manage a Cath lab during the COVID-19 pandemic have already been provided by different scientific societies.1,2 Here, we simply report our thoughts based on common sense, as nobody at present has any reliable data.
1. It is essential to set priorities.
For years, there have always been priorities in the Cath lab: radiological protection of the team and acting as fast as possible: ‘time is life’ was the mantra. Today, the first priority is the safety of the team: a team in quarantine means the inability to save many more patients. Radiological protection is needed, but it is not enough. It should be combined with effective protection from the virus. Time to revascularization remains a priority, but patient outcome does not change much if extra time is taken to secure the workforce first. The room and the team need to be well prepared to receive positive or suspected COVID-19 patients by wearing personal protective equipment including gloves, gowns, goggles, shields, glasses, and FFp3 or N95 masks.
Therefore, the first priority is to prepare each team beforehand. Cath lab directors have to:
obtain (and look at!) adequate protective equipment;
train (and train again and again) the teams;
define a command structure, learning from disaster medicine such as war, as we are actually at war!
not underestimate the psychological pressure on the teams.
Many team members will be afraid of becoming infected. Some will have children to look after at home as schools are closed. Others may be worried about the economic constraints, etc. For these reasons, it is essential to reduce the workload of the team as much as possible. It is reasonable to postpone elective procedures, at least after telephone communication for a clinical assessment of the real needs of the patient; (v) in line with the above, staff shortages (including the possibility of being infected and quarantined) should be anticipated and a rescue plan should be put in place; (vi) finally, human factors are vital; every effort should be made to maintain effective teambuilding and to allow sufficient time for listening to problems and concerns.
The other priority is to correct the behaviour of the patients.
It is universally accepted (although no definitive data are available) that since the beginning of the COVID-19 pandemic, hospitals are experiencing fewer admissions for acute coronary syndromes (ACS). This is surprising. Actually, it should be the opposite. Like all other infections, COVID-19 is expected to favour plaque instability and cause more myocardial infarctions (MIs).3 Media campaigns (TV, radio, newspapers, social media, etc.) recommend not to overcrowd the emergency department, and… ‘Stay at home’ is the current, consistent, message. Patients are afraid to go to the hospital and become infected, so they prefer to stay at home, even with chest pain. All of this is wrong. Patients should be reassured about the safety of hospitals with areas for COVID-19 patients separated from the others. The message should be reformulated: ‘Business as usual. If you have chest pain, call an ambulance. The risk of mortality for MI outweighs that of COVID-19 infection’. Indeed, scientists and epidemiologists will appropriately investigate this phenomenon and find out whether remodulation of the healthcare system due to the COVID-19 pandemic has caused more non-hospital casualties for ACS.
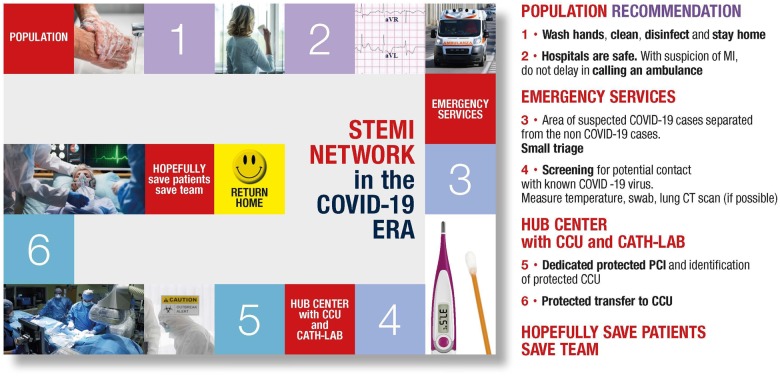
The third priority is to be prepared to treat known or suspected COVID-19 patients with ACS. Let us see these practicalities. As shown in Figure 1, patients will reach the hub for ACS either by ambulance or through the emergency department. In both cases, a simple triage (presence of fever, cough, dyspnoea, diarrhoea, etc., coming from ‘hot’ areas, and, when possible, a lung CT scan or a swab) for the presence of COVID-19 needs to be performed.
Figure 1.
Various steps of the journey of ACS patients in the COVID-19 pandemic.
Then, for suspected or confirmed COVID-19 ST-segment elevation myocardial infarction (STEMI) patients, there are two options: fibrinolytic therapy or primary angioplasty. Fibrinolysis is favoured in China for local conditions and for risks of staff contamination.4,5 The same is not true in Europe, where the superiority of PCI over thrombolysis is well established and where efficient networks between the hub and spoke centres are active.6 However, the current situation forces temporary reorganization of the networks.
In Lombardy (northern Italy), for instance, there are 129 accredited hospitals, 55 of which are equipped with Cath labs offering 24/7 service for acute MI to ∼10 million inhabitants. The regional government has reduced this to 13 hospitals with Cath labs now acting as hubs, with the remainder acting as spokes. Patients are referred to a hub on the basis of geographic proximity. The same model has been applied to other cardiovascular emergencies (e.g. stroke).7 Ideally, a dedicated Cath lab should be located in a COVID-19 area of the hospital, but this may not always be possible. In the latter case, a ‘temporary’ COVID-19 lab and procedure with a protected team needs to be set up for each patient. This might require a longer time. If the Cath lab is not ready, our suggestion is that patients wait in the ambulance rather than in the pre-operating room.
For non-STEMI patients, timing should allow diagnostic testing for COVID-19 infection (by either positive swab samples or lung CT scan) prior to cardiac catheterization. Positive cases should follow the same protocol as STEMI patients, if they cannot be managed by optimal medical therapy. Rapid discharge of these non-STEMI patients after revascularization is recommended to maximize bed availability and to reduce exposure within the hospital. Whenever possible, these patients should be followed-up at home via telemedicine. In both instances, transportation of suspected or positive COVID-19 patients from the Cath lab to the appropriate area of the hospital (either known COVID-19 or just suspect) should occur with protected staff following pre-determined pathways and safe corridors. At the end of each procedure, the necessary cleaning time for the Cath lab should be allowed. Whenever possible, these cases should be scheduled at the end of the working day, not to compromise the procedures which follow.
Some of these steps are summarized in Figure 1, from patient at home to the emergency department or Cath lab and then to the appropriate intensive care unit (ICU) or ward before discharge. For this journey in this present time of ‘war’, there is the need for strong alliances, perfect networking, and much training. However, inevitably, something will go wrong as no plan will work perfectly under a tsunami. However, one should aim, as a minimum, to reduce the disaster.
So, plan for the worst and hope for the best!
Gianluca Campo1,2, Claudio Rapezzi1,2, Luigi Tavazzi2, and Roberto Ferrari1,2*
1Cardiovascular Center, University of Ferrara, Ferrara, Italy and 2Maria Cecilia Hospital, GVM Care & Research, Cotignola, (RA), Italy
*Corresponding author. Ospedaliero-Universitaria di Ferrara, Ospedale di Cona, Aldo Moro 8, 2/C/3° piano, Room 3:13:03, 44124 Ferrara, Italy. Tel: +39 0532 239882, Fax: +39 0532 237841, Email: fri@unife.it
References
References are available as supplementary material at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.