Abstract
Objective
To describe the implementation of technological support important for optimizing clinical management of the COVID-19 pandemic.
Materials and Methods
Our health system has confirmed prior and current cases of COVID-19. An Incident Command Center was established early in the crisis and helped identify electronic health record (EHR)-based tools to support clinical care.
Results
We outline the design and implementation of EHR-based rapid screening processes, laboratory testing, clinical decision support, reporting tools, and patient-facing technology related to COVID-19.
Discussion
The EHR is a useful tool to enable rapid deployment of standardized processes. UC San Diego Health built multiple COVID-19-specific tools to support outbreak management, including scripted triaging, electronic check-in, standard ordering and documentation, secure messaging, real-time data analytics, and telemedicine capabilities. Challenges included the need to frequently adjust build to meet rapidly evolving requirements, communication, and adoption, and to coordinate the needs of multiple stakeholders while maintaining high-quality, prepandemic medical care.
Conclusion
The EHR is an essential tool in supporting the clinical needs of a health system managing the COVID-19 pandemic.
Keywords: coronavirus, pandemic, electronic health record, clinical informatics, telemedicine
INTRODUCTION
The novel coronavirus COVID-19 was initially identified in December 2019 as a case of pneumonia in Wuhan, China and has since become a global pandemic, affecting more than 150 countries around the world.1–6 The World Health Organization declared the outbreak a pandemic on March 11, 2020 and called for coordinated mechanisms to support preparedness and response to the infection across health sectors.7 On March 13, the Executive Office of the President of the United States proclaimed the pandemic a national emergency.8 While the incidence of COVID-19 continues to rise, healthcare systems are rapidly preparing and adapting to increasing clinical demands.9,10 Inherent to the operational management of a pandemic in the era of modern medicine is leveraging the capabilities of the electronic health record (EHR), which can be useful for developing tools to support standard management of patients.11 Technology-based tools can effectively support institutions during a pandemic by facilitating the immediate widespread distribution of information, tracking transmission in real time, creating virtual venues for meetings and day-to-day operations, and, perhaps most importantly, offering telemedicine visits for patients.12–16
During the Ebola outbreak in 2014, attention was brought to the use of the EHR as a potential public health tool.17 Unfortunately, despite the recent Ebola epidemic, the infrastructure for outbreak management was not present in many US health systems and their EHR applications.18 As we are now facing a pandemic, many institutions are working to rapidly develop supportive and reliable informatics infrastructure in order to prepare for managing an exponential increase in COVID-19-infected patients. However, the literature to describe the informatics tools required to successfully manage this novel infection is lacking.
OBJECTIVE
Here we discuss the rapid development and implementation of the EHR configuration necessary for outbreak management within a large regional public academic health center in the setting of new and pending COVID-19 cases. We detail the specific informatics tools we built to support the health system’s efforts to prepare for the current pandemic and the challenges associated with this task.
MATERIALS AND METHODS
University of California, San Diego Health (UCSDH) is a large regional academic health system encompassing 2 acute care hospitals, outpatient primary and specialty medical and surgical care, and emergency patient care. UCSDH is also 1 of 5 academic medical centers within a broader 10-campus University of California system. UCSDH utilizes a commercially available, electronic health record (EHR), Epic (Verona, WI), and hosts over 300 affiliate physicians across 10 medical groups on this EHR. San Diego County served as a quarantine site for both Chinese expatriates and cruise ship passengers, and also experienced community spread of COVID earlier than much of the US.19 An Incident Command Center (ICC) was established at UCSDH on February 5, 2020 for 24-hour monitoring and adaptation to rapidly evolving conditions and recommendations on a local, state, federal, and global scale. An assessment of the institutional current state revealed the need to develop a rapid screening process, hospital-based and ambulatory testing, new orders with clinical decision support, reporting/analytics tools, and the enhancement/expansion of current patient-facing technology.
RESULTS
With the guidance of the ICC, our clinical informatics team prioritized projects related to COVID-19 to enable expedited build and implementation. In response to the pandemic, we configured our EHR with the technology-based tools listed in Table 1. Awareness and training of novel resources for clinicians and staff were distributed via a variety of communication channels in concurrence with important epidemiologic, policy, and health safety information by the ICC and health system leadership.
Table 1.
Electronic health record tools for managing a pandemic
| Screening protocols |
| Triage of Patient Phone Calls |
| Required Registration/Check-In Screening Questions for All Patients |
| System Level EHR-Templates |
| Triage of patient phone calls, nurse directed |
| Managing patient concerns for providers |
| Home Isolation Instructions |
| Screening or treating a patient in an ambulatory care setting |
| Screening or treating a patient in an urgent care setting |
| Updated with Current Infection Control Specialist and Command Center Information |
| Inpatient, Emergency Department and Ambulatory Order Panels |
| Decision support for who needs testing |
| Embedded modifiable required isolation orders |
| Detailed personal protective equipment needs for providers |
| Detailed instructions for proper specimen collection |
| Reporting and Analytics |
| COVID-19 Operational Dashboard |
| Tracking of COVID-related infection in EHR embedded database |
| Tracking of persons under investigation (PUI) in EHR embedded database |
| Reports regarding prior PUI, existing and pending tests, training completion, and screening/documentation compliance |
| Communication Channels |
| EHR-integrated secure messaging |
| Artificial Intelligence |
| Real-time Covid-19 detection algorithm to assist in diagnostic imaging |
| Patient Facing Technology |
| Telemedicine – Video Visits for Outpatient Clinic Encounters |
| Repurposing and utilization of EHR optimization team to train end users in video visit workflow |
Screening tools
One of the first needs for the health system was the development of a rapid and effective multimodal COVID-19 screening process, including telephone calls, direct email, and EHR messaging, all before in person encounters. A protocolized triage system was developed and embedded into multiple EHR templates which could be rapidly updated as screening guidance evolved (Table 2). These instructions can be easily accessed by call centers and triage nurses, allowing them to provide guidance to patients regarding requirements for home isolation, appropriate locations to obtain COVID-19 testing, and when to visit the emergency department. In order to limit exposure and relieve the burden on physical healthcare locations, automated email notifications were sent to patients prior to their clinic appointments indicating that persons with fever and/or new cough should call the health system for proper triage before presenting to the healthcare facility.
Table 2.
Modifiable templates available in the electronic health record
| Smart phrase | Setting of use | Description of content |
|---|---|---|
| .UCSDCOVID19TRIAGE | Phone or in person patient triage | Updated travel and symptom screening, testing criteria, and clear guidance on best setting and location of patient care |
| .UCSDCOVID19PATIENTCONCERNS | Phone or in person patient encounter | Detailed information on frequently asked questions concerning COVID-19 |
| .UCSDCOVID19HOMEISOLATION | When instructing patients on home isolation | Isolation information for patients, including the discontinuation of home isolation |
| .UCSDCOVID19AMBULATORY | Ambulatory screening or testing | Clinical decision support on testing criteria, recommended additional work-up, admission criteria/protocol, and discharge information |
| .UCSDCOVID19URGENTCARE | Urgent Care/ED screening or testing | Clinical decision support on testing criteria, recommended additional work-up, admission criteria/protocol, and discharge information |
| .UCSDCOVID19VISITORSCREENING | Clinics or inpatient units | Standard documentation of any screening of patient visitors for symptoms of infection |
| UCSD COVID-19 WORK EXCUSE | Work excuse letter | Templated excuse letter for providers to recommend working from home |
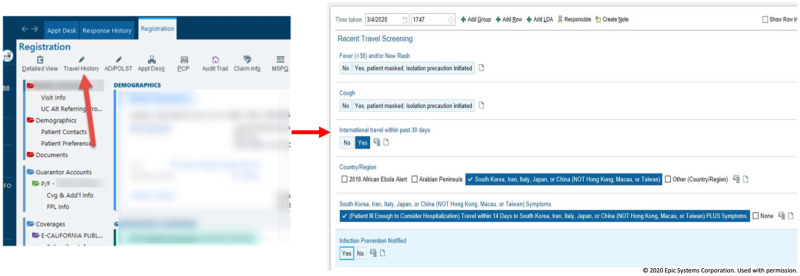
Travel and symptom screening questions were added to the registration/check-in process (Figure 1). The EHR was configured to require complete documentation by front desk staff, ensuring that all patients being seen for acute and elective care across the institution receive screening. EHR templates were used by frontline staff to adhere to a standardized screening “script.” Positive screening questions in both acute and ambulatory care settings triggered a provider alert with clinical decision support offering appropriate guidance for subsequent clinical care, including any testing or isolation orders needed to facilitate next steps. Again, this set of tools in the EHR can be rapidly adjusted based on evolving recommendations.
Figure 1.
Travel and symptom screening. The above screenshot demonstrates the required screening, as viewed by front desk staff, that was added to the registration/check-in process for all patients.
Ordering tools
We constructed order panels in the EHR for inpatient, emergency department, and ambulatory settings that included a defaulted, prepopulated COVID-19 lab order, appropriate isolation orders, and options for additional laboratory testing or imaging studies. UCSDH elected to use in-house COVID-19 testing for patients in the hospital and emergency department, but to have COVID-19 tests that were obtained in ambulatory and urgent care settings sent out to a reference laboratory due to initial existing limitations in testing capacity. As such, engineering the correct order to appear in the correct setting was essential to avoid confusion and process failures. Additionally, modifications were made to our existing respiratory pathogen panel, as several tests for non-COVID-19 coronaviruses were already present in the system. In order to avoid confusion for both clinicians and patients, these tests were clearly labeled to delineate between COVID-19 and other coronaviruses unrelated to the current pandemic or “NON-COVID-19 coronavirus.”
Clinical decision support at the moment of ordering was provided by including screening criteria, information on specimen acquisition, requirements for personal protective equipment, and expectations on test result turnaround time for easy review. In addition, a series of questions were added to the COVID-19 orders, requiring the ordering provider to document the testing criteria met by the patient. Our build construct allowed for rapid editing to maintain alignment with operational needs as screening requirements and lab handling processes frequently changed following the initial implementation. Similar COVID-19 ordering workflows were instituted in our occupational health department to prepare for the potential of increased healthcare worker exposures.
Team communication and coordination of health system efforts
To better respond to the rapidly evolving care needs during this outbreak, UCSDH assembled a 7-person Ambulatory COVID Team (ACT). Team members included 2 infectious disease physicians, 3 primary care physicians (our community care physician lead, an epidemiology expert, and our ambulatory Chief Medical Information Officer), and 2 nurses. We used a secured messaging platform (SMP) within the EHR to enable rapid communication between the ACT of any new requirements or updates while offering the ability to share protected health information when necessary. The SMP can be accessed in both the desktop EHR as well as the EHR mobile applications. Key benefits of EHR-integrated messaging over other forms of secure communication, namely email and pager, include the ability of the message sender to see which team members have reviewed a given message and one-click access to any patient chart attached to the message, whether using SMP on the desktop or on a mobile device. This platform enabled 24-hour secure communication among members of the ACT and other clinical care providers.
Reporting and analytics
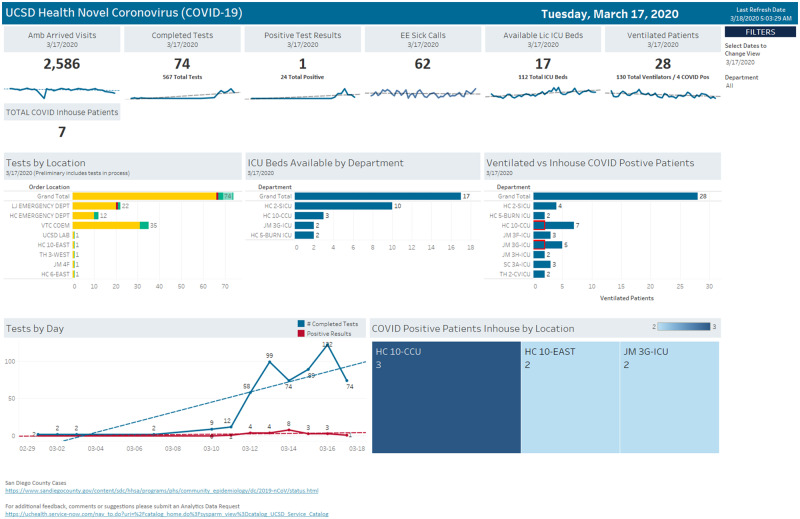
Having the ability to monitor the evolving current state of the health system was a key request from the ICC. The enterprise reporting team constructed a series of easily accessible reports within the EHR for use by the ICC, Infection Control, and other key organizational leaders. The reports were automatically distributed, accessible on mobile devices, and used to inform operational decisions on expanding testing capacity, patient isolation procedures, and geographic cohorting of patients and to monitor adherence to patient screening processes. We also created a COVID-19 Operational Dashboard with real-time data on the number of patients tested, test results, bed availability in the intensive care unit, availability of ventilator units, and volume of ambulatory visits (Figure 2). In addition, UCSDH had previously granted broad access to the EHR self-service analytics tool, with which key personnel can create ad hoc reports on items such as the use of isolation and frequency of testing.
Figure 2.
COVID-19 outbreak management dashboard. This dashboard was created and utilized by the Incident Command Center, institutional leaders, nursing supervisors, and other healthcare providers to monitor COVID-19 patient volume and distribution across the health system, COVID-19 test results, intensive care unit and ventilator use and availability, and the impact of the outbreak on daily ambulatory visits. The right side of the middle panel shows the number of ventilated patients; highlighted in red are ventilated patients who are COVID-19 positive versus non-COVID-19 ventilated patients.
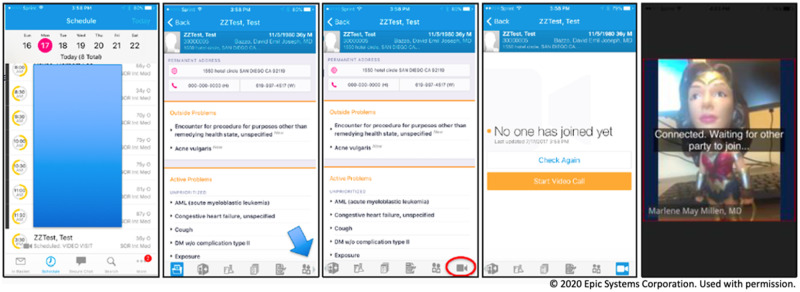
Patient-facing technologies
UCSDH prioritized moving in person clinic visits to telemedicine-based visits when appropriate in order to avoid unnecessary patient and staff exposure. Prior to the advent of the COVID-19 outbreak, UCSDH had already developed and implemented a telemedicine infrastructure for use by multiple outpatient clinics. In response to the federal government’s loosening of telehealth requirements and local desire to convert existing outpatient visits to video, we expanded access to all outpatient areas and created online self-guided learning videos on the conduct of virtual patient care (Figure 3).20,21 In addition, we repurposed an existing ambulatory EHR optimization team to provide assistance to onboarding clinical areas or those enhancing their telemedicine capacity. Within 72 hours of the executive proclamation of a national emergency, over 300 unique health employees were trained in telemedicine and approximately 1000 video visits were scheduled.
Figure 3.
Telemedicine - Video Visit. Graphic displaying the layout of UC San Diego’s virtual visit encounter.
Over 200 000 patients at UCSDH use the patient portal functionality within the EHR-tethered patient portal (Epic MyChart) which allows patients to utilize the video visit capability described above in addition to scheduling appointments, secure messaging with the care team, and viewing and downloading test results.22 The aforementioned modification of the display names for our preexisting coronavirus assay ensured that non-COVID coronavirus lab results displayed to patients as “non-COVID-19.” An early operational decision was made to delay the release of positive COVID-19-specific test results to allow UCSDH to directly contact and inform patients. However, we elected to immediately post negative COVID-19 test results to MyChart as testing volume made it more challenging to contact all tested patients in a timely fashion.
DISCUSSION
We describe a series of EHR enhancements designed to support the rapid deployment of new policies, procedures, and protocols across a healthcare system in response to the COVID-19 pandemic. Within the span of a few weeks, the magnitude of the outbreak within the United States became clear to healthcare leaders on local, state, and federal levels.10,18 As our own institution faced a growing number of known and suspected COVID-19 cases, as well as a variety of patient care and operational needs related to the pandemic, we recognized the importance of the EHR and other technology-based tools as an enabling adjunct to accelerated process design and implementation. The development of a multidisciplinary task force involving institutional leaders, infectious disease and infection prevention specialists, and technology experts is a critical first step in addressing hospital-specific concerns and developing open and productive communication.23–25 An initial needs-based assessment was done of the current state to determine the necessary operational processes for outbreak management, the existing informatics structure to support these processes, and the gaps that needed to be bridged in a timely fashion. Doing so allowed us to expediently configure the EHR to support COVID-19 outbreak management as detailed in this report.
Consideration of informatics needs in the setting of an outbreak or pandemic begins with strategic planning and a review of well described pandemic response protocols from established agencies such as the World Health Organization and the Centers for Disease Control and Prevention. In addition to constantly evolving recommendations from such agencies that specifically pertain to COVID-19, there is publicly available information on pandemic responses in general.17 Literature detailing actions taken to mitigate previous influenza outbreaks, such as the 2009 outbreak of the novel influenza A (H1N1) virus, also provides useful guidance.26 The basic principles of well-established protocols include planning and coordination, situation monitoring and assessment, reducing the spread of disease, continuity of healthcare provisions, and communications.26 Furthermore, a number of recently published articles have discussed COVID-19 specific guidelines and considerations for health systems and governments in mounting a strategic response to the pandemic.3,23,27,28 All of this information can serve to assist governments and regional health systems in combatting the outbreak. However, to our knowledge no reports have detailed the specific tools within an EHR that can be developed and leveraged to support the efforts of the public health response against COVID-19. In the modern era, essentially all of the processes mentioned above rely heavily on technology and, for individual health systems, direct interfacing with the EHR. Therefore, we have summarized our recent efforts to enhance our informatics infrastructure.
There are other recent examples of utilizing technology during this public health crisis. In Taiwan, a national health insurance database was integrated with immigration and customs data to generate real-time alerts during clinic visits to aid in case identification.29 Online questionnaires were utilized to risk stratify travelers so that low risk citizens were automatically sent a health declaration border pass while high-risk individuals were quarantined at home and remotely monitored for the development of symptoms with mobile device applications.29 Healthcare systems in Houston, Texas, developed remote communication channels between physicians and emergency responders to assist with triaging.14 Virtual home visits for high risk individuals and remote ICU monitoring is also being employed to reduce hospital staff contact with patients with suspected or confirmed cases of COVID-19.14
Multiple institutions across the United States have transitioned to telemedicine in an effort to reduce emergency room visits through remote triaging.23 Telemedicine has already proved useful during epidemiological emergencies, including through use of live video counseling with patients, virtual patient monitoring, and mobile applications for symptom observation.15 Telemedicine can be used to set emergency medicine to triage patients, decrease the rate of discharge without complete treatment and proper follow-up, and reduce the number of in person visits and subsequent risk of transmission of infection.12–13 An additional application is in early symptom identification and triaging as a mitigation strategy for potential delays in access to healthcare.30 This was previously observed in Wuhan, China during the initial outbreak of COVID-19 when 89% of patients were not hospitalized until at least 5 days into their illness.30 Enhancing existing EHR platforms with tools for triaging and screening for symptoms has the potential to identify symptomatic patients earlier and decrease the physical burden on healthcare systems.31
At our own institution, much of the informatics framework to support outbreak management already existed as a result of repetitive enhancements to the EHR, from both our vendor and our local configuration. Despite this robust starting point, we still experienced several challenges in implementation. The usual EHR enhancement project includes a thorough clinical and technical scoping process, a budgeting and planning stage, project management oversight, careful design with testing in multiple electronic environments, ample communication to end users prior to go-live, and, finally, implementation with field support in active clinical settings. Due to obvious time constraints, we were unable to follow this standard workflow. The result was an end product that required back and forth communication with frontline care providers, ongoing iterations, and unanticipated incidents and disruptions to daily practice. Education and training were difficult as providers dealt with a litany of internal and external communication streams in addition to managing an already full clinical workload. A surge in requests from clinical departments to start utilizing video visits placed a strain on the limited bandwidth of the informatics department and the EHR optimization team necessitating the development of a prioritization and onboarding process. Another important challenge was balancing the need to focus on the pandemic while maintaining high-quality healthcare and operations unrelated to the novel infection in order to provide service to all aspects of the community. Finally, the frequently changing landscape of a pandemic, with frequent daily guideline and protocol updates that generally require approval from multiple stakeholders within a large and complex health system, presented challenges to maintaining the rapid project momentum.
The most significant mitigation strategy for these challenges was the establishment of a 24-hour ICC that included representation from UCSDH Information Services. This enabled real-time identification of failures and successes, a focus on evolving needs, and feedback on subsequent interventions. The COVID-19 pandemic has highlighted the importance of a multidisciplinary team approach to medical care and building cohesive systems capable of sustaining unanticipated trials.
CONCLUSION
In the face of the COVID-19 pandemic, healthcare systems can best prepare by following guidelines and recommendations set forth by federal and global institutions. The electronic health record and associated technologies are vital and requisite tools in supporting outbreak management that should be leveraged to their full potential, and we hope that our experiences in developing these tools will be helpful to other health systems facing the same challenges.
FUNDING
Hannah Hollandsworth, MD is a funded researcher through the National Cancer Institute, National Institutes of Health, United States Department of Health and Human Services [NIH/NCI T32CA121938]. There are no funding sources to report for this research article.
ACKNOWLEDGMENTS
We would like to gratefully acknowledge Josh Glandorf, Jennifer Holland, Kirk Kurashige, Dean Pham, and Marc Sylwestrzak from the Department of Information Services and Chad VanDenBerg from Quality and Patient Safety at the University of California, San Diego for their contributions and nonstop dedication to the development of the informatics projects detailed in this article. We would also like to thank our vendor partners in Verona, Wisconsin.
AUTHOR CONTRIBUTIONS
Study concept and design: JJR, BJC, MM, MT-S, and CAL. Analysis and interpretation of data: JJR, BJC, and MM. Collection or assembly of data: JJR, BJC, MM, Torriani, Taplitz, an d Abeles. Drafting of the manuscript: JJR and HMH. Critical revision of the manuscript for important intellectual content: JJR, HMH, MT-S, Torriani, Taplitz, Abeles, MM, BJC, and CAL. Funding: HMH, BJC, and CAL. Administrative, technical and logistic support: BJC, MM, and CAL. Study Supervision and Coordination: BJC and CAL.
CONFLICT OF INTEREST
None declared.
REFERENCES:
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382 (8): 727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu JT, Leung K, Leung GM.. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 2020; 395: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johns Hopkins University Center for Systems and Science Engineering. Coronavirus COVID-19 Global Cases. https://coronavirus.jhu.edu/map.htmlAccessed March 18, 2020.
- 4. He F, Deng Y, Li W.. Coronavirus disease 2019 (COVID-19): what we know? J Med Virol 2020; 2019: 0–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Coronavirus Disease 2019. (COVID-19) Situation Report - 52.
- 6. Wu Z, McGoogan JM.. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 2019: 3–6. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Responding to community spread of COVID-19. Interim Guidance 2020; 1–6. [Google Scholar]
- 8.Proclamation on declaring a national emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/Accessed March 13, 2020.
- 9. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 19: 14–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Coronavirus disease 2019. (COVID-19) in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.htmlAccessed March 16, 2020.
- 11. Atreja A, Gordon SM, Pollock DA, Olmsted RN, Brennan PJ.. Opportunities and challenges in utilizing electronic health records for infection surveillance, prevention, and control. Am J Infect Control 2008; 36(3 suppl): 37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Joshi AU, Randolph FT, Chang AM, et al. Impact of emergency department tele-intake on left without being seen and throughput metrics. Acad Emerg Med 2020; 27 (2): 139–47. [DOI] [PubMed] [Google Scholar]
- 13. Langabeer JR, Gonzalez M, Alqusairi D, et al. Telehealth-enabled emergency medical services program reduces ambulance transport to urban emergency departments. West J Emerg Med 2016; doi : 10.5811/westjem.2016.8.30660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hollander JE, Carr BG.. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 1–3. [DOI] [PubMed] [Google Scholar]
- 15. Lurie N, Carr BG.. The role of telehealth in the medical response to disasters. JAMA Intern Med 2018; 178 (6): 745. [DOI] [PubMed] [Google Scholar]
- 16. Dong E, Du H, Gardner L.. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020; 3099 (20): 19–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fidler DP, Gostin LO.. The WHO pandemic influenza preparedness framework: a milestone in global governance for health. JAMA J Am Med Assoc 2011; 306 (2). doi : 10.1001/jama.2011.960 [DOI] [PubMed] [Google Scholar]
- 18. Adalja AA, Bloomberg H, Hopkins J, et al. Priorities for the US health community responding to COVID-19. JAMA 2020; 21202(December 2019): 2019–20. [DOI] [PubMed] [Google Scholar]
- 19. Jennewien C. San Diego County coronavirus developments on Sunday, March 15. Times of San Diego https://timesofsandiego.com/life/2020/03/15/san-diego-county-coronavirus-developments-on-sunday-march-15/
- 20.American Medical Association. 50-state survey: establishment of a patient-physician relationship via telemedicine. 2017.
- 21.Policy C for CH. State Telehealth Laws and Reimbursement Policies Report. 2019.
- 22. Dameff C, Clay B, Longhurst CA.. Personal health records: more promising in the smartphone era? JAMA J Am Med Assoc 2019; 321 (4): 339. [DOI] [PubMed] [Google Scholar]
- 23. Chopra V, Toner E, Waldhorn R, Washer L.. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med 2020; Epub ahead. doi : 10.7326/M20-0907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson. Novel coronavirus outbreak in Wuhan, China, 2020: intense surveillance is vital for preventing sustained transmission in new locations. J Clin Med 2020; doi : 10.3390/jcm9020498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Koonin L. Novel coronavirus disease (COVID-19) outbreak: now is the time to refresh pandemic plans. J Bus Contin Emer Plan 2020; 13 (4): 1–15. [PubMed] [Google Scholar]
- 26.World Health Organization. Pandemic influenza preparedness and response: a WHO guidance document. 2009. [PubMed]
- 27. MacLaren G, Fisher D, Brodie D.. Preparing for the most critically ill patients with COVID-19: the potential role of extracorp1oreal membrane oxygenation. JAMA 2020; doi: 10.1001/jama.2020.2342. [DOI] [PubMed] [Google Scholar]
- 28. Swerdlow DL, Finelli L.. Preparation for possible sustained transmission of 2019 novel coronavirus: lessons from previous epidemics. JAMA 2020; 323 (12): 1129. [DOI] [PubMed] [Google Scholar]
- 29. Wang CJ, Ng CY, Brook RH.. Response to COVID-19 in Taiwan. JAMA 2020; 14–5. [DOI] [PubMed] [Google Scholar]
- 30. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med 2020; 382 (13): 1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kukafka R, Ancker JS, Chan C, et al. Redesigning electronic health record systems to support public health. J Biomed Inform 2007; doi : 10.1016/j.jbi.2007.07.001 [DOI] [PubMed] [Google Scholar]