Abstract
Background
Evaluating whether an infectious disease has reached a turning point is important for planning additional intervention efforts. This study aimed to analyze the changing patterns and the tempogeographic features of the coronavirus disease 2019 (COVID-19) epidemic in China, to provide further evidence for real-time responses.
Methods
Daily data on COVID-19 cases between 31 December 2019 and 26 February 2020 were collected and analyzed for Hubei and non-Hubei regions in China. Observed trends for new and cumulative cases were analyzed through joinpoint regression analysis. Spatial analysis was applied to show the geographic distribution and changing patterns of the epidemic.
Results
By 26 February 2020, 78 630 confirmed COVID-19 cases had been reported in China. In Hubei, an increasing trend (slope = 221) was observed for new cases between 24 January and 7 February 2020, after which a decline commenced (slope = −868). However, as the diagnosis criteria changed, a sudden increase (slope = 5530) was observed on 12 February, which sharply decreased afterward (slope = −4898). In non-Hubei regions, the number of new cases increased from 20 January to 3 February and started to decline afterward (slope = −53). The spatial analysis identified Chongqing, Guangzhou, Shenzhen, Changsha, Nanchang, Wenzhou, Shanghai, Xinyang, Jining, and Beijing as the hotspots outside of Hubei Province in China.
Conclusions
The joinpoint regression analysis indicated that the epidemic might be under control in China, especially for regions outside of Hubei Province. Further improvement in the response strategies based on these new patterns is needed.
Keywords: COVID-19, geospatial pattern, epidemiological pattern, hotspot
The epidemic of COVID-19 reached the turning point in Hubei and non-Hubei regions on 14 February and 3 February, respectively, and the epidemic is under control in non-Hubei regions of China. The hotspots are in areas close to Hubei and the metropolitans.
In December 2019, a new coronavirus disease (COVID-19) emerged in Wuhan City located in central China’s Hubei Province, infecting 81 548 people (78 630 cases are in China and 2918 in 37 other countries) by 26 February 2020 and leading to the death of 2747 people in China [1, 2]. The high transmission rate (R0 = 2.2 [range, 1.4–3].9) and long incubation period (average, 6.4 days [range, 2.1–11.1 days) of the virus coupled with its relatively high mortality rate (2%) made it a global public health emergency event [3–6]. The situation is further compounded by the high number of presumed hospital-acquired infections and the potential for secondary transmission through asymptomatic contacts [4–8].
In response to this epidemic, China issued rapid and comprehensive public health emergency interventions at the national level; upgraded quarantine and isolation guidelines; and expanded its Level 1 Public Health Emergency Response to 31 provinces within mainland China. All provinces issued the highest level of emergency public health alerts and responses within the national public health management system, and cities with high numbers of reported cases went under lockdown with restricted access in most of their communities as part of preventive measures. Due to the high probability of the virus causing a global pandemic, the World Health Organization (WHO) on 30 January 2020 declared the COVID-19 outbreak a Public Health Emergency of International Concern [9].
The Chinese government continued to act and implement containment and preventive measures in the global public best interest by reporting the epidemic and improving transparency in data reporting. The ever-increasing flow of information freely available and easily accessible online has allowed the public to understand the emerging epidemic status and the need for compliance. The data have also provided a great opportunity for researchers and public authorities to better understand the epidemic trends, predict the disease patterns, and provide technical support through data analysis. Moreover, the data provided a better understanding of how severe acute respiratory syndrome coronavirus (SARS-CoV-2) spread temporally and geographically.
This study aimed to assess the turning point (which in this study was defined as the time when the rate of case accumulation changed from increasing to decreasing or vice versa) of the epidemic. The study also aimed to identify the tempogeographic patterns of the epidemic at the city, provincial, and national levels and to analyze the changing patterns of the infection.
METHODS
Data Collection and Processing
Multiple publicly available data were collected for this data analysis. Daily data on COVID-19 in China were derived from the national and provincial health commissions’ websites (http://www.nhc.gov.cn/) [1]. To reflect the entire process of the outbreak, the data were systematically collected from 31 December 2019, when the Hubei health commission first reported about an unknown pneumonia, till 26 February 2020. The measures collected from these sources included the report date; the number of new cases reported per day; the cumulative number of cases per day; and the cumulative number of deaths per day at the city, provincial, and national levels. Where only cumulative cases were reported by dates, the daily reported number of new cases was estimated by computing the difference between cumulative reported cases in the new day and the previous day. The number suspected cases in Hubei were collected from 8 February 2020 to 26 February 2020. The number of cumulative cases and deaths outside of China on 26 February 2020 were obtained from the WHO’s situation reports [2]. The spatial data on China were from GADM version 3.6 [10]. All of these data sources are freely accessible to the public.
Data Analysis
All the statistical analyses were conducted using RStudio software (R Core Team, 2016) and Joinpoint Trend Analysis version 4.7.0.0 software (US National Cancer Institute). The maps and spatial analysis were generated using ArcGIS 10.2 software (Esri Inc, Redlands, California). Mortality rate was defined as the proportion of deaths in confirmed cases during the study period and was calculated and compared by region (Hubei, China; non-Hubei, China; overall in China; and the rest of the world).
Because Hubei Province, as the center of the COVID-19 outbreak, had more reported cases, we hypothesized that its disease trend might differ from non-Hubei regions. Therefore, joinpoint regression was applied to analyze the trends of new and cumulative cases for Hubei and non-Hubei regions and to obtain the dates of the outbreak changing points. Trend analysis of suspected cases was calculated for Hubei Province as the disease diagnosis criteria was changed on 12 February for the region and multiple joinpoints were used to reflect the infection in stages to showcase the changing epidemic patterns.
Dynamic maps of new and cumulative cases for Hubei Province were created by grouping the number of COVID-19 cases into 8 classes based on natural breaks to help visualize the distribution change by city. Spatial autocorrelation analysis and hotspot analysis were applied to examine the presence of epidemic clusters and detect non-Hubei areas that are at high risk. Tibet, which had recorded only 1 COVID-19 case, was excluded from the spatial analysis. Clustering of COVID-19 was considered present if the Moran I index was > 0 and P was < .05 in the spatial autocorrelation analysis. In the hotspot analysis, the conceptualization of spatial relationship was set to inverse distance with the hypothesis that areas with smaller distance have a higher impact on the calculated field. The z score, P value, and Gi_Bin were calculated in the hotspot analysis. High z score with P values < .01, <.05, and <.1 indicated a hotspot. The area where Gi_Bin = 3 was the hotspot with 99% confidence; Gi_Bin = 2 was hotspot with 95% confidence; Gi_Bin = 1 was hotspot with 90% confidence; and Gi_Bin = 0 was classified as not significant.
RESULTS
By 26 February, a total of 78 630 COVID-19 cases had been reported in China and 2918 in 37 other countries.
Changing Trend of the Epidemic
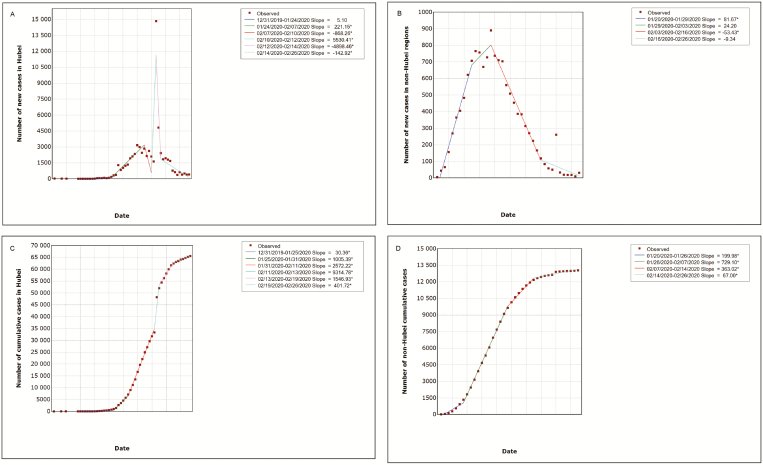
The joinpoint regression in this study was separated into 2 parts: (1) cases found in Hubei Province and (2) cases outside Hubei Province in China (Figure 1A–D).
Figure 1.
Joinpoint regression analysis for coronavirus disease 2019 cases reported in China between 31 December 2019 and 26 February 2020. A, Number of new cases found in Hubei varies with date elapsed from 31 December 2019. B, Number of new cases found in non-Hubei region of China varies with date elapsed from 20 January 2020. C, Number of cumulative cases found in Hubei varies with date elapsed from 31 December 2019. D, Number of cumulative cases found in non-Hubei region of China varies with date elapsed from 20 January 2020. *Slope is significantly different from zero at α = .05 level. Dates are presented as month/day/year.
The joinpoint regression for daily reported new cases showed 2 trends for new cases found in Hubei Province and non- Hubei regions in China (Figure 1A and 1B). The overall trend for new cases in Hubei Province increased very slowly at the beginning of the outbreak until 24 January 2020 (slope = 5) and started a fast increase until the first peak was reached around 7 February (slope = 221), after which it started to decrease (slope = −868). However, a sudden peak in the trend was observed with 14 840 new cases on 12 February 2020, as the disease diagnosis criteria were changed (from laboratory-based confirmation to clinical diagnosis; Figure 1A) for Hubei Province. The number then returned to 2420 on 14 February and continued to decrease to 409 on 26 February 2020 (slope = 143). Regions outside Hubei Province observed a different disease pattern as the trend for daily reported new cases rapidly increased after the new cases were reported on 20 January 2020 for the first time (slopes = 82). The increase of new cases became relatively slow after 29 January (slope = 24) and reached a peak on 3 February 2020. The number of newly reported cases in the regions quickly declined after the peak (slope = −53; see Figure 1B) and was < 100 in most days after 16 February 2020, when the decreasing trend of new cases became gentle (slope = −9). The cumulative cases showed increasing but different trends for both Hubei Province and non-Hubei provinces in China. The trend for Hubei Province stayed relatively stable from 31 December 2019 to 25 January 2020, with a slope of 30 (Figure 1C), and the number of cumulative cases kept accelerating in the next 3 stages (slope = 1005 in stage 2, slope = 2572 in stage 3, and slope = 9315 in stage 4) until 13 February 2020 (slope = 1547). The increase further slowed after 19 February 2020 (slope = 402). The trend for the cumulative cases outside Hubei Province in China behaved similarly in growth (trend slope increased from 200 in stage 1 to 729 in stage 2) to but more gentle than that of Hubei Province in stages 2 and 3 (Figure 1D); however, it changed at the third stage as the increasing trend of cumulative cases started to decelerate after 7 February 2020 (slope = 363), which was about 1 week before the trend in Hubei started to slow down; the increase of cumulative cases was gentle after 14 February 2020 (slope = 67).
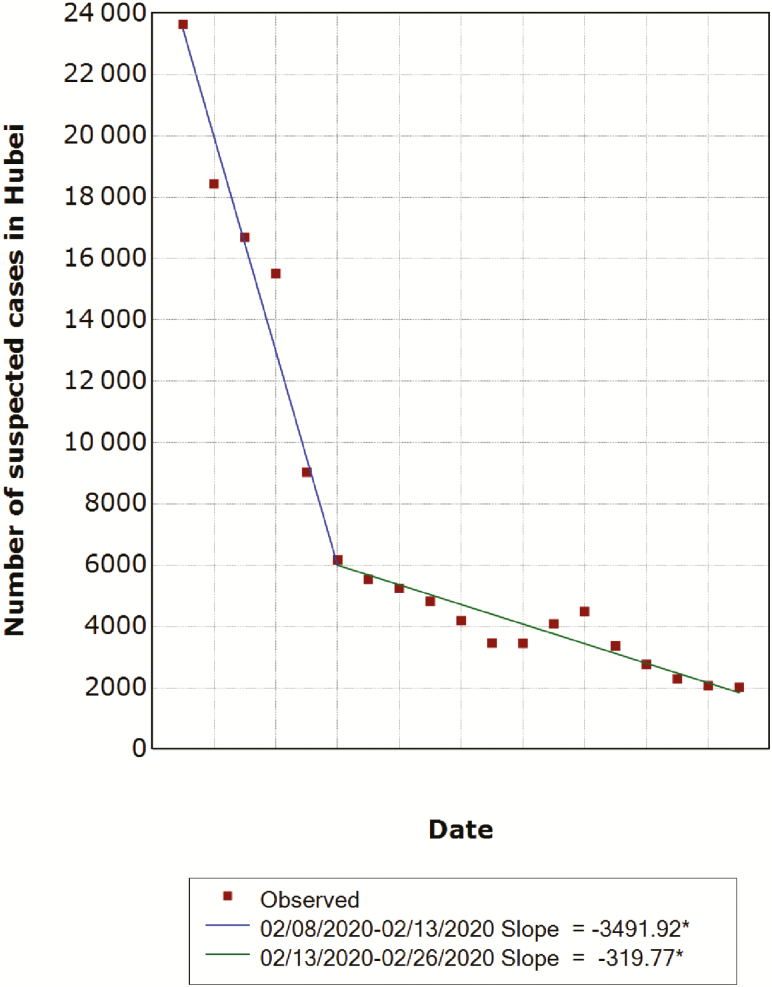
Suspected cases for Hubei showed a rapid decreasing trend from 8 February 2020, and the decrease slowed down after 13 February 2020 (Figure 2). The number of new cases also decreased in general after 9 February 2020, except on 12 February 2020, when the new cases rapidly increased and suspected cases largely decreased. The decreasing trends of both new and suspected cases in Hubei imply that the disease outbreak may be controlled gradually. However, as the number of new cases and suspected cases were still above 400 and 2000 on 26 February 2020, respectively, more efforts are needed to further reduce COVID-19 infection.
Figure 2.
Joinpoint regression analysis for coronavirus disease 2019 cases reported in China between 8 February and 26 February 2020. *Slope is significantly different from zero at α = .05 level. Dates are presented as month/day/year.
Disease Mortality
The mortality rate for COVID-19 in Hubei Province, non-Hubei regions in China, overall China, and regions outside of China were 4.0%, 0.8%, 3.5%, and 1.5%, respectively (Table 1). It is noteworthy that the mortality rate in non-Hubei regions in China and outside of China was much cumulatively lower than that in Hubei and that China’s national mortality rate was highly impacted by Hubei’s (Supplementary Materials 1).
Table 1.
Mortality Rate of Coronavirus Disease 2019 (COVID-19) in Hubei Province, China, and Other Countries, by 26 February 2020
| Region | Confirmed Cases | Mortality | Mortality Rate |
|---|---|---|---|
| Hubei Provincea | 65 596 | 2641 | 4.0% |
| Non-Hubei regions in China (including Hong Kong, Macau, and Taiwan)a | 13 034 | 106 | 0.8% |
| Overall in China | 78 630 | 2747 | 3.5% |
| Outside of Chinab | 2918 | 44 | 1.5% |
aData collected from the COVID-19 daily report of the National Health Commission of the People’s Republic of China.
bData collected from the COVID-19 situation report of the World Health Organization.
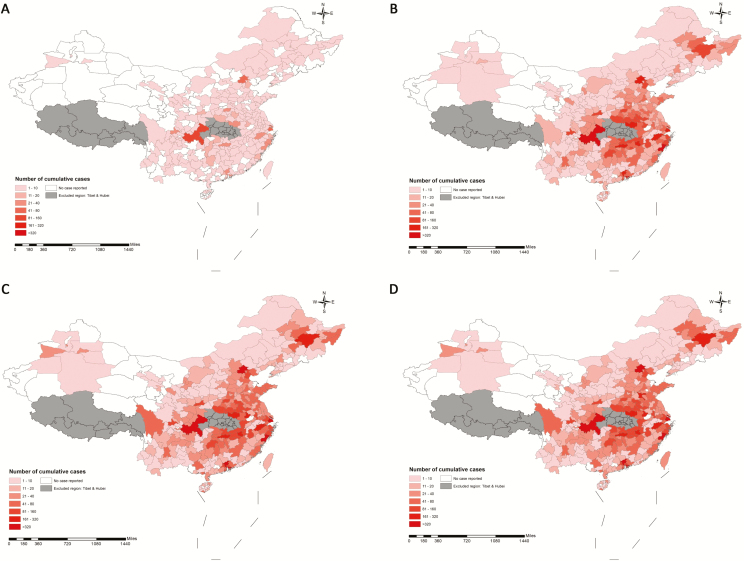
Spatial Pattern of COVID-19 Outbreak
Dynamic maps of Hubei were produced to show the new cases and cumulative cases changing patterns over time (Supplementary Materials 2 and 3). Huanggang, a neighboring city of Wuhan that recorded 12 cases on 20 January 2020, was the first city to record a case outside Wuhan. All other cities started to report new cases from 21 to 27 January 2020, and new cases reported in Wuhan rapidly increased after 26 January 2020, followed by Huanggang, Xiaogan, and other nearby cities. However, Qianjiang, Tianmen, and Xiantao, which are also near Wuhan, were not affected as severely as the other neighboring cities. The number of new cases in each city was < 42 from 20 February, except for Wuhan; furthermore, > 4 cities reported zero new cases every day since 22 February 2020. Joinpoint analysis identified the changing points for cumulative cases in the non-Hubei region to be 26 January, 7 February, and 14 February, and these data in addition to 26 February were used to develop a series of distribution maps to showcase the development of the disease outbreak. A few areas near Hubei and in east China reported COVID-19 cases in stage A (26 January 2020; Figure 3A) and later evolved into stage B (7 February 2020; Figure 3B) by spreading to most of east China. In stage B, the disease spread throughout the country but with < 20 cases in many cities except for parts of northwest China that were unaffected. More cases were found in areas near Hubei, especially Chongqing, where 426 people were infected. Some distant cities from Hubei, such as Guangzhou, Shenzhen, Wenzhou, Shanghai, and Beijing, were also highly affected with > 160 cases in each city, especially Wenzhou, where 438 people were infected. The number of cumulative cases in the areas near Hubei and highly affected cities gradually and slightly increased when the outbreak evolved into stage C (14 February 2020) and Stage D (26 February 2020), and all unaffected areas except Yichun in Heilongjiang Province remained safe (Figure 3C and 3D). This evidence indicated that although the disease rapidly spread at the beginning, preventive control was achieved.
Figure 3.
Distribution maps of cumulative coronavirus disease 2019 (COVID-19) cases in non-Hubei regions. A, Distribution of cumulative cases in non-Hubei regions by 26 January 2020. B, Distribution of cumulative cases in non-Hubei regions by 7 February 2020. C, Distribution of cumulative cases in non-Hubei regions by 14 February 2020. D, Distribution of cumulative cases in non-Hubei regions by 26 February 2020.
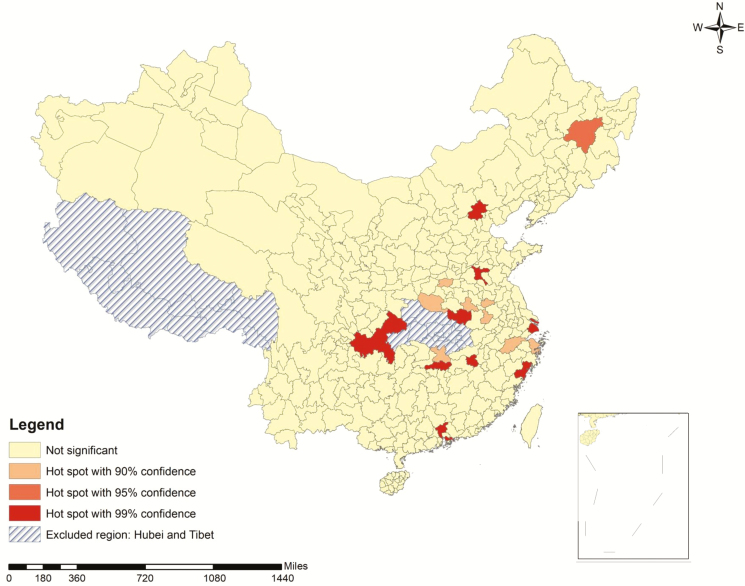
In spatial autocorrelation analysis for non-Hubei regions (Tibet excluded), the Moran I index was 0.13 (P < .01), demonstrating that the epidemic clusters of COVID-19 were present. The hotspot analysis (Figure 4) indicated Chongqing, Guangzhou, Shenzhen, Changsha, Nanchang, Wenzhou, Shanghai, Xinyang, Jining, and Beijing to be epidemic hotspots with about 99% confidence, meaning that these cities were at high risk during the disease outbreak. Harbin was the hotspot with 95% confidence and at relatively high risk. Hangzhou, Hefei, Yueyang, Zhengzhou, Ningbo, Bengbu, Fuyang, and Nanyang were also hotspots with 90% confidence and moderate risk of the disease.
Figure 4.
Map of hotpot analysis in non-Hubei regions of China.
DISCUSSION
Knowing the epidemic patterns of an infectious disease is important in the planning of public health responses. As the spread of COVID-19 trigged the highest level of global emerging response, especially in China, understanding the real-time patterns of the epidemic would be useful for guiding further time-sensitive responses. This study extended the existing literature by conducting assessment of the changing patterns of the epidemic, detecting the turning points of the outbreak, and analyzing the tempogeographic pattern of the infection.
Our findings indicated that a turning point of the epidemic may have been reached in both Hubei and non-Hubei regions in China, as evidenced by the overall decreasing trend of newly confirmed cases both in and outside Hubei Province. In Hubei Province, there was a sudden increase of the number of newly identified cases, which delayed the reaching of a turning point. However, the sudden increase in the number of confirmed cases was mainly due to a change in the diagnosis criteria of COVID-19 for the province (changed from laboratory-confirmed cases only laboratory-confirmed plus to clinically diagnosed cases since 12 February 2020) [11] to facilitate early treatment and care for suspected cases and to prevent secondary transmission. Without the observed sudden spike on 12 February 2020, the turning point may have been reached on 8 February. Nevertheless, all of these indicators suggest that the epidemic in China has been turning for the better since 14 February 2020.
However, reaching a turning point for an epidemic does not necessarily signify the end of the epidemic as secondary transmission of SARS-CoV-2 continues in China and worldwide. Thus, the need for improved efforts to reduce the timeline from case identification to confirmation still remains urgent. Also, efforts to strengthen quarantine and isolation procedures in areas with a serious epidemic are continually required. Differentiated prevention efforts should be implemented depending on a region’s epidemic level. For example, areas with relatively low numbers of or no SARS-CoV-2–infected cases should implement strategies aimed at reducing the impact of the epidemic on the economy and encouraging people to resume normal daily life activities. Future studies should aim to evaluate the impact of the de-quarantine and de-isolation strategies in these areas.
A distinct epidemiological pattern of the COVID-19 epidemic between Hubei Province and other regions in China was also observed. For example, while the turning point may have been reached by 3 February for non-Hubei regions, Hubei Province reached this much later and recorded yet another peak on 12 February 2020 [11]. Reasons that may have led to this situation include the fact that Hubei Province, as the center of the outbreak with > 80% of reported confirmed cases, faced the worst impact of the epidemic and recorded higher mortality rates than other regions [12]. Secondary transmission in the region was also hard to control as more time and effort were required to curb the epidemic. Furthermore, prevention reaction to the outbreak was slow at the outset as public health authorities in Hubei Province underestimated the potential of the virus and did not fully react even after hundreds of cases had been identified. Due to this slow reaction, the opportunity for timely prevention of secondary transmission was missed, which in turn led to the global epidemic. The slow reaction time also seriously handicapped the health system of Hubei Province as > 1700 healthcare workers became infected, thereby reducing available medical resources for epidemic control in the region. Other provinces, however, learnt from Hubei’s experiences and reacted early by issuing Level 1 public health emergency responses. These drastic measures enabled those regions to reach an early turning point during the epidemic before SARS-CoV-2 could spread further within their regions.
In terms of non–Hubei Province hotspots, Chongqing, Guangzhou, Shenzhen, Changsha, Nanchang, Wenzhou, Shanghai, Xinyang, Jining, and Beijing were found to be the epidemic hotspots. These cities were prone to being hotspots as they are either close to Hubei Province or are in mega-metropolises in China (especially for Chongqing, Shanghai, and Shenzhen), with > 10 million residents. Thus, even though large amounts of prevention efforts were instituted in these hotspots, the SARS-CoV-2 prevention and control burden is still extremely high in these regions. As such, even after the complete elimination of the infection, preventive measures will still be required to minimize the probability of any future epidemic relapse. Additionally, public health authorities in these regions should further investigate cases to better understand the facilitating factors of ongoing transmission in these areas.
This study has some limitations. First, as all of the data were from publicly available sources, we lacked detailed information on patients, which prevented us from further assessing the potential driving forces of the epidemic. Second, there is a time gap between a suspected case identification and case confirmation. Therefore, our analysis may not reflect the real-time situation of the epidemic; however, it still provides time-sensitive information, useful as evidence to aid in further response to the epidemic. Finally, due to the changes in diagnostic criteria for Hubei Province on 12 February 2020, the data reported before and 12 February 2020 onward may not be consistent with each other.
In summary, our study indicated that the turning point of the COVID-19 epidemic in China may have been reached in both Hubei and the non-Hubei regions in China. However, continuous prevention efforts are still needed to achieve total elimination, and tailored strategies should be implemented in regions with different epidemiological patterns.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors thank everyone who contributed to this study, especially the study participants.
Disclaimer. The funders had no role in the study design, data collection and analysis, preparation of the manuscript, or decision to submit the manuscript for publication.
Financial support. This work was supported by the National Key Research and Development Program of China (grant number 2017YFE0103800); National Institutes of Health (grant number R34MH119963); National Science and Technology Major Project (grant number 2018ZX10101-001-001-003); Special Found on Prevention and Control of New Coronary Pneumonia in Guangdong Universities (2020KZDZX1047); and the National Natural Science Foundation of China (grant number 81903371).
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. China’s National Health Commission. Epidemic nofitication. 2020. Available at: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. Accessed 20 April 2020.
- 2. World Health Organization. Coronavirus disease (COVID-19) situation reports. 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 11 April 2020. [Google Scholar]
- 3. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill 2020; 25:2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chang D, Lin M, Wei L, et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China [manuscript published online ahead of print 7 February 2020]. JAMA 2020. doi:10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lai S, Bogoch I, Ruktanonchai N, et al. Assessing spread risk of Wuhan novel coronavirus within and beyond China, January-April 2020: a travel network-based modelling study. Preprint [posted online 9 March 2020]. medRxiv 2020. 10.1101/2020.02.04.20020479. [Google Scholar]
- 6. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China [manuscript published online ahead of print 7 February 2020]. JAMA 2020. doi:10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Statement on the second meeting of the International Health Regulations (2005) emergency committee regarding the outbreak of novel coronavirus (2019-nCoV). Geneva, Switzerland: WHO, 2020. [Google Scholar]
- 10. Global administrative areas (boundaries). GADM maps and data. University of Berkeley, Museum of Vertebrate Zoology and the International Rice Research Institute, : 2020. [Google Scholar]
- 11. National Health Commission, People’s Republic of China. February 13: daily briefing on novel coronavirus cases in China. 2020. Available at: http://en.nhc.gov.cn/2020-02/13/c_76512.htm. [Google Scholar]
- 12. Johns Hopkins University Center for Systems Science and Engineering. Coronavirus COVID-19 global cases. Baltimore, MD: Johns Hopkins University; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.