ADDITIONAL CONTENT
An author video to accompany this article is available at: https://academic.oup.com/ndt/.
The acute crisis with the coronavirus disease of 2019 (COVID-19) caused by the novel coronavirus Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-COV-2) is the largest biomedical catastrophe of our lifetimes. Like so many other disasters in the past, such as war, famine, social unrest and economic calamities, this too shall pass, but it will undoubtedly leave the world changed. Some of the changes are already evident, but some are inevitable once we get over this pandemic. In this perspective, I provide examples of how the virus is already inducing change in the practice of medicine at large and for nephrology in particular. As is true for many changes, some persist after the emergency is over, so I speculate on how nephrology may change once we surmount this predicament (Figure 1).
FIGURE 1.
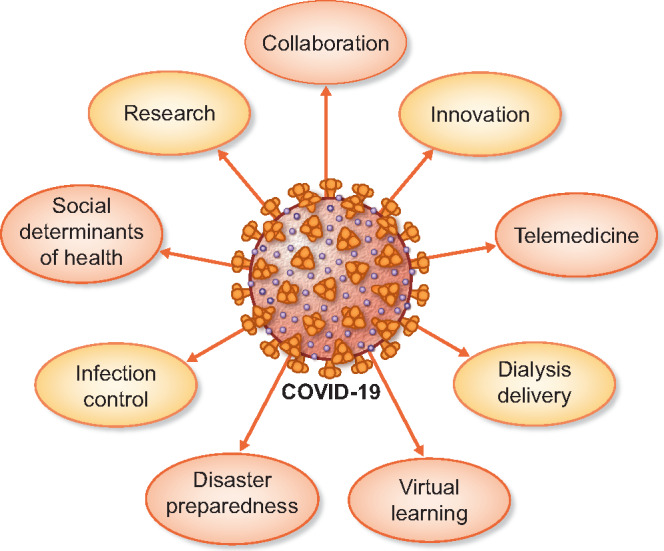
Coronavirus—devastation or a new dawn for nephrology?
COLLABORATION
In the worldwide fight against an invisible enemy, the world has learned incredible new ways to collaborate. Within days after the epidemic unfolded in North America, two young physicians, Matthew Sparks and Swapnil Hiremath, curated an annotated resource for use by nephrologists [1]. With a group of colleagues, they were among the first to address the question of whether angiotensin-converting enzyme inhibitors or angiotensin receptor blockers should be stopped in patients who are taking these drugs. Their answer—which was to continue to take these medications—was later supported both by a statement from the European Society of Cardiology [2] and a scholarly review in the New England Journal of Medicine [3]. In the context of the epidemic, under the umbrella of the World Health Organization, a large randomized worldwide trial was launched to evaluate outcomes of various drug regimens [4]. Medical journals collaborated with their readers. For example, JAMA sent out a call for ideas to conserve personal protective equipment, which was in short supply [5]. Engineers and physicians collaborated both at Oxford, UK [6] and at the Massachusetts Institute of Technology (MIT), Cambridge, MA, USA [7] to innovate low-cost ventilators that they made open source. The fight against the virus made humans unite, collaborate and forget their differences—it was a demonstration of global solidarity.
INNOVATION
As noted above, a ventilator for $100 with an open-source design developed by a team at MIT is an example of innovation that had the potential to impact respiratory failure in low- and middle-income countries. The virus brought the most innovative ideas to the forefront. The first set of tests required to detect COVID-19 required hours and sometimes days to be reported. This was impeding the fight against the virus. Abbott Diagnostics, a Chicago-based company, established a rapid test that could be performed using a point-of-care device, most units of which were already in use in urgent care facilities, where they were used to diagnose influenza A and B, Strep A and respiratory syncytial virus [8]. A positive test could be available in 5 min and a negative test in 13 min. A low-cost COVID-19 test was developed in India and the team was led by a woman in late-stage pregnancy; she delivered a baby soon after submitting the test for approval [9]. The cost of this test was one-third of what was being paid from tests coming from outside the country.
During the COVID-19 pandemic, a company that makes Internet-connected thermometers created a map of the USA by zip code to monitor influenza-like illness [10]. The aggregate, anonymized map provides different levels of information. Areas where illness is unusually high indicate early indicators of COVID-19 spread. Trends are color coded to visualize whether school closures and social distancing are working. This innovation has the potential to transform the health of dialysis patients.
Monitoring the health of entire dialysis units across the country is possible and desirable. With the large wealth of vital sign and temperature data within each dialysis unit, such anonymized monitoring may signal early changes in the health of the unit. Each 1% increase in quarterly influenza-like illness associates with a 1.5–2.0% increase in all-cause mortality among dialysis patients. These mortality rates are similar to mortality estimates for COVID-19 in the general population. Accordingly, such surveillance efforts may be particularly valuable to institute measures similar to those implemented in the COVID-19 pandemic [11]. Sharing of such data will need a national plan and should cross boundaries of data ownership for societal good. Extending this further, longitudinal data for individual patients using the algorithms of artificial intelligence may even provide diagnostic information for patients and serve as an early sign of infection or a cardiovascular event.
TELEMEDICINE
The fight against COVID-19 was not just against the virus. The deliberate actions taken by large healthcare systems to fight the virus created another problem. In the face of the pandemic, most routine medical services were suspended. Because of the lack of access to routine medical care, patients with chronic illnesses were now exposed to potential harm. COVID-19 was pushing all other diseases by the wayside, and telemedicine rapidly emerged. Many of the rules that would have taken years to be approved were passed almost overnight. Visits to patients using cameras next to the dialysis machine or by phone were rapidly adopted. Many practices started seeing patients by telehealth visits.
Could this drive a change in the system? Will patients want to see their doctor in person or on camera? Or could we have a hybrid system where many visits might be via telehealth and a few in person. The answers to these questions are complex and may be decided by organizations that pay for these services. If insurance companies pay for these services at a lower rate, but this lower rate is offset by an increase in volume, it may drive more telemedicine in the future. However, the behaviors of physicians and patients will also decide if these changes are transient or more secular.
DIALYSIS DELIVERY
COVID-19, being a droplet-borne viral infection, necessitated social distancing and required patients to be dialyzed in a manner that reduced the risk of viral transmission to other dialysis patients in the same unit. One option was to dialyze such patients at home. Thus home-based systems—instead of in-center dialysis requiring centralized water delivery systems—may emerge. Receiving self-care dialysis during catastrophes may make more sense for our patients and may enter the lexicon when planning care for patients reaching end-stage renal disease. Patients may therefore lean toward home therapies such as peritoneal dialysis or home hemodialysis, instead of in-center dialysis.
The increase in patients with multi-organ failure requiring acute dialysis posed another challenge to the system. Acute peritoneal dialysis has not been adopted in dialysis units, but the scarcity of resources led to resurrection of a technique that had almost been forgotten. Low-volume continuos veno-venous hemofiltration (CVVH) delivery was adopted due to the adequate supply of replacement solutions. Whether such interventions help or hurt can only be answered by future analyses, and even then, causality would be difficult to deduce. However, such data may challenge the paradigm of high-volume CVVH currently practiced.
The push to monitor the patient remotely without entering the room was acutely felt during this epidemic. Baby monitors were installed in patient's rooms to communicate with patients. Given that acute respiratory distress syndrome was an important feature of the disease, the need to monitor vital signs was never felt more acutely. These needs may drive innovation in remote monitoring systems that may benefit dialysis patients directly by noninvasively monitoring the hemodynamic state on a beat-to-beat basis.
VIRTUAL LEARNING AND CONFERENCES
Virtual learning became the norm for entire universities—almost overnight—and there was no time to prepare. Local teaching conferences were often held by videoconferencing. Large conferences, for example, the National Kidney Foundation and ERA-EDTA, became fully virtual. These unprecedented changes provide new opportunities for hybrid conferences, where a mix of virtual and physical conferences may happen. Such virtual conferences have the potential to allow participation of physicians from low- and middle-income countries and for those unable or unwilling to travel.
DISASTER PREPAREDNESS
The Ebola virus epidemic was a wake-up call for disaster preparedness, but it did not gain traction because of its limited impact on society. The COVID-19 pandemic is so widespread that disaster preparedness is inevitable. Like the fire drill, we may well have drills for such disasters in the future.
A stockpiling of personal protective equipment, N95 respirators and surgical masks and engineering controls are bound to emerge. While stockpiling may be necessary, it should not be reactive and should be carefully considered. For example, it may be more sensible to have such stockpiles at a national or state level in order to conserve resources.
Preparedness by dialysis chains to dedicate units or areas for such emergencies will emerge. Reduced reliance on central water delivery systems and increased performance of dialysis in individual rooms with the aid of innovative machines such as one that uses a cartridge to remove toxins is also likely [12].
Disaster preparedness would be remiss if it did not consider an equitable distribution of healthcare workforce resources during a pandemic. A global response to the availability of physicians, nurses, dialysis technicians and other providers would smooth out shortages. For example, if Italy faces a shortage of medical personnel, there should be a pool of physicians and providers who would be available to address this shortage from other countries. The medical licensing boards are likely to change in the face of this crisis.
INFECTION CONTROL
Nephrologists and other healthcare workers became acutely aware of social distancing; donning and doffing masks, gloves and gowns; and hand hygiene. Behaviors learned in the time of crisis were closely followed not just to protect patients, but also the health of the caregiver. Hand hygiene, discovered by the Hungarian physician Ignaz Semmelweis >150 years ago, is not universal among healthcare workers. However, this behavior is likely to stay. If so, we can expect to see a decrease in preventable infections such as exit-site infections, catheter-related bacteremia and peritonitis.
SOCIAL DETERMINANTS OF HEALTH
Homelessness, hunger and job insecurity are important determinants of health outcomes. The marginalized in society were not only exposed to a greater risk of COVID-19, but also had a greater barrier to receive medical attention due to the closure of routine visits. Social distancing taxed the shelters in which they were housed. Maps were created for the entire USA based on social determinants of health to identify populations at greater risk for COVID-19 [13]. Medical students in Pittsburgh volunteered to deliver medications at home [14]. In the state of California, with an estimated 130 000 homeless, many were provided with hotel rooms or trailers [15]. The impact of the homeless on society was never felt more acutely than at the time of the pandemic. COVID-19 induced a change in societal attitudes toward the homeless overnight. Will this change in societal attitudes and approaches to health persist after the crisis is over? We can hope so.
RESEARCH
Some changes are already evident. For example, the Food and Drug Administration issued new guidance for research during the pandemic and approved diagnostic tests in a matter of days. It also approved within a matter of days emergency use authorization for the use of imported anesthesia gas machines modified for use as ventilators. Trials of vaccines and drugs were fast-tracked. But the future of research is moot.
In a 2015 Ted Talk, 'The next outbreak? We’re not ready', Bill Gates speculated rather accurately that it is not a nuclear disaster but a virus that will kill more of humanity [16]. Yet globally, the allocation of national budgets to healthcare is often a fraction of defense budgets. If our society recognizes that a more realistic enemy we face is an infection—and not a nuclear war—it may dedicate more resources to healthcare as a deterrent to this calamity. If we so decide, then the resources to study and prevent such pandemics are the most likely beneficiaries. Hopefully there will be the political will to bolster the healthcare infrastructure, including research funding that is needed to predict, prevent and fight not only such pandemics, but also diseases such as chronic kidney disease that claim more lives than a pandemic.
CONCLUSIONS
When the pandemic is over, we will remember the vulnerability we faced, but perhaps more important we will remember the humility, courage and compassion that we witnessed. Our respect for people will grow, especially those who worked the frontlines, such as dialysis technicians, nurses and allied health workers, ambulance drivers and environmental health workers. They showed up for work every day to take care of patients who were fighting the virus. We will recognize that we could not have surmounted this pandemic alone; we needed their assistance. We will recognize and respect those who showed us the way forward, the people who forecasted the number of days for lockdowns and social distancing and those who made the critical decisions to keep society safe. We will also remember those who separated the fake news from real science with their scientific knowledge. For example, the social media amplification of COVID-19 was enormous and fact-checking by those trained in research methods and interpretation could inform the public about propaganda or false claims.
This is not the last time that the human race will face a pandemic. What we learn from this pandemic will decide how prepared we will be to face the next one. The answer to the question posed in the title is speculative, but I predict that Coronavirus will induce a rapid change in nephrology. In the end, we may wonder if all that was left behind by Corona was death and destruction—an eclipse—or was it a vibrant halo. In my view, nephrology will emerge stronger and better if we display the same solidarity we did while we fought the virus.
FUNDING
R.A. is supported by a National Institutes of Health grant (5 R01 HL126903-05) and a grant from VA Merit Review (1 I01 CX001753-01A1).
CONFLICT OF INTEREST STATEMENT
R.A. has the following disclosures: member data safety monitoring committees: AstraZeneca, Ironwood Pharmaceuticals; member steering committees of randomized trials: Akebia, Bayer, Janssen, GlaxoSmithKline, Relypsa, Sanofi and Genzyme; member adjudication committees: Bayer, Boehringer Ingelheim, Janssen; member scientific advisory board or consultant: Celgene, Daiichi Sankyo, Eli Lilly, Relypsa, Reata, Takeda Pharmaceuticals USA, ZS Pharma.
REFERENCES
- 1. Sparks M, Hiremath S.. Living Resource for Nephrologists during the COVID-19 Pandemic 2020. http://www.nephjc.com/covid19 (28 March 2020, date last accessed)
- 2. Simone D. G: Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers 2020. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (31 March 2020, date last accessed)
- 3. Vaduganathan M, Vardeny O, Michel T. et al. Renin angiotensin aldosterone system inhibitors in patients with Covid-19. N Engl J Med; doi:10.1056/NEJMsr2005760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kupferschmidt K, Cohen J.. Race to find COVID-19 treatments accelerates. Science 2020; 367: 1412–1413 [DOI] [PubMed] [Google Scholar]
- 5. Bauchner H, Fontanarosa PB, Livingston EH.. Conserving supply of personal protective equipment–a call for ideas. JAMA 2020; 10.1001/jama.2020.4770 [DOI] [PubMed] [Google Scholar]
- 6. OxVent: A Collaboration for COVID 19 Ventilation 2020. http://oxvent.org (31 March 2020, date last accessed)
- 7. MIT E-Vent | MIT Emergency Ventilator: Emergency Ventilator Design Toolbox 2020. https://e-vent.mit.edu/ (31 March 2020, date last accessed)
- 8. Abbott Launches Molecular Point-of-Care Test to Detect Novel Coronavirus in as Little as Five Minutes 2020. https://abbott.mediaroom.com/2020-03-27-Abbott-Launches-Molecular-Point-of-Care-Test-to-Detect-Novel-Coronavirus-in-as-Little-as-Five-Minutes (31 March 2020, date last accessed)
- 9. Pandey G. BBC News–Coronavirus: The Woman behind India’s First Testing Kit 2020. https://www.bbc.com/news/world-asia-india-52064427 (31 March 2020, date last accessed)
- 10. Kinsa Insights: US Health Weather Map 2020. https://healthweather.us/ (31 March 2020, date last accessed)
- 11. Gilbertson DT, Rothman KJ, Chertow GM. et al. Excess deaths attributable to influenza-like illness in the ESRD population. J Am Soc Nephrol 2019; 30: 346–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Outset: It Looks Different. But that’s Just the Beginning https://www.outsetmedical.com/tablo/ (31 March 2020, date last accessed)
- 13. Pennic F. New COVID-19 Community Vulnerability Map Uses Social Determinants of Health to Identify Populations at Greater Risk 2020. https://hitconsultant.net/2020/03/24/covid-19-community-vulnerability-map (31 March 2020, date last accessed)
- 14. Pitt Med Students Step Up to Deliver Life-Sustaining Medication https://pittwire.pitt.edu/news/pitt-med-students-step-deliver-life-sustaining-medication (31 March 2020, date last accessed)
- 15. Kendall M. Safe from Coronavirus? Dozens of Bay Area Homeless Move into Hotels to Ride Out Pandemic. But Thousands More Remain on the Streets 2020. https://www.mercurynews.com/2020/03/27/safe-from-coronavirus-dozens-of-homeless-move-into-hotels-to-ride-out-pandemic/ (31 March 2020, date last accessed)
- 16. Gates B. The Next Outbreak? We’re Not Ready 2015. https://www.ted.com/talks/bill_gates_the_next_outbreak_we_re_not_ready (31 March 2020, date last accessed)


