Abstract
Purpose
To report functional mobility in patients with diplegic cerebral palsy (CP) at long-term follow-up after single-event multilevel surgery (SEMLS). The secondary aim was to assess the relationship between functional mobility and quality of life (QoL) in patients previously treated with SEMLS.
Methods
A total of 61 patients with diplegic CP, mean age at surgery 11 years, eight months (sd 2 years, 5 months), were included. A mean of eight years (sd 3 years, 10 months) after SEMLS, patients were contacted and asked to complete the Functional Mobility Scale (FMS) questionnaire over the telephone and given a weblink to complete an online version of the CP QOL Teen. FMS was recorded for all patients and CP QOL Teen for 23 patients (38%).
Results
Of patients graded Gross Motor Function Classification System (GMFCS) I and II preoperatively, at long-term follow-up the proportion walking independently at home, school/work and in the community was 71% (20/28), 57% (16/28) and 57% (16/28), respectively. Of patients graded GMFCS III preoperatively, at long-term follow-up 82% (27/33) and 76% (25/33) were walking either independently or with an assistive device at home and school/work, respectively, while over community distances 61% (20/33) required a wheelchair. The only significant association between QoL and functional mobility was better ‘feelings about function’ in patients with better home FMS scores (r = 0.55; 95% confidence interval 0.15 to 0.79; p = 0.01).
Conclusion
The majority of children maintained their preoperative level of functional mobility at long-term follow-up after SEMLS.
Level of Evidence
IV
Keywords: cerebral palsy, quality of life, functional mobility, single-event multilevel surgery
Introduction
Cerebral palsy (CP) is a disorder of movement and posture caused by a defect or lesion of the immature brain.1 Differential growth between muscle-tendon units and bone results in muscle-tendon contractures, torsion of long bones and joint contractures or instability.2-4 The musculoskeletal sequelae of CP contribute to gait impairments, activity limitations and participation restrictions.4,5 Over the last three decades, single-level surgery has been replaced with the concept of single-event multilevel surgery (SEMLS), in which deformities at multiple anatomical levels are addressed during the same operative procedure.6-8
Studies evaluating SEMLS for children with CP usually focus on gait-related outcomes.8 There are now multiple reports that SEMLS improves gait kinematics at both short9-13 and long-term follow-up.10,13 However, the impact of SEMLS on functional mobility and quality of life (QoL) is less well understood as these domains have not been fully investigated.8,14,15 The literature on function and QoL following SEMLS for children with CP is limited by small study samples9,16-20 and short-term follow-up.12,17,18,20-23 Previous studies have reported stability of the Gross Motor Function Classification System (GMFCS) in patients with CP over time,24-26 including after SEMLS,27 and the GMFCS is suggested as an ideal classification tool. The primary aim of this study was to report the functional mobility of patients with diplegic CP at long-term follow-up after SEMLS with respect to their preoperative Gross Motor Function Classification System (GMFCS) grade. We hypothesize that patients would maintain functional mobility at long-term follow-up relative to their preoperative mobility status. The secondary aim was to assess if functional mobility is related to QoL in patients previously treated with SEMLS.
Materials and methods
Study design and setting
This study was a case series of children with CP that underwent SEMLS in a tertiary referral centre between 1 January 2005 and 31 December 2016 (level IV evidence). The study was approved by the Clinical Governance and Audit Team (ID: 5085).
Participants
Patients were included if they met the following criteria: 1) diplegic CP; 2) GMFCS I to III;5 3) SEMLS at age ≤ 18; 4) and completed the Functional Mobility Scale (FMS) questionnaire at long-term follow-up.28 SEMLS was defined as two or more bone and/or soft-tissue procedures at two or more anatomical levels bilaterally during one operative procedure.8
The gait laboratory database at our institution identified 74 eligible patients. Of these, 13 were excluded: six underwent surgery at a different unit and seven could not be contacted. Only one patient was classified as GMFCS I. As patients graded GMFCS I and II are, by definition, independent ambulators, these groups were combined when performing analyses.
Outcome measures
Patients undergoing SEMLS at our institution are routinely assessed with 3D gait analysis preoperatively and six, 12 and 24 months postoperatively. The cohort of 61 patients included in the study was subsequently contacted to evaluate long-term functional mobility and QoL. In May 2018 we contacted the patients meeting the inclusion criteria by telephone. If appropriate we asked the patient, but if not, we asked the parents to complete the FMS questionnaire over the telephone. FMS rates walking ability at three specified distances (five metres, 50 metres and 500 metres), taking into account the range of assistive devices a child/adolescent might use.28 These distances represent the patient’s mobility at home, school/work and in the community.
Following completion of the FMS questionnaire over the telephone, we assessed QoL using an online adapted version of the CP QOL Teen self-reported version 2.29 The CP QOL Teen is a condition-specific QoL instrument that reports on five domains of QoL including ‘general wellbeing and participation’, ‘communication and physical health’, ‘school wellbeing’, ‘social wellbeing’ and ‘feelings about function’. Following the authors’ permission, minor adaptions were made to make the questions applicable to the age of all patients (11 years, 10 months to 31 years, 4 months). Questions pertaining to school-related issues were modified for adults at work (e.g. ‘How do you feel about how you are accepted by other students at school or individuals at work?’) and a question relating to changes during puberty were only asked to those under 18 years old. The adapted CP QOL was converted into an online questionnaire, using REDCap electronic data capture tools (Vanderbilt University Medical Centre, Nashville, Tennessee),30 and a link to complete it online was sent to patients or parents. In an attempt to increase participation, an e-mail reminder was sent one and two weeks after the initial invitation to those who had not completed the online questionnaire.
Due to concerns about multiple testing when the QoL domains are examined against the FMS, hypotheses were formulated prior to the study. Firstly, we hypothesized that in patients graded GMFCS I and II preoperatively, better ‘feelings about function’ would be associated with better community FMS scores. Secondly, we hypothesized that in patients graded GMFCS III preoperatively, better ‘feelings about function’ would be associated with better home FMS scores.
Although all 61 patients completed the FMS questionnaire over the telephone at long-term follow-up, only 23 (38%) responded to the weblink to complete the online CP QOL Teen self-reported version 2. There were no significant differences in sex, GMFCS grade, age at surgery, preoperative Gait Profile Score (GPS),31 FMS scores or age at long-term follow-up between responders and non-responders.
The GPS at the routine 24-month postoperative gait analysis was compared with the preoperative value. A medical records review was performed to identify the surgical procedures performed as part of the SEMLS.
Statistical analysis
Continuous variables were summarized by mean and sd. Change in GPS was analyzed using a paired t-test. FMS was summarized by median and range. The associations between the five domains of QoL and FMS scores were summarized using Pearson correlation coefficients and tested for statistical significance. The QoL postulates were examined using methods of linear regression. Comparison of QoL domains between GMFCS grades I and II versus grade III utilized Student t-tests. The analyses were performed using IBM SPSS Statistics 24 (Armonk, New York). Statistical significance was concluded when p < 0.05.
Results
Demographics of the 61 included patients are reported in Table 1. There was a significant improvement in GPS from preoperative to 24 months postoperatively (mean 3.3°; sd 4.8; p < 0.001). There was a mean of 3.0 bone (sd 1.5) and 5.7 soft-tissue (sd 2.0) procedures per child as part of the SEMLS (Table 2).
Table 1.
Demographics of included patients
| Demographic | |
|---|---|
| Sex (M; F), n (%) | 33 (54); 28 (46) |
| GMFCS (I and II; III), n (%) | 28 (46); 33 (54) |
| Mean age at surgery (sd) | 11 yrs, 8 mths (2 yrs, 5 mths) |
| Mean length of follow-up (sd) | 8 yrs, 0 mths (3 yrs, 10 mths) |
| Mean age at long-term follow-up (sd) | 19 yrs, 7 mths (4 yrs, 4 mths) |
GMFCS, Gross Motor Function Classification System
Table 2.
Type and frequency of bone and soft-tissue procedures as part of single-event multilevel surgery
| Bone procedures | n | Soft-tissue procedures | n |
|---|---|---|---|
| Acetabuloplasty | 2 | Psoas lengthening | 4 |
| Femoral osteotomy | 103 | Adductor lengthening | 61 |
| Tibial osteotomy | 20 | Hamstring lengthening | 105 |
| Foot stabilization | 60 | Rectus femoris transfer | 62 |
| Bone procedures per child | 3.0 | Calf lengthening | 84 |
| Tibialis anterior split transfer | 4 | ||
| Tibialis posterior lengthening | 29 | ||
| Soft-tissue procedures per child | 5.7 |
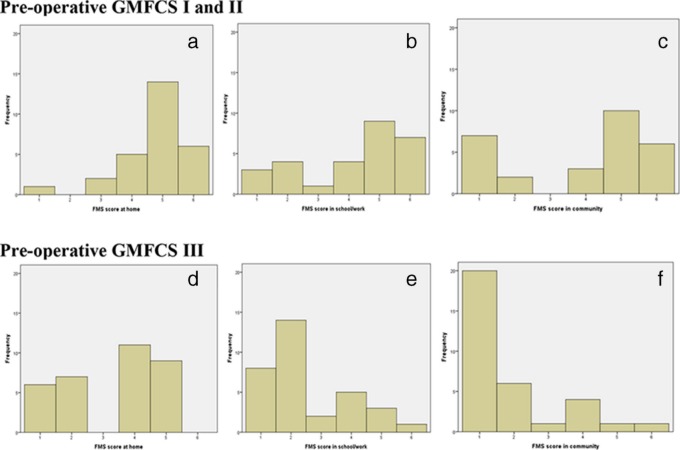
Of patients graded GMFCS I and II preoperatively, at long-term follow-up the median FMS score at home, school/work and in the community was 5 (1 to 6), 5 (1 to 6) and 5 (1 to 6), respectively. At long-term follow-up, the proportion walking independently at home, school/work and in the community was 71% (20/28; Fig. 1a), 57% (16/28; Fig. 1b) and 57% (16/28; Fig. 1c), respectively.
Fig. 1.
Histogram of Functional Mobility Scale (FMS) scores at long-term follow-up. Scores are shown for patients with respect to their preoperative Gross Motor Function Classification System (GMFCS) grade. Scores for children graded GMFCS I and II at home (a), school/work (b) and in the community (c) and children graded GMFCS III at home (d), school/work (e) and in the community (f).
Of patients graded GMFCS III preoperatively, at long-term follow-up the median FMS score at home, school/work and in the community was 4 (1 to 5), 2 (1 to 6) and 1 (1 to 6), respectively. Some patients graded GMFCS III preoperatively had acquired independent walking after SEMLS. At long-term follow-up, the proportion walking either independently or with an assistive device at home and school/work was 82% (27/33; Fig. 1d) and 76% (25/33; Fig. 1e), respectively. At long-term follow-up, 61% (20/33; Fig. 1f) of children graded GMFCS III preoperatively required a wheelchair over community distances.
The mean scores for the five QoL domains, both overall and according to preoperative GMFCS grade, are shown in Table 3. There were no statistically significant differences between the GMFCS grades for any domain.
Table 3.
Mean (sd) score for each domain of the Cerebral Palsy Quality of Life Teen (CP QOL Teen) for the entire cohort and comparison between groups based on preoperative Gross Motor Function Classification System (GMFCS) grade.
| CP QOL Teen domain | Total (n = 23) | GMFCS I and II (n = 11) | GMFCS III (n = 12) | p-value* |
|---|---|---|---|---|
| General wellbeing and participation | 71.4 (17.0) | 71.6 (20.0) | 71.1 (14.6) | 0.94 |
| Communication and physical health | 73.6 (15.8) | 76.7 (18.0) | 70.5 (13.4) | 0.37 |
| School/work wellbeing | 70.8 (20.6) | 73.8 (22.0) | 68.2 (19.8) | 0.55 |
| Social wellbeing | 83.6 (16.6) | 86.2 (14.1) | 81.3 (18.9) | 0.49 |
| Feelings about function | 75.4 (16.9) | 80.5 (16.4) | 70.7 (16.7) | 0.19 |
Significance tests were obtained by applying Student t-tests
There was a statistically significant association between home FMS score and ‘feelings about function’ (r = 0.55; 95% confidence interval (CI) 0.15 to 0.79; p = 0.01). When comparing the regressions of ‘feelings about function’ with home FMS in the two GMFCS groups it was found that there was no statistically significant difference between the groups (p = 0.89). There was no significant association between community FMS and ‘feelings about function’ (r = 0.22; 95% CI -0.24 to 0.59; p = 0.34). All other associations between any of the five QoL domains and home, school/work and community FMS scores were all non-significant (minimum p = 0.11).
Discussion
SEMLS is the standard treatment for correcting the musculoskeletal manifestations of CP. Most studies examining change following SEMLS focus on gait. Of the studies assessing function and QoL, the majority are limited by small study samples or insufficient length of follow-up. This study attempted to overcome these limitations by reporting the FMS in 61 children after a mean follow-up of eight years. The children included in this study had routine gait analysis preoperatively and at six, 12 and 24 months postoperatively. After 24 months the GPS had decreased by a mean of 3.3°, representing a two-fold improvement with respect to the minimally clinically important difference (1.6°).32 Table 2 reports a mean of 3.0 bone and 5.7 soft tissue procedures per child as part of the SEMLS, comparable with a recent large multicentre study that reported 8.7 procedures per child as part of SEMLS.13
Of patients graded GMFCS I and II preoperatively, at long-term follow-up, eight years later, over two-thirds were walking independently at home and over half were walking independently at school/work and in the community. Previous studies have reported that following a deterioration at three and six months postoperatively, the FMS returns to baseline by 12 months.33 This study adds to previous short-term studies by reporting outcomes at long-term follow-up. Our findings suggest that some of these children may be losing functional mobility in the longer term. However, the overall functional mobility of patients at final follow-up in this study echoes a recent long-term follow-up of children with flexed-knee gait that maintained function into adulthood following SEMLS.10
A previous short-term study reported that while 71% of children graded GMFCS III were using a wheelchair for community distances preoperatively, this had reduced to 58% at nine months and 50% at 12 months postoperatively.33 Rodda et al9 also reported improvements in functional mobility, but over a longer follow-up of five years. Although their study included a longer follow-up, it is limited by the inclusion of only ten patients. In our study, 61% (20/33) of patients graded GMFCS III preoperatively were using a wheelchair over community distances after a mean of eight years. Given that a large majority of patients graded GMFCS III require a wheelchair for community distances, the reported use at long-term follow-up in this study represents a success of surgery.
Gorton et al12 compared the change in function and QoL in a cohort of 75 children with spastic CP that underwent SEMLS with a matched cohort that did not undergo surgery. Despite reporting significant improvements following SEMLS, the study only reported outcomes after 12-month follow-up. Similarly, Cuomo et al22 reported that SEMLS improved QoL in a cohort of 57 ambulatory children with CP. However, the mean follow-up time was only 15.2 months. We hypothesized that better ‘feelings about function’ would be associated with better community FMS scores in those graded GMFCS I and II preoperatively, and better ‘feelings about function’ would be associated with better home FMS scores in those graded GMFCS III preoperatively. These pre-specified hypotheses were not confirmed. Although there was a significant association between ‘feelings about function’ and home FMS scores, it applied to patients irrespective of their GMFCS grade. A review by Livingston et al34 reported that while functional status measures such as the GMFCS are reliable indicators of variations in physical function, they do not correlate consistently with psychosocial wellbeing.
Shelly et al35 examined the strength of association between function and QoL domains using the CP QOL Child. In contrast to our study, all domains of QoL in their parent proxy-report were significantly associated with function levels, except access to services. For the child self-report, feelings about function, participation and physical health and pain and feelings about disability were significantly associated with functional level. It may be that function plays a less important role in QoL for older children and young adults in this cohort, or that we simply failed to detect significant associations because of the small sample that completed the QoL questionnaire.
This study has limitations to consider. First, there were no preoperative FMS or QoL data and there was no control group. This makes it difficult to draw conclusions about the effect SEMLS has on these parameters. However, this study adds to the literature by providing valuable information on the functional mobility of an unselected cohort of patients following SEMLS that has not previously been reported. Second, only 38% (23/61) of patients responded to the QoL survey. The lack of significant associations between FMS and QoL may be due to the small patient numbers. Third, the CP QOL Teen self-reported version 2 is not validated for the entire age range of the study participants. Minor adaptions were made in an attempt to make the questionnaire more applicable. This allowed valuable insight into patients across a wide range of ages that would otherwise not be possible.
In conclusion, this study reports that the majority of patients graded GMFCS I and II preoperatively are still ambulating independently at long-term follow-up. Similarly, the majority of patients graded GMFCS III preoperatively either walk independently or with an assistive device at home and school/work eight years after SEMLS. Despite the favourable functional mobility at long-term follow-up, there was little evidence in this small cohort to establish a link between functional status and quality of life.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: No patient identifying information was used in this study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
All authors were actively involved in drafting and critical revision of the manuscript.
References
- 1. Rosenbaum P, Paneth N, Leviton A, et al. . A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 2007;109:8-14. [PubMed] [Google Scholar]
- 2. Graham H. Mechanism of deformity In: Scrutton D, Daminao D, Mayston M, eds. Management of the Motor Disorders of Children with Cerebral Palsy. 2nd ed London: Mac Keith Press, 2004:105-129. [Google Scholar]
- 3. Ziv I, Blackburn N, Rang M, Koreska J. Muscle growth in normal and spastic mice. Dev Med Child Neurol 1984;26:94-99. [DOI] [PubMed] [Google Scholar]
- 4. Bache CE, Selber P, Graham HK II. The management of spastic diplegia. Curr Orthop 2003;17:88-104. [Google Scholar]
- 5. Palisano R, Rosenbaum P, Walter S, et al. . Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997;39:214-223. [DOI] [PubMed] [Google Scholar]
- 6. Narayanan UG. Management of children with ambulatory cerebral palsy: an evidence-based review. J Pediatr Orthop 2012;32:S172-S181. [DOI] [PubMed] [Google Scholar]
- 7. Lamberts RP, Burger M, du Toit J, Langerak NG. A systematic review of the effects of single-event multilevel surgery on gait parameters in children with spastic cerebral palsy. PLoS One 2016;11:e0164686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McGinley JL, Dobson F, Ganeshalingam R, et al. . Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol 2012;54:117-128. [DOI] [PubMed] [Google Scholar]
- 9. Rodda JM, Graham HK, Nattrass GR, et al. . Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J Bone Joint Surg [Am] 2006;88-A:2653-2664. [DOI] [PubMed] [Google Scholar]
- 10. Church C, Ge J, Hager S, et al. . Flexed-knee gait in children with cerebral palsy: a long-term follow-up study. Bone Joint J 2018;100-B:549-556. [DOI] [PubMed] [Google Scholar]
- 11. Gough M, Eve LC, Robinson RO, Shortland AP. Short-term outcome of multilevel surgical intervention in spastic diplegic cerebral palsy compared with the natural history. Dev Med Child Neurol 2004;46:91-97. [DOI] [PubMed] [Google Scholar]
- 12. Gorton GE III, Abel MF, Oeffinger DJ, et al. . A prospective cohort study of the effects of lower extremity orthopaedic surgery on outcome measures in ambulatory children with cerebral palsy. J Pediatr Orthop 2009;29:903-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dreher T, Thomason P, Švehlík M, et al. . Long-term development of gait after multilevel surgery in children with cerebral palsy: a multicentre cohort study. Dev Med Child Neurol 2018;60:88-93. [DOI] [PubMed] [Google Scholar]
- 14. Wilson NC, Chong J, Mackey AH, Stott NS. Reported outcomes of lower limb orthopaedic surgery in children and adolescents with cerebral palsy: a mapping review. Dev Med Child Neurol 2014;56:808-814. [DOI] [PubMed] [Google Scholar]
- 15. Morgan P, McGinley J. Gait function and decline in adults with cerebral palsy: a systematic review. Disabil Rehabil 2014;36:1-9. [DOI] [PubMed] [Google Scholar]
- 16. Buckon CE, Thomas SS, Piatt JH Jr, Aiona MD, Sussman MD. Selective dorsal rhizotomy versus orthopedic surgery: a multidimensional assessment of outcome efficacy. Arch Phys Med Rehabil 2004;85:457-465. [DOI] [PubMed] [Google Scholar]
- 17. Johnston TE, Finson RL, McCarthy JJ, et al. . Use of functional electrical stimulation to augment traditional orthopaedic surgery in children with cerebral palsy. J Pediatr Orthop 2004;24:283-291. [DOI] [PubMed] [Google Scholar]
- 18. Seniorou M, Thompson N, Harrington M, Theologis T. Recovery of muscle strength following multi-level orthopaedic surgery in diplegic cerebral palsy. Gait Posture 2007;26:475-481. [DOI] [PubMed] [Google Scholar]
- 19. Åkerstedt A, Risto O, Ödman P, Öberg B. Evaluation of single event multilevel surgery and rehabilitation in children and youth with cerebral palsy—A 2-year follow-up study. Disabil Rehabil 2010;32:530-539. [DOI] [PubMed] [Google Scholar]
- 20. Thompson N, Stebbins J, Seniorou M, et al. . The use of minimally invasive techniques in multi-level surgery for children with cerebral palsy: preliminary results. J Bone Joint Surg [Br] 2010;92-B:1442-1448. [DOI] [PubMed] [Google Scholar]
- 21. Schwartz MH, Viehweger E, Stout J, Novacheck TF, Gage JR. Comprehensive treatment of ambulatory children with cerebral palsy: an outcome assessment. J Pediatr Orthop 2004;2445-53. [PubMed] [Google Scholar]
- 22. Cuomo AV, Gamradt SC, Kim CO, et al. . Health-related quality of life outcomes improve after multilevel surgery in ambulatory children with cerebral palsy. J Pediatr Orthop 2007;27:653-657. [DOI] [PubMed] [Google Scholar]
- 23. Gupta A, Srivastava A, Taly AB, Murali T. Single-stage multilevel soft-tissue surgery in the lower limbs with spastic cerebral palsy: experience from a rehabilitation unit. Indian J Orthop 2008;42:448-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Palisano RJ, Cameron D, Rosenbaum PL, Walter SD, Russell D. Stability of the gross motor function classification system. Dev Med Child Neurol 2006;48:424-428. [DOI] [PubMed] [Google Scholar]
- 25. McCormick A, Brien M, Plourde J, et al. . Stability of the Gross Motor Function Classification System in adults with cerebral palsy. Dev Med Child Neurol 2007;49:265-269. [DOI] [PubMed] [Google Scholar]
- 26. Palisano RJ, Avery L, Gorter JW, Galuppi B, McCoy SW. Stability of the Gross Motor Function Classification System, Manual Ability Classification System, and Communication Function Classification System. Dev Med Child Neurol 2018;60:1026-1032. [DOI] [PubMed] [Google Scholar]
- 27. Rutz E, Tirosh O, Thomason P, Barg A, Graham HK. Stability of the Gross Motor Function Classification System after single-event multilevel surgery in children with cerebral palsy. Dev Med Child Neurol 2012;54:1109-1113. [DOI] [PubMed] [Google Scholar]
- 28. Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The Functional Mobility Scale (FMS). J Pediatr Orthop 2004;24:514-520. [DOI] [PubMed] [Google Scholar]
- 29. No authors listed CPQOL. Teen self-report version (13-18 years). Version 2. www.cpqol.org.au/ (date last accessed: 2 December 2019).
- 30. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Baker R, McGinley JL, Schwartz MH, et al. . The gait profile score and movement analysis profile. Gait Posture 2009;30:265-269. [DOI] [PubMed] [Google Scholar]
- 32. Baker R, McGinley JL, Schwartz M, et al. . The minimal clinically important difference for the Gait Profile Score. Gait Posture 2012;35:612-615. [DOI] [PubMed] [Google Scholar]
- 33. Harvey A, Graham HK, Morris ME, Baker R, Wolfe R. The Functional Mobility Scale: ability to detect change following single event multilevel surgery. Dev Med Child Neurol 2007;49:603-607. [DOI] [PubMed] [Google Scholar]
- 34. Livingston MH, Rosenbaum PL, Russell DJ, Palisano RJ. Quality of life among adolescents with cerebral palsy: what does the literature tell us? Dev Med Child Neurol 2007;49:225-231. [DOI] [PubMed] [Google Scholar]
- 35. Shelly A, Davis E, Waters E, et al. . The relationship between quality of life and functioning for children with cerebral palsy. Dev Med Child Neurol 2008;50:199-203. [DOI] [PubMed] [Google Scholar]