Abstract
Purpose
Paediatric radial neck fractures are challenging to treat. Multiple strategies exist for reduction and fixation; there is no clear consensus on the best surgical technique to achieve reduction. The percutaneous leverage technique is a method for reduction of radial neck fractures that has previously been described by Wallace, though there is a lack of published literature on this technique. We present a technical note and a modest case series on our modification to the percutaneous leverage technique accompanied by intramedullary fixation.
Methods
We describe a retrospective series of patients who underwent the modified percutaneous leverage technique for paediatric radial neck fracture reduction followed by flexible intramedullary nail fixation at a single Level I trauma centre from 2008 to 2016. This technique involves making a small incision over the dorsal border of the ulna and using a blunt curved surgical forceps to dissect towards the ulnar border of the radius just distal to the radial neck fracture site. The curved forceps is then used to push the radial shaft away from the ulnar shaft which reduces the radial neck fracture. Intramedullary fixation is then utilized to stabilize the reduction. Pre- and postoperative radiographs and clinical data from the medical record were reviewed, and patient, injury and treatment characteristics as well as complication rates are summarized.
Results
We successfully treated a series of eight radial neck fractures with the modified percutaneous leverage technique. This technique allows for a small incision and a minimally invasive method for the reduction of paediatric radial neck fractures. This allowed for subsequent intramedullary fixation and early postoperative elbow mobilization. In our series, no patients developed synostoses or sustained peripheral nerve injuries using this technique.
Conclusion
The modified percutaneous leverage technique followed by intramedullary fixation is a safe and effective technique for fixation of displaced paediatric radial neck fractures.
Level of Evidence
Level IV
Keywords: paediatric radial neck fracture, Wallace technique, percutaneous leverage
Introduction
Surgical management of paediatric radial neck fractures can be challenging. Multiple strategies exist for reduction and fixation of these fractures without clear consensus on the most appropriate approach for surgical treatment of these injuries. Concerns about elbow stiffness and avascular necrosis exist with open techniques, and while closed or percutaneous reduction options are favoured, these are often technically challenging with only a limited number of attempts recommended before resorting to open techniques due to concerns regarding increased injury, bleeding and stiffness with repeated attempts.1,2 Indeed, surgical management of paediatric radial neck fractures regardless of technique employed has been associated with suboptimal results in over 30% of patients in prior reports, with open reduction associated with increased predisposition toward poorer results.1,3
The Wallace technique for reduction of radial neck fractures is a previously described technique that employs percutaneous leverage for the reduction of radial neck fractures. A small incision is made on the dorsal subcutaneous border of the ulna at the level of the bicipital tuberosity. An elevator is then placed in the space between the radius and ulna. The elevator is then used to reduce the ulnarly-deviated radial shaft to the radial head.4-6 However, while this technique has been described, there is little published on the results of this technique in surgical practice and the description of this technique is almost entirely limited to textbooks.
At our institution, we have found this percutaneous leverage technique followed by the modification of using a flexible intramedullary nail fixation to be effective for surgical management of paediatric radial neck fractures. In this article, we present a description of our modification of the surgical technique as well as a case series of patients who underwent successful surgical treatment of their radial neck fractures using this technique at our institution.
Surgical technique
Indications
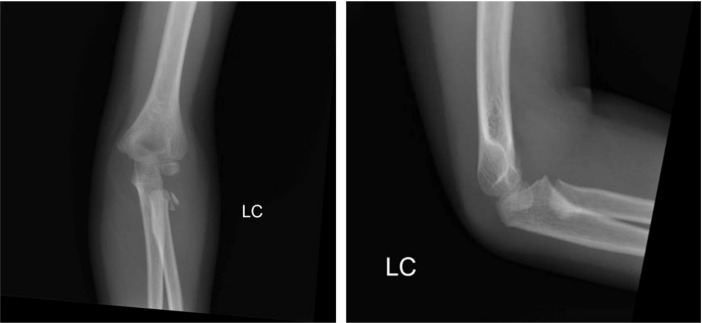
Surgical indications for this procedure were any radial neck fracture with displacement of > 30° or a mechanical block to movement on physical examination. In all cases, closed reduction was first attempted before attempting the percutaneous leverage technique. Figure 1 demonstrates the preoperative anteroposterior and lateral radiographs of a patient in our series with a displaced radial neck fracture who subsequently underwent surgical management with this technique.
Fig. 1.
Anteroposterior and lateral radiographs of a displaced paediatric radial neck fracture after injury.
Equipment and positioning
Patients were positioned supine with the operative arm extended on a radiolucent hand table. A tourniquet was used in most cases. Special equipment required for this procedure included a paediatric elastic flexible intramedullary nail system. A 2-mm flexible nail was most commonly used in our series.
Surgical technique
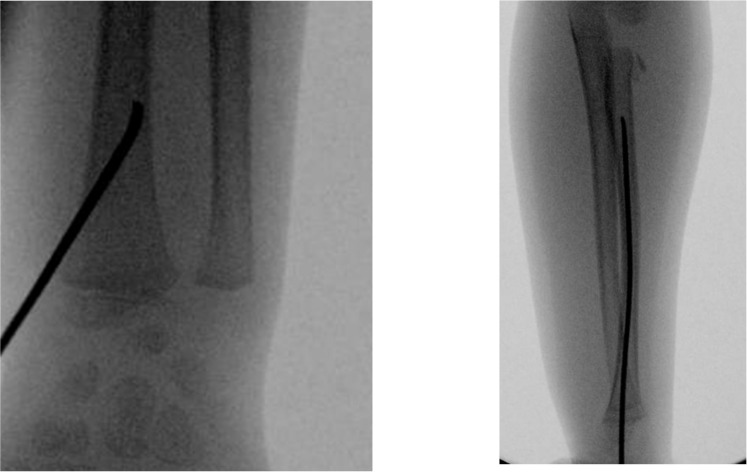
Following failed closed reduction, the decision to proceed with percutaneous leverage reduction was made. Attention is first directed to the distal radius of the injured limb for initiation of placement of a flexible intramedullary nail. This is done through a standard radial styloid approach or a dorsal approach over Lister’s tubercle. The nail is advanced just distal to the fracture site (Fig. 2). Attention is then turned to the fracture site.
Fig. 2.
Intraoperative fluoroscopic images demonstrating insertion of the flexible intramedullary nail and advancement to the site of the radial neck fracture.
With the elbow extended, intraoperative fluoroscopy is used to determine the maximum displacement of the radial head relative to the radial shaft by ranging the forearm through pronation and supination. Fluoroscopy is then used to identify a position proximal to the bicipital tuberosity but distal to the fracture site.
At this level, the radial nerve is lateral to the radius. A skin marker is used to draw a < 1 cm incision immediately radial to the subcutaneous border of the ulna (Fig. 3). Curved forceps are then used to bluntly dissect down to the proximal radius (Fig. 4). Of note, the forearm must be supinated to enable the forceps to enter the space between the ulna and radius. Fluoroscopy is then used to confirm the correct position of the forceps on the radius, which should be distal to the fracture but proximal to the bicipital tuberosity (Fig. 5). With thumb counterpressure on the skin over radial head fragment, the forceps or a surgical elevator is used to lever the radial shaft segment radially, away from the ulna, reducing the radial shaft to the radial head (Fig. 6). The ulna may be used as a fulcrum during this step to obtain more leverage. Oftentimes, an incomplete reduction is obtained at this point.
Fig. 3.
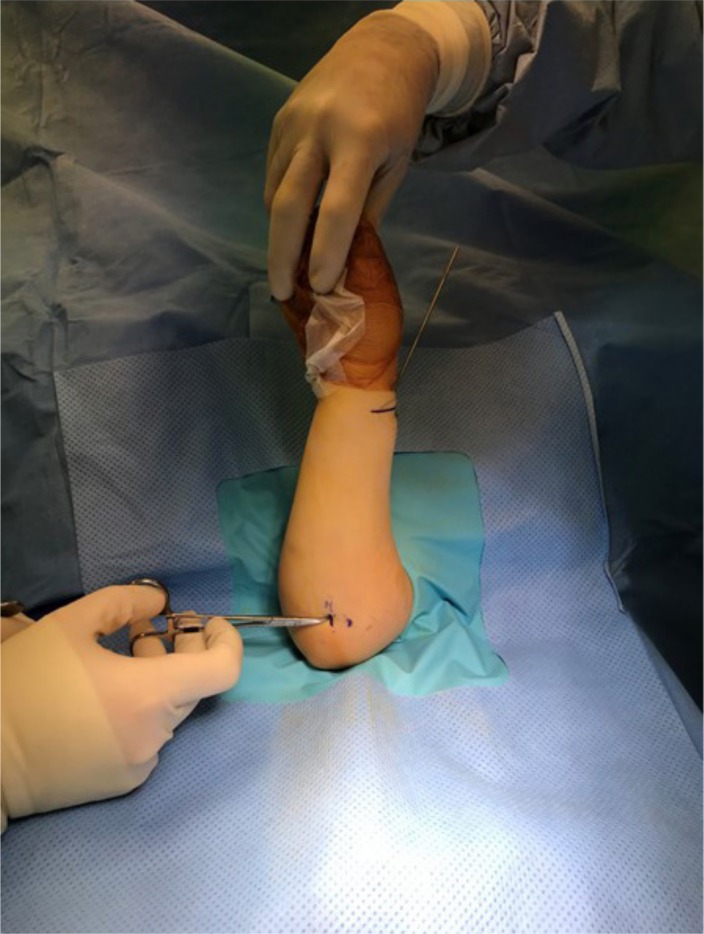
Fluoroscopy and surgical forceps are used to mark out a < 1-cm incision immediately radial to the subcutaneous border of the ulna.
Fig. 4.

Using surgical forceps, blunt dissection is carried out down to the level of the radius.
Fig. 5.

Intraoperative fluoroscopy is used to confirm the correct position of the forceps on the radius, which should be distal to the fracture but proximal to the bicipital tuberosity.
Fig. 6.

Using the ulna as a fulcrum, the radial shaft is reduced to the radial head under fluoroscopic guidance.
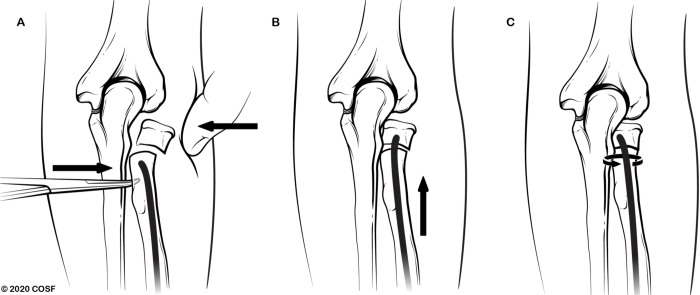
Then, with the radial head in an acceptable or near-acceptable position, the flexible nail is advanced across the fracture site into the proximal radial head fragment. If reduction is imperfect, the Metaizeau technique is then used to rotate the piece into anatomical position3 (Figs 7 and 8). This intramedullary nail may also be substituted with blunted long Kirschner wires or Ilizarov wires if needed.
Figure 7.
After the percutaneous leverage technique, the nail is advanced across the site of the fracture. If the radial head is still incompletely reduced (left), the nail is then rotated using the Metaizeau technique (centre) to obtain the final anatomical reduction as seen on anteroposterior and lateral intraoperative fluoroscopic images (center and right, respectively).
Figure 8.
Medical illustration of rotation of the nail using the Metaizeau technique to obtain final anatomical reduction. Illustration by Aimee Choi.
The intramedullary nail is then cut beneath the skin distally. The incisions are closed with absorbable suture. Final images should be taken to confirm reduction.
Postoperative protocol
The patient is placed into a bivalved, long-arm cast. The patient returns to the office at three weeks postoperatively and the cast is removed. The patient is allowed to begin elbow range of movement (ROM) in all planes at that time. The patients are scheduled for removal of hardware at approximately three months postoperatively.
Results
Data did not meet Shapiro-Wilk testing for normality; as such, medians and interquartile ranges (IQR) are reported. Our 0series included eight patients who underwent reduction with the percutaneous leverage technique as described. Over the study period, there were 96 patients who were treated via other open reduction techniques. There were four male and four female patients. The median age in our series was nine years (IQR 5.8 to 12.5). Median preoperative angulation was 52.5° (IQR 45.0° to 63.5°). Median postoperative angulation was 0° (IQR 0° to 7.5°). Four patients had a concomitant elbow injury in addition to the paediatric radial neck fracture: one patient also suffered an elbow dislocation with a concomitant olecranon fracture, another had an elbow dislocation with a medial epicondyle fracture, and the remaining two patients had concomitant olecranon fractures. No synostoses in any patient were noted on last follow-up. No peripheral nerve injuries were noted. One patient had acute compartment syndrome at time of presentation after the initial injury prior to surgical treatment, requiring fasciotomy in the setting of elbow dislocation. All patients underwent a second surgery for elective removal of hardware. Median follow-up was 97 days after the index operation (IQR 70.0 to 171.5). There were no intraoperative or postoperative complications related to the reduction technique.
Discussion
Surgical treatment of paediatric radial neck fractures remains challenging. The existence in the literature of multiple techniques of management confirms the data demonstrating that there is no benchmark method of reduction or fixation.1,4,5 However, available literature does suggest that fracture severity and open surgical reduction are associated with worse outcomes.1,7,8 On this note, an avenue for future study is to better understand the influence of the severity of the fracture on outcome versus the influence of the surgical technique on outcome. Nonetheless, given the poorer outcomes associated with open reduction, surgeons should have familiarity with percutaneous techniques of reduction of paediatric radial neck fractures.
We believe that this technique presented is paricularly useful for several reasons. Firstly, it is minimally invasive and requires a < 1-cm incision along the border of the ulna. If this technique fails and further open reduction is indicated, this incision does not interfere with placement of subsequent incisions. Secondly, the use of an intramedullary implant as a component of the technique allows the surgeon a second opportunity to improve the reduction with the Metaizeau technique.3 Notably, we prefer to begin with the percutaneous leverage technique followed by the Metaizeau technique as we have found that it is more facile to lever the larger distal radial shaft to the radial head rather than in the opposite sequence; we have also noted that in many cases the radial shaft is more displaced than the radial head. As such, in our experience this sequence has led to shorter operative times and improved reductions. A third benefit to our technique is that the procedure allows for internal fixation and early movement; patients are allowed to begin elbow ROM at three weeks postoperatively with this method to prevent stiffness. Importantly, we did not note any cases of synostoses or nerve damage in our series. An algorithm of attempting closed reduction techniques such as employing an Esmarch bandage should be attempted prior to attempting open reduction in most cases, though in our experience, in cases of highly displaced fractures, this may add to operative time and additional soft-tissue trauma and manipulation particularly in cases where open reduction is already felt to be required.
A disadvantage to this technique is the need for a second surgery for hardware removal. Additionally, not all paediatric radial neck fractures may be amenable to this fixation. In our series, the median age at time of injury was nine years old, but it is certainly possible that in very young children with Salter-Harris type I fractures, intramedullary fixation may instead result in pushing the fragment further away, complicating percutaneous reduction. We also realize the concern for immobilization of the elbow postoperatively after stabilization of the radial neck fracture. We have not observed any long-term complications resulting from this period of immobilization, however, and we do feel that this relatively brief period is necessary and allows for a balance between fragment control while the fracture heals and a short enough duration to prevent undesired permanent loss of movement of the elbow. A final drawback to our series is that this is from a single institution with limited follow-up.
When considering management of paediatric radial neck fractures, a stepwise approach is warranted. Existing literature suggests that closed and percutaneous reduction techniques should be attempted before open reduction. At our institution, we have found that our modification of the percutaneous leverage technique as described by Wallace is a valuable addition to the paediatric orthopaedic surgeon’s ‘toolbox’ in the surgical management of this difficult fracture.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: This study was Institutional Review Board-exempted. Patients were de-identified prior to analysis and did not require informed consent given the retrospective nature of this case series. The authors report no potential conflicts of interest regarding this work. This work was not conducted with any institutional or outside funding sources.
ICMJE Conflict of interest statement
None declared.
Acknowledgements
The authors would like to thank medical illustrator Aimee Choi, MS for creating Figure 8.
Author Contributions
CJW: Data acquisition, Analysis and interpretation of data, Study design; Drafting, Critical revision, Approval of final version.
CMY: Data acquisition, Analysis and interpretation of data, Study design, Drafting, Critical revision, Approval of final version.
ER: Data acquisition, Approval of final version.
DEK: Study design, Drafting, Critical revision, Approval of final version.
References
- 1. Zimmerman RM, Kalish LA, Hresko MT, Waters PM, Bae DS. Surgical management of pediatric radial neck fractures. J Bone Joint Surg [Am] 2013;95:1825-1832. [DOI] [PubMed] [Google Scholar]
- 2. Pring ME. Pediatric radial neck fractures: when and how to fix. J Pediatr Orthop 2012;32:S14-S21. [DOI] [PubMed] [Google Scholar]
- 3. Metaizeau JP, Lascombes P, Lemelle JL, Finlayson D, Prevot J. Reduction and fixation of displaced radial neck fractures by closed intramedullary pinning. J Pediatr Orthop 1993;3:355-360. [DOI] [PubMed] [Google Scholar]
- 4. Rockwood CA. Rockwood and Wilkins’ fractures in children. 7th ed. Philadelphia: Lippincott, Williams & Wilkins, 2010. [Google Scholar]
- 5. Rang M, MEWD Pring. Rang’s children’s fractures. 3rd ed. Philadelphia: Wolters Kluwer/Lippincott, Williams & Wilkins, 2006. [Google Scholar]
- 6. Wang J, Chen W, Guo M, Su Y, Zhang Y. Percutaneous reduction and intramedullary fixation technique for displaced pediatric radial neck fractures. J Pediatr Orthop B 2013;22:127-132. [DOI] [PubMed] [Google Scholar]
- 7. Gutiérrez-de la Iglesia D, Pérez-López LM, Cabrera-González M, Knörr-Giménez J. Surgical techniques for displaced radial neck fractures: predictive factors of functional results. J Pediatr Orthop 2017;37:159-165. [DOI] [PubMed] [Google Scholar]
- 8. Schmittenbecher PP, Haevernick B, Herold A, Knorr P, Schmid E. Treatment decision, method of osteosynthesis, and outcome in radial neck fractures in children: a multicenter study. J Pediatr Orthop 2005;25:45-50. [DOI] [PubMed] [Google Scholar]