Highlights
-
•
Intestine SARS-CoV-2 infection affects the disease course of COVID-19.
-
•
The digestive system is the main target organ of SARS-CoV-2 in some patients.
-
•
Viral excretion of SARS-CoV-2 in feces.
-
•
Management of patients with COVID-19 after discharge should include intestine SARS-CoV-2 infection.
Keywords: COVID-19, Intestinal infection, Environmental SARS-CoV-2 contamination, SARS-CoV-2, Viral excretion of SARS-CoV-2
Abstract
The current reports of COVID-19 focus on the respiratory system, however, intestinal infections caused by SARS-CoV-2 are also worthy of attention. This paper reported persistence of intestinal SARS-CoV-2 infection leads to re-admission after pneumonia resolved in three cases with COVID-19.
1. Introduction
The novel coronavirus disease (COVID-19) outbreak caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) in Wuhan City, Hubei Province, China, has been rapidly spreading globally. Studies have demonstrated that SARS-CoV-2 enters into human cells through human angiotensin-converting enzyme 2 (ACE2) as its receptor, which is highly expressed in type II alveolar epithelial cells (AT2) and also in absorptive enterocytes from the ileum and colon (Zhang et al., 2020). Besides the common symptoms of fever, fatigue and dry cough, gastrointestinal symptoms have also occurred in some patients with COVID-19 (Wang et al., 2020, Chen et al., 2020). Researchers have also tested and isolated viable SARS-CoV-2 from stool (Holshue et al., 2020, World Health Organization, 2020, Pan et al., 2020). This demonstrates that the digestive system is a potential route for SARS-CoV-2 infection. However, previous clinical diagnosis and discharge criteria have been mainly based on the respiratory system (National Health Commission of the People's Republic of China, 2020), and studies on the enteric involvement and viral excretion of SARS-CoV-2 in feces, as well as the influences of gastrointestinal infected SARS-CoV-2 on the disease course, were unavailable (Yeo et al., 2020). This paper reports three cases who were discharged, meeting all of the hospital discharge criteria (National Health Commission of the People's Republic of China, 2020), and were re-admitted due to persistence of intestinal SARS-CoV-2 infection.
2. Case reports
All the following criteria had to be met for hospital discharge of the three cases: (1) normal temperature lasting >3 days; (2) resolved respiratory symptoms; (3) substantially improved acute exudative lesions on chest computed tomography (CT) images; and (4) two consecutively negative RT-PCR test results of respiratory samples separated by at least 1 day.
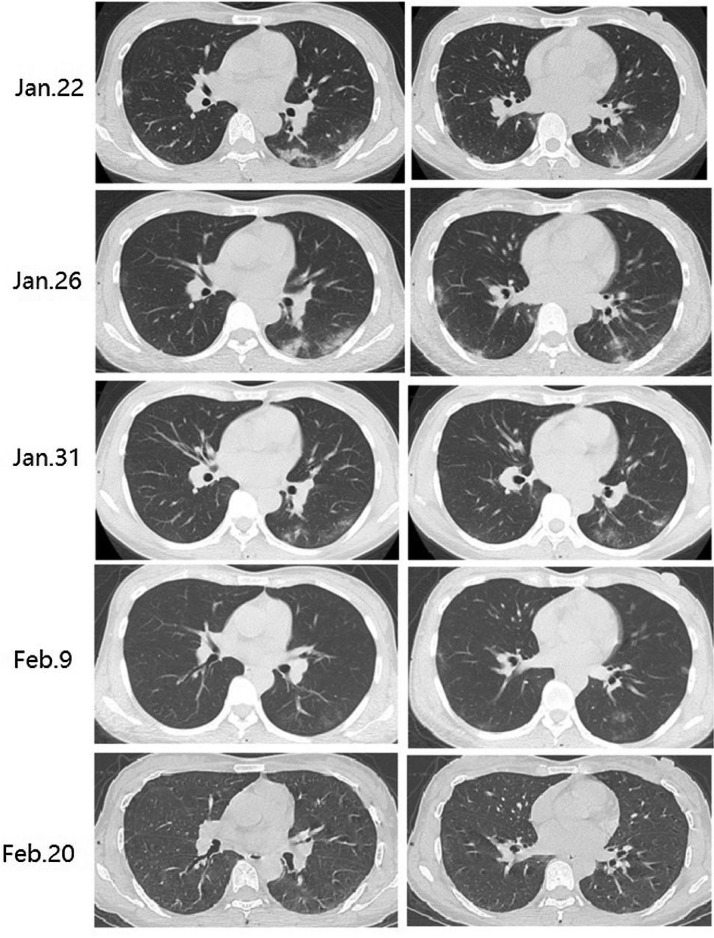
Case 1: On 16 January 2020, a 41-year-old woman with confirmed COVID-19 presented with pharyngalgia, nasal congestion, intermittent fever, fatigue and headache, and was admitted to hospital. On admission, she reported loose stool combined with watery diarrhea 5–6 times per day. On illness day 8, her clinical condition became worse (Supplementary Figure 1A and Table 1), with diarrhea 10–12 times per day and oxygen saturation values dropped to 94%. On illness day 10, she received Arbidol and interferon as well as probiotics including yeast and Bifidobacterium. All symptoms, with the exception of loose stool 2–3 times per day and the lesions on chest CT, had resolved (Fig. 1 ) and the throat swabs specimens for SARS-CoV-2 were negative on illness days 24 and 26. The patient was discharged on illness day 28. However, one day after discharge, she had fever combined with fatigue and watery diarrhea 6–7 times per day and was re-admitted. Laboratory results reflected leukopenia (Supplementary Table 1) and chest CT demonstrated that lesions were significantly resolved (Fig. 1). Throat swabs were negative for SARS-CoV-2 by RT-PCR on illness days 29, 35 and 40, while the stool samples were positive for SARS-CoV-2 by RT-PCR on illness days 31 and 36. Forty days after the onset of illness, the stool samples for SARS-CoV-2 turned negative, all symptoms had resolved and the patient was discharged again. Follow-up was performed by telephone and the patient did not report any particular problems.
Fig. 1.
Chest CT images of Case 1. Chest CT images demonstrated a bilateral and peripheral consolidation associated with a ground-glass opacity pattern on 22 January 2020. The range of lesions slightly expanded on 26 January 2020. The lesions were significantly reduced, leaving only a thin ground-glass opacity under the pleura on 31 January. Lesions were significantly resolved on 09 and 20 February.
Case 2: A 30-year-old female presented with diarrhea with yellow watery stools 3–5 times per day combined with changes in bowel habits (defecating after eating) on 23 January 2020, seven days after cesarean section. She reported fever with a dry cough on illness day 4. Her throat swab was positive by RT-PCR for SARS-CoV-2 while her chest CT was normal. She started taking Arbidol and moxifloxacin on her own. The symptoms, including diarrhea, had resolved with the exception of changes in bowel habits on illness day 13. The throat swabs for SARS-CoV-2 by RT-PCR were negative on illness days 15 and 16, and the patient was waiting to discharge. However on illness day 18, she reported fatigue. Her laboratory results reflected leukopenia (Supplementary Figure 1B and Table 2) while chest CT was normal on illness day 19. Additionally, the throat swabs and human milk samples for SARS-CoV-2 by RT-PCR were negative (Supplementary Figure 1B), whereas the stool samples for SARS-CoV-2 remained positive all the time (on illness days 18, 21, 23, 25, 30) and changes in bowel habit (defecating after eating) were not resolved.
Case 3: A 24-year-old female with confirmed COVID-19 presented with intermittent fever, nasal congestion, cough, fatigue, anorexia, and lost her sense of smell. She was treated in hospital. On admission, she received Arbidol and interferon for 5 days. Her temperature turned to normal on illness day 24 and symptoms gradually improved (Supplementary Figure 1C). The throat swabs for SARS-CoV-2 turned negative on illness days 26 and 28, and her chest CT improved (Supplementary Figure 2). The stool was positive for SARS-CoV-2 without any digestive symptoms on illness days 24, 26 and 30. The patient was discharged on illness day 31. However, one day after discharge, she appeared with a fever combined with nausea, vomiting and diarrhea with yellow watery stools five times per day. Her laboratory results reflected leukopenia again (Supplementary Table 3), her chest CT was fully resolved, and her throat swabs were negative but stool samples were still positive for SARS-CoV-2 by RT-PCR.
3. Discussion
This paper reported three SARS-CoV-2 confirmed patients with persistence of gastrointestinal symptoms and SARS-CoV-2 RNA in stool samples on re-admission after SARS-CoV-2 pneumonia had resolved. It is speculated that persistence of intestinal infection caused by SARS-CoV-2 leads to re-admission at the first discharge or time of waiting for discharge.
In early reports from Wuhan, China, the most common symptoms of COVID-19 included fever, fatigue, dry cough and shortness of breath, and the chest CT images showed lesions in the lungs of all patients; 2–10% of patients with COVID-19 had gastrointestinal symptoms such as diarrhea, abdominal pain and vomiting (Wang et al., 2020, Chen et al., 2020). The three patients who mainly presented with gastrointestinal symptoms such as diarrhea and changes in bowel habits and were positive for SARS-CoV-2 in stool samples were re-admitted after being found negative for SARS-CoV-2 respiratory specimens and chest CT images had resolved. This demonstrated that the digestive system may have been the main target organ of SARS-CoV-2 in the three patients and the viral load was in feces at a very low-risk status when COVID-19 patients were discharged from hospital. This highlights that clinicians should pay attention to properly manage the digestive symptoms of patients with COVID-19.
The disease course of the three patients was >30 days, which was much longer than all of the patients with COVID-19 that had been previously analyzed (unpublished data), which was an average 21 days from illness onset to discharge, and was also longer than that of patients reported by Zhou et al. (2020), in which the median time was 22 days in survivors. These results indicate that the intestinal infection with SARS-CoV-2 significantly affects the disease course of COVID-19.
Recent evidence has revealed that fecal nucleic acid was readily detected in stool and rectal swabs of patients with COVID-19 (Holshue et al., 2020, Zhang et al., 2020). Combined with the present cases, the environmental contamination by feces and induced aerosolization transmission of patients with COVID-19 should be given much attention. However, the current report had limitations as the presence of SARS-CoV-2 nucleic acid in stool alone cannot be used to define infection and transmission, and further studies are required on the influences of the enteric involvement and viral excretion of SARS-CoV-2 in feces on transmission dynamics of SARS-CoV-2.
Up to now, both diagnostic and discharge criteria of COVID-19 have been based on the symptoms and manifestations of the respiratory system (National Health Commission of the People's Republic of China, 2020); however, some patients may present with mainly digestive symptoms due to gastrointestinal tract infected by SARS-CoV-2. Therefore, current criteria for hospital discharge and continued patient management may need to be reevaluated.
Ethic approval
Ethics approval was waived by the Institutional Review Board of the hospital as all data were collected and analyzed from the patients according to the policy for public health outbreak investigation of emerging infectious diseases issued by the National Health Commission of the People's Republic of China.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities [No. 2020kfyXGYJ034].
Authors’ contributors
XW, WM and QZ had the idea for and designed the study. WM and QZ had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. XW, YZ contributed to the drafting of the manuscript. All authors contributed to data acquisition, data analysis, or data interpretation. The final version had been reviewed and approved by all authors.
Conflicts of interest
No potential conflict of interest was reported by the authors.
Acknowledgements
We thank all healthcare workers involved in the diagnosis and treatment of patients in Wuhan.
Footnotes
Supplementary material related to this article can be found, in the online version, at https://doi.org/10.1016/j.ijid.2020.04.063.
Appendix A. Supplementary data
The following are supplementary data to this article:
References
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the People's Republic of China . 2020. Diagnosis and treatment program of new coronary pneumonia (the seventh edition) http://www.nhc.gov.cn/xcs/zhengcwj/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. [Google Scholar]
- Pan Y., Zhang D., Yang P., Poon L.L.M., Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30113-4. S1473-3099(20)30113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020:e201585. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. [Google Scholar]
- Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5(4):335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Kang Z., Gong H., Xu D., Wang J., Li Z. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. BioRxiv 927806 [preprint]. January 31. 2020:927806. doi: 10.1101/2020.01.30. [DOI] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.