Abstract
SARS-CoV-2 (COVID-19) is a new virus causing respiratory illness outbreak. Nowadays, COVID-19 has spread to several countries around the world and is presently a major global concern. It appears that no certain effective pharmaceutical agent is currently available for it. It seems that obesity is one of the biggest risk factors related to COVID-19 hospitalization and critical illness. The strengthening of the body systems by non-drug ways is very important especially in obese people. On the basis of some indirect evidence, it seems that moderate physical activity can be recommended as a non-pharmacological, inexpensive, and viable way to cope with corona. On the other hand, recommending higher intensity exercise needs further consideration to make final decision in this regard.
Keywords: High-intensity exercise, Moderate-intensity exercise, Obesity, SARS- CoV-2 (COVID-19)
Graphical abstract
Highlights
-
•
As a conservative approach, high intensity exercise is not recommended against COVID-19 virus.
-
•
It seems that moderate intensity exercise can be recommended as a way to cope with COVID-19.
-
•
The ‘open window’ theory and ‘J curve’ concept explain the effect of exercise intensity on immune system.
1. Introduction
SARS-CoV-2 (COVID-19) is a new virus causing respiratory illness outbreak (Ghinai et al.). Nowadays, COVID-19 has spread to several countries around the world and is presently a major global concern. It seems that COVID-19 is a disease the risk of which is higher for obese people.
COVID-19 affects immune cells (Thevarajan et al., 2020). Thevarajan et al. showed that the blood levels of antibody-secreting cells (ASCs), follicular helper T cells (TFH cells), activated CD4+ T cells and CD8+ T cells and immunoglobulin M (IgM) and IgG increased in a COVID-19 patient (Thevarajan et al., 2020).
Today, people are following ways that improve immune ability i.e. nutrition and exercise. There are several investigations regarding the effects of nutrition supplementation on immune cells and inflammation in obesity condition (Chinchu et al., 2020; Mousavi et al., 2020; Tavvafian et al., 2020). Previous studies have shown that physical activity can improve immune health via an increase in immune cells (Nieman and Wentz, 2019). Therefore, it is suggested that the immune function should be increased by appropriate physical activity before the disease, which will boost the body against the virus. It is very useful in the present condition that there is no certain effective pharmaceutical agent against this virus (Fisher and Heymann, 2020). Physical activities with different intensity have different effects on the immune system (Nieman and Wentz, 2019; Romeo et al., 2010). The present study reviews the studies about the effect of exercise intensity on inflammatory factors and immune cells in obesity condition (as indirect evidence against viruses).
2. Exercise intensity considerations
Different physical activities in terms of intensity and type have different effects on immune system and inflammation (Nieman and Wentz, 2019; Romeo et al., 2010). Several studies have shown that high intensity exercise has positive effect on inflammatory factors in obesity conditions (Khaleghzadeh et al., 2020; TaheriChadorneshin et al., 2019). For example, Khaleghzadeh et al. showed that eight weeks of high intensity interval training (HIIT) led to a significant decrease in plasma interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α) and aspartate aminotransferase (AST) in male obese Wistar rats with non-alcoholic fatty liver disease (Khaleghzadeh et al., 2020). Some studies compared the effects of high intensity and moderate intensity exercise on inflammatory factors. de Souza et al. showed that a single high intensity interval session is able to decrease interferon gamma-/interleukin-4 (IFN-γ/IL-4) ratio (indicating an anti-inflammatory response), without alterations in the function of the mucosal immune system and lipoperoxidation. On the other hand, a session of moderate-intensity continuous exercise induced changes in the pattern of cytokines associated with increased cellular immune function (de Souza et al., 2018). Gerosa-Neto et al. showed that long-term HIIT (90% maximum heart rate, 3 times a week) increased TNF-α, while moderate-intensity continuous training (70% maximum heart rate, 5 times a week) decreased TNF-α in overweight/obese adults (Gerosa-Neto et al., 2016). In healthy young men, it was shown that moderate-intensity continuous training but not HIIT improved immune function biomarkers (Khammassi et al., 2020). Another study showed that HIIT induced inflammatory response and suppressed immune functions (Zwetsloot et al., 2014). The results of one review article showed that intense long exercise can lead to higher levels of inflammatory mediators, and consequently might increase the risk of injury and chronic inflammation, while moderate or vigorous exercise with appropriate resting periods can achieve maximum benefit (Cerqueira et al., 2020).
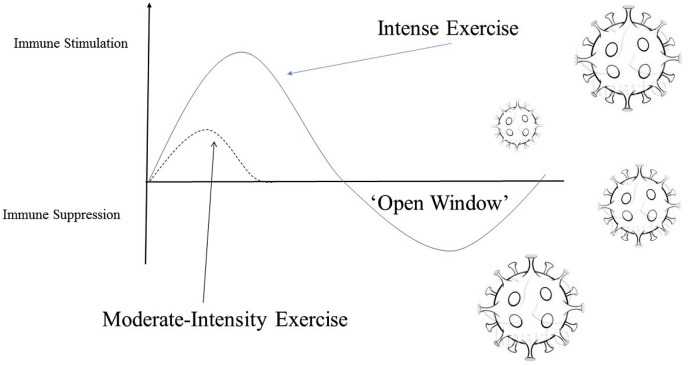
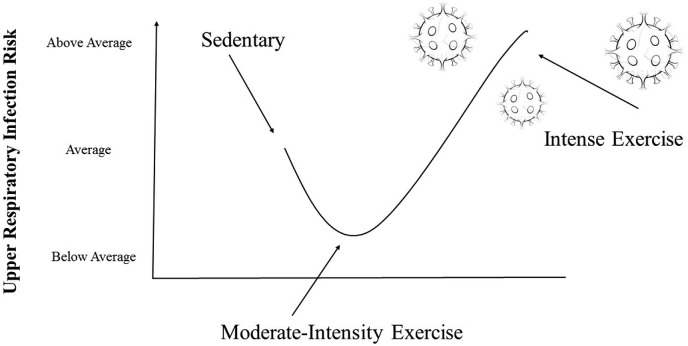
There is a theory that may explain the risk of high intensity exercise (Fig. 1 ). The ‘open window’ theory is characterized by suppression of the immune system following high intensity exercise (Kakanis et al., 2010). This window of opportunity may allow for an increase in susceptibility to upper respiratory illness (Kakanis et al., 2010). ‘J curve’ concept explains that individuals that regularly perform moderate intensity exercise improve their immune system, excessive bouts of prolonged training can impair immune function (Fig. 2 ) (Campbell and Turner, 2018). High intensity exercise due to the production of oxidants and suppression of immune system may be dangerous (especially, in obesity condition). The lipid peroxidation in obesity is higher than non-obesity condition (Marseglia et al., 2014). These are some indirect evidence that make a conservative approach regarding the use of high intensity exercise in COVID-19 outbreak. In addition, COVID-19 disease may be asymptomatic in several days and hence, severe high-intensity exercise may be more dangerous.
Fig. 1.
The ‘open window’ theory. It is characterized by suppression of the immune system following the intense exercise.
Fig. 2.
“J curve” concept. It suggests that, individuals that regularly perform moderate intensity exercise improve their immune system. Excessive bouts of prolonged training can impair immune function.
3. Conclusion
On the basis of indirect evidence and a conservative approach, high intensity exercise probably due to the production of oxidants and suppression of immune system may be dangerous (especially, in obese people) and help to exacerbate the COVID-19 virus. It is also noted that COVID-19 disease may be asymptomatic in several days and hence, severe high-intensity exercise may be more dangerous. The present study suggests a conservative approach on the basis of some evidence regarding use of high intensity exercise on inflammatory and immune factors. It means that moderate intensity exercise (and not high-intensity physical activity) should be recommended as a non-pharmacological, inexpensive, and viable way to cope with COVID-19 virus.
Authors’ contribution
SRA wrote the first draft of the manuscript. FH revised and improved the quality of the manuscript. All authors read and approved the final version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of competing interest
The authors declare no potential conflicts of interests with respect to the research, authorship, and/or publication of this article.
References
- Campbell J.P., Turner J.E. Debunking the myth of exercise-induced immune suppression: redefining the impact of exercise on immunological health across the lifespan. Front. Immunol. 2018;9(648) doi: 10.3389/fimmu.2018.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerqueira É., Marinho D.A., Neiva H.P. Inflammatory effects of high and moderate intensity exercise—a systematic review. Front. Physiol. 2020;10(1550) doi: 10.3389/fphys.2019.01550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinchu J.U., Mohan M.C., Prakash Kumar B. Anti-obesity and lipid lowering effects of Varanadi kashayam (decoction) on high fat diet induced obese rats. Obes. Med. 2020:17100170. doi: 10.1016/j.obmed.2019.100170. [DOI] [Google Scholar]
- de Souza D.C., Matos V.A.F., Dos Santos V.O.A. Effects of high-intensity interval and moderate-intensity continuous exercise on inflammatory, leptin, IgA, and lipid peroxidation responses in obese males. Front. Physiol. 2018;9567 doi: 10.3389/fphys.2018.00567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher D., Heymann D. Q&A: the novel coronavirus outbreak causing COVID-19. BMC Med. 2020;18(1):57. doi: 10.1186/s12916-020-01533-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerosa-Neto J., Antunes B.M.M., Campos E.Z. Impact of long-term high-intensity interval and moderate-intensity continuous training on subclinical inflammation in overweight/obese adults. J. Exerc. Rehabilitation. 2016;12(6):575–580. doi: 10.12965/jer.1632770.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghinai I, McPherson TD, Hunter JC, et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. doi:10.1016/S0140-6736(20)30607-3. [DOI] [PMC free article] [PubMed]
- Kakanis M.W., Peake J., Brenu E.W. The open window of susceptibility to infection after acute exercise in healthy young male elite athletes. Exerc. Immunol. Rev. 2010:16119–16137. [PubMed] [Google Scholar]
- Khaleghzadeh H., Afzalpour M.E., Ahmadi M.M. Effect of high intensity interval training along with Oligopin supplementation on some inflammatory indices and liver enzymes in obese male Wistar rats with non-alcoholic fatty liver disease. Obes. Med. 2020:17100177. doi: 10.1016/j.obmed.2019.100177. [DOI] [Google Scholar]
- Khammassi M., Ouerghi N., Said M. Continuous moderate-intensity but not high-intensity interval training improves immune function biomarkers in healthy young men. J. Strength Condit Res. 2020;34(1):249–256. doi: 10.1519/jsc.0000000000002737. [DOI] [PubMed] [Google Scholar]
- Marseglia L., Manti S., D'Angelo G. Oxidative stress in obesity: a critical component in human diseases. Int. J. Mol. Sci. 2014;16(1):378–400. doi: 10.3390/ijms16010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavi S.N., Saboori S., Asbaghi O. Effect of daily probiotic yogurt consumption on inflammation: a systematic review and meta-analysis of randomized Controlled Clinical trials. Obes. Med. 2020:18100221. doi: 10.1016/j.obmed.2020.100221. [DOI] [Google Scholar]
- Nieman D.C., Wentz L.M. The compelling link between physical activity and the body's defense system. J. Sport Health Sci. 2019;8(3):201–217. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo J., Warnberg J., Pozo T. Physical activity, immunity and infection. Proc. Nutr. Soc. 2010;69(3):390–399. doi: 10.1017/s0029665110001795. [DOI] [PubMed] [Google Scholar]
- TaheriChadorneshin H., Cheragh-Birjandi S., Goodarzy S. The impact of high intensity interval training on serum chemerin, tumor necrosis factor-alpha and insulin resistance in overweight women. Obes. Med. 2019:14100101. doi: 10.1016/j.obmed.2019.100101. [DOI] [Google Scholar]
- Tavvafian N., Darabi H., Ahani A. Effects of glycyrrhizic acid supplementation during nonlinear resistance training on inflammatory markers and muscular damage indices in overweight young men. Obes. Med. 2020:17100178. doi: 10.1016/j.obmed.2019.100178. [DOI] [Google Scholar]
- Thevarajan I., Nguyen T.H.O., Koutsakos M. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat. Med. 2020 doi: 10.1038/s41591-020-0819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwetsloot K.A., John C.S., Lawrence M.M. High-intensity interval training induces a modest systemic inflammatory response in active, young men. J. Inflamm. Res. 2014 doi: 10.2147/JIR.S54721. 79-17. [DOI] [PMC free article] [PubMed] [Google Scholar]