Abstract
This study aims to present the correlation between sunlight exposure and Covid-19 statuses in Jakarta, Indonesia. The secondary data analysis was derived from surveillance data for Covid-19 from government authorities, including the Ministry of Health, the Meteorological, Climatological, and Geophysical Agency, and the local government of Jakarta. Three statuses related to Covid-19 were examined in the study: incidence, death, and recovered. Meanwhile, sunlight exposure was presented as daily duration of it. Only the number of recovered patients correlated significantly with sunlight exposure (p-value = .025; r = 0.350). This study's findings showed that sunlight exposure was associated with recovery from Covid-19.
Keywords: Coronavirus, Sunlight, Recovery, Indonesia
Graphical abstract

Highlights
-
•
Covid-19 is a type of influenza virus that surpresses the body's immune system.
-
•
Sunlight triggered the vitamin D that increased body immune.
-
•
Sunlight correlated significantly to Covid-19 patients recovery in Jakarta, Indonesia
1. Introduction
Coronavirus disease 2019 (Covid-19) is not only rapidly spreading but has become a global pandemic that affects many, including developing countries with limited resources (Singhal, 2020). In fact, even the currently affected developed countries are overwhelmed in their fight against Covid-19 (Bénassy-Quéré et al., 2020; Heymann and Shindo, 2020; Saglietto et al., 2020). It is considered that most developing countries will face more challenges than developed countries in curbing the spread of Covid-19 in their regions, causing them to potentially evolve into the new epicenter of the pandemic, and Indonesia is not exempted (Hopman et al., 2020).
Covid-19 is caused by a type of influenza virus that suppresses the body's immune system so that the viruses can grow in the respiratory tissues and organs (Shi et al., 2020; Xu et al., 2020). In this situation, individuals who are elderly or with prior comorbidities are more vulnerable to the severe effects of Covid-19 due to inadequate immune systems (Garnier-Crussard et al., 2020; Le Couteur et al., 2020; Morley and Vellas, 2020). Besides that, inadequate healthcare management, such as failure to provide early diagnosis and prompt treatment, would decrease the rate of recovery among Covid-19 patients (Greenhalgh et al., 2020; Hopman et al., 2020).
Indonesia is one of the developing countries with reported Covid-19 cases (Indonesian National Task Team Force for Coronovirus 2019 (Covid-19), 2020; Organization, 2020a). International experts have expressed their doubt to the Indonesian government regarding the capability of the nation's healthcare system to control this pandemic since the authority reported the first multiple positive cases of Covid-19 on 2nd March 2020 (Djalante et al., 2020; Wenham et al., 2020). Moreover, Indonesia has one of the highest proportions of death related to Covid-19 cases among countries in the world, with the epicenter of the disease being its capital, Jakarta (Organization, 2020a).
The confirmed positive cases of Covid-19 in Indonesia are divided into three levels of severity: 1) high, 2) moderate, and 3) low (Indonesian Ministry of Health, 2020a). Patients whose conditions are of high or moderate severity are given intensive medical care in healthcare facilities. Meanwhile, low-severity cases of Covid-19 are managed the same way as the rest of the general population, meaning they should stay home and practice social isolation and physical distancing (Indonesian Ministry of Health, 2020a). At the same time, the government has strongly promoted the Clean and Healthy Living Behavior (PHBS) and People's Healthy Lifestyle Movement (Germas) programs to encourage the people to include routine outdoor/indoor exercise to decrease the spread of Covid-19 (Indonesian Ministry of Health, 2020b).
The World Health Organization (WHO) reported that there is still no evidence that sunlight can terminate Covid-19 (World Health Organization, 2020). Moreover, too much of sunlight may cause harm through its ultraviolet, infrared, etc. (Karapiperis et al., 2020). However, sunlight contributes to the healing of multiple health condition including respiratory diseases such as influenza and severe acute respiratory syndrome (SARS) (Geier et al., 2018; Miller, 2018). Weather factors have shown persistent correlation to the emergence and re-emergence of infectious diseases, including Covid-19 (Tosepu et al., 2020). Thus, evidence for the effect of sunlight on Covid-19 is needed as the correlation between the two is still rarely assessed.
2. Methods
2.1. Study area
Jakarta is the capital city and business center of Indonesia. It is geographically located within the range of 5°19′12″ south latitude to 6°23′54″ south latitude and 106°22′42″ east longitude to 106°58′18″ east longitude, with an average altitude of ±7 m above the sea surface. Jakarta, which has tropical climates, has two seasons: rainy season that happens annually from October to March and dry season that takes place from April to September annually.
There are 132 referral hospitals available to treat Covid-19 patients of high and moderate severity in Indonesia. Eight of these, plus an emergency hospital, are in Jakarta. They are Dr. Sulianti Saroso Central General Hospital of Infectious Disease, Persahabatan Central General Hospital of Pulmonary, Gatot Subroto Army Central Hospital, Fatmawati Central General Hospital, Tarakan Regional General Hospital, Pasar Rebo Regional General Hospital, Bhayangkara Said Soekanto Police Central Hospital, Mintoharjo Navy Central Hospital, and National Emergency Hospital of Kemayoran. These health facilities were built according to the National Hospital Accreditation Commission (KARS), including the availability of daylight exposure in each treatment unit (National Hospital Accreditation Commission, 2012) .
2.2. Data collection
The set of relevant data, ranging from 2nd March to 10th April 2020, was obtained from the Indonesian government authorities. The daily confirmed cases of Covid-19 incidence, death, and recovery were derived from the Jakarta local government. This data was also made available by the Indonesian Ministry of Health as well as the Indonesian National Task Force Team for Covid-19. Meanwhile, the dataset of daily sunlight in Jakarta was obtained from the Meteorological, Climatological, and Geophysical Agency of Indonesia.
2.3. Data analysis
Spearman's correlation was performed to analyze the coefficient correlation value and determine whether significance existed. This statistical analysis was used to determine correlation between the existing variables. These variables were number of Covid-19 positive cases, deaths, and patients who recovered, and sunlight exposure.
3. Results
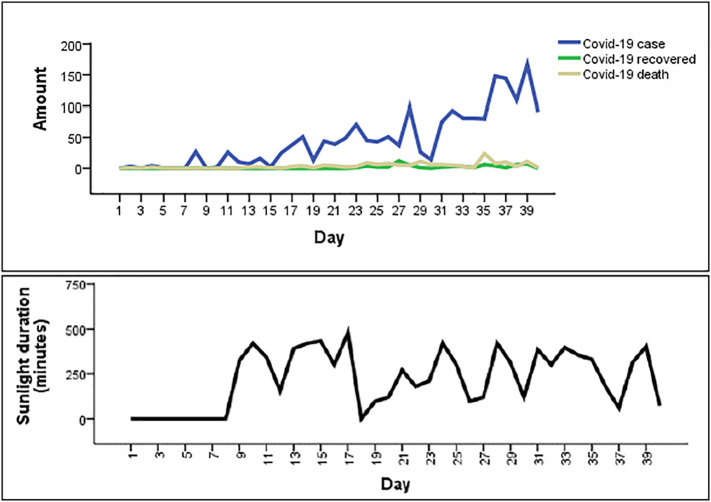
According to Fig. 1(a), the incidence of Covid-19 in Jakarta had been increasing. Since the first multiple cases of Covid-19 were reported on 3rd March 2020, Jakarta had seen an average of 45.25 new confirmed Covid-19 cases daily. The daily average number of recovered patients was 1.50, which was lower than the daily average deaths at 3.80 cases. Therefore, the death proportion of Covid-19 cases in Jakarta was 8.4% higher than the recovered proportion at 3.3%.
Fig. 1.
(a) Covid-19 status, (b) sunlight exposure duration (minutes).
Fig. 1(b) shows that the duration of sunlight exposure for Covid-19 patients in Jakarta fluctuated daily. The shortest duration of daily sunlight exposure was 0 min, while the longest duration was 480 min in Jakarta. The average duration of daily sunlight exposure was 217.95 min or 3.6 h.
Table 1 shows that sunlight exposure did not correlate significantly with both incidence and death cases of Covid-19 patients. Sunlight correlated significantly with cases of recovery from Covid-19.
Table 1.
Spearman's correlation coefficient between Covid-19 and sunlight exposure.
| Confirmed Covid-19 status | Spearmen's correlation coefficient |
|---|---|
| Incidence | 0.306 |
| Death | 0.284 |
| Recovery | 0.350⁎ |
Correlation is significant at the 0.05 level (2-tailed).
4. Discussion
In this study, we found that higher duration of sunlight exposure was related to more cases of recovery from Covid-19 among patients. This correlation is in line with previous evidence that sunlight does not terminate the Covid-19 virus so it cannot prevent the infection. Conversely, sunlight can maintain the health condition of Covid-19 patients so they have opportunity to recover from the disease. Sunlight boosts the immune system, which slows down the development of influenza and SARS agents in the human body (Cannell et al., 2006; Miller, 2018). In this case, Covid-19 patients who experienced sunlight exposure when they were receiving care either in hospitals or home settings were more likely to recover from the disease.
Sunlight triggers vitamin D production, which functions to increase the immune system (Slusky and Zeckhauser, 2018). Poor sunlight exposure activates influenza (Sagripanti and Lytle, 2007). Previous studies have shown that sunlight exposure significantly contributed to the healing of most respiratory conditions including tuberculosis and lung disease (Aloia and Li-Ng, 2007; Asyary et al., 2017).
Being in a region with a tropical climate, Jakarta can take advantage of the presence of abundant sunlight in every season. The health benefits of exposure to sunlight have been established (Singhal, 2020). Access to much-needed sunlight can enhance mood as well as release endorphins that will increase immunity against diseases such as Covid-19 (Sternberg and Engineer, 2020).
As it sits on the equator, the Indonesian territory, including Jakarta, is known as a tropical region that experiences two seasons: dry and rainy. However, even with its rainfall during the rainy season, Jakarta is still quite dry. The average duration of maximum sunlight is 3 to 3.5 h per day in Jakarta, which amounts to 4.8 kW-hour per square meter per day (kWh/m2/day), or 10 times the potential of European sunlight (Indonesia National Energy Board, 2013).
Most countries around the world, including Indonesia, are welcoming the dry or summer season, which takes place from April to September and can be potentially leveraged by each country to fight Covid-19. This potential approach can be accompanied by the formal treatment/therapy according to Covid-19 clinical guidelines (Organization, 2020b). WHO has only underlined the benefit of sunlight for clothes management (Organization, 2020c), so this finding will assist medical care particularly in low-resource health settings or places with inadequate Covid-19-mitigating response, including Jakarta (Hopman et al., 2020; Le Couteur et al., 2020).
Despite this study's significant finding about the relationship between sunlight and Covid-19 recovery, this research has limitations. The Covid-19 recovery factors could be affected by several others variables such as prompt treatment/therapy, PHBS and Germas, and physical capabilities. It is also essential to explore the type and characteristics of sunlight exposure in detail. Additionally, the available data provided by the authorities did not record the exposure of every Covid-19 patient to sunlight.
5. Conclusion
This study shows that sunlight exposure correlated significantly with recovery from Covid-19 among patients in Jakarta of Indonesia. However, sunlight exposure did not correlate significantly with the occurrence of and death from Covid-19. This preliminary study needs to be developed further as sunlight presents genuine potential in accelerating recovery from Covid-19 not only in Jakarta but also other countries, especially those with high death rates due to this pandemic.
CRediT authorship contribution statement
Al Asyary: Conceptualization, Methodology, Data curation, Software, Writing - original draft. Meita Veruswati: Visualization, Validation, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thanks to Indonesian government authorities for Covid-19, as well as to Directorate of Research and Community Engagement of Universitas Indonesia (DRPM-UI), that made the data available and supported to this study.
Editor: Wei Huang
References
- Aloia J.F., Li-Ng M. RE: epidemic influenza and vitamin D epidemiology and infection October 2007, Vol. 135, no. 7, pp. 1095-1098. Epidemiol. Infect. 2007;135:1095–1098. doi: 10.1017/S0950268807008308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asyary A., Eryando T., Purwantyastuti P., Junadi P., Clark C., Teijlingen E. Van. Level of exposure of childhood tuberculosis with adult pulmonary tuberculosis household contacts. Kesmas Natl. Public Heal. J. 2017;12:1–6. doi: 10.21109/kesmas.v12i1.1469. [DOI] [Google Scholar]
- Bénassy-Quéré A., Marimon R., Pisani-Ferry J., Reichlin L., Schoenmaker D., Weder B. 13 COVID-19: Europe needs a catastrophe relief plan. Mitigating COVID econ. Cris. Act Fast Do Whatever. 2020;121 [Google Scholar]
- Cannell J.J., Vieth R., Umhau J.C., Holick M.F., Grant W.B., Madronich S., Garland C.F., Giovannucci E. Epidemic influenza and vitamin D. Epidemiol. Infect. 2006;134:1129–1140. doi: 10.1017/S0950268806007175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djalante R., Lassa J., Setiamarga D., Mahfud C., Sudjatma A., Indrawan M., Haryanto B., Sinapoy M.S., Rafliana I., Djalante S. Review and analysis of current responses to COVID-19 in Indonesia: period of January to March 2020. Prog. Disaster Sci. 2020;100091 doi: 10.1016/j.pdisas.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnier-Crussard A., Forestier E., Gilbert T., Krolak-Salmon P. Novel Coronavirus (COVID-19) epidemic: what are the risks for older patients? J. Am. Geriatr. Soc. 2020:1–2. doi: 10.1111/jgs.16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geier D.A., Kern J.K., Geier M.R. A longitudinal ecological study of seasonal influenza deaths in relation to climate conditions in the United States from 1999 through 2011. Infect. Ecol. Epidemiol. 2018;8 doi: 10.1080/20008686.2018.1474708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T., Wherton J., Shaw S., Morrison C. 2020. Video Consultations for Covid-19. [DOI] [PubMed] [Google Scholar]
- Heymann D.L., Shindo N. COVID-19: what is next for public health? Lancet. 2020;395:542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low-and middle-income countries. JAMA. 2020:E1–E2. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- Indonesia National Energy Board Indonesia is high potential to sunlight beneficiary [WWW Document] News. 2013 https://www.den.go.id/index.php/dinamispage/index/396-.html [Google Scholar]
- Indonesian Ministry of Health . 2020. National Health Care Guideline for Coronavirus 2019 (Covid-19) in Indonesia. (Jakarta) [Google Scholar]
- Indonesian Ministry of Health . 2020. Prevent Covid-19 with Germas. (Jakarta) [Google Scholar]
- Indonesian National Task Team Force for Coronovirus 2019 (Covid-19) 2020. Coronovirus 2019 (Covid-19) in Indonesia. (Jakarta) [Google Scholar]
- Karapiperis C., Kouklis P., Papastratos S., Chasapi A., Ouzounis C. 2020. Assessment for the Seasonality of Covid-19 Should Focus on Ultraviolet Radiation and Not ‘Warmer Days.’. [Google Scholar]
- Le Couteur D.G., Anderson R.M., Newman A.B. COVID-19 is a disease of older people. J. Gerontol. A Biol. Sci. Med. Sci. 2020:1–5. [Google Scholar]
- Miller B. Oak Publication Sdn Bhd; 2018. Immune System: Your Best Defense against Viruses and Bacteria from the Common Cold to the SARS Virus. [Google Scholar]
- Morley J.E., Vellas B. COVID-19 and older adult. J. Nutr. Health Aging. 2020;1 doi: 10.1007/s12603-020-1349-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Hospital Accreditation Commission . 2012. Hospital Accreditation Assessment. (Jakarta) [Google Scholar]
- Organization, W.H . 2020. Coronavirus Disease 2019 (COVID-19): Situation Report; p. 72. [Google Scholar]
- Organization, W.H . World Health Organization; 2020. Infection Prevention and Control Guidance for Long-Term Care Facilities in the Context of COVID-19: Interim Guidance, 21 March 2020. [Google Scholar]
- Organization, W.H . World Health Organization; 2020. Water, Sanitation, Hygiene and Waste Management for COVID-19: Technical Brief, 03 March 2020. [Google Scholar]
- Saglietto A., D’Ascenzo F., Zoccai G.B., De Ferrari G.M. COVID-19 in Europe: the Italian lesson. Lancet. 2020;395:1110–1111. doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagripanti J., Lytle C.D. Inactivation of influenza virus by solar radiation. Photochem. Photobiol. 2007;83:1278–1282. doi: 10.1111/j.1751-1097.2007.00177.x. [DOI] [PubMed] [Google Scholar]
- Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X., Bucci E., Piacentini M., Ippolito G., Melino G. 2020. COVID-19 Infection: The Perspectives on Immune Responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal T. A review of Coronavirus Disease-2019 (COVID-19) Indian J. Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slusky D., Zeckhauser R.J. National Bureau of Economic Research; 2018. Sunlight and Protection against Influenza. [DOI] [PubMed] [Google Scholar]
- Sternberg E., Engineer A. Is COVID-19 making you stay at home or“ shelter-in-place”? Turn your home into a healing space! [WWW document] Andrew Weil Cent. Integr. Med. 2020 https://integrativemedicine.arizona.edu/COVID19/sheltering_in_place.html URL. [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta. Indonesia. Sci. Total Environ. 2020;725:1–4. doi: 10.1016/j.scitotenv.2020.138436. 138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395:846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Fact or Fiction [WWW Document]. Nov. Coronavirus 2019. 2020. https://www.who.int/southeastasia/outbreaks-and-emergencies/novel-coronavirus-2019/fact-or-fiction URL.
- Xu B., Fan C., Wang A., Zou Y., Yu Y., He C., Xia W., Zhang J., Miao Q. 2020. Suppressed T Cell-Mediated Immunity in Patients with COVID-19: A Clinical Retrospective Study in Wuhan, China. (China (3/16/2020) [DOI] [PMC free article] [PubMed] [Google Scholar]