Abstract
Several studies have been published describing the clinical and radiographic findings of coronavirus disease 2019–related pneumonia. Therefore, there is currently a lack of pathologic data on its effects in intubated patients. Pneumothorax may occur rarely and results from a combination of fibrotic parenchyma and prolonged high-pressure ventilation. Chest drainage represents first-line treatment. However, in cases of persistent pneumothorax, thoracoscopy and bleb resection may be feasible options to reduce air leak and improve ventilation. This report describes the cases of 2 patients with coronavirus disease 2019 who were successfully treated with thoracoscopy, bleb resection, and pleurectomy for persistent pneumothorax.
The Video can be viewed in the online version of this article [https://doi.org/10.1016/j.athoracsur.2020.04.011] on http://www.annalsthoracicsurgery.org.
Histologic data describing the pathologic changes of lung parenchyma caused by coronavirus disease 2019 (COVID-19) are scarce.1 A recent report showed edema, proteinaceous exudate, focal reactive hyperplasia of pneumocytes with patchy inflammatory cellular infiltration, and multinucleated giant cells.2 This thickened, stiff tissue makes it difficult for lungs to work properly, and sustained-pressure ventilation may be necessary to obtain acceptable gas exchanges. In this setting, fibrotic parenchyma and preexisting emphysematous blebs are prone to rupture, with consequent risk of pneumothorax. Chest drains may be required; however, in cases of persistent air leak, minimally invasive thoracoscopy with bleb resection may be indicated.
Case Reports
Patient 1
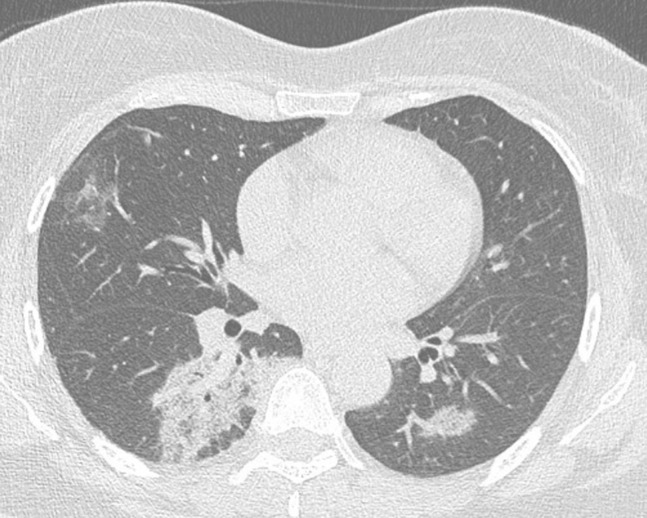
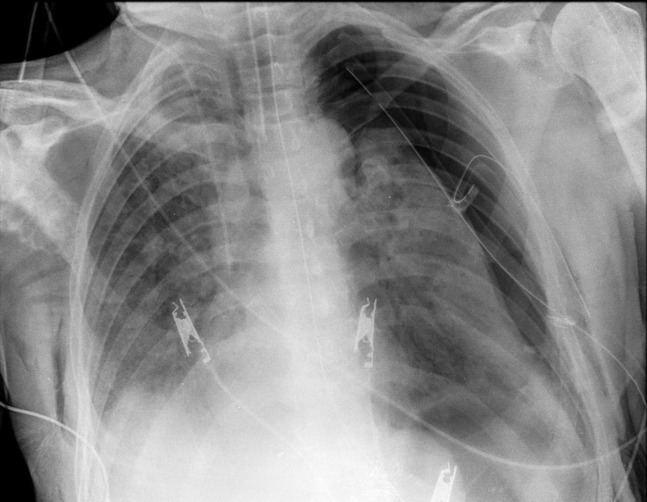
A 56-year-old man who was an active smoker was admitted to our hospital (Sant’Ambrogio Clinical Institute, University of Milan, Milan, Italy) for fever, cough, and respiratory distress. Laboratory values were as follows: white blood cells, 18,200/mm3; neutrophils, and 54%; C-reactive protein, 21.3 mg/dL. The nasopharyngeal swab test result was positive for COVID-19. The chest computed tomographic scan showed the presence of bilateral, peripheral ground-glass opacities (GGOs) (Figure 1 ). Because of worsening dyspnea, he was transferred to the intensive care unit (ICU) and intubated for acute respiratory insufficiency. Ventilator settings were as follows: tidal volume, 6 mL/kg; respiratory rate, 20 breaths/min; and positive end-expiratory pressure (PEEP) 10 cm H2O. Five days after intubation, the chest roentgenogram showed the presence of a left-sided pneumothorax, which was managed with a 28-Fr pleural drain (Figure 2 ). Because of the persistence of a significant air leak 7 days after drainage, a left-sided 3-port thoracoscopy in the right lateral decubitus position was planned. The inspection of the lung surface showed anthracotic pigmentation with significant air leakage coming from small, superficial bleb tears (Video). Blebs were grasped and resected using Endo GIA 60-mm black (4.0- to 5.0-mm) Tri-Staple technology (Medtronic, Minneapolis, MN). The suture line was checked and reinforced with human fibrin glue (Tisseel, Baxter, Deerfield, IL). No residual air leak was noticed, and mechanical pleurodesis was performed.
Figure 1.
The chest computed tomographic scan showed the presence of bilateral, peripheral ground-glass opacities.
Figure 2.
The chest roentgenogram showed persistent left-sided pneumothorax despite the presence of a 28-Fr chest tube.
Patient 2
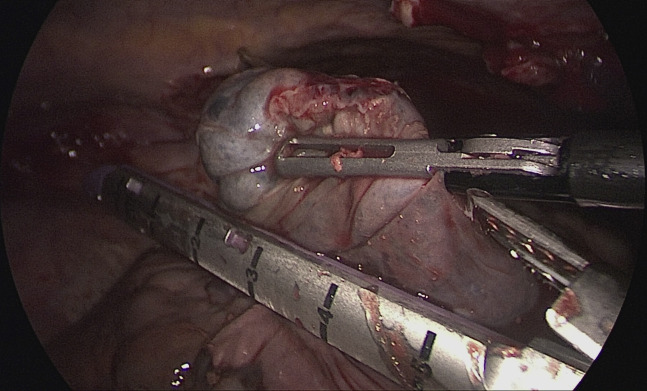
A 70-year-old man, positive for COVID-19 and without comorbidities, was transferred to our hospital for fatigue, fever, and respiratory distress. Laboratory values were as follows: white blood cells, 14,700/mm3; neutrophils, 48%; and C-reactive protein, 16.1 mg/dL. The chest computed tomographic scan confirmed the presence of bilateral, subpleural GGOs. He was admitted to the ICU and intubated for desaturation. Ventilator settings were as follows: tidal volume, 6 mL/kg; respiratory rate, 20 breaths/min; and PEEP, 8 cm H2O. Two days after intubation, the chest roentgenogram showed the presence of a left-sided pneumothorax, and a 28-Fr chest tube was placed. Three days after drainage, the pneumothorax was persistent, with substantial air leakage. A 3-port left-sided thoracoscopy was performed with the patient in the right lateral decubitus position. Inspection of the left lung showed lingular blebs with air leakage. Bleb resection with Endo GIA 60-mm purple (3.0- to 4.0-mm) Tri-Staple technology (Medtronic) (Figure 3 ), suture line fibrin glue reinforcement (Tisseel, Baxter), and pleural scratch were performed.
Figure 3.
Blebs were grasped and resected using Endo GIA Tri-Staple technology (Medtronic, Minneapolis, MN). The suture line was reinforced with fibrin glue.
These procedures were performed at the patient’s bedside in the ICU with nonselective low–tidal volume ventilation. A 28-Fr chest tube was placed at the end of the procedure. On postoperative day 1 there was no residual air leak, and the chest roentgenogram did not show evidence of residual pneumothorax in both cases. Drains were removed on postoperative day 2.
Comment
Reports of imaging findings in patients with COVID-19 are now emerging.3 The largest case series described multilobar involvement and rounded peripheral GGOs, whereas pneumothorax is rarely described as a presenting sign (1%).4 Iatrogenic pneumothorax related to mechanical ventilation is a potentially lethal complication reported in up to 15% of ventilated patients.5 Investigators have shown that iatrogenic pneumothorax occurs mostly in patients with an underlying lung disease (eg, chronic obstructive pulmonary disease, acute respiratory distress syndrome) during the early phase of intubation.6 As described for acute respiratory distress syndrome, the lungs of patients with COVID-19 who have significant interstitial involvement seem physiologically small, with low compliance and reduced elastance. This observation seems to be supported by recent pathologic findings showing edema, proteinaceous exudates, vascular congestion, and inflammatory changes.1 Therefore, overinflation and high PEEP in such fibrotic and hypoelastic lungs may cause alveolar or preexisting bleb rupture.
Iatrogenic pneumothorax in intubated patients with COVID-19 is uncommon but may be seen with progression of the disease.3 Although chest tube placement should be considered first-line treatment, the persistence of an air leak may constitute an indication for low–tidal volume 2-lung ventilation thoracoscopy.7 , 8 Ideal timing of the procedure is unclear and was discussed by a multidisciplinary team in our cases. In the first case, after chest tube placement, a wait-and-see strategy was preferred because of doubts about the effectiveness of the procedure. In the second case, a more aggressive and earlier operative attempt was planned. Although the procedure was successful in both patients, because of a stiffer parenchyma in the first case, black cartridges were used for resection. Hence, we believe that an early indication for thoracoscopy may be presumably better because the interstitial tissues are less traumatized, less fibrotic, and less inflamed.
This report describes 2 patients with COVID-19 who were treated with thoracoscopy and bleb resection for persistent pneumothorax. Treatment of pneumothorax in these patients is uncertain. Although chest tube drainage seems indicated as a first-step treatment, thoracoscopy may be warranted in cases of persistent or recurrent pneumothorax. Timing of minimally invasive treatment is unclear; therefore, an early indication for thoracoscopy may presumably result in better outcomes and more effective air leak control.
Supplementary Data
References
- 1.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian S., Hu W., Niu L., Liu H., Xu H., Xiao S.Y. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salehi S., Abedi A., Balakrishnan S., Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215:87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 4.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sassoon C.S., Light R.W., O'Hara V.S., Moritz T.E. Iatrogenic pneumothorax: etiology and morbidity. Results of a Department of Veterans Affairs Cooperative Study. Respiration. 1992;59:215–220. doi: 10.1159/000196061. [DOI] [PubMed] [Google Scholar]
- 6.Hsu C.W., Sun S.F. Iatrogenic pneumothorax related to mechanical ventilation. World J Crit Care Med. 2014;3:8–14. doi: 10.5492/wjccm.v3.i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cerfolio R.J. Advances in thoracostomy tube management. Surg Clin North Am. 2002;82:833–848. doi: 10.1016/s0039-6109(02)00026-9. [DOI] [PubMed] [Google Scholar]
- 8.Kim H., Kim H.K., Choi Y.H., Lim S.H. Thoracoscopic bleb resection using two-lung ventilation anesthesia with low tidal volume for primary spontaneous pneumothorax. Ann Thorac Surg. 2009;87:880–885. doi: 10.1016/j.athoracsur.2008.12.071. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.