Highlights
-
•
Co-infections of RSV are common in acute lower respiratory tract infections.
-
•
Co-infection of RSV has no significant effect on clinical presentation except fever.
-
•
RSV-B shows a more local pattern in Hangzhou.
-
•
A new genotype, BA11 was identified.
Keywords: Human respiratory syncytial virus, Co-infection, Epidemic pattern, Genotype, Children
Abstract
Background
Human respiratory syncytial virus (RSV) is the most important viral pathogen in children. However, its epidemic patterns and co-infection characteristics are not fully understood.
Objectives
We attempted to determine the level of genetic variation of RSV, and describe the prevalence and co-infection characteristics of RSV in Hangzhou during two epidemic seasons.
Study design
Single respiratory samples from 1820 pediatric patients were screened for RSV and genotyped by RT-PCR and sequencing. In all RSV positive specimens, we screened for viruses and atypical bacteria. Demographic and clinical information was recorded and analyzed.
Results
A total of 34.5% and 3.8% of samples from acute lower respiratory tract infections (ALRI) and influenza-like illness (ILI) were positive for RSV, respectively. Phylogenetic analysis revealed that 61.1% of the selected 167 RSV strains were NA1, 31.1% were BA, 3.6% were ON1, 2.4% were CB1, and 1.8% were NA3. A new genotype, BA11 was identified, which comprised 98.1% of BA strains in this study, while the rest were BA10. A total of 36.4% and 9.1% of RSV-positive children with ALRI and ILI respectively were found to be co-infected. Rhinovirus was the most common additional respiratory virus, followed by human metapneumovirus. Except for fever, no significant differences in other clinical presentation between the RSV mono-infection and co-infection groups were observed.
Conclusions
The circulating RSV strains had high genetic variability with RSV-B showing a more local pattern. In ALRI cases, co-infection of RSV with other viruses or atypical bacteria has no significant effect on the clinical presentation except fever.
1. Background
Human respiratory syncytial virus (RSV) is the most important viral agent of acute respiratory infections in infants, young children and immunocompromised and elderly individuals [1], [2]. RSV can be rapidly transmitted within childcare institutions [3]. Infection with RSV can result in mild to severe illness, including lower respiratory syndromes such as bronchiolitis and pneumonia. It has been estimated that nearly all two-year-old children have been infected [4]. The attachment G glycoprotein (G protein), a type II glycoprotein, is the most variable region both within and between the major RSV genotypes [5]. The G protein contains 2 hypervariable regions (HVR), with the second HVR (HVR2), located at the C-terminal end, which is widely used to study the genetic diversity of RSV [6], [7]. To date, 13 RSV-A genotypes, GA1-GA7 [8], [9], SAA1 [10], NA1-NA4 [11], [12], and ON1 [13], and 22 RSV-B genotypes, GB1-GB4 [8], BA1-BA6 [14], BA7-BA10 [15], SAB1-SAB3 [10], SAB4[16], URU1-URU2 [17], CB1, and BA-C [12] have been identified based on sequence analyses of HVR2. The frequent appearance of new genotypes may facilitate RSV evasion of existing herd immunity, further influencing disease severity, causing repeated infections and even larger outbreaks [11], [18].
The study of the genetic variability of RSV is necessary to better understand its molecular epidemiology. The relationship between the clinical symptoms and co-infection of RSV with other pathogens has been evaluated in previous studies with different approaches and conclusions [19], [20], [21]. Moreover, there is little information available on RSV infection among children with influenza -like illness (ILI) and on the distribution pattern of RSV epidemic strains in Hangzhou, Southeast China.
2. Objectives
We attempted to describe the prevalence, clinical, molecular and co-infection characteristics of RSV in children with acute lower respiratory tract infections (ALRI) and influenza-like illness (ILI) in Hangzhou, China.
3. Study design
3.1. Patients and specimens
Samples were collected from April 2011 to March 2013. 652 lower respiratory tract aspirates were collected from children (inpatients) admitted with symptoms of ALRI. 1168 throat swabs were collected from children (outpatients) with symptoms of influenza-like illness. All the samples are collected every week in The Chindren’s Hospital Zhejiang University School of Medicine, China. Informed consent was obtained from the parents of all children who provided specimens. All specimens were collected and transported immediately to the laboratory at Hangzhou Center for Disease Control and Prevention, and stored at −80 °C prior to testing. Demographic and clinical data were recorded.
3.2. Nucleotide extraction and cDNA synthesis
Viral RNA was extracted from 200 μL of each specimen, using the QIAamp viral RNA minikits (Qiagen, Germany). Viral DNA was extracted from 200 μL of each specimen, using the QIAamp viral DNA minikits (Qiagen, Germany). RNA and DNA were eluted in 50 μL of Qiagen TE buffer respectively and stored at -80°C until analyzed. cDNA was synthesized using random hexamer primers with PrimeScript II 1st Strand cDNA Synthesis Kit (Takara, Dalian, China).
3.3. Virus detection
For RSV screening, Real time PCR was performed, with subgroup-specific primers and probes used to amplify N gene as described elsewhere [22]. Primers RSVGF (5′-TCACTTTGAAGTGTTCAACT-3′) and RSVGR (5′-GGCAACTCCATTGTTATTTG-3′) were used to amplify RSV G protein for both genotype A and B strains in All RSV positive specimens [23]. All RSV positive specimens were screened for human metapneumo-virus (HMPV), influenza virus A and B (FluA and FluB), parainfluenza virus types 1 to 3 (PIV1 to 3), human rhinoviruses (HRV), and human coronaviruses (HCoVs: 229E, OC43, NL63, and HKU1), saffold virus (SAFV), adenovirus (ADV), human bocavirus (HBoV) and mycoplasma pneumonia (MP), chlamydia pneumonia (CP) using real time PCR [22], [24], [25], [26], [27], [28], [29], [30].
3.4. Sequencing and phylogenetic analysis
All RSV positive PCR products were sequenced by Sangon Biotech (Shanghai) Co., Ltd. Nucleotide sequences of reference strains were obtained from GenBank and used to construct alignments and phylogeny. The nucleotide and amino acid sequences of the group A and B viruses were aligned separately with RSV reference strains by using ClustalX 1.81. Phylogenetic trees were constructed by the neighbor-joining method using MEGA 5.0. Statistical significance of tree topologies was tested by bootstrapping (1000 replicates).
3.5. Statistical analysis
Significant differences in rates between various groups were tested with a chi-square test, a P value of <0.05 was considered to be statistically significant. Analyses were performed with SPSS17.0 software.
3.6. Nucleotide sequence accession numbers
Representative HVR2 sequences used in this study were submitted to GenBank under accession numbers KP336492 to KP336546.
4. Results
4.1. Patient characteristics
A total of 1820 children were tested for RSV in this study. The ages of children ranged from 1 month to 11 years. The majority of patients (92.8%) were under 5 years old. The ratio of boys to girls was 1.61:1, and the ratio of inpatients to outpatients was 1:1.79.
4.2. RSV distribution
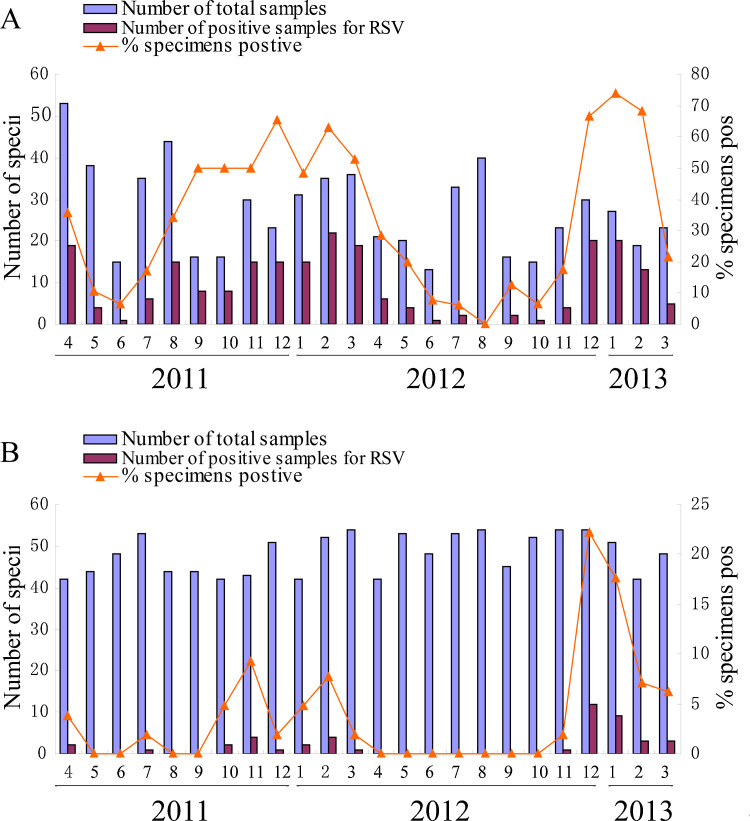
We found that 34.5% (225/652) and 3.8% (44/168) of samples from ALRI and ILI cases, respectively, were positive for RSV and the difference between the two groups was significant (p < 0.001). While the epidemic season and epidemic peak of RSV were similar in the two groups. The majority of cases (71.6%) were reported in the winter to spring months (November to March) (Fig. 1 ). All samples were determined as group A or group B by real time RT-PCR: 169 samples were identified as RSV A positive, and 99 samples were identified as RSV B positive. RSV A strains were predominant in the 2011–2012 epidemic season, accounting for 93.0% of cases. The predominant strains changed from group A to group B (76.7%) during the 2012–2013 period. RSV-A and RSV-B were co-circulating during these two RSV seasons. From 268 RSV positive samples, 167HVR2 sequences were obtained for subgroup analysis. The failure in the amplification of viral genomic fragments in the other samples may be due to low viral loads or variations in primer binding sites. 111 RSV A specimens and 56 RSV B specimens were sequenced successfully. Subgroup distribution of RSV A and RSV B infections in children with ALRI or ILI is shown (Table 1 ).
Fig. 1.
Monthly distribution of RSV infections in ALRI (A) and ILI (B).
Table 1.
Subgroup distribution of RSV A and RSV B infections in children with ALRI or ILI from 2011 to 2013.
| Epidemic season | No. of samples | No. (%) of RSV positive samples | No. (%) of RSV cases by subgroup: |
No. of RSV-A genotypes (N = 111) |
No. of RSV-B genotypes (N = 56) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RSV A | RSV B | ON1 | NA1 | NA3 | CB1 | BA10 | BA11 | ||||
| ALRI | 2011–2012 | 372 | 147(39.5) | 137(93.2) | 10(6.8) | 1 | 91 | 2 | 2 | 1 | 6 |
| 2012–2013 | 280 | 78(27.9) | 14(17.9) | 64(82.1) | 5 | 7 | 1 | 2 | 0 | 43 | |
| Total | 652 | 225(34.5) | 151(67.1) | 74(32.9) | 6 | 98 | 3 | 4 | 1 | 49 | |
| ILI | 2011–2012 | 582 | 17(2.9) | 16(94.1) | 1(5.9) | 0 | 4 | 0 | 0 | 0 | 0 |
| 2012–2013 | 586 | 26(4.4) | 2(7.7) | 24(92.3) | 0 | 0 | 0 | 0 | 0 | 2 | |
| Total | 1168 | 44(3.9) | 19(43.2) | 25(56.8) | 0 | 4 | 0 | 0 | 0 | 2 | |
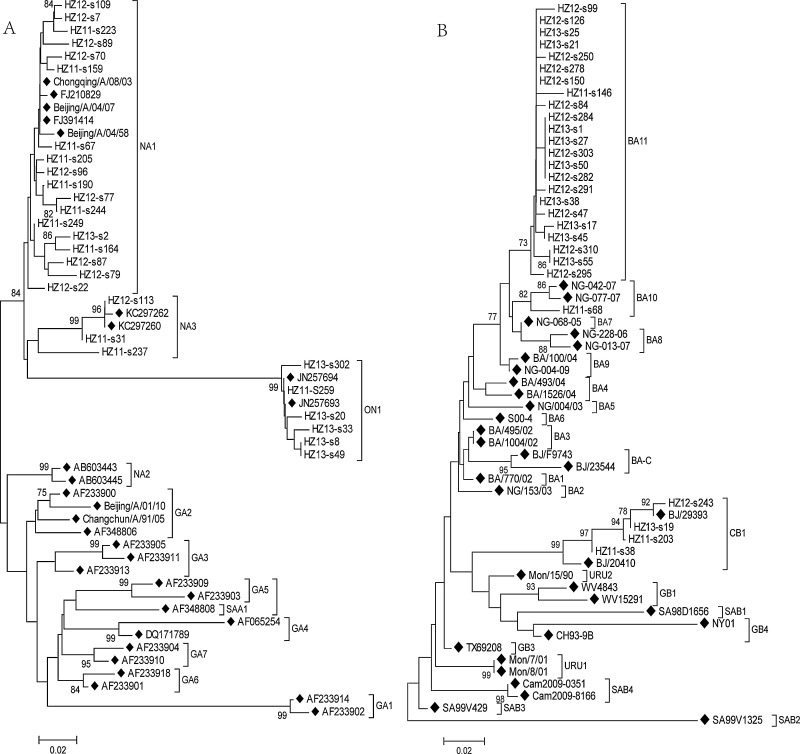
4.3. Phylogenetic analysis of RSV
HVR2 sequences obtained in the present study were aligned with the HVR2 sequences of other reported strains found in GenBank (Fig. 2 ). Phylogenetic analysis revealed that the 111 subgroup A strains clustered into three groups: 6 strains with a 72-nucleotide duplication clustered as the ON1 genotype, 3 strains clustered as the NA3 genotype, 102 strains clustered as the NA1 genotype. The nucleotide and amino acid homologies among the strains ranged from 90.9 to 100% and 79.7 to 100%, respectively. The 56 subgroup B strains clustered into three groups: 4 were placed in the CB1 genotype, 1 was placed in the BA10 genotype, and 51 strains which did not cluster with other BA strains with a high bootstrap value, were placed in a new genotype, BA11, for RSV-B (Fig 2). Major nodes with bootstrap values of >50% were considered a cluster [15]. Bootstrap value of cluster BA11 was 74%. Furthermore, the maximum p-distance of cluster BA11 was 0.027. The nucleotide and amino acid homologies among these group B viruses were from 79.8 to 100% and from 65.7 to 100%, respectively. The BA11 strains shared 95.8 to 100% nucleotide identity and 96.1 to 100% amino acid identity.
Fig. 2.
Phylogenetic trees of RSV group A (A) and group B (B) nucleotide sequences from the second variable region of the G protein. Reference strains obtained from GenBank are marked with ◆.
4.4. Co-infection with the other respiratory viruses and atypical bacteria
36.4 % (82/225) of all RSV-positive hospitalized children with ALRI were found to be co-infected with at least one of the other respiratory viruses or atypical bacteria, and 9.1% (4/44) of RSV-positive outpatient with ILI were found to be co-infected (Table 2 ). The difference in the two groups was significant (p < 0.001). In total, the highest co-infection rate of RSV was with HRV (24/82), the second-highest was with HMPV (18/82), but there were no significant differences (p = 0.283). Co-infections of RSV with saffold virus, human coronavirus 229E and PIV were also observed. Double infections were most frequent in ALRI, with triple and quadruple infections being common. Combinations of pathogens in the co-infections were various, and no obvious patterns observed.
Table 2.
Co-infection of RSV with other viruses and atypical bacteria.
| Viruses | No. of samples | Viruses | No. of samples | Viruses | No. of samples | |
|---|---|---|---|---|---|---|
| ALRIa | RSV + HRV | 17 | RSV + ADV | 2 | RSV + SAFV + HMPV | 2 |
| RSV + HMPV | 12 | RSV + MP + CP | 3 | RSV + HRV + HMPV | 1 | |
| RSV + SAFV | 10 | RSV + HBoV | 1 | RSV + ADV + MP | 2 | |
| RSV + 229E | 5 | RSV + HMPV + Mp | 1 | RSV + ADV + HBoV | 1 | |
| RSV + PIV | 5 | RSV + HRV + PIV | 4 | RSV + PIV + ADV | 1 | |
| RSV + MP | 6 | RSV + Flu + HMPV | 2 | RSV + Flu + SAFV + MP | 1 | |
| RSV + Flu | 2 | RSV + HRV + HBoV | 2 | RSV + Flu + SAFV + ADV | 1 | |
| ILIb | RSV + HRV | 1 | RSV + PIV | 1 | RSV + Flu | 2 |
82 Co-infections among 225 RSV positive samples in ALRI.
4 Co-infections among 44 RSV positive samples in ILI.
4.5. Clinical characteristics of RSV infection
Complete information on the clinical characteristics was available for the 225 RSV positive patients, and all were suffering from ALRI. The most frequent clinical findings among RSV-positive patients were cough (95%), fever (57%), and wheezing (50%). Chest radiographs were obtained from 101 RSV-positive patients, and 93 showed abnormal findings: 53 patients had intrapulmonary punctate and patchy shadows, 39 displayed coarse lung markings, and 1 had lobar infiltrations. Except for fever, there were no significant differences with respect to other clinical presentations observed in RSV-positive children (Table 3 ). Fever rate was significantly higher among the co-infection group (p < 0.001). Although infection rates had no significant difference between the two age groups, patients in the younger groups (≤12 months old) were more prone to be co-infected with other respiratory viruses and atypical bacteria (p = 0.051).
Table 3.
Comparison of clinical manifestations in the RSV Mono-infection group and co-infection group with ALRI
| Characteristic | No. (%) of patients in group with: |
P value | |
|---|---|---|---|
| Mono-infection (n = 143) |
Co-infection (n = 82) |
||
| Age(MO) | |||
| >12 | 127(88.8) | 65(79.3) | 0.051a |
| ≤12 | 16(11.2) | 17(20.7) | |
| Symptoms | |||
| Cough | 140(97.9) | 81(98.8) | 1.000b |
| Fever | 34(23.8) | 48(58.5) | 0.000a |
| Shortness of breath | 60(42.0) | 34(41.5) | 0.942a |
| Abnormality of lung Identified by X-ray | 117(81.8) | 71(86.6) | 0.353a |
| Congenital heart disease | 17(11.9) | 12(14.6) | 0.554a |
| Complication | |||
| Pneumonia | 123(86.0) | 76(92.7) | 0.132a |
| Respiratory failure | 10(7.0) | 7(8.5) | 0.673a |
| Hepatic insufficiency | 7(4.9) | 4(4.9) | 1.000b |
Chi-square test.
Continuity correction.
5. Discussion
While RSV infection was shown to be often associated with acute respiratory tract infections (ARTI), there is less knowledge about RSV infection among children with influenza-like illness (ILI). In this study higher rates of RSV infections were found in children with ALRI (34.5%) compared to children with ILI (3.8%). Similar rates for ALRI patients were found in other studies [29], [31], [32], while for ILI the rates in Hangzhou were lower than found in a study of children with fever and respiratory symptoms conducted in Shanghai, China: 3.8% versus7.6%, respectively [33].
The clinical implications of multiple viral infections remain controversial. Several studies have shown that respiratory virus co-infection may increase the clinical severity of RSV disease [20], [34], whereas other studies have reported opposite findings[19], [21], [31]. Franz et al. [34] reported that RSV/non-RSV co-infection was more strongly associated with pneumonia than RSV single infection. Harada et al. [20] reported that the association with moderate-to-severe nonpneumonic ARI cases was stronger with RSV/non-RSV respiratory virus co-infection than with RSV mono-infection. While equivalent clinical severity was observed between children with single RSV virus infection and virus co-infection [19]. Our study shows a significant difference found in fever rates between mono-infected and co-infected groups of RSV-positive patients, while there was no difference found in fever rates reported by Zhang et al., [31]. These differences may be attributable to variations in clinical settings, study populations, the type of clinical sample, the seasonality of circulating viruses and even bacteria co-infections.
Analysis of the genotype distribution of Hangzhou showed that six RSV genotypes were found in the two epidemic seasons studied. Most of Hangzhou RSV-A strains were classified as NA1 genotype. Similar situations were reported in Italy, Beijing and Shanghai of China during the same period [12], [33], [35]. Most of BA viruses in this study further clustered with BA11, a new genotype within BA lineage. BA11 genotype is not associated with large outbreaks in the community. Since during the second RSV season (2012–2013), when this strain predominated, morbidity levels were relatively low. Only BA9 and BA10 strains were detected in Shanghai and Beijing, during the same period. CB1 and NA3 are newly found genotypes identified in Beijing, and also detected in Shanghai and Hangzhou, but were not found to circulate in Belgium and Italy [35], [36]. It may indicate that RSVB distributions have more regional characteristics.
ON1 genotype carries the ON1-specific 24-amino acid repeat, and represents a newly characterized RSV genotype identified in Canada in December 2010 [13]. Since then, it was detected sporadically in other regions (e.g., China, Korea, South Africa, Italy) [12], [37], [38]. Our lab found 6 ON1 strains. One was detected early in 2011. It is interesting to point out that ON1 genotype strains appear to have emerged during the same period. The precise geographic distribution of ON1 genotype still awaits further elucidation. By early 2013, ON1 strains had spread so efficiently that they had nearly replaced other RSV-A strains in Italy [35]. In Hangzhou, we have only collected the samples from January to March in 2013. Among the 38 RSV positive strains, there were only 6 RSV-A strains, among them, 5 were successfully sequenced and all belonged to the ON1 genotype. This result suggests that the ON1 genotype has become the dominant genotype of RSV-A in Hangzhou.
Our study may indicate that the novel RSV variants have a fairly rapid global spread, and RSV-B showed a more local pattern. Similar patterns were observed in Kilifi, Kenya[39], the 27 novel Kilifi RSV genomes (11 RSVA and 16 RSVB) were used to assess local versus global RSV variety. Kilifi RSV strains are similar to strains that circulate in other regions of the world and reveal only limited local evolution. Phylogenetic clustering appeared to be more influenced by time of virus sample collection than by geographical location. Also, Agoti CN et al. [39] indicated that RSVB variants may spread less efficiently, with a higher variation, which is specific for local. Our study clarified this phenomenon, it may have strong consequences on the efficacy of any RSV vaccine used locally.
The deduced amino acid homologies of HVR2 in HRV-A were 79.7 to 100%, and two different G protein lengths (86 amino acids (aa), 110 aa) were observed; Among all group B strains, the deduced amino acid homologies in HVR2 were 65.7 to 100% and four different G protein lengths (80 aa, 83 aa, 86 aa, and 100 aa) were observed. These results demonstrate that subgroup B viruses display more mechanisms of variation in the G gene than subgroup A viruses. Similar amino acid homologies were also observed by Zhang and colleagues [31]. The variation was greatest among the four CB1 strains where three different lengths of the protein G were found (80aa, 83aa and 86aa). This prompts further RSV monitoring, particularly of CB1 genotype.
RSV is a very important pathogen in children with ALRI in Hangzhou, China. Since the present study was limited to a period of two years, additional consecutive investigations should be conducted in order to provide useful information about RSV prevalence, variation and control.
Funding
This work was supported by Hangzhou Scientific and Technological Development Program of China (Grant No. 20120533Q24).
Competing interests
The authors declare that they have no competing interests. All authors approved the final manuscript.
Ethical approval
This study was approved by the ethics committee of the Hangzhou Center for Disease Control and Prevention, China (2012).
Acknowledgments
We thank Jean K. Millet, PhD of Cornell University for critical reading of the manuscript.
References
- 1.Falsey A.R., Hennessey P.A., Formica M.A., Cox C., Walsh E.E. Respiratory syncytial virus infection in elderly and high-risk adults. N. Engl. J. Med. 2005;352(17):1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 2.Nair H., Nokes D.J., Gessner B.D., Dherani M., Madhi S.A., Singleton R.J. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chu H.Y., Kuypers J., Renaud C., Wald A., Martin E., Fairchok M. Molecular epidemiology of respiratory syncytial virus transmission in childcare. J. Clin. Virol. 2013;57(4):343–350. doi: 10.1016/j.jcv.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cane P.A. Molecular epidemiology of respiratory syncytial virus. Rev. Med. Virol. 2001;11(2):103–116. doi: 10.1002/rmv.305. [DOI] [PubMed] [Google Scholar]
- 5.Johnson P.R., Spriggs M.K., Olmsted R.A., Collins P.L. The G glycoprotein of human respiratory syncytial viruses of subgroups A and B: extensive sequence divergence between antigenically related proteins. Proc. Natl. Acad. Sci. U. S. A. 1987;84(16):5625–5629. doi: 10.1073/pnas.84.16.5625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parveen S., Sullender W.M., Fowler K., Lefkowitz E.J., Kapoor S.K., Broor S. Genetic variability in the G protein gene of group A and B respiratory syncytial viruses from India. J. Clin. Microbiol. 2006;44(9):3055–3064. doi: 10.1128/JCM.00187-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reiche J., Schweiger B. Genetic variability of group A human respiratory syncytial virus strains circulating in Germany from 1998 to 2007. J. Clin. Microbiol. 2009;47(6):1800–1810. doi: 10.1128/JCM.02286-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peret T.C., Hall C.B., Schnabel K.C., Golub J.A., Anderson L.J. Circulation patterns of genetically distinct group A and B strains of human respiratory syncytial virus in a community. J. Gen. Virol. 1998;79(Pt 9):2221–2229. doi: 10.1099/0022-1317-79-9-2221. [DOI] [PubMed] [Google Scholar]
- 9.Peret T.C., Hall C.B., Hammond G.W., Piedra P.A., Storch G.A., Sullender W.M. Circulation patterns of group A and B human respiratory syncytial virus genotypes in 5 communities in North America. J. Infect. Dis. 2000;181(6):1891–1896. doi: 10.1086/315508. [DOI] [PubMed] [Google Scholar]
- 10.Venter M., Madhi S.A., Tiemessen C.T., Schoub B.D. Genetic diversity and molecular epidemiology of respiratory syncytial virus over four consecutive seasons in South Africa: identification of new subgroup A and B genotypes. J. Gen. Virol. 2001;82(Pt 9):2117–2124. doi: 10.1099/0022-1317-82-9-2117. [DOI] [PubMed] [Google Scholar]
- 11.Shobugawa Y., Saito R., Sano Y., Zaraket H., Suzuki Y., Kumaki A. Emerging genotypes of human respiratory syncytial virus subgroup A among patients in Japan. J. Clin. Microbiol. 2009;47(8):2475–2482. doi: 10.1128/JCM.00115-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cui G., Zhu R., Qian Y., Deng J., Zhao L., Sun Y. Genetic variation in attachment glycoprotein genes of human respiratory syncytial virus subgroups a and B in children in recent five consecutive years. PLoS One. 2013;8(9):e75020. doi: 10.1371/journal.pone.0075020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eshaghi A., Duvvuri V.R., Lai R., Nadarajah J.T., Li A., Patel S.N. Genetic variability of human respiratory syncytial virus A strains circulating in Ontario: a novel genotype with a 72 nucleotide G gene duplication. PLoS One. 2012;7(3):e32807. doi: 10.1371/journal.pone.0032807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trento A., Galiano M., Videla C., Carballal G., Garcia-Barreno B., Melero J.A. Major changes in the G protein of human respiratory syncytial virus isolates introduced by a duplication of 60 nucleotides. J. Gen. Virol. 2003;84(Pt 11):3115–3120. doi: 10.1099/vir.0.19357-0. [DOI] [PubMed] [Google Scholar]
- 15.Dapat I.C., Shobugawa Y., Sano Y., Saito R., Sasaki A., Suzuki Y. New genotypes within respiratory syncytial virus group B genotype BA in Niigata, Japan. J. Clin. Microbiol. 2010;48(9):3423–3427. doi: 10.1128/JCM.00646-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnott A., Vong S., Mardy S., Chu S., Naughtin M., Sovann L. A study of the genetic variability of human respiratory syncytial virus (HRSV) in Cambodia reveals the existence of a new HRSV group B genotype. J. Clin. Microbiol. 2011;49(10):3504–3513. doi: 10.1128/JCM.01131-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanc A., Delfraro A., Frabasile S., Arbiza J. Genotypes of respiratory syncytial virus group B identified in Uruguay. Arch. Virol. 2005;150(3):603–609. doi: 10.1007/s00705-004-0412-x. [DOI] [PubMed] [Google Scholar]
- 18.Yamaguchi M., Sano Y., Dapat I.C., Saito R., Suzuki Y., Kumaki A. High frequency of repeated infections due to emerging genotypes of human respiratory syncytial viruses among children during eight successive epidemic seasons in Japan. J. Clin. Microbiol. 2011;49(3):1034–1040. doi: 10.1128/JCM.02132-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asner S.A., Rose W., Petrich A., Richardson S., Tran D.J. Is virus coinfection a predictor of severity in children with viral respiratory infections. Clin. Microbiol. Infect. 2015;21(3):261–264. doi: 10.1016/j.cmi.2014.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harada Y., Kinoshita F., Yoshida L.M., Minh L.N., Suzuki M., Morimoto K. Does respiratory virus coinfection increases the clinical severity of acute respiratory infection among children infected with respiratory syncytial virus. Pediatr. Infect. Dis. J. 2013;32(5):441–445. doi: 10.1097/INF.0b013e31828ba08c. [DOI] [PubMed] [Google Scholar]
- 21.Martinez-Roig A., Salvado M., Caballero-Rabasco M.A., Sanchez-Buenavida A., Lopez-Segura N., Bonet-Alcaina M. Viral coinfection in childhood respiratory tract infections. Arch. Bronconeumol. 2015;51(1):5–9. doi: 10.1016/j.arbr.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raymond F., Carbonneau J., Boucher N., Robitaille L., Boisvert S., Wu W.K. Comparison of automated microarray detection with real-time PCR assays for detection of respiratory viruses in specimens obtained from children. J. Clin. Microbiol. 2009;47(3):743–750. doi: 10.1128/JCM.01297-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jalal H., Bibby D.F., Bennett J., Sampson R.E., Brink N.S., MacKinnon S. Molecular investigations of an outbreak of parainfluenza virus type 3 and respiratory syncytial virus infections in a hematology unit. J. Clin. Microbiol. 2007;45(6):1690–1696. doi: 10.1128/JCM.01912-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu X.F., Pan J.C., Ye R., Xiang H.Q., Kou Y., Huang Z.C. Preparation of armored RNA as a control for multiplex real-time reverse transcription-PCR detection of influenza virus and severe acute respiratory syndrome coronavirus. J. Clin. Microbiol. 2008;46(3):837–841. doi: 10.1128/JCM.01904-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van de Pol A.C., van Loon A.M., Wolfs T.F., Jansen N.J., Nijhuis M., Breteler E.K. Increased detection of respiratory syncytial virus, influenza viruses, parainfluenza viruses, and adenoviruses with real-time PCR in samples from patients with respiratory symptoms. J. Clin. Microbiol. 2007;45(7):2260–2262. doi: 10.1128/JCM.00848-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deffernez C., Wunderli W., Thomas Y., Yerly S., Perrin L., Kaiser L. Amplicon sequencing and improved detection of human rhinovirus in respiratory samples. J. Clin. Microbiol. 2004;42(7):3212–3218. doi: 10.1128/JCM.42.7.3212-3218.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Damen M., Minnaar R., Glasius P., van der Ham A., Koen G., Wertheim P. Real-time PCR with an internal control for detection of all known human adenovirus serotypes. J. Clin. Microbiol. 2008;46(12):3997–4003. doi: 10.1128/JCM.00563-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drexler J.F., Luna L.K., Stocker A., Almeida P.S., Ribeiro T.C., Petersen N. Circulation of 3 lineages of a novel Saffold cardiovirus in humans. Emerg. Infect. Dis. 2008;14(9):1398–1405. doi: 10.3201/eid1409.080570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bezerra P.G., Britto M.C., Correia J.B., Duarte M.C., Fonceca A.M., Rose K. Viral and atypical bacterial detection in acute respiratory infection in children under five years. PLoS One. 2011;6(4):e18928. doi: 10.1371/journal.pone.0018928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Touati A., Benard A., Hassen A.B., Bebear C.M., Pereyre S. Evaluation of five commercial real-time PCR assays for detection of Mycoplasma pneumoniae in respiratory tract specimens. J. Clin. Microbiol. 2009;47(7):2269–2271. doi: 10.1128/JCM.00326-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang R.F., Jin Y., Xie Z.P., Liu N., Yan K.L., Gao H.C. Human respiratory syncytial virus in children with acute respiratory tract infections in China. J. Clin. Microbiol. 2010;48(11):4193–4199. doi: 10.1128/JCM.00179-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang X.L., Shao X.J., Wang J., Guo W.L. Temporal characteristics of respiratory syncytial virus infection in children and its correlation with climatic factors at a public pediatric hospital in Suzhou. J. Clin. Virol. 2013;58(4):666–670. doi: 10.1016/j.jcv.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 33.Liu J., Mu Y., Dong W., Yao F., Wang L., Yan H. Genetic variation of human respiratory syncytial virus among children with fever and respiratory symptoms in Shanghai, China, from 2009 to 2012. Infect. Genet. Evol. 2014;27:131–136. doi: 10.1016/j.meegid.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 34.Franz A., Adams O., Willems R., Bonzel L., Neuhausen N., Schweizer-Krantz S. Correlation of viral load of respiratory pathogens and co-infections with disease severity in children hospitalized for lower respiratory tract infection. J. Clin. Virol. 2010;48(4):239–245. doi: 10.1016/j.jcv.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pierangeli A., Trotta D., Scagnolari C., Ferreri M.L., Nicolai A., Midulla F. Rapid spread of the novel respiratory syncytial virus A ON1 genotype, central Italy, 2011 to 2013. Euro Surveill. 2014;19(26) doi: 10.2807/1560-7917.es2014.19.26.20843. [DOI] [PubMed] [Google Scholar]
- 36.Houspie L., Lemey P., Keyaerts E., Reijmen E., Vergote V., Vankeerberghen A. Circulation of HRSV in Belgium: from multiple genotype circulation to prolonged circulation of predominant genotypes. PLoS One. 2013;8(4):e60416. doi: 10.1371/journal.pone.0060416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee W.J., Kim Y.J., Kim D.W., Lee H.S., Lee H.Y., Kim K. Complete genome sequence of human respiratory syncytial virus genotype A with a 72-nucleotide duplication in the attachment protein G gene. J. Virol. 2012;86(24):13810–13811. doi: 10.1128/JVI.02571-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Valley-Omar Z., Muloiwa R., Hu N.C., Eley B., Hsiao N.Y. Novel respiratory syncytial virus subtype ON1 among children, Cape Town, South Africa, 2012. Emerg. Infect. Dis. 2013;19(4):668–670. doi: 10.3201/eid1904.121465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agoti C.N., Otieno J.R., Munywoki P.K., Mwihuri A.G., Cane P.A., Nokes D.J. Local evolutionary patterns of human respiratory syncytial virus derived from whole-genome sequencing. J. Virol. 2015;89(7):3444–3454. doi: 10.1128/JVI.03391-14. [DOI] [PMC free article] [PubMed] [Google Scholar]