Abstract
International collaboration and understanding is becoming increasingly important as we face a soaring number of emerging and re-emerging infectious diseases. Management of these conditions calls for a cohesive international effort, with contributions from many infectious disease specialists. To optimise collaborative efforts, an international understanding of training, capabilities, and skills would be valuable. An investigation of postgraduate training programmes in the infectious disease specialties around the world was done. 33 countries contributed information. 26 of these countries had established training programmes—one of which was changing its duration and research component; three were in the process of setting up programmes, two provided specialist training that had no official recognition, and two had no specialist training. In addition to promoting international understanding and collaboration, this article should catalyse a global assessment of postgraduate training programmes within the field of infectious diseases.
Introduction
The global importance of tackling infectious pathogens has been emphasised recently with the rapid international spread of emerging and re-emerging infectious diseases, such as severe acute respiratory syndrome, West Nile virus, and avian influenza, and the threat of bioterrorism.1 The prevention and management of infectious diseases in refugees, internally displaced people, and disaster situations is an ever increasing problem. One essential arm of defence is experienced and competent personnel who have received training in the management of infectious diseases and can work together effectively. National and international capabilities for handling infectious diseases are wholly dependent on communication, collaboration, and a solid bedrock of appropriate training. An understanding of the training provided across the international community would help to facilitate better collaboration and communication. In addition, increasing awareness of the training and skills of colleagues overseas may provide other benefits, such as highlighting training and research opportunities,2 developing clinical and public-health networks, and sharing educational goals and expertise. Combating emerging and re-emerging infectious diseases cannot be achieved by national initiatives alone, or even scattered international activities, but requires a cohesive international programme that includes collaborative training and research opportunities to prepare scientists and physicians.3
Training in the management of infectious diseases encompasses many specialties, including adult infectious diseases, clinical/medical microbiology, virology, paediatric infectious diseases, HIV medicine, public health, interventional epidemiology, infection control, tropical medicine, vaccinology, travel medicine, and genitourinary medicine. These specialties undoubtedly overlap, and many training schemes include exposure to the “subsidiary specialties” to varying degrees. The above list is not all inclusive, and there is considerable overlap with other branches of medicine and surgery.
This paper seeks to set the ball rolling and begin to establish a knowledge base of training programmes within the infectious disease specialties. Features of programmes that already exist will be described, and changes that are taking place in training in different countries will be examined. Although we focus on postgraduate training programmes for medically qualified individuals, we acknowledge the vast contribution from non-medical experts in terms of personal experience and training—eg, nurses and paramedical personnel, basic scientists, microbiology laboratory workers, infection control practitioners, pharmacists, and epidemiologists. The short-term training courses that focus on more specific topics will be discussed. Our overall aim is to promote international understanding between different infectious disease specialists (panel 1 ). Furthermore, training directors could learn from the different models of programmes already established or being developed in other countries. Increased international appreciation may present new opportunities to develop productive exchange programmes, joint research programmes, supportive links, shared learning objectives, pooled web-based learning programmes, mutual recognition of training, skill sharing, and surveillance networks. To begin to disseminate information about training opportunities available, two of the authors (FJC, AHH) researched and directed the compilation of the UK manual Training in infection, which is currently being developed as a website (http://www.trainingininfection.org.uk) in collaboration with Imperial College, London, the National Electronic Library of Infection, City University, London, and the British Infection Society. This resource is currently directed at all trainees within the infectious disease specialties in the UK, but there is potential for international expansion.
Panel 1. Aims of this review.
Investigate the international picture of postgraduate medical training in the infectious disease specialties.
Review content of current training programmes.
Compare organisational aspects of training programmes.
Provide a platform for future research in this area.
Promote international understanding between different infectious disease specialists.
Methods
The objective was to collect information from a range of countries. Most information was obtained from a semi-structured questionnaire (panel 2 ) sent electronically to individuals identified as key senior figures within the infectious disease community in their country. The questionnaire asked whether infectious diseases was a recognised specialty and if there was a specialist postgraduate training scheme. If so, details of the training were requested (length of scheme, entry requirements, syllabus, governing body responsible, supervision of the trainee, formal examinations/mode of assessment). Information on the number of infectious disease specialists in each country was difficult to collect and is not presented here. All questionnaire respondents were also encouraged to express their personal opinions on aspects of training, in free text.
Panel 2. Semi-structured questionnaire.
-
1
Is infectious diseases a recognised specialty?
-
2
Does it require specialist postgraduate training?
-
3
If so, which governing body is responsible?
-
4
What is the length of a typical training scheme?
-
5
How does supervision of the trainee take place?
-
6
What are the entry requirements?
-
7
Is there a syllabus?
-
8
Is there a formal examination or mode of assessment?
-
9
Which specialties/areas are covered in the training programme—eg, public health, HIV?
-
10
How many infectious disease specialists/consultants are there in your country?
We expected that the senior figures selected to receive the questionnaire would present the consensus attitude towards training programmes. Respondents included those on the editorial board of international journals such as The Lancet Infectious Diseases, presidents of infectious diseases societies, country representatives listed on the WHO website, and individuals identified through medical school and ministry of health websites. If the individual contacted felt it inappropriate for them to complete the questionnaire, they were requested to forward the questionnaire to someone more closely involved in training. Information collated from the survey was tabulated, edited for uniformity, and returned to the original respondents for verification.
Results
The respondents
Representatives in 50 countries were contacted, and 33 completed questionnaires were received (response rate 66%; table 1 ). There was a high bias in both countries contacted and respondents from Europe and the developed world.
Table 1.
Contacted and responding countries
| Region | Number of countries contacted | Countries contacted | Number of respondents |
|---|---|---|---|
| Europe | 29 | Austria, Belgium, Croatia, Czech Republic, Denmark, Finland, France, Germany, Greece, Hungary, Ireland, Israel, Italy, Luxembourg, Macedonia, Netherlands, Norway, Poland, Portugal, Romania, Russia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey, UK, Ukraine | 23 |
| North and Central America | 4 | USA, Canada, Mexico, Cuba | 2 |
| South America | 4 | Brazil, Argentina, Chile, Peru | 0 |
| Asia | 8 | India, Hong Kong, Taiwan, Japan, China, Singapore, Malaysia, Saudi Arabia | 5 |
| Africa | 4 | South Africa, Malawi, Kenya, Ghana | 2 |
| Australasia | 1 | Australia | 1 |
| Total | 50 | 33 |
The responses
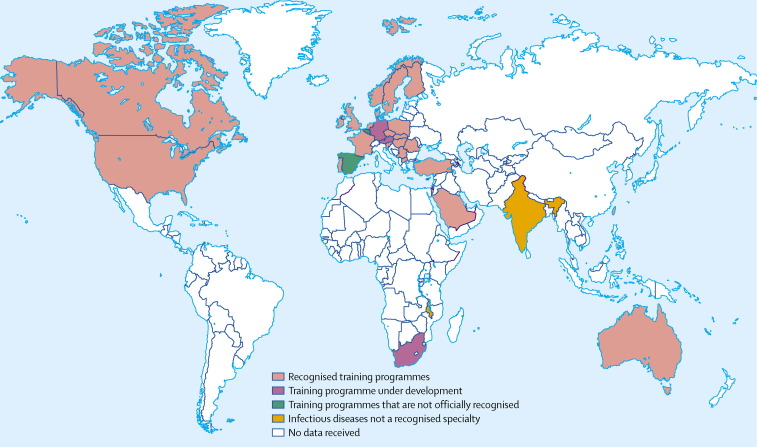
At the time of completion of the questionnaires (early 2004), 26 of 33 countries had an established training programme (79%; figure , table 2 ). Three countries (South Africa, Austria, and Germany) were in the process of introducing training programmes (table 3 ). However, towards the end of 2004 the sub-specialty of infectious diseases was accepted in South Africa, and recognised by the Health Professionals Council of South Africa. Specific training for new infectious disease specialists in South Africa was expected to commence as soon as the Minister of Health had ratified the specialty. Two countries—Belgium and Spain—provided specialist training but without official national recognition (table 4 ). Malawi and India had no specialist training programme in infectious diseases (table 5 ).
Figure.
World map showing countries with an established training programme, those with no training programme, and those with a programme under development
Table 2.
Established infectious diseases training programmes that are nationally recognised
| Country | Training duration (years) | Entry requirements | Supervision process | Exit examination | Authority for approval of course |
|---|---|---|---|---|---|
| Australia | 3 | 3 years basic training and passed Part I examination of Royal Australasian College of Physicians | By suitably qualified supervisor trained in infectious diseases. Process involves formal meetings and written reports | No | The Specialist Accreditation Committee of Australia, under the auspices of the Royal Australasian College of Physicians |
| Canada | 2 | Minimum 3 years paediatric or internal medicine training | By university faculty members trained in infectious diseases | Yes | The Royal College of Physicians and Surgeons of Canada |
| Czech Republic | 3 | Postgraduate training in internal or paediatric medicine | By the Institute of Postgraduate Education | Yes | The Ministry of Health |
| Denmark | 5 | 2·5 years training post graduation (at least 1·5 years internal medicine). | By a senior specialist | No | The National Board of Health |
| Finland | 6 | MD degree, although in practice many candidates have been trained in general internal medicine or have done scientific research | By a senior lecturer | Yes | The medical faculty of the university (total of five medical faculties in Finland) |
| France | 1–2 years fellowship programme | 4–5 years residency in specified subjects | Practical, theoretical, and some optional internships, plus report writing and assessments | Specific degree (Diplôme d'Etudes Spécialisées Complémentaires de Pathologie Infectieuse et Tropicale) | The French Infectious Diseases Society (inter-regional co-ordinator) |
| Hong Kong | 4 years for dual training in infectious diseases and general internal medicine; 3 years for single training in infectious diseases | Postgraduate training in internal medicine | By senior specialists and programme directors of the Hong Kong College of Physicians | Yes | The Hong Kong College of Physicians |
| Hungary | 5 | MD degree and specific entry examination | By a senior specialist | Yes | Dean of medical faculty |
| Ireland | 4–6 | At least 2 years postgraduate training in general medicine and MRCP or equivalent | By the head of department and a local committee | Not for infectious diseases. Microbiology/virology trainees must pass MRCPath examination | Irish Committee on Higher Medical Training |
| Israel | 2 | Training in internal medicine, paediatrics, or family medicine | By the head of department and hospital board nominated by the Israeli Medical Association | Yes | The Israeli Medical Association and the Infectious Diseases Society of Israel |
| Macedonia | 4 | State medical licence examination | By a senior consultant | Yes | The university department of infectious diseases and medical faculty |
| Netherlands | 2 | Licence in internal medicine, or in final 2 years of internal medicine specialty training | By infectious diseases senior staff | No | Licence must be approved by the head of the training programme |
| Norway | 2 | Medical qualification | No formal supervision, but the department must qualify as a training department | No (but there is an examination in tropical diseases) | The Norwegian Medical Association |
| Poland | 5 | Medical residency and entrance exam held at recognised training centre | By an appointed senior specialist | Yes | Special accreditation committee |
| Portugal | 5 | 2 years postgraduate training and entrance examination | By a senior consultant | Yes | State hospitals |
| Romania | 5 | Entrance examination | By the head of department | Yes | The Institute for the Training of Medical Doctors and Pharmacists |
| Saudi Arabia | Currently 2 years—to be increased to 3 years | Training in internal medicine or paediatrics | By an experienced infectious diseases physician and microbiologist | Yes (also examination after 1 year) | Saudi Council for Health Specialities |
| Singapore | 3 | 3 years postregistration training in general internal medicine, and medical qualification such as MRCP (UK) | By a senior specialist from a public institution | Yes | Specialist Training Committee (Infectious Diseases) under the Singapore Medical Council |
| Slovakia | 3 | Board certified in internal medicine or paediatrics | By a senior infectious diseases specialist | Yes | Slovak Medical University |
| Slovenia | 6 | Entrance examination | By a local specialist | Yes | Medical Chamber of Slovenia |
| Sweden | 5 | Medical qualification, plus internship in internal medicine, surgery, psychiatry, and general practice | By a senior specialist at a certified training centre | No (examination under development) | The state |
| Switzerland | 3 | 3 years training in internal medicine or paediatrics | By a senior specialist | Yes | The Swiss Association of Physicians |
| Taiwan | 2 | Minimum 3 years training in internal medicine or paediatrics | The Infectious Diseases Society of Taiwan, Republic of China and local infectious diseases/microbiology specialists | Yes | The Infectious Diseases Society of Taiwan, Republic of China |
| Turkey | 5 years for integrated infectious diseases and clinical microbiology | Foreign language examination and medical specialisation examination | By professors at the university hospitals or chiefs at the training hospitals of the Ministry of Health | Yes | Ministry of Health and university medical faculties, under the Council of Higher Education |
| UK | 5 years for joint infectious diseases and general internal medicine; 6 years if tropical medicine included; 6 years training for combined infectious diseases, microbiology, or virology; 5 years for microbiology | Minimum 2 years training in general medicine or paediatrics post registration. Passed MRCP examination | By nominees of postgraduate deans | Assessment in penultimate year highlights deficiencies needing attention during the final training period. Microbiology/virology trainees must pass the MRCPath examination | Joint Committee for Higher Medical Training, through the Royal College of Physicians |
| USA | 2 | Completion of residency in internal medicine | The responsibility of the programme director | Sub-specialty board examination given by the American Board of Internal Medicine | American Board of Internal Medicine/accreditation committee on graduate medical education |
MRCP=Membership of the Royal College of Physicians; MRCPath=Membership of the Royal College of Pathologists
Table 3.
Infectious diseases training programmes under development
| Country | Details |
|---|---|
| Austria | The Austrian Society for Infectious Diseases has applied to the Austrian Chamber of Physicians and the Ministry of Health for infectious diseases to be accepted as a recognised specialty. The current entry requirement is completion of training in internal medicine or microbiology, and there is an exit examination. |
| Germany | A training programme is under development (as a sub-specialty of internal medicine), and still requires official national recognition. The current entry requirement is for full training in internal medicine (minimum 3 years). The supervision process requires qualification as a specialist in internal medicine, certified by the German Society for Infectious Diseases. At the end of the course, individuals sit an exit examination, which is approved by the Committee for Training and Education of the German Society for Infectious Diseases. |
| South Africa | When the questionnaire was completed, infectious diseases was about to be recognised as a sub-specialty. Since then, L Blumberg of the Infectious Diseases Society of South Africa informed us that it was recognised by the Health Professions Council of South Africa in the latter half of 2004. The programme is likely to consist of 2 years of specialisation after training as a general physician, paediatrician, or microbiologist. Microbiologists will require 3 years of clinical training. The exit examination will be likely to operate through the College of Medicine of South Africa and overall supervision will be by the university medical schools. Authority for approval of the course will be by the Health Professions Council of South Africa. |
Table 4.
Infectious diseases training programmes that are not officially recognised
| Country | Details |
|---|---|
| Belgium | The infectious diseases course is not recognised by the government and the infectious diseases training is not formally standardised. |
| There is currently no recognised status for clinical microbiology. | |
| Spain | Infectious diseases is not an officially recognised specialty in Spain. Microbiology and parasitology focuses on laboratory work and these specialists do not take care of patients. |
| Despite this there are many infectious diseases practitioners in Spain, who are usually general physicians who have not taken part in an official residency programme or equivalent (unless this was overseas). | |
| There are also a few official infectious disease services in Spain. |
Table 5.
Countries where infectious diseases is not a recognised specialty
| Country | Details |
|---|---|
| Malawi | The training in internal medicine consists of a Masters of Medicine degree that was introduced recently. Infectious diseases is an important component of internal medicine in Malawi, which is reflected in teaching time in the pregraduate and postgraduate curriculum. Further specialties including infectious diseases may be developed in the future. |
| India | Infectious diseases is not recognised as a specialty by the Indian Medical Council. |
Established, recognised training programmes
Entry requirements, format and duration of training, the supervision process, exit examinations, and accreditation procedures varied between countries. Training duration ranged from 1 year to 6 years (plus optional time for research). The duration also varied within countries, depending on the individual's experience and desire for a formal period of research. Some respondents totalled the number of years post-registration, thus including general periods of training in medicine or paediatrics, before entry into an infectious diseases programme. In most countries, the trainee's actual experience is likely to differ from place to place, depending on local expertise, resources, and opportunity. For example, the trainee may work at a single institute throughout, or rotate between centres for different aspects of their programme
Entry requirements also varied. Most specified a period of general training, usually expecting a postgraduate qualification equivalent to membership of one of the UK royal colleges. In Sweden, an internship in internal medicine, surgery, general practice, and psychiatry is required.4 A 6-month period in general practice is required in Norway.5 Hungary and Slovenia mentioned a specific entrance examination. In Finland, a period of scientific research is necessary before entry into a training programme, and Turkey stipulated that all candidates should pass a foreign language examination.
Most countries have a formal system for supervision of trainees. Some respondents provided details as to whether this includes written work, clinical assessment, or project work. In general, direct supervisors are senior consultants in the local units, often overseen by a national body. In Norway, there is no named supervisor, but the training department must be nationally accredited. Two countries specifically involve a national society in the supervision process—in Taiwan, the Infectious Diseases Society of Taiwan is involved in supervision, along with local specialists, and this society also approves and accredits the trainee at the end of their training. The Israeli Medical Association nominates training supervisors and, along with the Infectious Diseases Society of Israel, is responsible for approval and accreditation of the trainee. 19 of 23 countries surveyed have exit examinations, and four have continuous assessment without exit examinations (table 2). No country that had once introduced an infectious diseases training scheme appears to have abandoned it or incorporated it into other specialties.
Discussion
To our knowledge, this paper is the first international investigation of training in the infectious disease specialties. There are publications that discuss specific national issues about training, which may apply elsewhere—eg, joint training in microbiology and infectious diseases in the UK6 and postgraduate training in tropical and travel medicine in Australasia.7 There have been collections of articles or themed supplements on international topics, such as the issues published by Clinical Microbiology and Infection in August 2000 and April 20058, 9 discussing the challenges in clinical microbiology and infectious disease training in Europe. No global reviews on postgraduate training in other specialties were identified. Again there were opinion papers and anecdotal pieces,10 and national/European articles, but no truly international papers. The issues we discuss may indeed apply to other specialties.
Development of infectious diseases
Historically the specialty of infectious diseases has developed differently in different countries. In some places the specialty has assumed a strong and structured clinical base, being largely teaching hospital centred, whereas elsewhere it has not particularly developed as an independent specialty. This difference may be partly due to the false perception in the 1960s that infectious diseases had been controlled, and partly because in some countries infectious diseases are so common they form the bulk of general medicine. Where specific postgraduate training programmes exist, there is considerable variation in training opportunities. Currently, little is known about the overall picture and the international skill mix in infectious diseases—eg, in some countries microbiologists have a presence on the hospital wards and advise on specific patient management issues, whereas elsewhere they are solely laboratory based. Knowledge of national training programmes and an understanding of international training resources are vital in the management of current and emerging diseases and will undoubtedly contribute to the growth of effective networks and collaborations.
European initiatives
Since 1975, basic and specialist medical qualifications have been recognised within different countries of Europe. The consolidated European Community Directive 93/16—known as the “Doctors Directive”—aims “to facilitate the free movement of doctors and the mutual recognition of their diplomas, certificates and other evidence of formal qualification”. To facilitate the movement of clinicians between countries, there have been efforts to standardise training programmes within Europe. In 1958, the European Union of Medical Specialists (UEMS; http://www.uems.net) was established to “harmonise and improve the quality of medical specialist practice in the European Union”. The UEMS aims to provide a training framework so countries can compare training programmes, and to help countries establish new written training programmes and log books. In most European countries, the training content is similar to that of the UEMS. Initially, not enough national authorities recognised infectious diseases as a specialty for it to be a separate “section”. Despite a growing recognition that infectious diseases still present considerable challenges, it was not until the mid-1990s that enough national authorities recognised infectious diseases as a specialty to apply for a new section. Approval was granted in 1996, and in the following year a section for infectious diseases was established as a sub-section within general internal medicine (http://www.uemsinfect.org). The Board for Infectious Diseases was established in 1998, and in 1999 the section approved a European training programme at the annual meeting in Geneva. The board proposed that there should be a 2 year minimum common trunk of general internal medicine and a 4-year minimum of specialty training. Microbiology is not yet an independent section but a subsection within the UEMS specialist section for medical biopathology.11
USA
In the USA, infectious diseases is a popular residency programme, although there have been discussions about reducing the numbers of fellows in training.12 In most institutes, there is a core clinical curriculum and three training tracks: clinician track, clinical investigator track, and basic investigator track. There may also be an option to “short track” into a medical sub-specialty, including infectious diseases. Residents who only wish to pursue basic science research can complete a 2-year residency training in internal medicine, and then short track into infectious diseases. This pathway requires 4 years of infectious diseases training (1 clinical year, 3 research years, incorporating 3 years of clinics).
Infectious diseases training in the USA is accredited through the Accreditation Committee on Graduate Medical Education (ACGME; http://www.acgme.org). ACGME provides detailed, rigorous standards for infectious diseases training that all programmes must comply with. Each infectious diseases training programme has a specific programme director, who must spend 50% of their time in the educational programme of the fellowship, and must be certified by both infectious disease and general internal medicine boards. There are strict policy guidelines on supervision by all infectious diseases faculty members at each training base, and on clinical and research career development activities for all faculty members involved in fellowship training. Each infectious diseases fellow must complete 2 years of clinics, at least 1 year of clinical training, and 1 year of research; however, most fellows do at least 3 years of research. Fellows must receive specific training in infection control, HIV/AIDS, microbiology (including laboratory work), sexually transmitted diseases, care of immunocompromised patients, and other subjects listed in the guidelines. However, there is still room for improvement—eg, a survey of infectious disease fellows who had recently graduated found that only half thought that training in infection control was adequate.13
The tradition in the USA was for hospital microbiology laboratories to be led by scientists rather than clinicians. Thus a completely different pattern emerged, and infectious diseases became the larger and stronger specialty, firmly entrenched in general hospitals.14 Over recent years, this situation has started to change, as clinically trained microbiologists, some of whom are also trained in public health and outbreak investigation, are heading for laboratories. According to Daniel Shapiro, director of microbiology at the Lahey Clinic, Massachusetts, USA, “the training of microbiology laboratory directors takes place in formalised post-doctoral fellowship programmes in clinical microbiology for both PhDs and MDs. Unfortunately there are not many of these programmes”.
The changing picture of training
Our survey showed that almost 80% of countries had an established training programme that was nationally recognised (table 2). Some countries reported recent changes in their training programmes—eg, standardisation of the adult and paediatric infectious disease programmes in Saudi Arabia has taken place over the past 2 years. Training duration is being increased from 2 years to 3 years, with an optional research year. Infection control is a young, rapidly growing specialty in Saudi Arabia, and an infrastructure to encourage growth of this important discipline is fast being established.15
Training programmes are in the process of being introduced in three countries (table 3). In South Africa, infectious diseases was recognised as a sub-specialty in September 2003 by the Health Professions Council, and the training programme is now being defined. In Germany, infectious diseases was recognised as a sub-specialty in 2003 and the proposed training programme is currently being recognised and adopted by the official national body. Ulf B Goebel (Charité-Universitätsmedizin, Berlin, Germany) says that the programme is a “hot and controversial topic. There is ongoing debate about who should actually participate and what a curriculum should look like”. As elsewhere, there are several disciplines involved—general internal medicine, paediatrics, clinical microbiology, hospital hygiene/epidemiology—and each specialty has particular interests. Goebel, a clinical microbiologist, is convinced that microbiology and hospital hygiene should be an integral part of infectious diseases training and practice.
Training in the absence of recognised programmes
Although Belgium and Spain provide specialist training programmes, these are not recognised at a national level. In Belgium, neither infectious diseases nor clinical microbiology are recognised as separate specialties, and microbiology is often studied within laboratory medicine. J Van Eldere, professor of microbiology at Leuven University, thinks it is advantageous that microbiology trainees become familiar with the other branches of pathology such as haematology and clinical chemistry. However, he feels this practice may result in too much emphasis on the laboratory side and not enough on medical aspects. Van Eldere suggests that “the situation may be improved by recognising medical microbiology as a specific competence with a defined core curriculum, and striving to achieve a careful balance between the development of laboratory and clinical skills, through sufficient contact with infectious disease clinics”.
Two countries, Malawi and India, have no specialist training programme in infectious diseases (table 5). These countries are both developing countries, where training in general internal medicine involves wide exposure to infectious diseases. However, like other countries, medical politics and the protection of practice may dissuade the formation of new programmes. In India, T Jacob John, former professor and head of the department of virology at the Christian Medical College in Vellore says that “all my career, physicians resisted such a sub-specialisation, partly due to apathy, partly due to fear of loss of business, and most importantly because of lack of understanding of the issues involved”.
Research within training programmes
A discrete period of research within training programmes was specifically stated by some questionnaire respondents. However, within each country, research opportunities vary between local areas, depending on expertise and priorities. Different specialties also place different weight on whether an individual has undertaken a formal period of research, and this practice may have important implications for an individual's career progression. For example, until recently the postgraduate examination for microbiologists in the UK (Membership of the Royal College of Pathologists) required submission of a research project or dissertation. However, the impression is that more infectious disease trainees undertake research for a higher degree, compared with microbiology trainees, as this practice is favoured for career progression in infectious diseases. Funding may come from specific junior and senior research training fellowships, administered by charities, governmental, and research organisations that enable some trainees to pursue clinical or laboratory-based research.
Joint training in infectious diseases and microbiology
Integration of microbiology and infectious diseases training is a key issue in many countries. Thomas Lai, consultant physician and head of infectious diseases at the Princess Margaret Hospital in Hong Kong, and chairman of the subcommittee in infectious diseases at the Hong Kong College of Physicians, thinks that “the knowledge base of many infectious disease trainees in microbiology is only very rudimentary, and their experience in laboratory technique is grossly deficient”. The only period of training is a mandatory 3-month full-time attachment to microbiology. In Hong Kong there is currently no combined training programme in infectious diseases and microbiology, although the Hong Kong Colleges of Physicians and Pathologists are exploring a joint programme for the future. Lai proposes that at present, trainees should attend combined rounds of infectious disease physicians and microbiologists to learn the view of both groups. He suggests that exposure must be wide, and include general infectious diseases, infections of immunocompromised hosts, transplant recipients, critical care patients, HIV/AIDS, sexually transmitted infections, travel medicine, antibiotic policy, and epidemiology.
Shapiro summarises how many people feel about the situation: “The practice of clinical infectious diseases is dependent not only upon the intelligent use of the data acquired from the microbiology laboratory, but also knowledge of the limitations of both the quality and accuracy of those data. Unfortunately many infectious disease fellows do not have a defined rotation in clinical microbiology in which to acquire a knowledge base in this area.”
In the UK, a joint training programme in infectious diseases and microbiology was established in the late 1990s,6, 16 but disappointingly only about ten schemes have been approved so far. Jon S Friedland (professor of infectious diseases at the Hammersmith Hospital, Imperial College, London, and chair of the education and training committee at the Royal Society of Tropical Medicine and Hygiene) feels this lack of programmes is mainly due to “conservatism within the profession”. Certainly the length of the training scheme—particularly with an additional 2–3 years research for a higher degree—may be off-putting to some. It remains to be seen what career paths will be taken or positions created for these individuals. One disadvantage is that joint infectious diseases/microbiology training excludes general internal medicine, which many infectious disease physicians regard as essential for infectious diseases practice. A report from the UK Academy of Medical Sciences—Academic bacteriology in the 21st century 17—emphasised the importance of joint training in microbiology and infectious diseases. Many agree that it is no longer tenable to justify these two disciplines as separate specialties, since both are dependent on each other and should therefore be integrated.18 This report named joint specialty training as one of its key areas for action, and emphasised the need to keep training requirements as flexible as possible.19
Other potential joint training programmes
Respondents to our questionnaire suggested exploring the following disciplines as future joint training schemes, in combination with infectious diseases or microbiology: public health, genitourinary/HIV medicine, clinical epidemiology, hospital epidemiology, travel medicine, and clinical pharmacology.
Public health and epidemiology
A recurring theme in our questionnaire responses was increasing training in the public health aspect of infectious diseases. For example, the threat of antimicrobial resistance demonstrates the importance of integrating clinical and public-health microbiology.19 Another example is emergency responsiveness and disaster management, which requires individuals trained in public health and management of clinical infectious diseases. No questionnaire respondents identified emergency responsiveness and disaster management as a component of a recognised training programme, although relief agencies (such as Médecins sans Frontières) run short courses and it may be included in Masters of public health programmes.
In Singapore, Wong Sin-Yew says that there is no formal public-health module in the infectious diseases training programme but he hopes that this will change. There is currently one infectious disease physician who is also qualified in public health and another trainee who is planning to proceed to the Masters of public health course. The aim is that these doubly qualified individuals will not only address the many public-health issues within infectious diseases, but also revise the training programme so infectious disease physicians can be more involved in public-health policy. In India, according to Jacob John, “public health is not understood by the medical system, by and large”. J van der Meer (professor of medicine and head of the internal medicine training programme at Radboud University, Nijmegen Medical Centre, and one of the directors of the national infectious diseases training programme in the Netherlands), also feels that training in the public health aspect of infectious diseases, epidemiology, and outbreak management could be improved.
Excellent interventional epidemiology training is provided by the Epidemic Intelligence Service (EIS) of the Centers for Diseases Control and Prevention (CDC; http://www.cdc.gov/eis) in the USA and the European Programme for Intervention Epidemiology Training (EPIET; http://www.epiet.org) in Europe. However, such opportunities are not integrated into most training schemes.
Many respondents highlighted the lack of training in hospital epidemiology and infection control. Although these disciplines are not formally included in many training programmes, there are supplementary short courses available as an option—eg, courses organised by the Society for Healthcare Epidemiology of America and the CDC (http://www.shea-online.org/about/shea_courses.cfm). Some national programmes are actively expanding this area within their training curriculum.
Setting up infectious disease departments and clinical teams
The UK House of Lords' Select Committee on Science and Technology's fourth report—Fighting infection—in 2003 recommended that the UK Government create a number of “infection centres”.20 This recommendation arose from concerns about the lack of critical mass and the need for academic leadership and interdisciplinary collaboration. The report proposed that infection centres would develop collaborative working, create a critical mass of expertise, and provide a setting for high-quality research and training. The UK Academy of Medical Sciences also recommended establishing a small number of “centres of excellence in microbiology and infection”, with multidisciplinary teams comprising basic research and clinical bacteriology working with cell biologists, immunologists, epidemiologists, and infectious disease clinicians.19 At a local level this practice may improve working relations between clinicians, laboratory-based staff, and public health. Julius Weinberg, specialist advisor to the House of Lords' Select Committee on Science and Technology subcommittee which conducted the inquiry resulting in the Fighting infection report points out that “there is plenty for microbiologists, virologists, infectious disease physicians, infection control nurses, environmental health officers, and epidemiologists to do, but as much energy seems to be expended on protecting areas of professional expertise and influence as on developing multidisciplinary teams essential for a modern infection service”.19 Goebel agrees that “infectious disease specialists should form a team together with clinical microbiologists, hospital hygienists, and clinical pharmacologists, the latter not being discussed at all!” It is likely to be more difficult to establish such departments or networks in smaller hospitals, although equally important.
The umbrella term “infection” clearly has a broad remit, and individuals may choose to be general infection specialists, or to focus on specific aspects, according to experience and local service demands. Daily practice often depends on whether the infectious disease physician has admitting rights, whether they provide consultation services for patients under the care of other teams (including those on intensive care units), whether they have outpatient clinics for patients with recurrent or chronic infections (eg, chronic hepatitis B and C), and whether they give advice to general practitioners or others in the community, including pre-travel advice.21 Nick Beeching, president of the British Infection Society and consultant at the tropical and infectious diseases unit, Royal Liverpool University Hospital, reiterates that it is vital to ensure that breaking down the barriers between the individual groups does not result in dilution of the specific skills associated with each area.
Short-term training in specific diseases
In addition to long-term postgraduate specialty training, there are many highly acclaimed short training courses with excellent international reputations and influence. One example is the International Centre of Diarrhoeal Diseases in Dhaka, Bangladesh (http://www.icddrb.org), which provides realistic training courses for students from the developing world. The centre's strength has been attributed to mixing clinical training and direct patient care with research, and it can rapidly respond to disasters—eg, the identification of the causative agent in the diarrhoeal epidemic in Goma, Zaire, in 1994 as Shigella spp.22
The Research Institute of Tuberculosis in Japan (http://www.jata.or.jp/eindex.htm) first established an international training programme in 1963. By providing short courses for physicians and laboratory staff, international networks are developed for information exchange, support, and collaborative research.3 Since the start, almost 2000 people from over 80 countries have participated. The institute works in collaboration with the WHO, the International Union Against Tuberculosis and Lung Disease, and the Japan International Cooperation Agency for the global fight against tuberculosis, and has projects in many developing countries such as the Philippines, Nepal, Yemen, and Cambodia.
An international network of trained experts is essential to develop and sustain these short programmes. The long-term effectiveness of training, especially in the developing world, hinges on it being realistic, in terms of facilities available at the trainee's base. The internet has facilitated collaborative research activities and post-training information exchange, and provides a perfect platform to share training resources, such as distance-learning materials on the emerging infections network for public-health professionals in the Asia Pacific region (http://depts.washington.edu/einet).23
Limitations
Due to different interpretation of the term “infectious diseases”, many respondents assumed the questionnaire was only about clinical infectious diseases training and not the other infectious disease specialties. The questions were intended to be open ended and broad, but many individuals contacted who called themselves microbiologists then forwarded the questionnaire to their infectious disease colleagues. Although we tried to identify appropriate individuals who were involved in postgraduate training, this could not be guaranteed. Difficulties with comparing answers between countries arose—eg, with length of training, some respondents included years of general medical training.
Although it was relatively easy to contact experts in Europe, USA, Canada, and Australia, it was a challenge to contact experts from countries in Asia, Africa, and South and Central America. Only English language papers were identified in the literature, thus potentially missing papers about local training programmes in national journals—eg, in South America. This report has focused on developed countries, but increasingly the development of training and medical infrastructure in developing countries will have a key role in translating scientific advances into operational reality.24 However, the information obtained gives a useful indication of the global situation and the data and interesting ideas that have been voiced are worthy of discussion.
Conclusion
This investigation of current training programmes may act as a catalyst for further discussion and reflection at national, regional, and international level. Although we are not advocating a “mould” into which all infectious disease trainees should be shaped, there is a need for a regionally adapted, common core syllabus, with more focused training for individuals. In our opinion, the core components of a training scheme should include a defined programme of supervised work and attachments, selected entry and exit requirements, national recognition by a professional body and objective external assessment (panel 3 ). The common training thread should be widely understood by international colleagues to enable productive collaborations and research. Furthermore, it would facilitate the rapid integration of refugee and overseas doctors working elsewhere. Our investigation has identified key areas for further exploration (panel 4 ). These areas include increased exposure to microbiology within infectious diseases training programmes, and greater experience in public health and infection prevention and control within all training programmes. The further development of joint infectious diseases and microbiology training schemes is welcomed, and new dual training programmes—eg, combined public health and infectious disease training—should be explored. To provide effective training, centres of infection should have a combined skill and expertise mix. Educational networks, particularly web-based distance learning, will become increasingly important and may further the development of surveillance networks and research collaborations. We welcome a comprehensive international study that includes trainees as well as training directors to explore these areas in greater depth and to optimise postgraduate training in infectious diseases around the world.
Panel 3. Proposed components of a training programme.
Core syllabus, with additional training addressing local and national needs.
Defined programme of supervised work and attachments.
Selected entry and exit requirements.
National recognition by a professional body.
Objective external assessment.
Panel 4. Summary opinion.
Combined infectious diseases and microbiology training is regarded as optimal.
Some infectious diseases training programmes are not considered to have enough microbiology experience.
There is a need for combined public health/epidemiology and infectious diseases.
Centres of infection need to have a combined skill and expertise mix to provide effective training.
Infection prevention and control must be a substantial part of training.
Networks of education, particularly web-based distance learning, will become increasingly important and may further the development of networks of surveillance and research.
Search strategy and selection criteria
Published articles on training in infectious diseases were identified through PubMed searches and personal knowledge of the literature. Additional details were obtained through web-based searches of infectious disease societies, international meetings, training institutions and individual hospitals and universities, often suggested by the questionnaire respondents.
Acknowledgments
Acknowledgments
We thank everyone who has contributed by providing information or comments for this article. In particular we acknowledge the following individuals: H Pichler, president of Austrian Society of Infectious Diseases; G Kronborg, head of the Danish Society of Infectious Diseases and Department of Infectious Diseases, University of Copenhagen, Denmark; T S T Lai, chairman of the subcommittee in infectious diseases of the Hong Kong College of Physicians and head of infectious diseases, Princess Margaret Hospital, Hong Kong; F Rozgonyi, Semmelweis University, Budapest, Hungary; K Grozdanovski, Macedonian Infectious Diseases Society and Clinic for Infectious Diseases, Skopje, Macedonia; B J Kullberg, professor of medicine and infectious diseases and head of the Infectious Diseases Training Program, Nijmegen University Centre for Infectious Diseases, Netherlands; J W M van der Meer, professor of medicine and head of the Internal Medicine Training Program, Radboud University Nijmegen Medical Centre, Netherlands; W Halot, president of the Polish Society of Infectious Diseases, Poland; C Bergen, St James's Hospital, Dublin, Ireland; P Murphy, Adelaide Meath and National Children's Hospital, Dublin, Ireland; Z Memish, head of infectious diseases and executive director, Infection Prevention and Control, King Fahad National Guard Hospital, Riyadh, Saudi Arabia; Wong Sin-Yew, chairperson of the Chapter of Infectious Diseases Physicians, College of Physicians, Singapore; V Krcmery, professor and dean, OUSA, Bratislava, Slovakia; I Nilsson-Ehle, Department of Infectious Diseases, Lund University Hospital, Sweden; M Täuber, Institute for Infectious Diseases, University of Bern, Switzerland; P R Hsueh, National Taiwan University College of Medicine, Taiwan; H Eraksoy, professor of infectious diseases and clinical microbiology, president of the Turkish Society of Clinical Microbiology and Infectious Diseases, Turkey; M McKendrick, president of the Section of Infectious Diseases at the European Union of Medical Specialities, Sheffield, UK; N Beeching, president of the British Infection Society, Liverpool, UK; J Friedland, professor of infectious diseases at the Hammersmith Hospital and Chair of the Education and Training Committee at the Royal Society of Tropical Medicine and Hygiene, London, UK; D Shapiro, director of microbiology, Lahey Clinic, Massachusetts, USA; Henry Sacks, Division of Infectious Diseases, Mount Sinai School of Medicine, New York, USA; U Gobel, Charité–Universitätsmedizin, Berlin, Germany; F Jacobs, head of Infectious Diseases Clinic, Erasme University Hospital, Brussels, Belgium; J Van Eldere, professor of microbiology at Leuven University, Belgium; E E Zijlstra, head of the Department of Medicine, Chichiri, Blantyre, Malawi; Dr T Jacob John, former professor and head of the Department of Virology, Christian Medical College, Vellore, India; Lucille Blumberg, Infectious Diseases Society of South Africa; Jan Galsky, scientific secretary of the Czech Society of Infectious Diseases, Czech Republic; V Valtonen, chief of infectious diseases, Helsinki University Central Hospital, Finland; M Gubina, Institute of Microbiology and Immunology, University of Ljubljana, Slovenia; M Whitby, chairman of the Infectious Diseases Specialist Advisory Committee of the Royal Australasian College of Physicians, Australia; C Rotstein, director of the Division of Infectious Diseases, McMaster University, Ontario, Canada; E Rubinstein, Infectious Diseases Unit, Chaim Sheba Medical Centre, Israel. We also thank the individuals from Norway, Portugal, Romania, Sweden, and Spain who completed the original questionnaire.
Conflicts of interest
We declare that we have no conflicts of interest.
References
- 1.Morens DM, Folkers GK, Fauci AS. The challenge of emerging and re-emerging infectious diseases. Nature. 2004;430:242–49. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breman J, LeDuc J. International partnerships in infectious diseases research, training, and control. Emerg Infect Dis. 2001;7(suppl 3):542. doi: 10.3201/eid0707.017721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takeda Y, Mahmoud AA. Collaborative research and training programs in infectious diseases: summary of roundtable discussion. FEMS Immunol Med Microbiol. 1997;18:333–36. doi: 10.1111/j.1574-695X.1997.tb01064.x. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson-Ehle I. Clinical infection services in Sweden. Clin Microbiol Infect. 2000;6:416–18. doi: 10.1046/j.1469-0691.2000.00126.x. [DOI] [PubMed] [Google Scholar]
- 5.Solberg C. Training for the infections diseases speciality in Norway. Clin Microbiol Infect. 2000;6:428–31. doi: 10.1046/j.1469-0691.2000.00121.x. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J. Training in infectious diseases—looking to the future. Clin Microbiol Infect. 2000;6:449–52. doi: 10.1046/j.1469-0691.2000.00123.x. [DOI] [PubMed] [Google Scholar]
- 7.Leggat P. Postgraduate training in tropical and travel medicine in Australasia. Travel Medicine and Infectious Diseases. 2003;1:77–79. doi: 10.1016/S1477-8939(03)00017-6. [DOI] [PubMed] [Google Scholar]
- 8.Anon Meeting the challenges in clinical microbiology and infectious diseases. Proceedings of a workshop. April 1999, Birmingham, United Kingdom. Clin Microbiol Infect. 2000;6:401–52. [PubMed] [Google Scholar]
- 9.Anon Progress towards meeting the challenges in clinical microbiology and infectious diseases. Clin Microbiol Infect. 2005;11(suppl 1):1–51. doi: 10.1111/j.1469-0691.2005.01080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hooker J, Eccher M, Lakshminarayan K. Neurology training around the world. Lancet Neurol. 2003;2:572–79. doi: 10.1016/s1474-4422(03)00507-6. [DOI] [PubMed] [Google Scholar]
- 11.Cornaglia G. The present status of clinical microbiology in Europe. ESCMID News. 2002;3:14–18. [Google Scholar]
- 12.Joiner KA, Powderly WG, Blaser MJ. Fellowship training in infectious diseases: a report from the regional and national meetings of infectious diseases division chiefs and program directors. Clin Infect Dis. 1998;26:1060–65. doi: 10.1086/520294. [DOI] [PubMed] [Google Scholar]
- 13.Joiner KA, Dismukes WE, Britigan BE. Adequacy of fellowship training: results of a survey of recently graduated fellows. Clin Infect Dis. 2001;32:255–62. doi: 10.1086/318462. [DOI] [PubMed] [Google Scholar]
- 14.Cohen J. Whither the infection specialities? CME Bulletin Infectious Diseases and Tropical Medicine. 1998;1:12–14. [Google Scholar]
- 15.Memish Z. Infection Control in Saudi Arabia: Meeting the challenge. Am J Infect Control. 2002;30:57–65. doi: 10.1067/mic.2002.120905. [DOI] [PubMed] [Google Scholar]
- 16.Cohen J, Roberts C. A new joint training programme in infectious diseases and medical microbiology. J R Coll Physicians Lond. 2000;34:363–65. [PMC free article] [PubMed] [Google Scholar]
- 17.Academy of Medical Sciences . Academic medical bacteriology in the 21st century. Academy of Medical Sciences; London, UK: 2001. http://www.acmedsci.ac.uk/ac_bac.pdf (accessed May 20, 2005) [Google Scholar]
- 18.Banatvala JE, Roberts C, Crook D, Peto T. Infectious disease training: challenges and opportunities. Lancet Infect Dis. 2002;2:9–10. doi: 10.1016/s1473-3099(01)00167-0. [DOI] [PubMed] [Google Scholar]
- 19.Weinberg J. Fighting infection. Commun Dis Public Health. 2004;7:5–7. [PubMed] [Google Scholar]
- 20.House of Lords Select Committee on Science and Technology. 4th report: fighting infection. HMSO; London, UK: 2003. HL paper 138. [Google Scholar]
- 21.Thompson AB, Bonnington A, Beeching N. Infectious diseases and tropical medicine. BMJ. 2002;324:S193–95. [Google Scholar]
- 22.Anonymous. Public health impact of Rwandan refugee crisis: what happened in Goma, Zaire, in July, 1994? Lancet. 1994;345:339–44. [PubMed] [Google Scholar]
- 23.Kimball AM, Shih L, Brown J. International distance-learning outreach: the APEC EINet experience. Int J Med Inf. 2003;69:57–62. doi: 10.1016/s1386-5056(02)00080-1. [DOI] [PubMed] [Google Scholar]
- 24.Fauci A. Infectious diseases: considerations for the 21st century. Clin Infect Dis. 2001;32:675–85. doi: 10.1086/319235. [DOI] [PubMed] [Google Scholar]