Summary
Acute respiratory failure occurs in up to half of patients with haematological malignancies and 15% of those with solid tumours or solid organ transplantation. Mortality remains high. Factors associated with mortality include a need for invasive mechanical ventilation, organ dysfunction, older age, frailty or poor performance status, delayed intensive care unit admission, and acute respiratory failure due to an invasive fungal infection or unknown cause. In addition to appropriate antibacterial therapy, initial clinical management aims to restore oxygenation and predict the most probable cause based on variables related to the underlying disease, acute respiratory failure characteristics, and radiographic findings. The cause of acute respiratory failure must then be confirmed using the most efficient, least invasive, and safest diagnostic tests. In patients with acute respiratory failure of undetermined cause, a standardised diagnostic investigation should be done immediately at admission before deciding whether to perform more invasive diagnostic procedures or to start empirical treatments. Collaborative and multidisciplinary clinical and research networks are crucial to improve our understanding of disease pathogenesis and causation and to develop less invasive diagnostic strategies and more targeted treatment options.
Introduction
A growing number of adults have immune dysfunction.1 Up to 5% of the general population are cancer survivors,2 transplantation is on the rise,3 and immunosuppressant drugs are being used for more indications.4 Moreover, intensive treatments now improve disease-free survival,2 but also increase the risk of life-threatening events, many of which affect the lungs.5, 6, 7, 8
Acute respiratory failure can be defined as a triad of clinical signs, radiographic findings, and gas exchange alterations. Most patients present with newly developing or worsening respiratory symptoms over a period of 7 days. Severe acute respiratory failure manifests as respiratory distress with severe tachypnoea, laboured breathing, and recruitment of accessory respiratory muscles. Various patterns of pulmonary infiltrates might be seen, the most common of which are diffuse bilateral infiltrates.9 Patients with acute respiratory failure require oxygen therapy and most studies of acute respiratory failure included patients receiving ≥6 L/min of standard oxygen. However, depending on the country and number of available hospital beds, patients with acute respiratory failure can be managed on wards, in intermediate care units, or in intensive care units (ICUs). Overall, the need for ICU admission, need for invasive mechanical ventilation (IMV), or mortality increase with the required oxygen flow.10 Thus, for patients that require 6 L/min of standard oxygen or more, need for intubation throughout the ICU stay and mortality before hospital discharge are up to 40%.9, 10, 11, 12, 13, 14, 15, 16 Delayed ICU admission has been associated with increased mortality.13, 14, 17
Immunocompromised patients with acute respiratory failure can be encountered by all clinicians in their daily practice. In this Review, we look at the epidemiology, outcomes, and diagnostic investigations in immunocompromised patients with acute respiratory failure, with emphasis on the broad range of causes that must be considered. We discuss the role for invasive and non-invasive tests in identification of the cause of acute respiratory failure, although the huge diversity of tests available for each cause, coupled with the scarcity of randomised controlled trials, creates major challenges. We also suggest an approach to the management of hypoxaemia based on the latest literature.
Epidemiology
The incidence of respiratory events varies across different groups of immunocompromised patients (table 1 ). Few studies have followed cohorts of patients with the main objective of collecting information about the incidence of pulmonary infiltrates or respiratory complications. Observational studies have shown that among haematological malignancies, lymphoproliferative disorders (acute lymphoblastic leukaemia and lymphoma) were associated with a moderate incidence of respiratory events (8–18%)18 compared with acute myeloid leukaemia and myelodysplastic syndromes (22–84%; table 1).19, 20, 38 Moreover, patients with prolonged neutropenia6 and autologous or allogeneic stem cell transplant recipients24, 25, 26, 27 have higher incidences of respiratory events compared with other haematology patients. Solid tumours are associated with a lower incidence of respiratory events than haematological malignancies, with lung cancer having the highest rates (up to 50%), because endobronchial obstruction and atelectasis are risk factors for pneumonia.30 However, in patients with breast cancer treated with radiation and paclitaxel, the crude rate of pneumonitis was 14·6% (95% CI 5·6–29·2).31 Of note, in patients with cancer receiving immunotherapy (mostly with programmed death 1 and programmed death ligand 1 inhibitors), the incidence of pneumonitis can reach 4%.32, 39 Acute respiratory failure occurs in about 5% of kidney transplant recipients and 12–14% of heart or lung transplant recipients.34, 36 Overall, mortality among patients with acute respiratory failure is about 50%, depending on the underlying condition, nature, severity, and course of the respiratory failure, need for IMV, and associated organ dysfunctions.13
Table 1.
Incidence of respiratory events in various types of immunocompromised patients
| Incidence of respiratory events | Need for ICU admission | Hospital respiratory mortality | |
|---|---|---|---|
| Haematological malignancies | |||
| Acute myeloid leukaemia5, 18, 19, 20, 21, 22, 23 | 22–84% | 66% | 45% |
| Acute lymphoblastic leukaemia18, 22, 23 | 7–18·5% | 12–15% | 38·5% |
| Lymphoproliferative diseases5 | 8% | 8% | 40-50% |
| Myelodysplastic syndrome18 | 29·4% | 20% | 17% |
| Autologous haemopoietic stem cell therapy24, 25 | 3–28% | 42% | 3–55% |
| Allogeneic haemopoietic stem cell therapy26, 27 | 24–30% | 50% | 51% |
| Prolonged neutropenia6, 28 | 8–29·5% | 11–16% | 5–12% |
| Solid tumours | |||
| Lung cancer29, 30 | 26–50% | 100% | 11·2–60% |
| Other solid tumours5, 30, 31 | 0·7–10·3% | 100% | 6·1–55% |
| Patients on immunotherapy32, 33 | 1·3–3·6% | 1·3%* | .. |
| Solid organ transplantation | |||
| Lung transplantation34 | 14% | All | 65% |
| Heart transplantation35 | 12·5% | All | 76·5% |
| Kidney transplantation36, 37 | 3·3–4·8% | All | 16·4–22·5% |
Data on patients with drug-related immunosuppression are sparse.
Refers to grade 3–4 toxicities. ICU=intensive care unit.
Key messages.
-
•
Acute respiratory failure occurs in up to 50% of haematology patients (primarily patients with acute myeloid leukaemia or allogeneic haemopoietic stem cell transplantation) and in up to 15% of patients with solid tumours (chiefly lung cancer) or solid organ transplants (chiefly of the heart or lung).
-
•
Mortality is high and is associated with invasive mechanical ventilation and organ dysfunction; older age; frailty or poor performance status; delayed intensive care unit admission; and acute respiratory failure due to an invasive fungal infection or unknown cause.
-
•
In addition to appropriate antibacterial therapy, initial management aims to restore oxygenation and predict the most probable cause on the basis of variables related to the underlying disease, the characteristics of acute respiratory failure, and the radiographic findings. The cause of acute respiratory failure must then be confirmed using the most efficient, least invasive, and safest diagnostic tests.
-
•
In patients with acute respiratory failure of undetermined cause, a standardised diagnostic investigation should be done immediately at admission before deciding whether to perform more invasive diagnostic procedures or to start empirical treatments.
-
•
Collaborative and multidisciplinary clinical and research networks are crucial both to improve our understanding of disease pathogenesis and causation and to develop less invasive diagnostic strategies and more targeted treatment options.
Factors associated with mortality
Several studies have assessed risk factors for mortality in immunocompromised patients with acute respiratory failure. These factors can be grouped into five categories: (1) factors reflecting the severity of the acute respiratory failure and associated organ dysfunctions, (2) factors related to delayed ICU admission, (3) factors related to the underlying disease and comorbid conditions, (4) factors related to the initial oxygenation and ventilation strategy, and (5) factors related to the cause of acute respiratory failure.
Hypoxaemia is the hallmark of respiratory failure. The clinical signs and tolerance of hypoxaemia are usually a function of respiratory symptom duration. For instance, an acute hypoxaemic episode can lead to respiratory distress within a few hours, whereas a subacute or non-acute lung insult of similar magnitude can result in deep hypoxaemia without signs of respiratory distress. Overall, degree of hypoxaemia reflects the extent of lung involvement. Hypoxaemia, measured directly as the PaO2 on room air or assessed on the basis of the oxygen flow needed to achieve an peripheral capillary oxygen saturation (SpO2) of 95% or the estimated or calculated ratio of partial pressure arterial oxygen and fraction of inspired oxygen (PaO2/FiO2 ratio), has been used for many years to risk-stratify patients and guide ICU admission decisions. Increased oxygen flow has been associated with the need for ICU admission,10 need for IMV,10, 16 and hospital mortality.17 Similarly, lower PaO2/FiO2 has been associated with mortality in patients with acute respiratory distress syndrome,40 the need for non-invasive ventilation (NIV),41 or failure of high-flow nasal oxygen therapy (HFNO).42 Persistent tachypnoea has also been associated with failure of standard oxygen,42 NIV,41 or high-flow nasal cannula, requiring the implementation of another strategy (eg, intubation).43 No study has evaluated the impact of hyperoxygenation in this setting.44 Associated organ dysfunctions are best depicted by the Sequential Organ Failure Assessment (SOFA) score, which has consistently been identified as a determinant of mortality, with higher scores associated with increased mortality.5, 13, 45 Delayed ICU admission has been associated with increased mortality in immunocompromised patients,14 particularly in those with acute respiratory failure.10, 13, 17 Benefits from earlier ICU admission might be the result of the careful clinical assessment, optimal oxygenation strategy, avoidance of potentially harmful investigations, and selection of the least invasive diagnostic tests in ICUs. The characteristics of the underlying immunosuppressive condition are not usually associated with hospital mortality following ICU admission,46 although variations occur depending on ICU admission policies. A higher proportion of patients admitted to ICU with do-not-resuscitate or do-not-intubate status results in stronger associations between variables reflecting characteristics of disease status and mortality.47, 48 Performance status and comorbidities have been associated with increased mortality.13, 14, 49, 50 The effects of initial oxygenation and ventilation strategy on mortality are discussed later in this Review. Furthermore, as previously mentioned, several studies have assessed the association between the cause of acute respiratory failure and mortality. Mortality is lowest in patients with cardiac pulmonary oedema and highest in those with invasive fungal infections or no identified cause of acute respiratory failure.
Early assessment of pre-test probability of acute respiratory failure cause
One of the first and key steps in the early management of immunocompromised patients with acute respiratory failure is to establish the probable cause of acute respiratory failure, at the bedside, based on clinical examination before undertaking tests. No standard combination therapy is suitable for all patients with acute respiratory failure; each patient must be considered individually. Clinicians should make every effort to identify the cause of acute respiratory failure in patients at high risk of intubation and mortality (eg, those with a higher SOFA score or more hypoxaemic). Bacterial infection is the main cause of acute respiratory failure, and up to 90% of patients receive antibacterial drugs soon after admission.9 Cardiogenic pulmonary oedema must be considered in every patient. However, other diagnoses should be considered on a case-by-case basis. Thus, the basic diagnostic investigation is the same for all patients (panel 1 ). It includes tests for cardiogenic pulmonary oedema, sputum examination, and blood cultures to detect bacterial or fungal infections, induced sputum examination for Pneumocystis, viral multiplex PCR on nasopharyngeal aspirates or swabs, viral PCR on plasma or blood, an assessment of the likelihood that the underlying condition and its treatments will affect the lungs, and an analysis of the imaging data.
Panel 1. Basic diagnostic investigations to be applied to all immunocompromised patients presenting with acute respiratory failure.
Tests to diagnose or rule out cardiogenic pulmonary oedema
-
•
Echocardiography
-
•
Biomarkers such as natriuretic peptide or N-terminal pro b-type natriuretic peptide could be used in the emergency department to rule out cardiogenic pulmonary oedema for their good negative predictive value
Sputum examination to detect bacterial (and mycobacterial) infections
Blood cultures to detect bacterial or fungal infections
Urine antigen for Legionella pneumophila and Streptococcus pneumoniae
-
•
Induced sputum examination for Pneumocystis jirovecii pneumonia. Both classic staining, immunofluorescence, and PCR can be useful on induced sputa
Induced sputum is performed after inhalation (during 15–20 min) of nebulised sterile hypertonic saline solution followed by coughing and expectoration of airway secretions. In patients with severe chronic obstructive pulmonary disease or asthma, pre-treatment with inhaled salbutamol and monitoring of lung function during the procedure are needed
Viral multiplex PCR on nasopharyngeal aspirates or nasal swabs to detect respiratory viruses (adenovirus, metapneumovirus, some types of coronavirus, parainfluenza virus types 1, 2, 3, and 4, influenza virus types A and B, respiratory syncytial virus A and B, rhinovirus A, B, and C, bocavirus, and enterovirus). This test also detects L pneumophila, Mycoplasma pneumoniae, and Chlamydia pneumoniae
Viral PCR on plasma or blood to detect herpesviruses (including cytomegalovirus).
Other PCR tests: although the results of most PCR methods lack specificity for the detection of Aspergillus sp, PCR allows early detection of other fungi (eg, Mucorales) or parasites (eg, Toxoplasma gondii)
Biomarkers
-
•
Procalcitonin has limited predicitive value in immunocompromised patients
-
•
Serum Aspergillus galactomannan is useful for the detection of both invasive aspergillosis and histoplasmosis
-
•
Serum 1,3 β-D-glucan for all fungal infections except mucormycosis
Echography-guided pleurocentesis (check platelet count and haemostasis)
Biopsy or puncture of extra-pulmonary involvement (skin, joints, peripheral lymph nodes, sternal puncture, buccal smear, etc)
Imaging data, including chest X-ray, lung and pleural echography, and high-resolution CT scan (without first-line contrast media unless there is a clinical suspicion of pulmonary vascular disease)
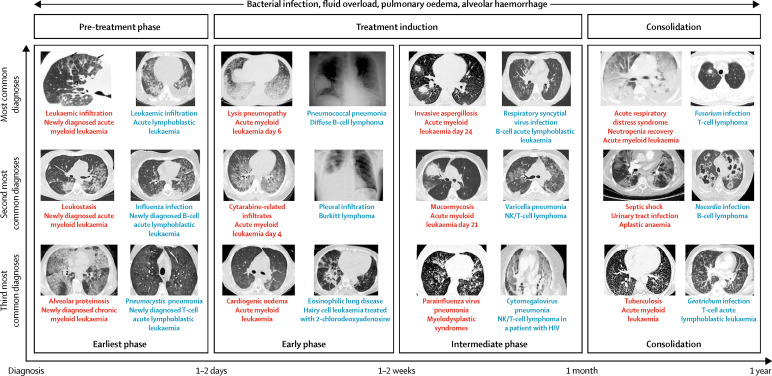
When performing the first clinical examination, the mnemonic DIRECT can be used to assess the cause of acute respiratory failure at the bedside.51, 52 D refers to respiratory symptom duration in days, I to the type of immunosuppression, R to the chest X-ray pattern, E to the clinician's experience of similar cases, C to the clinical findings, and T to high-resolution CT. In patients with myeloproliferative diseases such as acute myeloid leukaemia, myelodysplastic syndrome, or chronic myeloid leukaemia, most cases of acute respiratory failure that occur early after disease onset are related to leukaemic infiltrates (figure 1 ), although some patients might present with pneumonia or cardiogenic pulmonary oedema.20, 53, 54 Acute respiratory failure of infectious origin is, however, more common at the earliest phase of lymphoproliferative disorders (figure 1), such as acute lymphoblastic leukaemia or lymphoma.21, 55 In patients with T-cell proliferations, opportunistic infections have been reported before cancer treatment initiation, exemplifying the role played by disease-related immunosuppression.56 Later, during follow-up, infection is the main cause (figure 1), although treatment-related toxicities and disease relapse can also lead to acute respiratory failure. Clinicians can struggle with non-infectious causes whose diagnosis is believed to rely solely on biopsies, which are difficult to obtain in hypoxaemic patients with thrombocytopenia and haemostatic disorders, or on bronchoscopy and bronchoalveolar lavage, and have been reported as possibly deteriorating the respiratory status and increasing IMV needs. However, a multidisciplinary and collaborative approach allows earlier recognition of typical patterns of clinical and laboratory findings, for which no additional diagnostic procedures are needed (lung infiltration by the underlying condition, leukaemic infiltrates in patients with acute myeloid leukaemia, diffuse alveolar haemorrhage, cytarabine-related pulmonary toxicity, immunotherapy-related pneumonitis, etc). Patients with these patterns are often considered to have no known cause of acute respiratory failure until a multidisciplinary team makes the appropriate diagnosis. Similarly, conditions such as neutropenia or allogeneic haemopoietic stem cell transplantation are associated with both a high risk of respiratory events and specific acute respiratory failure causes such as exacerbation of previous lung injury during neutropenia recovery,57 or non-infectious interstitial lung diseases following haemopoietic stem cell transplantation.26, 58
Figure 1.
Causes of acute respiratory failure by time since diagnosis of haematological malignancy
CT scans with red text refer to myeloid malignancies and those with blue text to lymphoid malignancies. The x-axis indicates time since diagnosis of the malignancy. For each scenario, the three most common diagnoses (in decreasing order) are reported at each timepoint and for each condition.
Acute respiratory failure in the first few days after solid organ transplantation is probably related to either a surgical complication or to decompensation of a chronic respiratory or cardiac comorbid condition.34, 36, 59, 60 Invasive candidiasis might occur quite early after transplantation.37 However, most opportunistic infections are reported more than 3 months after transplantation and depend heavily on adherence to prophylactic regimens by the patient.35, 37, 61, 62, 63, 64, 65, 66 Of note, with the use of intensive immunosuppression in patients experiencing acute humoral or interstitial rejection67 and with the use of immunosuppressant drug combinations to ensure graft tolerance, clinicians must carefully assess the individual risk for each possible cause and perform a complete diagnostic investigation.68
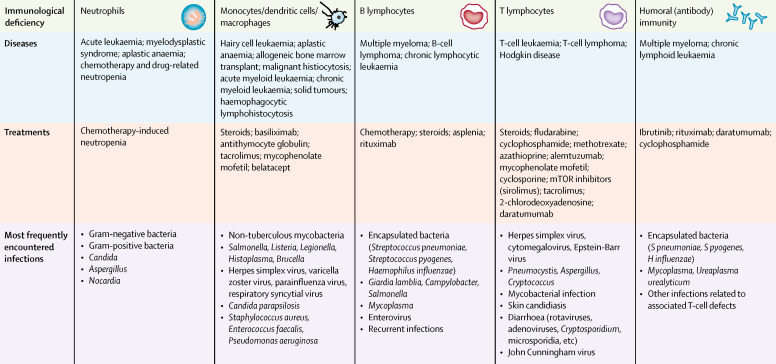
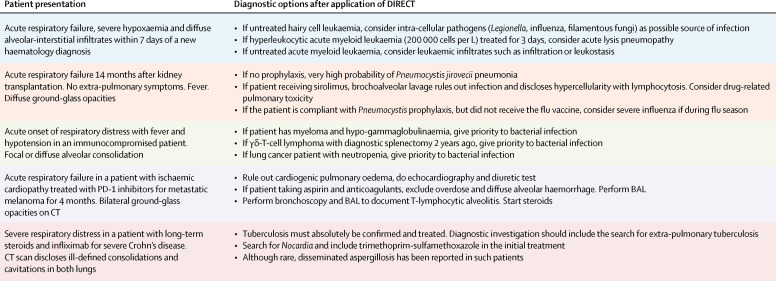
In each individual case, the type of immune deficiency must be assessed to allow appropriate adjustment of the initial anti-infectious treatment (figure 2 ) and to avoid treatment delays. Imaging studies, particularly high-resolution CT, are another important bedside tool for determining the cause of acute respiratory failure.69 This Review does not detail the radiological findings in immunocompromised patients with acute respiratory failure. Patterns of lung involvement are an important piece of the puzzle but are not predictive of a specific cause.69 However, a combination of positive and negative high-resolution CT findings suggest specific causes of lung infiltrates.70 Different components of the DIRECT mnemonic contribute to determining the pre-test clinical probability for each individual diagnosis (figure 3 ). A given clinical situation can be related to different causes of acute respiratory failure, because contextual elements and clinical findings vary across patients. However, the administration of antifungal drugs or anti-Pneumocystis therapy should not be delayed if the pre-test probability of the disease is substantial.
Figure 2.
Risk for specific pathogens according to the type of haematological malignancy or treatment
This figure illustrates the most frequently encountered types of infection according to the main disease-related or treatment-related immunological deficiency. It focuses mainly on secondary immunosuppression in adults, as data for primary immune deficiencies are scarce.
Figure 3.
Five clinical vignettes for which the application of the DIRECT mnemonic leads to different diagnostic probabilities
Diagnoses such as bacterial infection, pulmonary oedema, and alveolar haemorrhage need to ruled out or treated in every case. BAL=bronchoalveolar lavage.
Avoiding situations in which the acute respiratory failure cause remains undetermined
Non-invasive diagnostic tests offer an alternative to bronchoscopy and bronchoalveolar lavage, which carry a risk of respiratory deterioration requiring IMV.51 However, bronchoalveolar lavage might be required when non-invasive respiratory samples are either not feasible or of poor quality. Performing bronchoalveolar lavage with the support of NIV or high-flow nasal cannula can help patients tolerate the procedure. Also, first-line bronchoalveolar lavage must be considered in situations in which patients have a possible diagnosis of diffuse alveolar haemorrhage, Pneumocystis jirovecii pneumonia, or drug-related pulmonary toxicity, or when lung infiltrates might be involved in the underlying disease (vasculitis, lymphoma, etc). The diagnostic yield of non-invasive tests has, however, increased since the introduction of more sensitive diagnostic tests, such as PCR. However, these tests are more sensitive than specific, and the clinical relevance of a positive PCR is sometimes uncertain. In patients with cancer, the standard diagnostic investigation done immediately at ICU admission includes a physical examination, a pre-test probability assessment using DIRECT, sputum (if possible) and induced sputum examinations, nasopharyngeal aspirates or swabs, blood cultures, serum and urine antigen assays, imaging studies, and biomarker assays. These non-invasive tests perform as well as bronchoscopy and bronchoalveolar lavage.9, 71 In solid organ transplant recipients, however, bronchoalveolar lavage has a higher diagnostic yield,36 although the risk–benefit ratio has not been assessed in this population. Moreover, with the advent of omics to assist in the diagnosis of infections,72 as well as sophisticated immunology and molecular biology methods and advances in imaging techniques to establish the diagnosis of non-infectious conditions, a reappraisal of the diagnostic yield of non-invasive tests in immunocompromised patients is warranted.
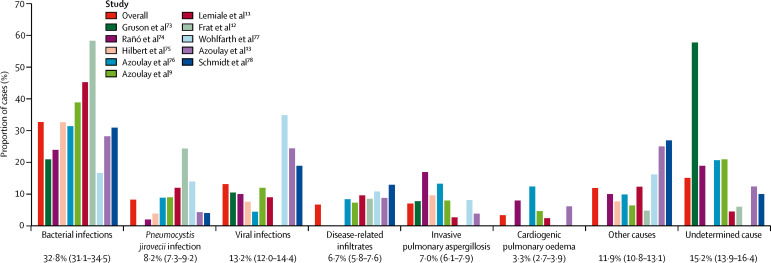
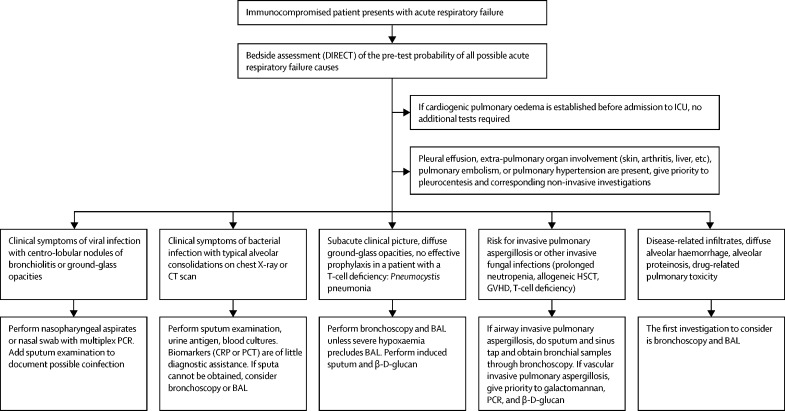
Nevertheless, despite an optimal early diagnostic investigation, the cause remains undetermined in 10–15% of patients with acute respiratory failure (figure 4 ; table 2 ). Failure to identify the cause of acute respiratory failure was independently associated with mortality in several studies.5, 13, 76, 84 In some patients, the cause of acute respiratory failure is identified late, and the impact of a late diagnoses and correspondingly late treatment has not been assessed. The association between absence of a documented cause and mortality raises several questions (table 3 ). The association might be related in part to patients who die within a few hours with intractable hypoxaemia and multiple organ dysfunction before diagnostic tests can be performed. When providing expert opinion, careful attention should be directed to the clinical situation, underlying disease, comorbid conditions, and ongoing long-term treatments, as well as to the response to treatments given for the current acute respiratory failure episode. Figure 5 shows first-line diagnostic strategy according to clinical and radiographic presentation. The expert will also have the (sometimes difficult) task of determining which tests are actually performed, obtaining their exact results (as opposed to a classification as positive or negative), and potentially obtaining results that might not yet have been made available to the bedside physicians.
Figure 4.
Causes of pulmonary infiltrates in immunocompromised patients with acute respiratory failure
Mean percentage is reported in the first column in red for each cause, with 95% confidence intervals reported underneath. The study by Gruson and colleagues73 included only bone marrow transplant recipients and the studies by Wohlfarth and colleagues77 and Schmidt and colleagues78 included only patients with severe acute respiratory distress syndrome treated with extra-corporeal membrane oxygenation.
Table 2.
Studies reporting intubation and mortality in immunocompromised patients receiving standard oxygen, non-invasive ventilation, or high-flow nasal oxygen therapy
| N | Cause of immunosuppression |
Intubated (%) |
Mortality (%) |
Underwent bronchoalveolar lavage (%) | Undetermined cause (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | O2 | NIV | HFNO | All | O2 | NIV | HFNO | |||||
| Antonelli et al79* | 40 | Solid organ transplants | 33·7 | 70 | 20 | .. | 35 | 50 | 20 | .. | 27·5 | 0 |
| Hilbert et al75* | 52 | All types | 61·5 | 66 | 46·1 | .. | 53·8 | 80·8 | 50 | .. | 32·7 | .. |
| Azoulay et al9 | 203 | Oncology and haematology patients | 85·0 | .. | 57 | .. | 56 | 9 | 48·1 | .. | 72 | 20·7 |
| Lemiale et al16 | 380 | Haematology patients | 24·7 | 20 | 32 | .. | 32 | 26 | 44 | .. | .. | 24·7 |
| Lemiale et al80* | 374 | All types | 41·4 | 45 | 38·2 | .. | 25·7 | 34·4 | 30·9 | .. | 38 | 4·5 |
| Mokart et al81 | 178 | Oncology and haematology patients | 48·0 | 50 | 45·9 | 75 | 46 | 55 | 56 | 25 | .. | 25 |
| Frat et al12†‡ | 82 | All types | 46·3 | 43 | 65 | 31 | 29·3 | 27 | 46 | 15 | 4·9 | |
| Coudroy et al82 | 115 | All types | 44·0 | .. | 55 | 35 | 30 | .. | 40 | 20 | .. | .. |
| Lemiale et al11† | 353 | All types | 40·2 | 38 | .. | 45 | 22·6 | 20·7 | .. | 25·9 | 38·2 | 4·5 |
| Azoulay et al13 | 1611 | All types | 40·9 | 41 | 41 | 41 | 36·5 | 32·7 | 36·9 | 38·4 | 60 | 12·9 |
| Tu et al83 | 38 | Solid organ transplants | 34·2 | .. | 50 | 20 | 22·7 | .. | 22·2 | 5 | .. | .. |
| Total | 3426 | .. | 45·0 | 47 | 45 | 41 | 35 | 37 | 40 | 21 | 45 | 12 |
Only studies published in English from Jan 1, 1998, to April 30, 2018, were taken into account. Studies that comprised only postoperative patients and studies on palliative NIV were not included. NIV=non-invasive ventilation. HFNO=high-flow nasal oxygen therapy.
Randomised controlled trials.
Post-hoc analysis of randomised controlled trials.
Indicates day-90 mortality; all other studies reported hospital mortality.
Table 3.
Hypothetical examples of causes of increased mortality when the cause of acute respiratory failure is not identified
| Unidentified, unsuspected, and untreated condition | Unidentified, suspected, but suboptimally treated condition | Undocumented coinfection in which one pathogen remains untreated | Infectious and non-infectious condition, of which one is unidentified or untreated | Identified aetiology mistakenly considered as irrelevant finding | |
|---|---|---|---|---|---|
| Actual underlying cause | Pneumonitis while taking checkpoint inhibitors | Lung infiltration by lymphoma | Tuberculosis in a kidney transplant recipient | Pneumocystis pneumonia in a patient with lung cancer | Invasive aspergillosis |
| Incorrectly presumed cause | Positive nasal swab (rhinovirus) in a patient treated for melanoma; no clinical sign of viral infection | Patient treated for bacterial infection based on high plasma C-reactive protein and procalcitonin | The only positive result is a positive PCR for cytomegalovirus (2 logs) | Patient receiving steroids for radiation pneumonitis without prophylaxis | Patient believed to have an undetermined acute respiratory failure cause |
| Procedure that should have been performed | CT scan suggested hypersensitivity pneumonia; bronchoalveolar lavage cell analysis was not performed | CT-guided lung biopsy (the diagnosis of lymphoma was made based on node and bone marrow biopsies) | CT findings suggested tuberculosis with 3 apical cavitated nodules in the right upper lobe | As hypoxaemia worsened and ground-glass opacities extended, bronchoalveolar lavage should have been considered | Galactomannan at 0·50 and sputum positive for Aspergillus fumigatus, both considered irrelevant |
| Missed treatment | Steroids; drug withdrawal | Chemotherapy | Antituberculosis drugs | Trimethoprim and sulfamethoxazole | Antifungal agents |
Figure 5.
First-line diagnostic strategy according to clinical and radiographic presentation
ICU=intensive care unit. HSCT=haemopoietic stem cell therapy. GVHD=graft versus host disease. CRP=C-reactive protein. PCT=procalcitonin. BAL=bronchoalveolar lavage.
We are aware that lung biopsy is often not feasible, due to haemodynamic instability, deep hypoxaemia, or thrombocytopenia or other severe haemostatic abnormalities. Data on surgical lung biopsies in this setting are, therefore, scarce (table 4 ). Nevertheless, valuable information can be gleaned from studies reporting surgical lung biopsy or autopsy data in immunocompromised patients with acute respiratory failure of unknown cause. Overall, lung biopsy had a diagnostic yield above 60%, with complications in 10% of patients, despite careful patient selection for the procedure. Lung biopsy had a lower diagnostic yield in patients receiving IMV. Invasive fungal infections and malignant or potentially steroid-sensitive lung infiltrates were the most common causes of acute respiratory failure (table 4). The diagnostic yield of surgical lung biopsy for unexplained pulmonary infiltrates was assessed in a retrospective study of 62 haematology patients.95 The exact diagnosis was established in 67% of patients, with invasive aspergillosis and malignancy being the main causes. The biopsy result prompted a treatment change in 40% of patients, and complications occurred in 11% of patients. The diagnostic yield was lower in patients with acute respiratory failure who were receiving IMV at the time of biopsy than in non-intubated patients. In a cohort of 63 haematology patients, the diagnostic yield of lung biopsy was 62% and the therapeutic yield 57%.73 The diagnostic yield was lower in patients on IMV and in those with neutropenia, but was higher in patients with focal infiltrates. Invasive aspergillosis was also a common biopsy finding in this study. Complications occurred in 13% of patients.73 The 15% prevalence of invasive aspergillosis is in line with data on acute respiratory distress syndrome in patients with cancer40 and with autopsy findings in patients with acute respiratory distress syndrome.90 In 21 haematology patients, including 10 in whom the lung biopsies were obtained post-mortem, inflammatory and malignant infiltrates were the most common diagnoses.85 A retrospective autopsy study of 7 haemopoietic stem cell transplant recipients showed that fungal infections, potentially steroid-responsive lung involvement, and malignant infiltrates were underdiagnosed.96 Complications associated with lung biopsies occurred in about 10% of patients who were highly selected based on platelet count, performance status, and goals of care. Given the lower diagnostic yield of lung biopsy in ICU patients, the risk–benefit ratio is not favourable; therefore, lung biopsy is rarely performed in critically ill immunocompromised patients with acute respiratory failure and lung infiltrates of unknown cause. However, minimally invasive CT-guided lung biopsies and transbronchial cryobiopsies are increasingly done.88, 89, 92, 93, 97, 98 Studies to assess the timing of these minimally invasive diagnostic techniques in this setting are warranted. The diagnostic yield should be better defined as the identification of a new diagnosis that was not detected by any other less invasive technique and that resulted in a change in treatment. Moreover, the risk–benefit ratio needs to be re-assessed. If these minimally invasive biopsy techniques are evaluated in a randomised controlled trial, control patients should receive empirical treatment for the most common lung biopsy diagnoses, namely, invasive fungal infection or steroid-responsive lung disease (panel 2 ).
Table 4.
Studies reporting the results of surgical or post-mortem lung biopsies
|
Lung biopsy |
Invasive fungal infections | Mycobacterial infections | Need for steroids or chemotherapy | Comments | ||
|---|---|---|---|---|---|---|
| Surgical | Post-mortem | |||||
| White et al (2000)85 | 63 | 0 | 8 (13%) | 6 (9·5%) | 47 (75%) | Complication rate 13%; lower diagnostic yield in neutropenic patients and patients on IMV; higher diagnostic yield if focal infiltrates |
| Gossot et al (2001)86 | 21* | 0 | 0 | 0 | 8 of 29 (26%) | 0 of 9 biopsies of residual mass in patients with lymphoma |
| Dai et al (2001)87 | 7 | 0 | 1 (14%) | 0 | 3 (43%) | .. |
| Kim et al (2002)88 | 31 | 0 | 17 (55%) | 1 | 12 (39%) | All patients underwent lung biopsy for suspected invasive pulmonary aspergillosis |
| Sharma et al (2005)89 | 71 | 0 | 12 (17%) | 14 (20%) | 19 (27%) | All were adult bone marrow transplant recipients (39 allogeneic) |
| Zihlif et al (2005)90 | 62 | 0 | 14 (23%) | 0 | 31 (50%) | Complication rate 11%; lower diagnostic yield in patients on IMV |
| Gupta et al (2010)91 | 213 | 0 | 32 (15%) | 13 (6%) | 85 (40%) | Large or cavitary lesions or lung masses were more likely to yield a specific diagnosis |
| Sharma et al (2013)92 | 34† | 0 | 15 (44%) | NA | NA | .. |
| Gay et al (2013)93 | 11 | 10 | 0 | 5 (24%) | 5 (24%) | Only haematology patients |
| Uhlving et al (2015)94 | 44 | 13 (29·5%) | NA | 4 (9%) | Allogeneic bone marrow transplant recipients with biopsy-verified bronchiolitis obliterans | |
IMV=invasive mechanical ventilation. NA=not applicable.
8 CT-guided biopsies.
All CT-guided.
Panel 2. Unresolved issues and future directions in acute respiratory failure in patients with solid or haematological malignancies, solid organ transplant recipients, and patients taking immunosuppressive drugs.
Update data on the prevalence of pulmonary involvement in immunocompromised patients
-
•
Develop and implement multinational patient registries
-
•
Analyse the severe forms of drug-related toxicity from targeted therapy, immunotherapy, and other new drugs
-
•
Collect longer-term follow-up data to assess the true morbidity of acute respiratory failure
Define the best standard of care for immunocompromised patients with acute respiratory failure
-
•
Monitor times to intensive care unit (ICU) admission, to treatment implementation, and to diagnosis
-
•
Manage respiratory failure and associated organ dysfunctions according to the latest guidelines
-
•
Find a balance between aggressive and non-beneficial care, and implement full-code intensive care in patients with a substantial hope of survival
Educate all stakeholders to avoid delays in ICU management
-
•
Provide information on outcomes according to oxygen needs
-
•
Explain how delayed ICU admission leads to increased mortality
-
•
Encourage clinicians to assess the pre-test probability of each acute respiratory failure cause and start the corresponding treatments early
Develop a minimal early diagnostic investigation that applies to all patients, combined with targeted diagnostic strategies for patients at risk for specific diseases
-
•
Search for bacterial and fungal infections (sputum examination, blood cultures), viral infection (multiplex PCR on nasopharyngeal aspirates or swabs), and cardiogenic pulmonary oedema; evaluate the extent to which the underlying condition and its treatments may affect the lungs; obtain imaging data in all patients
-
•
Apply specific clinical algorithms and perform targeted non-invasive or minimally invasive diagnostic tests in patients at risk for specific diseases (Pneumocystis pneumonia, invasive aspergillosis, mycobacterial disease, etc)
-
•
Identify situations in which more invasive tests may be required
Evaluate omics technologies on non-invasive samples
-
•
Apply genomics, metagenomics, proteomics, metabolomics, and transcriptomics on samples that can be collected easily from patients with tachypnoea and hypoxaemia
-
•
Use clinical algorithms and evaluate their ability to confirm the diagnosis in high-risk patients or to rule out the diagnosis in low-risk patients
-
•
Assess whether the use of these technologies can result in improved clinical outcomes
Provide convincing data regarding the superiority of non-invasive ventilation or high-flow nasal oxygen therapy
-
•
When standard oxygen alone alleviates respiratory distress and maintains SpO2 ≥95%; or when standard oxygen fails to achieve these clinical goals
-
•
Clarify whether patients who are intubated after failed non-invasive ventilation or high-flow nasal oxygen therapy would have had better outcomes if they had received earlier intubation and lung-protective ventilation
-
•
Define consensual intubation criteria, as the need for invasive mechanical ventilation is an important outcome measure
Develop a multinational network to improve the management of immunocompromised patients with acute respiratory failure
-
•
To define a non-invasive diagnostic and therapeutic strategy that is readily feasible at many locations and to demonstrate, using cohort studies and randomised controlled trials, how this strategy translates into improved outcomes
-
•
To validate clinical algorithms that help identify patients at low vs high risk for a given disease
-
•
To develop and implement multicentre basic and translational research
-
•
To promote education, update guidelines, and establish patient-centred outcome measures
Oxygenation and ventilation strategies
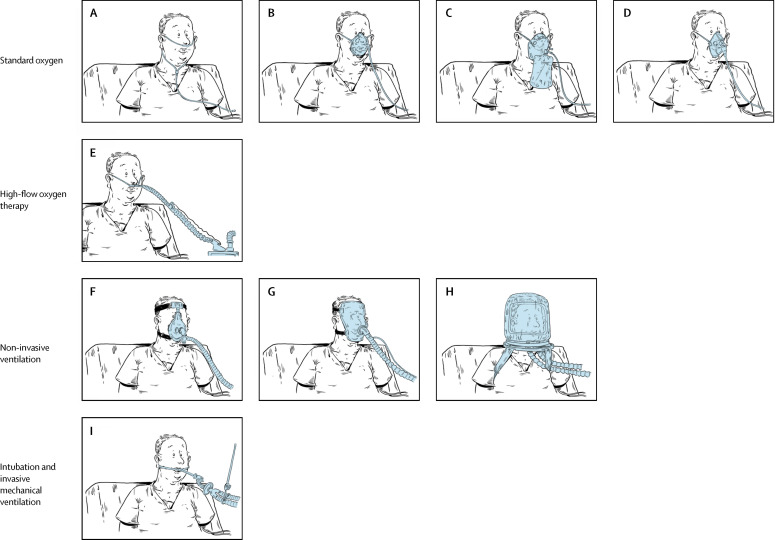
The initial oxygenation and ventilation strategy aims to restore safe oxygenation, reduce the respiratory rate, alleviate the dyspnoea and respiratory distress, and improve patient comfort.99 Over the past two decades, studies have consistently shown higher mortality in immunocompromised patients who required IMV. Priority has, therefore, been given to avoidance of IMV by use of non-invasive oxygenation or ventilation devices (figure 6 ). However, failure of NIV13, 41, 100 or HFNO13 was associated with higher mortality,13 and two older studies even suggested that early IMV was associated with improved survival.101, 102 Furthermore, because respiratory disease severity or associated organ dysfunctions are usually worse in intubated patients, determining whether the excess mortality in patients on IMV is due to the IMV itself or to the greater severity of the acute illness is difficult. In other words, a focus on avoiding intubation might not be effective, because the need for IMV might identify a group of patients with high disease severity.
Figure 6.
Nine oxygenation and ventilation methods
Standard oxygen can be administered through a wide array of devices. Low-flow oxygen systems comprise a nasal cannula (or nasal catheters; A) providing supplemental oxygen at flows below the total minute ventilation, leading to oxygen dilution with ambient air and lowering the inspired oxygen concentration. A standard nasal cannula delivers an inspiratory FiO2 of 0·24–0·44 at supply flows 1–8 L/min, depending on respiratory rate and tidal volume. A humidification device is recommended for flows >4 L/min. Reservoir masks (B) can deliver FiO2 values of 0·40–0·60 at 5–10 L/min. The reservoir system (∼100–300 cm3) stores oxygen. A flow rate >5 L/min must be set to ensure the washout of exhaled gas and avoid CO2 retention. The non-rebreathing facemask (C) may deliver up to 0·90 FiO2 at flow settings >10 L/min. It should be used only for short periods, as humidification is difficult and there is also a risk of CO2 retention if the mask's reservoir bag is allowed to collapse on inspiration. Lastly, the Venturi system (D) mixes oxygen with room air (humidification is not necessary) and provides an accurate and constant FiO2 despite variations in respiratory rate and tidal volume. It is employed when concern arises about CO2 retention or when the respiratory drive is inconsistent. High-flow oxygen therapy through nasal prongs or cannulas (high-flow nasal oxygen therapy; E) supplies an exact FiO2 (up to 1) at a flow equal to or greater than the patient's inspiratory flow demand. Nasal oxygen is administered at a flow rate of up to 60 L/min. It is warmed to body temperature and saturated to full humidity by molecular humidification. Non-invasive positive-pressure ventilation provides ventilator support without an endotracheal tube, using an oronasal (F) or total face (G) mask or a helmet (H). The main non-invasive ventilation mode used in hypoxaemic acute respiratory failure is pressure support; continuous positive airway pressure and bi-level positive airway pressure are used less often. Finally, invasive mechanical ventilation (I) uses a tracheal tube inserted into the trachea under general anaesthesia and a neuromuscular-blocking drug. The tube is then secured to the face or neck and connected to a ventilator. In patients with hypoxaemic acute respiratory failure, intubation and invasive mechanical ventilation are used after failure of standard oxygen and, in some cases, of the aforementioned non-invasive options. FiO2= fraction of inspired oxygen.
Overall, five initial oxygenation methods are available for patients with hypoxaemic acute respiratory failure (figure 6). Guidelines from the European Respiratory Society and American Thoracic Society advocate the use of NIV.101 This recommendation is based mainly on a 2001 single-centre trial in 52 patients,75 in which mortality was 81% in the group assigned to standard oxygen, the highest ever reported in this setting (table 2). Another seminal trial in solid organ transplant recipients103 also documented NIV benefits, but these results were obtained within 3 weeks following surgery. The European Respiratory Society and American Thoracic Society guidelines have been challenged by recent findings. A multicentre, randomised controlled trial in 374 patients in 28 centres in France and Belgium compared NIV with oxygen.11 This trial showed neither benefits nor harms from NIV, in sharp contrast with a post-hoc analysis of the trial by Frat and colleagues,12 which compared outcomes in 82 immunocompromised patients treated with HFNO, NIV, or standard oxygen. In this trial, the IMV and mortality rates were higher in the NIV group compared with the HFNO and standard oxygen groups. These results are consistent with studies reporting an increased risk of failure and mortality in patients receiving NIV for severe acute respiratory distress syndrome.41, 75, 79 Thus, these data raise concerns about the use of NIV in immunocompromised patients with hypoxaemic acute respiratory failure.
When first introduced, HFNO seemed a promising alternative to NIV. HFNO is easy to use and delivers humidified warmed oxygen, thereby allowing high flows by improving tolerability and comfort.104 HFNO improves oxygenation, lowers the respiratory rate, inspiratory effort, and work of breathing, and reduces minute ventilation at a constant PaCO2.105 HFNO also increases end-expiratory lung volume and dynamic lung compliance.105 These physiological effects are even more pronounced when increasing flow rates are delivered.106 However, in a randomised controlled trial in 310 unselected patients with hypoxaemic acute respiratory failure and a PaO2/FiO2 ratio ≤300 mm Hg,107 the number of patients requiring intubation was not significantly reduced with HFNO compared with NIV or standard oxygen. However, the number of ventilator-free days on day 28 was significantly higher with HFNO, and the hazard ratio for day-90 mortality was lower with HFNO.
Five studies evaluated the feasibility and safety of HFNO in immunocompromised patients with acute respiratory failure. In a retrospective single-centre study of 45 patients with haematological malignancies (half were bone marrow transplant recipients,108 half had recently received systemic chemotherapy, and 42% were neutropenic), HFNO allowed recovery without intubation in one-third of the patients. The hospital mortality rate was 13·3% when HFNO was successful and 86·7% when HFNO failed. The HFNO failure rate was only 15% in a single-centre study of 183 patients with solid tumours,109 but was 80% in a study of 56 haematology patients.110 A phase 2 trial in 30 patients with advanced cancer and persistent dyspnoea compared HFNO with biphasic positive airway pressure.111 Oxygen saturation improved only with HFNO, whereas both treatments provided similar improvements in dyspnoea and respiratory rate. In 37 lung transplant recipients with acute respiratory failure, HFNO proved feasible and safe and decreased the absolute risk of intubation by 29·8%, with a number-needed-to-treat to avoid one intubation of 3.34
Although no results from trials specifically assessing HFNO in immunocompromised patients with hypoxaemic acute respiratory failure are available, six studies compared HFNO with other oxygenation or ventilation strategies in this setting (table 2). In a retrospective cohort of 178 patients with cancer and acute respiratory failure,112 76 (43%) patients received NIV plus HFNO, 74 (42%) NIV plus standard oxygen, 20 (11%) HFNO alone, and 8 (4%) standard oxygen alone. The combination of NIV and HFNO was associated with lower mortality rates (37% vs 52% in the other patients, p=0·04) and was independently associated with higher day-28 survival. In a post-hoc analysis of data from the iNVIctus randomised controlled trial of early NIV in immunocompromised patients with acute respiratory failure,11 neither the intubation rate nor day-28 mortality differed significantly between the HFNO arm and the standard oxygen arm.113 In the post-hoc analysis of the trial by Frat and colleagues,12 outcomes were compared across standard oxygen, NIV, and HFNO. Although NIV was associated with increased need for intubation and higher mortality, neither parameter differed significantly between the 30 patients assigned to standard oxygen and the 26 patients assigned to HFNO. In a retrospective study of 115 immunocompromised patients with acute respiratory failure,81 the proportion of patients that required intubation (55% vs 35%) and mortality (40% vs 20%) were higher with NIV than with HFNO. In the Efraim multicentre, multinational, prospective cohort study of 1611 immunocompromised patients,13 915 patients were not intubated on ICU admission and received standard oxygen, HFNO, NIV, or NIV plus HFNO. Hospital mortality was not affected by the initial oxygenation or ventilation management. There was a non-significant trend towards reduced intubation in patients given HFNO. In a retrospective study of 38 kidney recipients,80 the number of ventilator-free days on day 28 was significantly higher in the HFNO group than in the NIV group. The results of two trials of HFNO focusing specifically on immunocompromised adults with acute respiratory failure (NCT02739451 and NCT02978300) are expected to be available in a few months.82 HFNO has not yet been properly evaluated regarding its ability to assist diagnostic procedures such as bronchoscopy with bronchoalveolar lavage and bronchial or transbronchial biopsies.
Changes in the initial oxygenation and NIV strategy are unlikely to translate into improved survival. The response of patients to standard oxygen, HFNO, or NIV should be carefully assessed. If the initial strategy of standard oxygen, NIV, or HFNO lowers the respiratory rate and minute ventilation then it should be continued and continuously revaluated. If the tachypnoea and high respiratory drive persist, the risk of intubation is very high and it is reasonable to evaluate the potential benefits of avoiding delayed intubation and adding self-inflicted lung injury to the initial pulmonary insult.83 Early intubation has been associated with improved survival in haematology patients.101, 102 Studies of early intubation in patients with a persistently high respiratory drive despite the initial oxygenation strategy are warranted.
Conclusion
In summary, acute respiratory failure is a common and often fatal event in immunocompromised patients that raises major diagnostic and therapeutic challenges. In the near future, with the use of more intensive therapeutic regimens designed to cure cancer, induce transplant tolerance, or control autoimmune and inflammatory diseases in ever older and frailer patients, the incidence of acute respiratory failure against a background of immunodeficiency can be expected to increase. Moreover, the expanding use of targeted therapies and immunotherapies will lead to a growing burden of toxicity and infection during the increasing life spans of these populations. Our knowledge of the effects of acute respiratory failure needs to be improved by longer-term follow-up studies. Multinational registries must be developed to analyse the effect of new drugs and update clinicians on future trends in the incidence of acute respiratory failure and in the use of intensive care for patients with acute respiratory failure. Targets for improving survival, such as early ICU admission and the early identification or treatment of the cause of acute respiratory failure, require evaluation in large randomised controlled trials. Patients with substantial life expectancy and who agree to undergo ICU management should be offered unrestricted access to diagnostic and therapeutic strategies. The greatest challenges are the identification of patients at high risk for specific diagnoses, earlier treatment of acute respiratory failure causes, and selection of the least invasive diagnostic tests. The non-invasive approach is promising but still needs to be refined and updated. Combining clinical algorithms and sophisticated tests, such as genomics, metagenomics, proteomics, or transcriptomics, on non-invasive samples to document or rule out infections will be a major advance only if the results include survival benefits, shorter ICU and hospital stay lengths, reduced costs, and improved patient-reported outcomes. Given that the initial oxygenation and NIV strategy is unlikely to be associated with survival, assessing the patient's response to standard oxygen, HFNO, or NIV within 1–4 h following ICU admission might be the best approach. Patients who improve, whether quickly or slowly, can then be differentiated from those with persistent tachypnoea, high respiratory drive, and increasing oxygen needs, for whom avoiding late intubation might have lung-protective effects.
Search strategy and selection criteria
We searched Medline and PubMed for reviews and original articles on pulmonary involvement in immunocompromised adults published in English between Jan 1, 1998 and April 30, 2018, using the terms (“respiration disorders”[Mesh]) AND “immunocompromised host”[Mesh]), (“pneumonia”[Mesh]) AND (“immunocompromised host”[Mesh]), and (“respiratory insufficiency”[Mesh]) AND “immunocompromised host”[Mesh]). We also searched using individual terms such as “leukaemia”, “lymphoma”, “solid tumours”, “cancer”, “haematology”, “malignancies”, “transplantation”, “immunosuppressant drugs”, “systemic vasculitis”, “connective tissue diseases”, and “primary immunodeficiency”. Although most of the studies we retrieved were published within the specified period, we did not exclude earlier reports. Furthermore, we searched the reference lists of the articles identified by this search strategy and our own personal files. We used original reports when available. Patients with HIV infection are not in the scope of this Review.
Declaration of interests
EA reports personal fees from Gilead, Alexion, Baxter, and Astellas and a grant from MSD. AD reports personal fees from Medtronic, Philips, Resmed, Fisher & Paykel, Baxter, and Hamilton. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
We thank Olivier Lescale for the illustrations in figure 6.
Declaration of interests
EA reports personal fees from Gilead, Alexion, Baxter, and Astellas and a grant from MSD. AD reports personal fees from Medtronic, Philips, Resmed, Fisher & Paykel, Baxter, and Hamilton. All other authors declare no competing interests.
References
- 1.Harpaz R, Dahl RM, Dooling KL. Prevalence of immunosuppression among US adults, 2013. JAMA. 2016;316:2547–2548. doi: 10.1001/jama.2016.16477. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.Israni AK, Zaun D, Rosendale JD, Schaffhausen C, Snyder JJ, Kasiske BL. OPTN/SRTR 2016 annual data report: deceased organ donation. Am J Transplant. 2018;18(suppl 1):434–463. doi: 10.1111/ajt.14563. [DOI] [PubMed] [Google Scholar]
- 4.Weyand CM, Goronzy JJ. Clinical practice. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med. 2014;371:50–57. doi: 10.1056/NEJMcp1214825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azoulay E, Thiéry G, Chevret S. The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 2004;83:360–370. doi: 10.1097/01.md.0000145370.63676.fb. [DOI] [PubMed] [Google Scholar]
- 6.Orasch C, Weisser M, Mertz D. Comparison of infectious complications during induction/consolidation chemotherapy versus allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2010;45:521–526. doi: 10.1038/bmt.2009.187. [DOI] [PubMed] [Google Scholar]
- 7.Bos MMEM, Verburg IWM, Dumaij I. Intensive care admission of cancer patients: a comparative analysis. Cancer Med. 2015;4:966–976. doi: 10.1002/cam4.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee D-S, Suh GY, Ryu J-A. Effect of early intervention on long-term outcomes of critically ill cancer patients admitted to ICUs. Crit Care Med. 2015;43:1439–1448. doi: 10.1097/CCM.0000000000000989. [DOI] [PubMed] [Google Scholar]
- 9.Azoulay E, Mokart D, Lambert J. Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med. 2010;182:1038–1046. doi: 10.1164/rccm.201001-0018OC. [DOI] [PubMed] [Google Scholar]
- 10.Gruson D, Vargas F, Hilbert G. Predictive factors of intensive care unit admission in patients with haematological malignancies and pneumonia. Intensive Care Med. 2004;30:965–971. doi: 10.1007/s00134-004-2237-1. [DOI] [PubMed] [Google Scholar]
- 11.Lemiale V, Mokart D, Resche-Rigon M. Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure: a randomized clinical trial. JAMA. 2015;314:1711–1719. doi: 10.1001/jama.2015.12402. [DOI] [PubMed] [Google Scholar]
- 12.Frat J-P, Ragot S, Girault C. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med. 2016;4:646–652. doi: 10.1016/S2213-2600(16)30093-5. [DOI] [PubMed] [Google Scholar]
- 13.Azoulay E, Pickkers P, Soares M. Acute hypoxemic respiratory failure in immunocompromised patients: the Efraim multinational prospective cohort study. Intensive Care Med. 2017;43:1808–1819. doi: 10.1007/s00134-017-4947-1. [DOI] [PubMed] [Google Scholar]
- 14.Azoulay E, Mokart D, Pène F. Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol. 2013;31:2810–2818. doi: 10.1200/JCO.2012.47.2365. [DOI] [PubMed] [Google Scholar]
- 15.Lemiale V, Resche-Rigon M, Mokart D. Acute respiratory failure in patients with hematological malignancies: outcomes according to initial ventilation strategy. A groupe de recherche respiratoire en réanimation onco-hématologique (Grrr-OH) study. Ann Intensive Care. 2015;5:28. doi: 10.1186/s13613-015-0070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lemiale V, Lambert J, Canet E. Identifying cancer subjects with acute respiratory failure at high risk for intubation and mechanical ventilation. Respir Care. 2014;59:1517–1523. doi: 10.4187/respcare.02693. [DOI] [PubMed] [Google Scholar]
- 17.Mokart D, Lambert J, Schnell D. Delayed intensive care unit admission is associated with increased mortality in patients with cancer with acute respiratory failure. Leuk Lymphoma. 2013;54:1724–1729. doi: 10.3109/10428194.2012.753446. [DOI] [PubMed] [Google Scholar]
- 18.Garcia JB, Lei X, Wierda W. Pneumonia during remission induction chemotherapy in patients with acute leukemia. Ann Am Thorac Soc. 2013;10:432–440. doi: 10.1513/AnnalsATS.201304-097OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaoui D, Legrand O, Roche N. Incidence and prognostic value of respiratory events in acute leukemia. Leukemia. 2004;18:670–675. doi: 10.1038/sj.leu.2403270. [DOI] [PubMed] [Google Scholar]
- 20.Moreau A-S, Lengline E, Seguin A. Respiratory events at the earliest phase of acute myeloid leukemia. Leuk Lymphoma. 2014;55:2556–2563. doi: 10.3109/10428194.2014.887709. [DOI] [PubMed] [Google Scholar]
- 21.Azoulay E, Fieux F, Moreau D. Acute monocytic leukemia presenting as acute respiratory failure. Am J Respir Crit Care Med. 2003;167:1329–1333. doi: 10.1164/rccm.200206-554OC. [DOI] [PubMed] [Google Scholar]
- 22.Specchia G, Pastore D, Carluccio P. Pneumonia in acute leukemia patients during induction therapy: experience in a single institution. Leuk Lymphoma. 2003;44:97–101. doi: 10.1080/1042819021000040297. [DOI] [PubMed] [Google Scholar]
- 23.Rossini F, Verga M, Pioltelli P. Incidence and outcome of pneumonia in patients with acute leukemia receiving first induction therapy with anthracycline-containing regimens. Haematologica. 2000;85:1255–1260. [PubMed] [Google Scholar]
- 24.Puig N, De La Rubia J, Jarque I. Characteristics of and risk factors for pneumonia in patients with hematological malignancies developing fever after autologous blood stem cell transplantation. Leuk Lymphoma. 2007;48:2367–2374. doi: 10.1080/10428190701694178. [DOI] [PubMed] [Google Scholar]
- 25.Afessa B, Abdulai RM, Kremers WK, Hogan WJ, Litzow MR, Peters SG. Risk factors and outcome of pulmonary complications after autologous hematopoietic stem cell transplant. Chest. 2012;141:442–450. doi: 10.1378/chest.10-2889. [DOI] [PubMed] [Google Scholar]
- 26.Bergeron A, Chevret S, Peffault de Latour R. Noninfectious lung complications after allogeneic haematopoietic stem cell transplantation. Eur Respir J. 2018;51:1702617. doi: 10.1183/13993003.02617-2017. [DOI] [PubMed] [Google Scholar]
- 27.Ho VT, Weller E, Lee SJ, Alyea EP, Antin JH, Soiffer RJ. Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7:223–229. doi: 10.1053/bbmt.2001.v7.pm11349809. [DOI] [PubMed] [Google Scholar]
- 28.Meyer E, Beyersmann J, Bertz H. Risk factor analysis of blood stream infection and pneumonia in neutropenic patients after peripheral blood stem-cell transplantation. Bone Marrow Transplant. 2007;39:173–178. doi: 10.1038/sj.bmt.1705561. [DOI] [PubMed] [Google Scholar]
- 29.Rolston KVI, Nesher L. Post-obstructive pneumonia in patients with cancer: a review. Infect Dis Ther. 2018;7:29–38. doi: 10.1007/s40121-018-0185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cupp J, Culakova E, Poniewierski MS, Dale DC, Lyman GH, Crawford J. Analysis of factors associated with in-hospital mortality in lung cancer chemotherapy patients with neutropenia. Clin Lung Cancer. 2018;19:e163–e169. doi: 10.1016/j.cllc.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 31.Taghian AG, Assaad SI, Niemierko A. Risk of pneumonitis in breast cancer patients treated with radiation therapy and combination chemotherapy with paclitaxel. J Natl Cancer Inst. 2001;93:1806–1811. doi: 10.1093/jnci/93.23.1806. [DOI] [PubMed] [Google Scholar]
- 32.Khunger M, Rakshit S, Pasupuleti V. Incidence of pneumonitis with use of programmed death 1 and programmed death-ligand 1 inhibitors in non-small cell lung cancer: a systematic review and meta-analysis of trials. Chest. 2017;152:271–281. doi: 10.1016/j.chest.2017.04.177. [DOI] [PubMed] [Google Scholar]
- 33.De Velasco G, Je Y, Bossé D. Comprehensive meta-analysis of key immune-related adverse events from CTLA-4 and PD-1/PD-L1 inhibitors in cancer patients. Cancer Immunol Res. 2017;5:312–318. doi: 10.1158/2326-6066.CIR-16-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roca O, de Acilu MG, Caralt B, Sacanell J, Masclans JR. Humidified high flow nasal cannula supportive therapy improves outcomes in lung transplant recipients readmitted to the intensive care unit because of acute respiratory failure. Transplantation. 2015;99:1092–1098. doi: 10.1097/TP.0000000000000460. [DOI] [PubMed] [Google Scholar]
- 35.Komurcu O, Ozdemirkan A, Camkiran Firat A, Zeyneloglu P, Sezgin A, Pirat A. Acute respiratory failure in cardiac transplant recipients. Exp Clin Transplant. 2015;13(suppl 3):22–25. doi: 10.6002/ect.tdtd2015.O14. [DOI] [PubMed] [Google Scholar]
- 36.Canet E, Osman D, Lambert J. Acute respiratory failure in kidney transplant recipients: a multicenter study. Crit Care. 2011;15:R91. doi: 10.1186/cc10091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ulas A, Kaplan S, Zeyneloglu P, Torgay A, Pirat A, Haberal M. Acute respiratory failure in renal transplant recipients: a single intensive care unit experience. Exp Clin Transplant. 2015;13(suppl 3):44–47. doi: 10.6002/ect.tdtd2015.O37. [DOI] [PubMed] [Google Scholar]
- 38.Rabbat A, Chaoui D, Montani D. Prognosis of patients with acute myeloid leukaemia admitted to intensive care. Br J Haematol. 2005;129:350–357. doi: 10.1111/j.1365-2141.2005.05459.x. [DOI] [PubMed] [Google Scholar]
- 39.Rashdan S, Minna JD, Gerber DE. Diagnosis and management of pulmonary toxicity associated with cancer immunotherapy. Lancet Respir Med. 2018;6:472–478. doi: 10.1016/S2213-2600(18)30172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Azoulay E, Lemiale V, Mokart D. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40:1106–1114. doi: 10.1007/s00134-014-3354-0. [DOI] [PubMed] [Google Scholar]
- 41.Adda M, Coquet I, Darmon M, Thiery G, Schlemmer B, Azoulay E. Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure. Crit Care Med. 2008;36:2766–2772. doi: 10.1097/CCM.0b013e31818699f6. [DOI] [PubMed] [Google Scholar]
- 42.Frat J-P, Ragot S, Coudroy R. Predictors of intubation in patients with acute hypoxemic respiratory failure treated with a noninvasive oxygenation strategy. Crit Care Med. 2017;46:208–215. doi: 10.1097/CCM.0000000000002818. [DOI] [PubMed] [Google Scholar]
- 43.Azoulay E, Lemiale V, Mokart D. High-flow nasal oxygen vs. standard oxygen therapy in immunocompromised patients with acute respiratory failure: study protocol for a randomized controlled trial. Trials. 2018;19:157. doi: 10.1186/s13063-018-2492-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 45.Roca O, Messika J, Caralt B. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016;35:200–205. doi: 10.1016/j.jcrc.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 46.Chu DK, Kim LH-Y, Young PJ. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693–1705. doi: 10.1016/S0140-6736(18)30479-3. [DOI] [PubMed] [Google Scholar]
- 47.Gristina GR, Antonelli M, Conti G. Noninvasive versus invasive ventilation for acute respiratory failure in patients with hematologic malignancies: a 5-year multicenter observational survey. Crit Care Med. 2011;39:2232–2239. doi: 10.1097/CCM.0b013e3182227a27. [DOI] [PubMed] [Google Scholar]
- 48.Azoulay E, Pène F, Darmon M. Managing critically ill hematology patients: time to think differently. Blood Rev. 2015;29:359–367. doi: 10.1016/j.blre.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Soares M, Toffart A-C, Timsit J-F. Intensive care in patients with lung cancer: a multinational study. Ann Oncol. 2014;25:1829–1835. doi: 10.1093/annonc/mdu234. [DOI] [PubMed] [Google Scholar]
- 50.Martos-Benítez FD, Soto-García A, Gutiérrez-Noyola A. Clinical characteristics and outcomes of cancer patients requiring intensive care unit admission: a prospective study. J Cancer Res Clin Oncol. 2018;144:717–723. doi: 10.1007/s00432-018-2581-0. [DOI] [PubMed] [Google Scholar]
- 51.Puxty K, McLoone P, Quasim T, Kinsella J, Morrison D. Survival in solid cancer patients following intensive care unit admission. Intensive Care Med. 2014;40:1409–1428. doi: 10.1007/s00134-014-3471-9. [DOI] [PubMed] [Google Scholar]
- 52.Zampieri FG, Bozza FA, Moralez GM. The effects of performance status one week before hospital admission on the outcomes of critically ill patients. Intensive Care Med. 2017;43:39–47. doi: 10.1007/s00134-016-4563-5. [DOI] [PubMed] [Google Scholar]
- 53.Azoulay E, Schlemmer B. Diagnostic strategy in cancer patients with acute respiratory failure. Intensive Care Med. 2006;32:808–822. doi: 10.1007/s00134-006-0129-2. [DOI] [PubMed] [Google Scholar]
- 54.Schnell D, Mayaux J, Lambert J. Clinical assessment for identifying causes of acute respiratory failure in cancer patients. Eur Respir J. 2013;42:435–443. doi: 10.1183/09031936.00122512. [DOI] [PubMed] [Google Scholar]
- 55.Azoulay É, Canet E, Raffoux E. Dexamethasone in patients with acute lung injury from acute monocytic leukaemia. Eur Respir J. 2012;39:648–653. doi: 10.1183/09031936.00057711. [DOI] [PubMed] [Google Scholar]
- 56.Schellongowski P, Staudinger T, Kundi M. Prognostic factors for intensive care unit admission, intensive care outcome, and post-intensive care survival in patients with de novo acute myeloid leukemia: a single center experience. Haematologica. 2011;96:231–237. doi: 10.3324/haematol.2010.031583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Algrin C, Faguer S, Lemiale V. Outcomes after intensive care unit admission of patients with newly diagnosed lymphoma. Leuk Lymphoma. 2015;56:1240–1245. doi: 10.3109/10428194.2014.922181. [DOI] [PubMed] [Google Scholar]
- 58.Maeda T, Babazono A, Nishi T, Matsuda S, Fushimi K, Fujimori K. Quantification of the effect of chemotherapy and steroids on risk of Pneumocystis jiroveci among hospitalized patients with adult T-cell leukaemia. Br J Haematol. 2015;168:501–506. doi: 10.1111/bjh.13154. [DOI] [PubMed] [Google Scholar]
- 59.Azoulay E, Darmon M, Delclaux C. Deterioration of previous acute lung injury during neutropenia recovery. Crit Care Med. 2002;30:781–786. doi: 10.1097/00003246-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Seo S, Renaud C, Kuypers JM. Idiopathic pneumonia syndrome after hematopoietic cell transplantation: evidence of occult infectious etiologies. Blood. 2015;125:3789–3797. doi: 10.1182/blood-2014-12-617035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Andes DR, Safdar N, Baddley JW. The epidemiology and outcomes of invasive Candida infections among organ transplant recipients in the United States: results of the Transplant-Associated Infection Surveillance Network (TRANSNET) Transpl Infect Dis. 2016;18:921–931. doi: 10.1111/tid.12613. [DOI] [PubMed] [Google Scholar]
- 62.Lebeaux D, Freund R, van Delden C. Outcome and treatment of nocardiosis after solid organ transplantation: new insights from a European study. Clin Infect Dis. 2017;64:1396–1405. doi: 10.1093/cid/cix124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Natori Y, Humar A, Husain S. Recurrence of CMV infection and the effect of prolonged antivirals in organ transplant recipients. Transplantation. 2017;101:1449–1454. doi: 10.1097/TP.0000000000001338. [DOI] [PubMed] [Google Scholar]
- 64.Kritikos A, Manuel O. Bloodstream infections after solid-organ transplantation. Virulence. 2016;7:329–340. doi: 10.1080/21505594.2016.1139279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Helfrich M, Dorschner P, Thomas K, Stosor V, Ison MG. A retrospective study to describe the epidemiology and outcomes of opportunistic infections after abdominal organ transplantation. Transpl Infect Dis. 2017;19:e12691. doi: 10.1111/tid.12691. [DOI] [PubMed] [Google Scholar]
- 66.Ulubay G, Kupeli E, Duvenci Birben O. A 10-year experience of tuberculosis in solid-organ transplant recipients. Exp Clin Transplant. 2015;13(suppl 1):214–218. [PubMed] [Google Scholar]
- 67.Dizdar OS, Ersoy A, Akalin H. Pneumonia after kidney transplant: incidence, risk factors, and mortality. Exp Clin Transplant. 2014;12:205–211. [PubMed] [Google Scholar]
- 68.Tu G, Ju M, Zheng Y. Early- and late-onset severe pneumonia after renal transplantation. Int J Clin Exp Med. 2015;8:1324–1332. [PMC free article] [PubMed] [Google Scholar]
- 69.Chung BH, Yun JT, Ha SE. Combined use of rituximab and plasmapheresis pre-transplant increases post-transplant infections in renal transplant recipients with basiliximab induction therapy. Transpl Infect Dis. 2013;15:559–568. doi: 10.1111/tid.12135. [DOI] [PubMed] [Google Scholar]
- 70.Khanna R. Immune monitoring of infectious complications in transplant patients: an important step towards improved clinical management. J Clin Microbiol. 2018;56:e02009–e02117. doi: 10.1128/JCM.02009-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heussel CP, Kauczor HU, Heussel GE. Pneumonia in febrile neutropenic patients and in bone marrow and blood stem-cell transplant recipients: use of high-resolution computed tomography. J Clin Oncol. 1999;17:796–805. doi: 10.1200/JCO.1999.17.3.796. [DOI] [PubMed] [Google Scholar]
- 72.Maschmeyer G, Carratalà J, Buchheidt D. Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO) Ann Oncol. 2015;26:21–33. doi: 10.1093/annonc/mdu192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gruson D, Hilbert G, Valentino R. Utility of fiberoptic bronchoscopy in neutropenic patients admitted to the intensive care unit with pulmonary infiltrates. Crit Care Med. 2000;28:2224–2230. doi: 10.1097/00003246-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 75.Hilbert G, Gruson D, Vargas F. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481–487. doi: 10.1056/NEJM200102153440703. [DOI] [PubMed] [Google Scholar]
- 76.Azoulay E, Mokart D, Rabbat A. Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med. 2008;36:100–107. doi: 10.1097/01.CCM.0000295590.33145.C4. [DOI] [PubMed] [Google Scholar]
- 77.Wohlfarth P, Beutel G, Lebiedz P. Intensive care in hematologic and oncologic patients (iCHOP); caring for critically ill immunocompromised patients multinational network (NINE-I) Crit Care Med. 2017;45:e500–e507. [Google Scholar]
- 78.Schmidt M, Schellongowski P, Patroniti N. Six-month outcome of immunocompromised severe acute respiratory distress syndrome patients rescued by extracorporeal membrane oxygenation. An international multicenter retrospective study. Am J Respir Crit Care Med. 2018;197:1297–1307. doi: 10.1164/rccm.201708-1761OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Antonelli M, Conti G, Bufi M. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA. 2000;283:235–241. doi: 10.1001/jama.283.2.235. [DOI] [PubMed] [Google Scholar]
- 80.Lemiale V, Resche-Rigon M, Mokart D. High-flow nasal cannula oxygenation in immunocompromised patients with acute hypoxemic respiratory failure: a groupe de recherche respiratoire en réanimation onco-hématologique study. Crit Care Med. 2017;45:e274–e280. doi: 10.1097/CCM.0000000000002085. [DOI] [PubMed] [Google Scholar]
- 81.Mokart D, Geay C, Chow-Chine L. High-flow oxygen therapy in cancer patients with acute respiratory failure. Intensive Care Med. 2015;41:2008–2010. doi: 10.1007/s00134-015-3994-8. [DOI] [PubMed] [Google Scholar]
- 82.Coudroy R, Jamet A, Petua P, Robert R, Frat J-P, Thille AW. High-flow nasal cannula oxygen therapy versus noninvasive ventilation in immunocompromised patients with acute respiratory failure: an observational cohort study. Ann Intensive Care. 2016;6:45. doi: 10.1186/s13613-016-0151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tu G, He H, Yin K. High-flow nasal cannula versus noninvasive ventilation for treatment of acute hypoxemic respiratory failure in renal transplant recipients. Transplant Proc. 2017;49:1325–1330. doi: 10.1016/j.transproceed.2017.03.088. [DOI] [PubMed] [Google Scholar]
- 84.Lewandowska DW, Schreiber PW, Schuurmans MM. Metagenomic sequencing complements routine diagnostics in identifying viral pathogens in lung transplant recipients with unknown etiology of respiratory infection. PloS One. 2017;12:e0177340. doi: 10.1371/journal.pone.0177340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.White DA, Wong PW, Downey R. The utility of open lung biopsy in patients with hematologic malignancies. Am J Respir Crit Care Med. 2000;161:723–729. doi: 10.1164/ajrccm.161.3.9904016. [DOI] [PubMed] [Google Scholar]
- 86.Gossot D, Girard P, de Kerviler E. Thoracoscopy or CT-guided biopsy for residual intrathoracic masses after treatment of lymphoma. Chest. 2001;120:289–294. doi: 10.1378/chest.120.1.289. [DOI] [PubMed] [Google Scholar]
- 87.Dai MS, Lee SC, Ho CL, Chen YC, Kao WY, Chao TY. Impact of open lung biopsy for undiagnosed pulmonary infiltrates in patients with hematological malignancies. Am J Hematol. 2001;68:87–90. doi: 10.1002/ajh.1158. [DOI] [PubMed] [Google Scholar]
- 88.Kim K, Lee MH, Kim J. Importance of open lung biopsy in the diagnosis of invasive pulmonary aspergillosis in patients with hematologic malignancies. Am J Hematol. 2002;71:75–79. doi: 10.1002/ajh.10168. [DOI] [PubMed] [Google Scholar]
- 89.Sharma S, Nadrous HF, Peters SG. Pulmonary complications in adult blood and marrow transplant recipients: autopsy findings. Chest. 2005;128:1385–1392. doi: 10.1378/chest.128.3.1385. [DOI] [PubMed] [Google Scholar]
- 90.Zihlif M, Khanchandani G, Ahmed HP, Soubani AO. Surgical lung biopsy in patients with hematological malignancy or hematopoietic stem cell transplantation and unexplained pulmonary infiltrates: improved outcome with specific diagnosis. Am J Hematol. 2005;78:94–99. doi: 10.1002/ajh.20258. [DOI] [PubMed] [Google Scholar]
- 91.Gupta S, Sultenfuss M, Romaguera JE. CT-guided percutaneous lung biopsies in patients with haematologic malignancies and undiagnosed pulmonary lesions. Hematol Oncol. 2010;28:75–81. doi: 10.1002/hon.923. [DOI] [PubMed] [Google Scholar]
- 92.Sharma SK, Kumar S, Singh AK. Feasibility and outcome of CT-guided lung biopsy in patients with hematological diseases and suspected fungal pneumonia. J Infect Dev Ctries. 2013;7:748–752. doi: 10.3855/jidc.2823. [DOI] [PubMed] [Google Scholar]
- 93.Gay J, Lemiale V, Meignin V. Diagnostic contribution from pulmonary biopsies in hematology patients with acute respiratory failure from undetermined etiology. Minerva Anestesiol. 2013;79:853–860. [PubMed] [Google Scholar]
- 94.Uhlving HH, Andersen CB, Christensen IJ. Biopsy-verified bronchiolitis obliterans and other noninfectious lung pathologies after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21:531–538. doi: 10.1016/j.bbmt.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 95.Contejean A, Lemiale V, Resche-Rigon M. Increased mortality in hematological malignancy patients with acute respiratory failure from undetermined etiology: a groupe de recherche en réanimation respiratoire en onco-hématologique (Grrr-OH) study. Ann Intensive Care. 2016;6:102. doi: 10.1186/s13613-016-0202-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.de Hemptinne Q, Remmelink M, Brimioulle S, Salmon I, Vincent J-L. ARDS: a clinicopathological confrontation. Chest. 2009;135:944–949. doi: 10.1378/chest.08-1741. [DOI] [PubMed] [Google Scholar]
- 97.de Bazelaire C, Coffin A, Cohen-Zarade S. CT-guided biopsies in lung infections in patients with haematological malignancies. Diagn Interv Imaging. 2013;94:202–215. doi: 10.1016/j.diii.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 98.Nosari A, Anghilieri M, Carrafiello G. Utility of percutaneous lung biopsy for diagnosing filamentous fungal infections in hematologic malignancies. Haematologica. 2003;88:1405–1409. [PubMed] [Google Scholar]
- 99.Fruchter O, Fridel L, Rosengarten D, Rahman NA, Kramer MR. Transbronchial cryobiopsy in immunocompromised patients with pulmonary infiltrates: a pilot study. Lung. 2013;191:619–624. doi: 10.1007/s00408-013-9507-z. [DOI] [PubMed] [Google Scholar]
- 100.Dhooria S, Sehgal IS, Aggarwal AN, Behera D, Agarwal R. Diagnostic yield and safety of cryoprobe transbronchial lung biopsy in diffuse parenchymal lung diseases: systematic review and meta-analysis. Respir Care. 2016;61:700–712. doi: 10.4187/respcare.04488. [DOI] [PubMed] [Google Scholar]
- 101.Rochwerg B, Brochard L, Elliott MW. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 102.Gristina GR, De Gaudio R, Mazzon D, Curtis JR. End of life care in Italian intensive care units: where are we now? Minerva Anestesiol. 2011;77:911–920. [PubMed] [Google Scholar]
- 103.Depuydt PO, Benoit DD, Vandewoude KH, Decruyenaere JM, Colardyn FA. Outcome in noninvasively and invasively ventilated hematologic patients with acute respiratory failure. Chest. 2004;126:1299–1306. doi: 10.1378/chest.126.4.1299. [DOI] [PubMed] [Google Scholar]
- 104.Neuschwander A, Lemiale V, Darmon M. Noninvasive ventilation during acute respiratory distress syndrome in patients with cancer: trends in use and outcome. J Crit Care. 2017;38:295–299. doi: 10.1016/j.jcrc.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 105.Bellani G, Laffey JG, Pham T. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 106.Papazian L, Corley A, Hess D. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42:1336–1349. doi: 10.1007/s00134-016-4277-8. [DOI] [PubMed] [Google Scholar]
- 107.Mauri T, Turrini C, Eronia N. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–1215. doi: 10.1164/rccm.201605-0916OC. [DOI] [PubMed] [Google Scholar]
- 108.Mauri T, Alban L, Turrini C. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43:1453–1463. doi: 10.1007/s00134-017-4890-1. [DOI] [PubMed] [Google Scholar]
- 109.Frat J-P, Thille AW, Mercat A. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 110.Lee HY, Rhee CK, Lee JW. Feasibility of high-flow nasal cannula oxygen therapy for acute respiratory failure in patients with hematologic malignancies: a retrospective single-center study. J Crit Care. 2015;30:773–777. doi: 10.1016/j.jcrc.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 111.Epstein AS, Hartridge-Lambert SK, Ramaker JS, Voigt LP, Portlock CS. Humidified high-flow nasal oxygen utilization in patients with cancer at Memorial Sloan-Kettering Cancer Center. J Palliat Med. 2011;14:835–839. doi: 10.1089/jpm.2011.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harada K, Kurosawa S, Hino Y. Clinical utility of high-flow nasal cannula oxygen therapy for acute respiratory failure in patients with hematological disease. SpringerPlus. 2016;5:512. doi: 10.1186/s40064-016-2161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hui D, Morgado M, Chisholm G. High-flow oxygen and bilevel positive airway pressure for persistent dyspnea in patients with advanced cancer: a phase II randomized trial. J Pain Symptom Manage. 2013;46:463–473. doi: 10.1016/j.jpainsymman.2012.10.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Uncited Reference
- 74.Rañó A, Agustí C, Jimenez P. Pulmonary infiltrates in non-HIV immunocompromised patients: a diagnostic approach using non-invasive and bronchoscopic procedures. Thorax. 2001;56:379–387. doi: 10.1136/thorax.56.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]