Abstract
Toona sinensis (TS), which is also known as Cedrela sinensis, belongs to Meliaceae family, the compounds identified from this TS leaves possess a wide range of biologic functions, such as hypoglycemic effects, anti–LDL glycative activity, antioxidant activities, and inhibition of sudden acute respiratory syndrome (SARS) coronavirus replication. However, their effect against cancer cells is not well explored. In this study, to understand the cytotoxic effect and molecular mechanism stimulated by TSL-1 (TS leaf extract fraction) we employed three different non–small-cell lung cancer (NSCLC) cell lines: H441 cells (lung adenocarcinoma), H661 cells (lung large cell carcinoma) and H520 cells (lung squamous cell carcinoma). IC50 value was varied between these three cell lines, the least IC50 value was observed in TSL-1–treated H661cells. Exposure of NSCLC cells to TSL-1 caused cell-cycle arrest in subG1 phase and caused apoptosis. Moreover, TSL-1 treatment decreased the cell-cycle regulators; cyclin D1 and CDK4 proteins by up regulating p27 expression in a dose-dependent manner. Thus, the TSL-1–induced apoptosis was further confirmed by cell morphology, subG1 peak accumulation, poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP) cleavage, propidium iodide (PI)-Annexin-V double staining, and terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling (TUNEL) assay. The decreased Bcl2 protein level was concurrent with an increased Bax protein level in all 3 cell lines. Additionally, the tumoricidal effect of TSL-1 was measured using a xenograft model, after 5 weeks of TSL-1 treatment by various regimen caused regression of tumor. Taken together both these in vitro and in vivo studies revealed that TSL-1 is a potent inhibitor against NSCLC growth and our provoking result suggest that TSL-1 can be a better nutriceutical as a singlet or along with doublet agents (taxane, vinorelbine, and gemcitabine) for treating NSCLC.
Abbreviations: CDK, cyclin-dependent kinase; ECL, enhanced chemiluminescence; FACS, fluorescence-activated cell sorting; FBS, fetal bovine serum; IC50, half maximal inhibitory concentration; MTT, tetrazolium dye; NSCLC, non–small-cell lung cancer; PARP, poly(adenosine diphosphate [ADP]-ribose) polymerase; PBS, phosphate-buffered saline; PI, propidium iodide; SKOV3, human ovarian cancer cell; RT, room temperature; TS, Toona sinensis; TSL-1, TS leaf extract fraction-1; TUNEL, terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling
At a Glance Commentary.
Yang C-J, et al.
Background
The chemotherapeutic benefits and the prognosis for advanced non-small-cell lung cancer (NSCLC) remain to be promoted. Toona sinensis (TS), which is a traditional Chinese herb, possesses a variety of biologic functions.
Translational significance
Flow cytometry analysis showed that the TS leaf extract fraction-1 (TSL-1) treatment induced a G1 phase arrest in NSCLC cells and was accompanied by the downregulation of cyclin-D1 protein levels. Cyclin-dependent kinase-4 (CDK4) protein levels decreased in H441 and H661, whereas TSL-1–treated H520 and H661 cells showed an increase in p27 activity. TSL-1–induced apoptosis was confirmed by cell morphology, subG1 peak accumulation, poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP) cleavage, propidium iodide (PI)-Annexin-V double staining, TUNEL assay, Bcl-2, and Bax expression. Furthermore, the tumoricidal effect of TSL-1 was confirmed by a nude mice model. Thus, we conclude that TSL-1 could be taken as a nutriceutical and is an efficacious candidate for developing an anticancer drug.
In world wide, lung carcinoma is one of the leading causes of cancer related death in both men and women.1 Compared with the other subtype (small cell lung cancer), non small-cell lung cancer (NSCLC) represents 75% to 80% of all lung neoplasms. The majority of these patients present with advanced, unresected, or metastatic disease, and approximately 15% of unselected patients are expected to be active for five years.1 Thus the chemotherapeutic benefits in developing new anti-lung cancer drugs and the prognosis for advanced NSCLC has become an important and insistent issue.2
Cell-cycle is a critical regulator for cell growth and cell proliferation following DNA damage: for proper functioning of cell-cycle machinery; cyclin-dependent kinases (CDKs), has to be positively regulated by cyclins and negatively regulated by cyclin dependent kinase inhibitors. It is well known that the drugs which target cyclin dependent kinase can be used as a better anticancer agent. Now a days naturally occurring substances are recognized as antioxidants, cancer-preventive agents, or even as cancer therapy drugs, such as taxol2 or flavopiridol,3, 4, 5, 6 and UCN-01 (7-hydroxytaurosporine).7, 8, 9 Those bioactive substances exert their anticancer activity by blocking cell-cycle progression and triggering tumor cell apoptosis. Similarly, substances inducing G1 phase arrest are considered a potential candidate to treat developing cancer slowly.10
However, chemotherapy does not substantially improvise the survival of the lung cancer patients, and it is clear that chemotherapy has reached a plateau of activity in treating NSCLC.11 Toona sinesis (TS) a traditional Chinese herb leaf extract possess anti-proliferative properties against human lung adenocarcinoma cells (A549),12 ovarian cancer cells (SKOV3),13 and human premyelocytic leukemia cells (HL-60).14 In a recent report, it was found that TS-1 (leaf extract fraction) could inhibit H441 cell proliferation both in vitro and in vivo.15 To support the former data in the present study, the cellular and molecular mechanisms of TSL-1 action against human cancer cells was examined using in vitro and in vivo models. Our results indicate that inhibition of cell-cycle progression and induction of apoptotic cell death contributes to the antiproliferative effects of TSL-1 in NSCLC cells.
Materials and Methods
Plant materials and preparation of TSL-1
The leaves used in this study were obtained from TS grown in Tuku (Yunlin County, Taiwan). The leaves were collected and washed briskly with water; TSL-1 fraction was extracted as mentioned in our previous study.16
Cell viability assays
H441 (lung adenocarcinoma cell lines), H520 (lung squamous cell lines), and H661 (lung large-cancer cells) were obtained from the American Type Culture Collection (Rockville, Md). H441 (1 × 104 cells/well), H520 (1 × 104 cells/well), and H661 cells (4 × 103 cells/well) were seeded in 96-well plates and grown in RPMI 1640 medium supplemented with 10% heat inactivated fetal bovine serum (FBS), 100 IU/mL penicillin, 2 mmol/L L-glutamine, 10 mmol/L HEPES, and 1.0 mmol/L sodium pyruvate in a 5% CO2 incubator at 37 °C overnight. The cells were then incubated in 10% FBS media with different concentration of TSL-1 for 24 h and 48 h. Cell growth was estimated by a colorimetric assay based on the conservation of tetrazolium dye (MTT) to a blue formazan product by live mitochondria.17
Western blot analysis
After treatment, the cells were rinsed with ice-cold phosphate-buffered saline (PBS) and harvested in a lysis buffer16 for 20 min on ice. Cellular lysates were centrifuged at 12,000 × g for 10 min, and the protein concentrations of the lysates were determined using a bicinchoninic acid (BCA) protein assay kit (Pierce, Rockford, Ill). The procedure for Western blot was slightly modified from our previous study.17 The blots were incubated with various primary antibodies, such as cyclin D1, CDK4, p27, Bcl-2, and Bax (Santa Cruz Biotechnology, Santa Cruz, Calif) for 1 h at room temperature (RT), and then incubated with peroxidase-conjugated secondary antibody for an additional 1 h. The signals of blots were then developed using the enhanced chemiluminescence (ECL) system (Amersham Biosciences Corp., Piscataway, NJ).
Analysis of cell-cycle distribution
The cells were cultured in the absence or presence of TSL-1 (0.5 mg/mL) for 24 h in 10% FBS media. The cells were fixed with 95% ethanol and stained with propidium iodide (PI). Cell-cycle distribution was analyzed by fluorescence-activated cell sorting (FACS) flow cytometry (Becton Dickinson, Mountain View, Calif).
Apoptosis assays
The cells were cultured in 6-well plates in 10% FBS media and were incubated with vehicle or different amounts of TSL-1 for 24 or 48 h. After incubation, the detached cells were collected by centrifugation, and the attached cells were harvested by trypsinization. The cells were pooled and were analyzed for degradation of PARP as described previously.17
Measurement of apoptosis by flow cytometry
After treatment, Annexin-V (Annexin V-FITC, 1 μg/mL; Strong Biotech, Taipei, Taiwan) staining was performed to detect apoptotic cells. The cells were washed with cold HEPES buffer (10 mmol/L HEPES/NaOH, pH 7.4, 140 mmol/L NaCl, 5 mmol/L CaCl2) and centrifuged at 1500 × g for 10 min. The cell pellets were resuspended in 100 μL of staining solution (2 μL Annexin-V-fluos and 20 μL PI in 100 μL HEPES buffer) and incubated for 10–15 min at RT in darkness. Annexin-V or PI fluorescent intensities were analyzed by flow cytometry, and 10,000 cells were evaluated in each sample.
Terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling (TUNEL) assay
The TUNEL assay was used to detect DNA strand breaks. Detection was carried out according to the instructions of the TACSTM2 TdT-DAB In Situ apoptosis detection kit (Trevigen, Gaithersburg, Md). Briefly, the cells were rinsed once with PBS and fixed in 4% buffered formaldehyde at RT for 5 min. The fixed sections were pretreated with 3% H2O2, and end labeling was performed with TdT labeling reaction mix at 37 °C for 1.5 h. Nuclei exhibiting DNA fragmentation were visualized by incubation in 3′, 3-diamino benzidine DAB for 1–3 min. Lastly, the sections were counterstained with methyl green and observed by optical microscope (Zeiss Axiovert100M; Carl Zeiss, Oberkochen, Germany). The nuclei of the apoptotic cells were stained dark brown.
Nude mice experiments
Animal experiments were performed according to the guidelines set by our institute (Guide for Care and Use of Laboratory Animals, Kaohsiung Medical University). Male BALB/cA-nu nude mice (8 wks old) were housed in pathogen free barrier facilities. Tumors were induced by subcutaneous (sc) injection of H441, H520 and H661 (2×107 cells in 0.1 mL of PBS each cell line) on the right flank. Tumors (visualized as small nodules at the sites of injection) appeared after 14 days of H441 cells injection. Tumor bearing nude mice were randomly distributed into 4 groups (n = 7). Mice in the TSL-1 treated group were PO injected with both i) low dosage (1 g/kg Bwt TSL-1), ii) high dosage (5 g/kg Bwt TSL-1), and iii) mice treated with high dose of TSL-1 by i.p (50 mg/kg Bwt TSL-1). The control group was treated with an equal volume of vehicle (double distilled water, DDW).
In another set of experiments, the animals were pretreated with vehicle or TSL-1 for 35 days. For the therapeutic or preventive experiments, tumors were induced by subcutaneous (sc) injection as mentioned above. After 14 days of injection, nude mice bearing tumors were randomly distributed into 3 groups: the control group, which received the vehicle (DDW), where as in TSL-1 received groups (1 g/kg Bwt) were further treated for 42 days (1) mice pretreated with TSL-1 were post treated with DDW and other group (2) post treated with (1 g/kg Bwt) TSL-1. After transplantation, tumor size was measured using calipers and tumor volume was estimated according to the formula:
Tumor volume = larger diameter L × small diameter2/2.
Statistical analysis
Data are presented as mean ± standard deviation for the indicated number of separate experiments. Analysis of variance (ANOVA) was followed by Dunnett's test for pair wise comparisons. Statistical significance was defined as P-value less than 0.05 in all tests.
Results
Cytotoxicity of TSL-1 on the 3 lung cancer cell lines
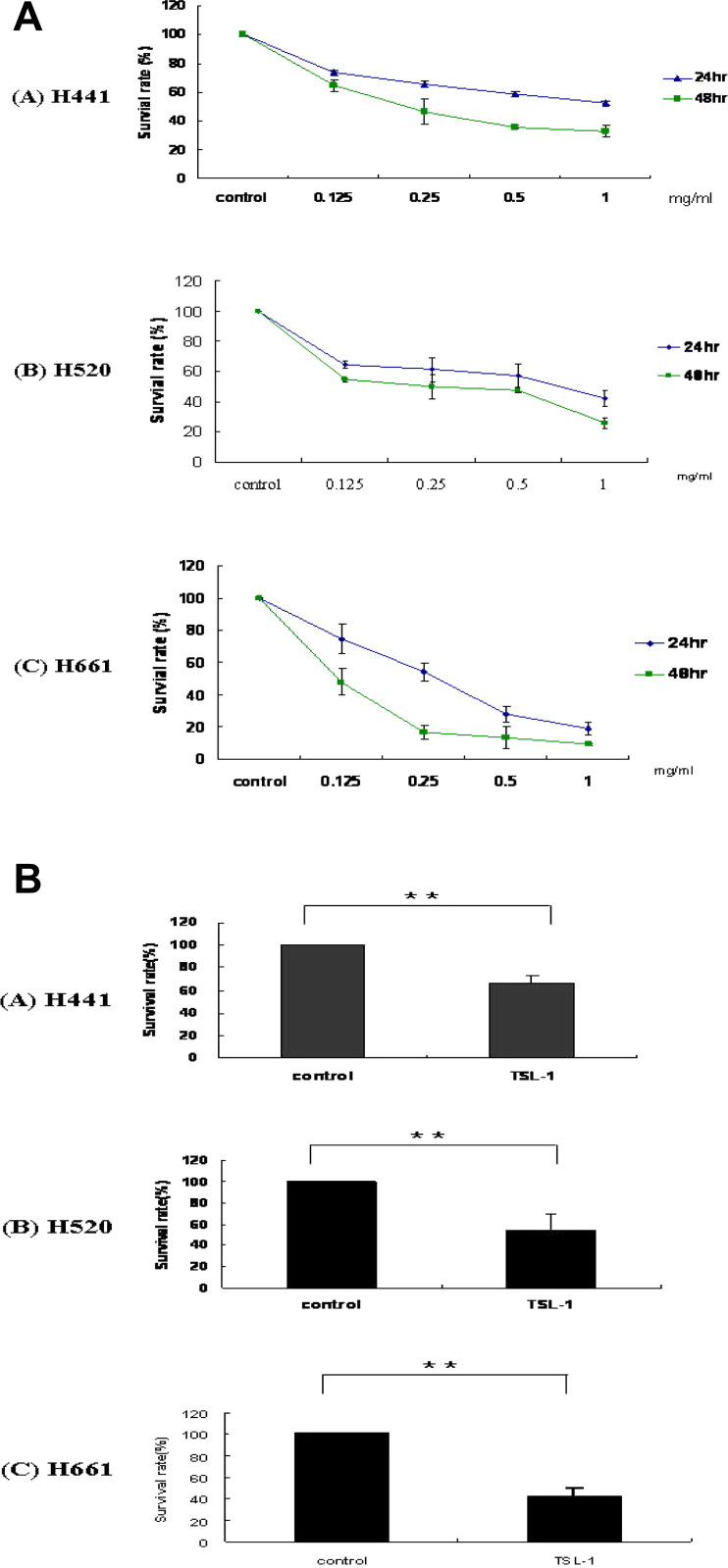
NSCLC cells were treated with or without TSL-1 for different time points; IC50 values of TSL-1 treated tumor cells for 48 h were, 0.20 mg/mL for H441 cells, 0.25 mg/mL for H520 cells, and 0.12 mg/mL for H661 cells, respectively. Compared with the 24 h time point, 48 h treatment showed better inhibitory effect in all 3 lung cancer cell lines. Among the 3 cell lines, H661-treated cells displayed a lower IC50 value (Fig 1 , A and B). These experiments showed that TSL-1 could induce high cytotoxicity against NSCLC cells.
Fig 1.
The cell viability of NSCLC cells after TSL-1 treatment. (A) The dose response of TSL-1 extract (0.125–1 mg/mL) on H441, H520, and H661 cells after 24 and 48 h treatment was assessed by MTT. (B) Percentage of survival rate for 24 h was calculated between 0.5 mg/mL of TSL-1 treatment and control. The data are presented as mean ± SD from three different experiments. ∗∗P < 0.01 represents the level of significance differences between control and TSL-1 treatments.
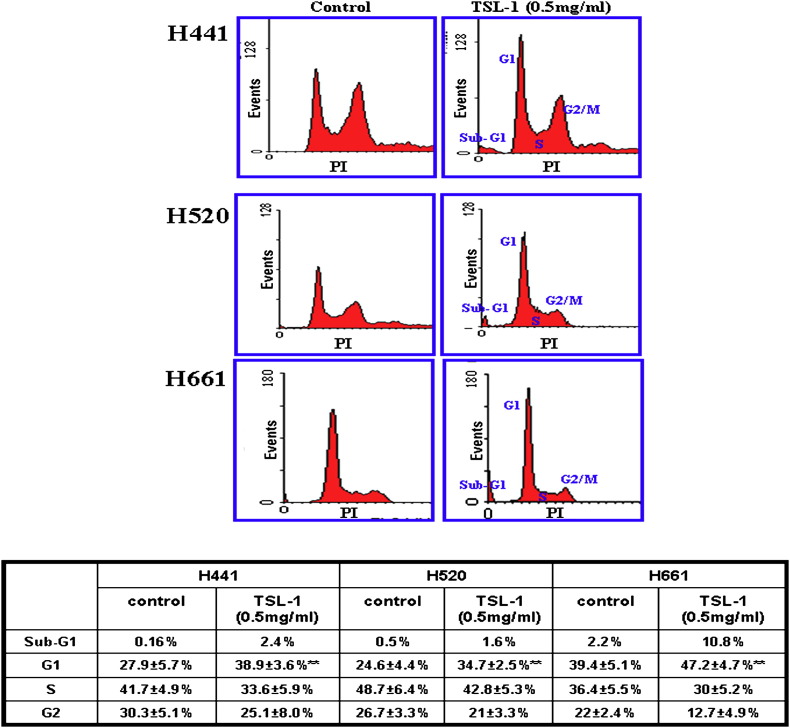
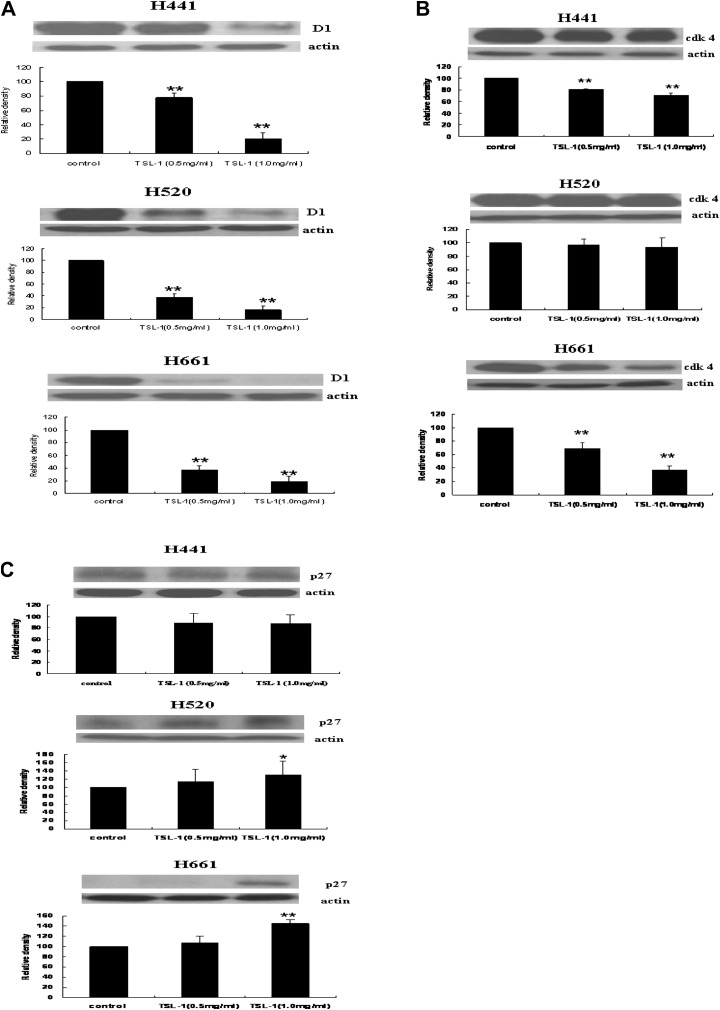
Effects of TSL-1 on cell-cycle distribution and cell-cycle–related proteins
To examine the underlying mechanism for TSL-1–mediated cell proliferation inhibition, cell-cycle distribution was evaluated using flow cytometric analysis. TSL-1–treated NSCLC cells showed a significant increase in the G1-phase compared with the control group (Fig 2 ). Next, we analyzed the effect of TSL-1 on cell-cycle proteins; the result showed that TSL-1 could inhibit cyclin D1 and CDK4 protein levels in all 3 NSCLCs, thereby upregulating the p27 expression level. The decrease in both cyclin D1 and CDK4 coupled with an increase in p27 was more significant in H661 cells when compared with the other 2 cell lines (Fig 3 ). Thus, TSL-1 treatment induced G1 cell-cycle arrest was associated with the result of cell-cycle–related proteins.
Fig 2.
The alterations of cell cycle after TSL-1 treatment on various types of NSCLC. Arrest of H441, H520, and H661 cells in the subG1 and G1 phase of the cell cycle after treatment with TSL-1 (0.5 mg/mL) for 24 h was assayed by propidium iodide staining and FACS analysis. The data are presented as mean ± SD from 3 different experiments. ∗∗P < 0.01 represents the level of significance differences between control and TSL-1 treatments. (Color version of figure is available online.)
Fig 3.
The effect of TSL-1 in NSCLC cells on cell-cycle-related molecules. The alterations of (A) cyclin D1, (B) CDK4, and (C) P27 after TSL-1 treatment (0.5 and 1 mg/mL) for 24 h were assessed using Western blotting. All bands present in the different panels are the typical picture as a representative one. The data are presented as mean ± SD from 3 different experiments. ∗P < 0.05; ∗∗P < 0.01 represents the level of significance differences between control and TSL-1 treatments.
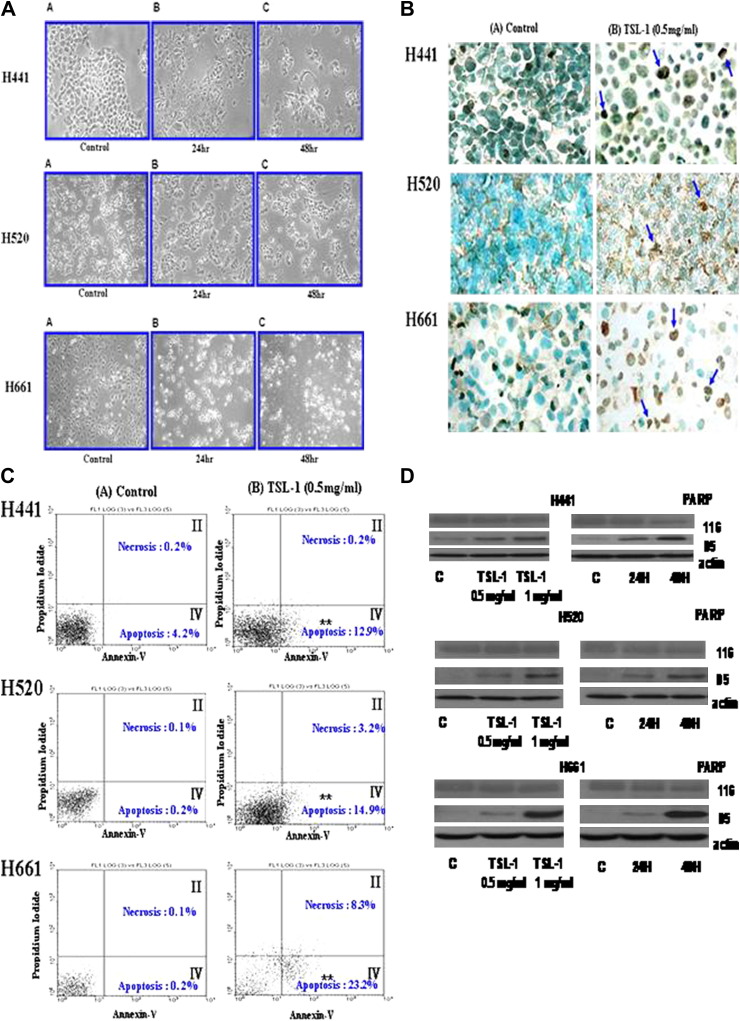
Apoptotic effect of TSL-1 on the 3 cancer cell lines
Four separate assays were applied to investigate the induction of apoptosis in NSCLC by TSL-1 treatment (Fig 4 ). The cells were treated for 48 h with 0.5 mg/mL TSL-1 and were analyzed for apoptosis by the TUNEL, cell morphology, subG1 peak accumulation, the cleavage of PARP, and PI-Annexin-V double staining.
Fig 4.
Induction of apoptosis by TSL-1(0.5 or 1 mg/mL) in NSCLC cells after 48 h treatment. The data were determined by the (A) cell morphology, (B) TUNEL assay, (C) PI-Annexin-V double staining, and (D) PARP cleavage by Western blotting. (Color version of figure is available online.)
Cell morphology was determined to analyze the effect of treatment in inducing apoptosis in both untreated and TSL-1–treated NSCLC; apoptotic bodies were observed and some substances in the cytosol were released to the media with a time-dependent effect (Fig 4, A). TSL-1 treatment induced apoptosis as shown by the TUNEL assay (Fig 4, B). These apoptotic features observed in the TSL-1 treated cells include brown-stained fragmented nuclei, irregular-shaped cells, and irregular cytoplasmic membranes. In addition, the percentage of Annexin V-positive cells, which is indicative of early apoptosis, increased from 4.2% in the control to 12.9% in TSL-1–treated H441 cells; similarly, an increase of apoptosis from 0.2% in the H520 and H661 control cells to 14.9% to 23.2% of TSL-1–treated cells was observed. Moreover, TSL-1 treatment increased the percentage of cells positive for both Annexin V and propidium iodide (hallmarks of late apoptosis) from 0.2% in the controls to 0.2%, 3.2%, and 8.3% in H441, H520, and H661 cells, respectively (Fig 4, C). A Western blot analysis was performed to evaluate the activation of PARP downstream of the mitochondria-mediated apoptotic pathway. From (Fig 4, D). we observed an increase in 85- kDa cleavage product with respect to TSL-1 concentration. This result was consistent with all the 3 cell lines used. Taken together, we conclude that TSL-1 induces the apoptosis on NSCLC cells.
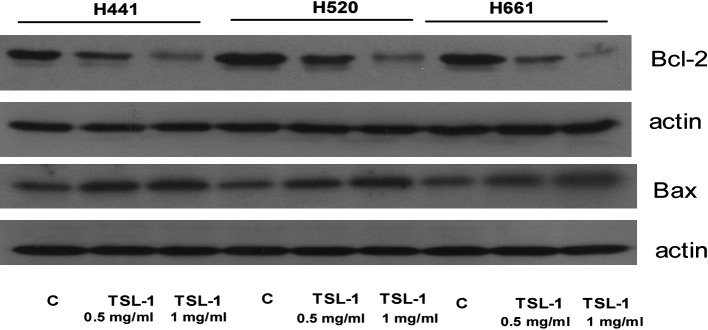
Effects of TSL-1 on Bcl-2 family proteins
It is well known that Bcl-2 family members can induce or inhibit apoptosis. Western blot analysis showed that with increase in TSL-1 concentration decreased Bcl-2 proteins expression in all the 3 cell lines. At the same time TSL-1 treated H441, H520 and H661 cell lines showed increased Bax protein levels when compared with their respective control (Fig. 5 ). These results indicate that Bcl-2 protein family might involve in TSL-1 mediated apoptosis.
Fig 5.
Bcl-2 families of proteins are involved in TSL-1–induced apoptosis. Expression of Bcl-2 family proteins, H441, H520, and H661 cells were treated with 0.5 or 1 mg/mL of TSL-1 for 24 h. All proteins were extracted, and the levels of Bcl-2 and Bax expression were analyzed using Western blotting.
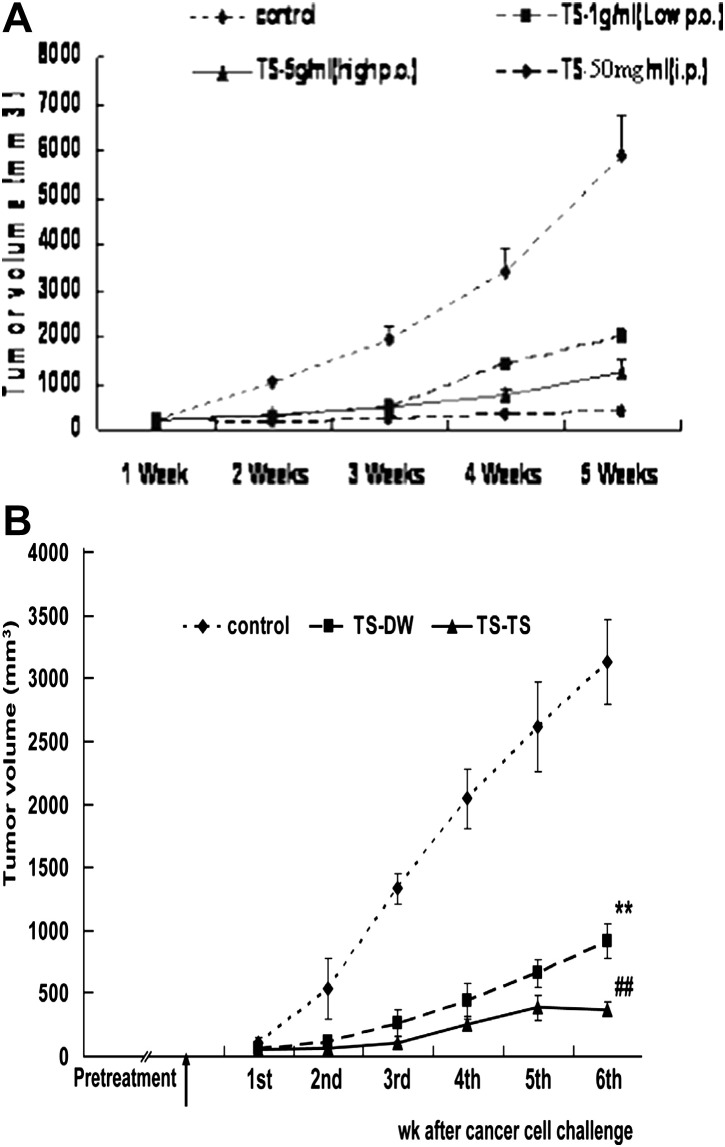
TSL-1 inhibits tumor growth in nude mice
To understand the effect of TSL-1 on NSCLC cells, equal number of H441, H520 and H661 cells were injected on the right flank of nude mice, tumor was (visualized as small nodules at the sites of injection) appeared after 14 days of H441 cells injection; but the other 2 cell lines failed to induce tumor formation. Compared with the control (5.87 ± 1.13 ×103 mm3), TSL-1 treatment (intraperitonial) for 35 days showed reduction in tumor size (0.38 ± 0.06 × 103 mm3). Similar result was found when low (2.03 ± 0.12 × 103 mm3) and high dose (1.24 ± 0.15 × 103 mm3) of TSL-1 was administrated via p.o (Fig. 6 A). These results revealed that TSL-1 caused tumor shrinkage in a dose dependent manner. To test the preventive effects of TSL-1 on tumor formation, mice were pretreated with vehicle (Control) or TSL-1 for 30 days and then inoculated with H441 cells. These groups were further treated using distilled water or TSL-1 for an additional 42 days and were observed for tumor shrinkage. Compared with the control [distilled water (Control)] tumor volume (3.13 ± 0.32 × 103 mm3), pretreatment with TSL-1 and posttreatment with distilled water showed reduction in tumor volume by (0.94 ± 0.21 × 103 mm3), where as in both pre and post treated mice with TSL-1 showed reduction in the tumor size to (0.32 ± 0.13 × 103 mm3) (Fig. 5 B). No hepatic, kidney and renal toxicity were observed in TSL-1 administrated mice (Po and IP) (data not shown).
Fig 6.
The antitumorgenesis activity at various doses and regimens of TSL-1. (A) Nude mice were inoculated with adenocarcinoma (H441) NSCLC cells on the right flank of skin. The control group received double distilled water (vehicle), and other group received 3 different TSL-1 treatments for 35 days. Group 1 mice were treated with a low dose (1 g/kg body weight [Bwt]) of TSL-1 via PO; group 2 mice were treated with a high dose (5 g/kg Bwt) of TSL-1 via PO; and group 3 mice were treated with a high dose (50 mg/kg Bwt) of of TSL-1 intraperitoneally. (B) Nude mice were pretreated (PO) with TSL-1 or vehicle (DDW) for 30 days; the nude mice were then inoculated with adenocarcinoma (H441) through the skin after tumor formation control groups received distilled water for 42 days, where as the other 2 groups were treated for an additional 42 days as follows: group a: TS-DW received double distilled water and group b: TS-TS received 1 g/kg Bwt of TSL-1 for an additional 42 days. The data are presented as mean ± SD (n = 7). ∗∗P < 0.01 represents the level of significance of differences between control and TSL-1 treatment. ##P < 0.01 represents the level significant of differences between groups a and b at 42 days.
Discussion
Chemotherapy is usually the best choice for treating late-stage NSCLC; however, the appearance of chemotherapeutic drug resistance results in a poor remedy and low survival rates.18 The application of Chinese herbs or medicines to treat malignant diseases has dramatically increased in recent years. In this article, TSL-1, the extract from TS leaves, demonstrated antiproliferative activity by inducing apoptosis in 3 NSCLC cell lines. A variety of phytochemical components has been isolated and characterized from TS leaves, including gallic acid, methyl gallic acid, 3-O-b-D-(60-O-galloyl)-glucopyranoside, 4-O-b-D-(60-Ogalloyl)-glucopyranoside, methyl gallate, ethyl gallate, kaempferol, kaempferol-3-O-b-glucoside, quercitrin, quercetin-3-O-b-glucoside, rutin and catechin; furthermore, polyphenols, limonoids, and methyl gallate found to have antioxidant activities to inhibit lipid peroxidation.19 Gallic acid, which is 1 of the major compounds found in TSL-1, has anti-inflammatory, antimutagenic, and anticarcinogenic effects, and it has been found to induce apoptosis in cancer cells through antioxidation.20, 21 Other bioactive components of TS, such as methyl gallate,22 limonoids,23 and catechin,24 are also shown to have anticancer effects. A recent study indicates that TSL-1 extract in tumor accumulated nude mice showed tumor shrinkage.15 TS leaves can provide an antioxidative capability by decreasing reactive oxygen species damage, and it subsequently induces tumor cell apoptosis. Our results strengthen the potential of TSL-1 as a new alternative medicine for anticancer therapy.
The current study shows that tumor cells are significantly more sensitive to chemotherapeutic agents when treated with TSL-1; differences in half maximal inhibitory concentration (IC50) of TSL-1 were observed among 3 NSCLC cell lines, of which H661 had the lowest concentration of IC50. This result could be caused by the different cell line characteristics. To test the underlying mechanism of cell growth inhibition by TSL-1 treatment in relation to cell-cycle change, we performed a cell-cycle analysis in TSL-1–treated cells with a 0.5-mg dose of TSL-1 induced subG1/G1 phase arrest in all 3 cell lines. Therefore, the subG1/G1 phase arrest of the cell cycle can be considered as a pathway to suppress the growth of NSCLC cells. A similar phenomenon of sub G1 phase arrest has been demonstrated in TSL-1–treated H441 cells.15 From this result, it is evident that the specificity of cell-cycle arrest by TSL-1 depends on differences in cell types, TSL-1 dosage, and exposure time.
The cell-cycle arrest in TSL-1–treated NSCLC cells was accompanied by the alteration of cell-cycle–regulated proteins. Agents that inhibit CDK activity or alter its levels could cause cell-cycle arrest, and this strategy is important for the potential use of novel anticancer drugs. CDKs and cyclins are major molecules required for proper cell-cycle events.25 Each cyclin/CDK complex phosphorylates a unique set of substrates required for continued cell-cycle progression.26 Among the CDKs that regulate the cell cycle, CDK2, CDK4, and CDK6 are activated in association with D-type cyclins or cyclin E during the progression of G1 and the G1-S transition. We found that the expressions of these CDK4 were decreased significantly in H661 compared with the other 2 cell lines. The overexpression of cyclin D1 has been found in various types of cancer, including lung cancer, hepatoma, breast cancer, uric bladder cancer, and esophageal cancer.27 The increased expression of cyclin D1 plays a critical role in tumor development and maintenance of malignant phenotype.28 Patients with cyclin D1-positive tumors had shorter survival than those with cyclin D1-negative tumors (5-year survival rates at 48% and 74%, respectively).29 The treatment of NSCLC cells with TSL-1 resulted in the downregulation of cyclin D1 and CDK4 in a dose-dependent manner by increasing the expression of cyclin-dependent inhibitor p27, which was consistent with the cell-cycle analysis.
Morphological changes of apoptosis are considered to be the results of complex cellular biochemical pathway;30 this apoptosis machinery can be initiated by multiple pathways using different initiating events and insults.31 In this study TSL-1–induced apoptosis in H441, H520, and H661 was further confirmed by morphologic study, phosphatidylserine externalization, PARP cleavage, and TUNEL assay. In fact, the presence of cleaved PARP is one of the most utilized diagnostics for the detection of apoptosis in many cell types.32 In particular, the 24-kDa fragment, which contains the DNA binding domain, may facilitate the apoptotic process by blocking the access of DNA repair enzymes to the fragmented chromatin.33 TSL-1–treated H441, H661, and H520 cells showed the induction of a cleaved 24- and 85-kDa DNA fragment, in addition to PARP cleavage; a down stream of mitochondrial mediated apoptosis pathway, we also observed that TSL-1 treatment in all the 3 cell lines decreased its Bcl-2 protein expression there by increasing Bax protein levels. Similarly, Yang et al reported TSL-1 induced Bcl-2 dependent mitochondrial pathway in H441 treated cells.15
To confirm the inhibitory effect of TSL-1 against NSCLC, we induced H441, H661 and H520 cells by subcutaneous injection in athymic nude mice. Except H441 cells; the other 2 failed to induce cancer in nude mice. In our study, various regimen and administrations (per o or i.p.) of TSL-1 in nude mice caused tumor shrinkage in contrast with the mice treated with vehicle alone. Thus TSL-1 exhibited anti-proliferative and anti-tumorogenic effects without any renal and hepato- toxicity. In vivo studies further confirm that TSL-1 is safe13 and are effective anti-proliferative compound17 as a complimentary and alternative medicine.
Conclusively, the current study demonstrates that human NSCLC cell lines became sensitive to TSL-1 treatment in both in vitro and in vivo models. These findings suggest that the extracts of TS could be taken as a nutriceutical to prevent cancer or may be a promising chemopreventive agent against human NSCLC.
References
- 1.Jemal A., Siegel R., Ward E. Cancer statistics. CA Cancer J Clin. 2006;56(106):130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.AbouEl Hassan M.A., Braam S.R., Kruyt F.A. Paclitaxel and vincristine potentiate adenoviral oncolysis that is associated with cell cycle and apoptosis modulation, whereas they differentially affect the viral life cycle in non-small-cell lung cancer cells. Cancer Gene Ther. 2006;13:1105–1114. doi: 10.1038/sj.cgt.7700984. [DOI] [PubMed] [Google Scholar]
- 3.Losiewicz M.D., Carlson B.A., Kaur G., Sausville E.A., Worland P.J. Potent inhibition of cdc2 kinase activity by the flavonoid L86-8275. Biochem Biophys Biophys Res Commun. 1994;201:589–595. doi: 10.1006/bbrc.1994.1742. [DOI] [PubMed] [Google Scholar]
- 4.Carlson B.A., Dubay M.M., Sausville E.A., Brizuela L., Worland P.J. Flavopiridol induces G1 arrest with inhibition of cyclin-dependent kinase CDC2 and CDK4 in human breast carcinoma cells. Cancer Res. 1996;56:2973–2978. [PubMed] [Google Scholar]
- 5.Carlson B.A., Pearlstein R.A., Naik R.G., Sedlacek H.H., Sausville E.A., Worland P.J. Inhibition of CDK2, CDK4 and CDK7 by flavopiridol and structural analogs. Proc Am Assoc Cancer Res. 1996;34:424. [Google Scholar]
- 6.Dumant JA. HMR Report No. B/98/0189/R, B/98/0188/R, 8/98/0187/R. HMR Oncology; 1996.
- 7.Seynaeve C.M., Stetler-Stevenson M., Sebers S., Kaur G., Sausville E.A., Worland P.J. Cell cycle arrest and growth inhibition by the protein kinase antagonist UCN-01 inhuman breast carcinoma cells. Cancer Res. 1993;53:2081–2086. [PubMed] [Google Scholar]
- 8.Akinaga S., Nomura K., Gomi K., Okabe M. Effect of UCN-01, a selective inhibitor of protein kinase C, on the cell-cycle distribution of human epidermoind carcinoma, A431 cells. Cancer Chemother Pharmacol. 1994;33:273–280. doi: 10.1007/BF00685899. [DOI] [PubMed] [Google Scholar]
- 9.Kawakami K., Futami H., Takahara J., Yamaguchi K. UCN-01, 7 hydroxylstaurosporine, inhibits kinase activity of cyclin-dependent kinases and reduces the phosphorylation of the retinoblastoma susceptibility gene product in A549 human lung cancer cell line. Biochem Biophys Res Commun. 1996;219:778–783. doi: 10.1006/bbrc.1996.0310. [DOI] [PubMed] [Google Scholar]
- 10.Wille J.J., Scott R.E. Topography of the predifferentiation GD growth arrest state relative to other growth arrest states in the G1-phase of the cell cycle. J Cell Physiol. 1982;112:115–122. doi: 10.1002/jcp.1041120117. [DOI] [PubMed] [Google Scholar]
- 11.Carney D.N. Lung cancer-time to move on from chemotherapy. New Engl J Med. 2002;2:126–128. doi: 10.1056/NEJM200201103460211. [DOI] [PubMed] [Google Scholar]
- 12.Chang H.C., Hung W.C., Huang M.S., Hsu H.K. Extract from the leaves of Toona sinensis roemor exerts potent antiproliferative effect on human lung cancer cells. Am J Chin Med. 2002;30:307–314. doi: 10.1142/S0192415X02000223. [DOI] [PubMed] [Google Scholar]
- 13.Chang H.L., Hsu H.K., Su J.H. The fractionated Toona sinensis leaf extract induces apoptosis of human ovarian cancer cells and inhibits tumor growth in a murine xenograft model. Gynecol Oncol. 2006;102:309–314. doi: 10.1016/j.ygyno.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Yang H.L., Chang W.H., Chia Y.C. Toona sinensis extracts induces apoptosis via reactive oxygen species in human premyelocytic leukemia cells. Food Chem Toxicol. 2006;44:1978–1988. doi: 10.1016/j.fct.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 15.Yang C.J., Huang Y.J., Wang C.Y. Anti-proliferative and anti-tumorgenic activity of Toona sinensis leaf extracts in lung adenocarcinoma. J Med Food. 2010;155:305–314. doi: 10.1089/jmf.2009.1166. [DOI] [PubMed] [Google Scholar]
- 16.Wang P.H., Tsai M.J., Hsu C.Y., Wang C.Y., Hsu H.K., Weng C.F. Toona sinensis Roem (Meliaceae) leaf extract alleviates hyperglycemia via altering adipose glucose transporter 4. Food Chem Toxicol. 2008;46:2554–2560. doi: 10.1016/j.fct.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Yang C.J., Wang C.S., Hung J.Y. Pyrogallol induces G2-M arrest in human lung cancer cells and inhibits tumor growth in an animal model. Lung Cancer. 2009;66:162–168. doi: 10.1016/j.lungcan.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Zochbauer-Muller S., Gazdar A.F., Minna J.D. Molecular pathogenesis of lung cancer. Annu Rev Physiol. 2002;64:681–708. doi: 10.1146/annurev.physiol.64.081501.155828. [DOI] [PubMed] [Google Scholar]
- 19.Cho E.J., Yokozawa T., Rhyu D.Y., Kim H.Y., Shibahara N., Park J.C. The inhibitory effects of 12 medicinal plants and their component compounds on lipid peroxidation. Am J Chin Med. 2003;31:907–917. doi: 10.1142/S0192415X03001648. [DOI] [PubMed] [Google Scholar]
- 20.Gali H.U., Perchellet E.M., Klish D.S., Johnson J.M., Perchellet J.P. Antitumor-promoting activities of hydrolyzable tannins in mouse skin. Carcinogenesis. 1992;13:715–718. doi: 10.1093/carcin/13.4.715. [DOI] [PubMed] [Google Scholar]
- 21.Inoue M., Sakaguchi N., Isuzugawa K., Tani H., Ogihara Y. Role of reactive oxygen species in gallic acid-induced apoptosis. Biol Pharm Bull. 2000;23:1153–1157. doi: 10.1248/bpb.23.1153. [DOI] [PubMed] [Google Scholar]
- 22.Bailey A.E., Asplund R.O., Ali M.S. Isolation of methyl gallate as the antitumor principle of Acer saccharinum. J Nat Prod. 1986;49:1149–1150. doi: 10.1021/np50048a040. [DOI] [PubMed] [Google Scholar]
- 23.Zhang H., Wang X., Chen F., Androulakis X.M., Wargovich M.J. Anticancer activity of limonoid from Khaya senegalensis. Phytother Res. 2007;21:731–734. doi: 10.1002/ptr.2148. [DOI] [PubMed] [Google Scholar]
- 24.Valcic S., Timmermann B.N., Alberts D.S. Inhibitory effect of six green tea catechins and caffeine on the growth of four selected human tumor cell lines. Anticancer Drugs. 1996;7:461–468. doi: 10.1097/00001813-199606000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Buolamwini J.K. Cell cycle molecular targets in novel anticancer drug discovery. Curr. Pharm Des. 2000;6:379–392. doi: 10.2174/1381612003400948. [DOI] [PubMed] [Google Scholar]
- 26.Diehl J.A. Cycling to cancer with cyclin D1. Cancer Biol Ther. 2002;1:226–231. doi: 10.4161/cbt.72. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y.J., Jiang W., Chen C.J. Amplification and overexpression of cyclin D1 in human hepatocellular carcinoma. Biochem Biophys Res Commun. 1993;196:1010–1016. doi: 10.1006/bbrc.1993.2350. [DOI] [PubMed] [Google Scholar]
- 28.Tashiro E., Tsuchiya A., Imoto M. Functions of cyclin D1 as an oncogene and regulation of cyclin D1 expression. Cancer Sci. 2007;98:629–635. doi: 10.1111/j.1349-7006.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.K Ayed A., Adesina A. Prognostic significance of cyclin D1 expression in resected stage I, II non-small cell lung cancer in Arabs. Interact Cardiovasc Thorac Surg. 2006;5:47–51. doi: 10.1510/icvts.2005.120030. [DOI] [PubMed] [Google Scholar]
- 30.Tsuruo T., Nait M., Tomida A., Fujita N., Mashima T., Sakamoto H. Molecular targeting therapy of cancer: drug resistance, apoptosis and survival signal. Cancer Sci. 2003;94:15–21. doi: 10.1111/j.1349-7006.2003.tb01345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Otsuki Y., Li Z., Shibata M.A. Apoptotic detection methods — from morphology to gene. Prog Histochem Cytochem. 2003;38:275–339. doi: 10.1016/s0079-6336(03)80002-5. [DOI] [PubMed] [Google Scholar]
- 32.Boulares A.H., Yakovlev A.G., Ivanova V. Role of poly(ADP-ribose) polymerase (PARP) cleavage in apoptosis Caspase 3-resistant PARP mutant increases rates of apoptosis in transfected cells. J Biol Chem. 1999;274:22932–22940. doi: 10.1074/jbc.274.33.22932. [DOI] [PubMed] [Google Scholar]
- 33.D'Amours D., Sallmann F.R., Dixit V.M., Poirier G.G. Gain-of function of poly(ADP-ribose) polymerase-1 upon cleavage by apoptotic proteases: implications for apoptosis. J Cell Sci. 2001;114:3771–3778. doi: 10.1242/jcs.114.20.3771. [DOI] [PubMed] [Google Scholar]