Abstract
The objective of this communication is to introduce a conceptual framework for a study that applies a rigorous systems approach to rural disaster preparedness and planning. System Dynamics is a well-established computer-based simulation modeling methodology for analyzing complex social systems that are difficult to change and predict. This approach has been applied for decades to a wide variety of issues of healthcare and other types of service capacity and delivery, and more recently, to some issues of disaster planning and mitigation. The study will use the System Dynamics approach to create computer simulation models as “what-if” tools for disaster preparedness planners. We have recently applied the approach to the issue of hospital surge capacity, and have reached some preliminary conclusions – for example, on the question of where in the hospital to place supplementary nursing staff during a severe infectious disease outbreak—some of which we had not expected. Other hospital disaster preparedness issues well suited to System Dynamics analysis include sustaining employee competence and reducing turnover, coordination of medical care and public health resources, and hospital coordination with the wider community to address mass casualties. The approach may also be applied to preparedness issues for agencies other than hospitals, and could help to improve the interactions among all agencies represented in a community's local emergency planning committee.
The simulation models will support an evidence-based approach to rural disaster planning, helping to tie empirical data to decision-making. Disaster planners will be able to simulate a wide variety of scenarios, learn responses to each and develop principles or best practices that apply to a broad spectrum of disaster scenarios. These skills and insights would improve public health practice and be of particular use in the promotion of injury and disease prevention programs and practices.
Keywords: Disaster, Preparedness, Planning, Rural, Public health, System dynamics
Introduction
Disaster preparedness planning operates in a convoluted, confused, and fragmented environment (NRC, 2002; Rudman et al., 2003; Nash, 2003; Gilmore et al., 2003). It involves a variety of governmental and non-governmental agencies, including fire, emergency medical services (EMS), hospitals, police, and public health (Rudman et al., 2003), with overlapping jurisdictions and competing agendas and interests (Landesman, 2001; Heinrich, 2001; NRC, 2002). For example, the evidence-gathering requirements of law enforcement may potentially conflict with the patient confidentiality requirements of medical providers. Also, some agencies, such as local public health agencies and hospitals, may not be as involved in disaster planning efforts as they should be (IOM, 2002; NRC, 2002). The challenges of effective collaboration and communication among agencies are made even greater when the agencies are limited in resources and funding (IOM, 2002; Rudman et al., 2003), a situation often found in rural areas (ORHP, 2002).
The outbreaks of Severe Acute Respiratory Syndrome (SARS) and epidemic influenza continually emphasize the importance of the resources that public health and healthcare communities contribute to ensure for a disaster planning process that is dynamic, robust, and flexible. The challenge has become, however, how to ensure that all of the different community players work within one system to achieve common goals of community-wide preparedness.
Evidence-based research is needed to meet the growing challenges associated with disaster preparedness planning, including terrorism (NRC, 2002; IOM, 2002; Kirschenbaum, 2002). New and innovative research initiatives will provide emergency planners with the best possible data and methods to make the most effective and timely decisions.
In order to begin to build an evidence base for rural disaster preparedness research, this paper proposes a study that applies systems modeling and simulation to rural community disaster planning. Systems modeling would help to illustrate the complex web of causality that exists in disaster preparedness systems and if used correctly will have much to add to its evidence-based policymaking (Gunning-Schepers, 1999; Kirschenbaum, 2002).
In developing systems models as multifaceted and interwoven as the disaster preparedness system is, one must first select a logical and reasonable beginning point. After considering what would be required to model the entire system with all of its interacting organizations, we concluded that it would be most practical to first identify and define the internal challenges of single organizations, before considering multiple organizations simultaneously. Following this approach, we are now engaged in a study of a single hospital's surge capacity. The next step would be to look at how that hospital fits into a regional healthcare response, and subsequently into an overall community response. Ultimately, we foresee the possibility of developing a comprehensive model of community disaster planning that considers all major agencies and organizations.
The systems approach will identify the factors that can negatively impact and limit the planning process and address these concerns through computer-based simulations. These simulations will enable disaster planners to use a variety of scenarios to address different disasters and threat levels, and develop appropriate response and action plans that can be especially important to rural communities.
Rural disaster preparedness and planning
Disasters are broadly defined as emergencies of severity and magnitude resulting in deaths, injuries, illness, and or property damage that cannot be effectively managed by the application of routine procedures or resources (Landesman, 2001).
Natural disaster such as floods, earthquakes, and hurricanes pose a greater risk to populations than terrorist events (Landesman, 2001; PAHO, 2000; Levy and Sidel, 2003). Thus, many feel it is important for emergency planners to take a broad approach to disaster preparedness and plan for the consequences from both natural and man-made disasters (Landesman, 2001; Rudman et al., 2003; Gilmore et al., 2003). This “all-hazards” approach ensures that resources are effectively used in the dual capacity of responding to terrorist attacks, as well as enhancing emergency capabilities for addressing natural disasters (Rudman et al., 2003).
An “all-hazards” approach, however, does not come without its own inherent problems. One such problem is the need for, and coordination of, a mixed cadre of community personnel (e.g., fire, police, hospitals, public health, public works, etc.) to plan for and respond to a wide variety of disasters (Landesman, 2001; Rudman et al., 2003; ORHP, 2002; Heinrich, 2001). This community group may have already reached or exceeded their limitations.
In general, local health departments have less capacity, resources, funding, and numbers of adequately trained personnel (ORHP, 2002; NRC, 2002; Heinrich, 2001; Levy and Sidel, 2003); hospitals are reaching or possibly beyond their staffing and capacity limits (ORHP, 2002; Rudman et al., 2003; Rubin, 2004; JCAHO, 2003); and police and fire units/departments are under-funded and under-equipped (Rudman et al., 2003) across the nation. These challenges make it difficult for local agencies to balance daily needs against events that, they believe, have a small potential of occurring in their areas (ORHP, 2002; Levy and Sidel, 2003; GAO, 2003). Temper this with geographic constraints and weather extremes, infrastructure and technological barriers (MRHA, 2003; ORHP, 2002), and cultural uniqueness (ORHP, 2002), the problematic coordination of personnel from a wide-variety of agencies and jurisdictions makes rural disaster preparedness planning all the more difficult (Rudman et al., 2003; Heinrich, 2001).
Information and research needs for disaster planning
Lack of resources is commonly regarded as a major stumbling block in disaster preparedness. Although, during a critical time of need, most responders will get the job done with the resources they have (Rudman et al., 2003). However, these best efforts may be compromised and rendered less effective by a lack of clear and universal preparedness standards and guidelines (Rudman et al., 2003; Becker et al., 2003; Rubin, 2004; Gilmore et al., 2003). On the whole, the programs and regulations that do exist, although providing tools for planning, may lack systematic integration and consistency, effective means to address major problems or issues, and may be difficult to administer in practice (Rudman et al., 2003; Becker et al., 2003; Rubin, 2004).
The National Research Council's book, “Making the Nation Safer”, outlines an agenda for evidence-based research that creates a pool of data that can be translated into practice for catastrophic event planning (NRC, 2002). This agenda includes research on a systems perspective for homeland security, agent-based and system-dynamics modeling, modeling of interdependencies among critical infrastructures, and development of simulators and learning environments (NRC, 2002). Additionally, in their recent publication, “Biological Threats and Terrorism: Assessing the Science and Response Capabilities” (IOM, 2002), the Institute of Medicine suggests the need for research to determine effectiveness of preparedness plans.
Systems approaches and system dynamics
Complex public health problems have often proved resistant to simple solutions. The difficulty of dealing effectively with such problems has led to calls for systems approaches, including application of the theory of complex adaptive systems (IOM, 2001). However, there is no single definition of what constitutes a systems approach, a term which has been used variously to describe:
-
•
team-building facilitation and “learning organization” techniques that help multiple stakeholders work together more effectively (Senge, 1990);
-
•
so-called “qualitative modeling” or “soft operations research” or “systems thinking” methods that, through the use of cause-and-effect diagramming tools, help leaders diagnose problems and design better functioning organizations (Checkland, 1981; Wolstenholme and Coyle, 1983; Senge, 1990);
-
•
the development and use of computerized simulation models that can permit the analysis of complex problems not amenable to conventional statistical techniques (Meadows and Robinson, 1985; Sterman, 1988).
In the spectrum of systems approaches, System Dynamics (SD) is among the most quantitative and analytical, though it is also decidedly problem-focused and policy-oriented. SD applications involve the development of causal diagrams and computer simulation models that are unique to each problem setting. The types of problems to which SD has been applied are too numerous to mention. In the health field specifically, studies go back more than 30 years and include a variety of studies of healthcare delivery (Levin et al., 1976; Gardner, 1991; Hirsch and Immediato, 1999; Lane, 2000; Homer et al., 2004) and population health and epidemiology (Levin et al., 1975; Homer and St. Clair, 1991; Homer, 1993; Tengs et al., 2001). The causal diagrams of an SD application are often created by groups of diverse stakeholders and subject matter experts brought together for the purpose of establishing a common framework for policy analysis (Vennix, 1996). The simulation models themselves are typically constructed by specially trained experts who take the ideas and data of the stakeholder group and integrate them into an interlocking set of equations. A single SD model typically consists of a multitude of such equations, constructed and refined through an iterative process of scope selection, hypothesis generation, causal diagramming, quantification, reliability testing, and policy analysis (Sterman, 2000).
The SD modeling approach was developed by Jay W. Forrester in the mid-1950s and first propounded fully in his book “Industrial Dynamics” (Forrester, 1961), with some key additional insights presented in a later book entitled “Urban Dynamics” (Forrester, 1969). A central tenet of SD is that the difficult-to-change and difficult-to-anticipate behaviors of organizational and social systems are the result of ongoing accumulations and both balancing and reinforcing feedback mechanisms, which we can only hope to dissect with the aid of computer models. The unique contribution of SD to policy analysis is not the notion that feedback is important (an idea that has been around in various forms for centuries) but is the practical application of this fundamental concept in the form of models that can be tested, calibrated, and refined in a rigorous and scientific way (Forrester and Senge, 1980; Randers, 1980; Morecroft, 1985; Richardson, 1991; Homer, 1996; Sterman, 2000, Sterman, 2001).
The role of computer-based simulation in evidence-based research
How can simulation help satisfy the demand for evidence-based research? Commonly, in the social sciences, one thinks of research as involving experimentation done directly on the subject of interest. To obtain reliable results from such direct experimentation, a large enough sample is required with a minimum of uncontrolled variables. This sort of research may be readily performed in relatively simple systems, but becomes increasingly impractical and unreliable in systems with multiple interacting actors and “moving parts”. However, multiple actors and moving parts are precisely what one finds when considering the complexities of disaster planning. Aside from certain simple measures of capacity, and preparedness drills limited to a single organization or one possible disaster scenario out of many, direct research is of limited practical value in this context.
Computer simulations can be used to build the capacity of individuals and organizations to use the evidence they generate and put these findings into practice (Glasziou and Longbottom, 1999). Simulations provide the opportunity to test contingency plans under a variety of possible disaster scenarios (Kirschenbaum, 2002), and may allow staff to work through and gain valuable experience in emergency procedures under crisis conditions (NRC, 2002). Computer-based models and simulations, if used correctly, can provide evidence-based data that can support research, policy development, planning, and training (Gunning-Schepers, 1999), leading to the ultimate improvement of the community's health and well-being (Glasziou and Longbottom, 1999; Brownson et al., 1999).
Simulation can make a contribution to the understanding and evaluation of a complex system by offering a virtual world which mimics the real world, but which makes possible controlled experimentation in a low-cost, risk-free setting. The difficulty with this approach, not surprisingly, is that the virtual world is not identical to the real world, and may differ from it in some significant way that invalidates the simulation results. For this reason, the assumptions in a simulation model must be carefully vetted, and the model carefully tested for its accuracy and realism under all possible scenarios (Forrester and Senge, 1980; Morecroft, 1985; Homer, 1996). To the extent that the parameter values and other assumptions are uncertain, it is important to perform a full battery of sensitivity tests to determine the significance of such uncertainty to the experimental findings.
Typically, the findings will be sensitive to only a small fraction of the assumptions in a well-constructed simulation model, in which case it may be possible to go back and do more targeted data gathering or other research on those assumptions; or, at a minimum, to state findings that are conditional on those assumptions.
Applying system dynamics to rural disaster planning
How may SD be applied to rural disaster planning? There are many possible sub-issues to address and approaches that one might take. What we propose below is just one possible approach. Whatever the specific angle of attack, one should start with the existing literature.
Prior applications of SD that will help inform our work are in several related areas, including:
-
•
disaster planning and mitigation (Conrad et al., 2002; Cooke, 2003; Robards, 2001; Rudolph and Repenning, 2002; Hirsch, 2004);
-
•
service capacity and delivery in the healthcare system (Altinel and Ulas, 1996; Gardner, 1991; Hirsch and Immediato, 1999; Huang et al., 1995; Lane, 2000; Homer et al., 2004);
-
•
service capacity and delivery, more generally (Homer, 1999; Levin et al., 1976; Oliva, 2001; Repenning and Sterman, 2001);
-
•
human risk behaviors and epidemiology (Tengs et al., 2001; Homer and Milstein, 2002; Homer and St. Clair, 1991; Levin et al., 1975; Homer, 1996, Homer, 1993).
In thinking about an approach to applying SD to rural disaster planning, one should start by recognizing that the value of the technique will be best realized when it is applied to those issues in which the full ramifications of tactical and operations-level decisions are not well understood; also when such decisions may have significant unexpected or undesirable second- and third-order effects. Such non-trivial planning issues exist even within a single organization, like a hospital, and we suggest that may be the best place to demonstrate the value of SD. In fact, we recently completed an SD modeling project to study certain aspects of rural hospital disaster planning. In subsequent projects, we will address other hospital planning issues, and issues for other types of organizations and affecting the coordination of multiple organizations.
Phase 1
Our recent project focused on the issue of surge capacity for a single hospital in a remote rural area. Victims from a mass casualty event could overwhelm a hospital and create a backlog of patients who have not received care. One previous application of SD to questions of hospital capacity has suggested that a surge of emergency patients could lead indirectly to the cancellation of elective procedures, thereby disrupting schedules, affecting hospital productivity (thus, inadvertently reducing capacity as a second-order effect), and placing some patients at greater risk for sickness and death (Lane, 2000).
As part of any analysis of hospital surge capacity, one should evaluate the potential impact of different time patterns of demand. As stated in the American Hospital Association's report, “Hospital Preparedness for Mass Casualties” (AHA, 2000),
While some mass casualty incidents may follow the pattern of an intense, short-time peak of activity, others (e.g. bioterrorism incidents) will present the community and health system with rapidly increasing demands that plateau and have to be addressed for days or weeks.
One should also examine the impact on surge capacity of different approaches to triage. Quoting again from the American Hospital Association's report (AHA, 2000):
In the military, the triage concept is focused on making decisions to facilitate completing the mission. In the civilian community, triage has traditionally meant treating the most injured first. In a mass casualty incident, it may be necessary to use a triage approach more similar to the military's definition than the traditional civilian one. Moreover, depending upon the duration and pattern of the incident, the definition of triage may change over time.
Our surge capacity project considered a variety of disaster types, and traced the effects over time from triage to emergency care to inpatient care. The SD simulation model we developed focused on nurses, radiological technicians, and beds as key limiting resources in a rural hospital, the shortage of which could lead to bottlenecks and delays at different points along the pathways of diagnosis and care. This model – calibrated to represent a small rural hospital whose clinical leaders assisted us during the project – led to some preliminary conclusions, some of which we had not anticipated.
For example, the model suggests that, in the event of a large outbreak of a life-threatening infectious disease such as SARS, supplementing the acute ward nursing staff may do even more to reduce ER waiting room congestion (and related morbidity and mortality) than similar expansion of the ER nursing staff itself would. This is because the ER staff are responsible not only for patients currently receiving ER care, but also for patients following ER care awaiting admission to the acute wards. These post-ER patients may accumulate and become an increasing time sink for the ER staff if ward capacity is inadequate to admit them.
Phase 2
Moving beyond the initial focus on hospital surge capacity, we will next expand the initial SD model to address other concerns raised in the AHA report. Three that seem potentially appropriate for SD simulation analysis include the following (AHA, 2000):
-
•
Sustaining competence in disaster skills: Hospital employee turnover in many communities ranges from 16% to 20% annually. What is the feasibility of rapid re-education of new staff? Or, approaching the problem more preventively, what are the factors leading to turnover and can these be mitigated?
-
•
Coordination of medical care and public health resources: The traditional separation between the medical care community (e.g., hospitals, physicians, nursing homes) and the public health community needs to be bridged in preparation for mass casualty incidents. Mass casualties will provide more work than any organization itself can address. Coordination is the key, and the historic separation is a genuine disadvantage... Funds should be provided to a community-wide organization which is required to involve the community's political leadership, public safety services, public health services, hospitals, and community health centers.
-
•
Mass casualty preparedness as a community-wide effort: If the disaster is a mass casualty event, such as a major earthquake or biological terrorism, the patient load may overwhelm all of the hospitals, the offices of physicians, and the general resources of the community... Therefore, hospital preparedness should expand from planning within the context of a single hospital organization to planning by the hospital to become part of a community-wide initiative to address mass casualties (Hirsch 2004 describes an SD study taking this community-wide approach to mass casualty preparedness).
Phase 3
Beyond modeling hospital preparedness issues described in the AHA report, we are considering a multi-year program of simulation modeling that could ultimately involve many, if not all, of the various entities involved in rural disaster preparedness and planning. We envision developing models that could help disaster planners and emergency managers in a rural area visualize the consequences of many potential scenarios; use such models to test different approaches to disaster prevention or mitigation; and identify those that are most effective. Some of these models may, like the hospital surge capacity model, focus on a single agency. Others may focus on the interactions among agencies.
We propose that the client for this third phase of work be the entire local emergency planning committee (LEPC) of a community. The LEPC board consists of: elected and local officials, law enforcement, civil defense, firefighting, first aid, health, local environmental and transportation agencies, hospitals, broadcast and print media, community groups, and representatives of facilities subject to the emergency planning and community right-to-know requirements (LEPC/SERC Net, 2003; EPA, 2001) to ensure whole community involvement and input.
Initially established to “prepare and maintain” community emergency plans to address issues involved in the transportation, storage and manufacture of hazardous materials (EPA, 2001), many communities have begun to look to the LEPC to provide leadership in terrorism (EPA, 2001), emergency, and environmental hazard preparedness and planning (LEPC/SERC, 2003). Because of its broad-based membership, an LEPC is in a unique position to ensure that the concerns of the various stakeholders are heard and addressed (EPA, 2001; LEPC/SERC, 2003; CEPPO, 1998). Our hope is that SD modeling may be able to support the planning efforts of LEPCs by providing them with a common platform – a model or series of models – from which to view, evaluate, and coordinate their intersecting roles in disaster response.
Potential impact on rural disaster planning and public health
The daily role of public health in improving a population's health can be complex due to the structural and behavioral changes needed to do this (Waters and Doyle, 2003). It is also compounded by a decision-making process that often relies on anecdotal evidence and is driven by hot-topic, politically charged issues (Brownson, 1999). Add to these daily demands, the fiscal and personnel needs of preparing for, and responding to a disaster, and the need for robust decision support tools, including computer simulation models, becomes apparent.
Of course, no model can perfectly represent reality nor predict the future (De Geus, 1994). Nonetheless, a well-constructed computer model can provide a unique perspective into the unknown and can be used to help understand the cause-and-effect relationships that are at the heart of a complex issue (Gunning-Schepers, 1999).
Unlike static table-top exercises and cumbersome re-enactments, computer models can be dynamic, robust tools that can assist in training a cadre of emergency planners for many types of disasters involving a large number of variables, some previously encountered and some new. Models allow for flexibility of circumstances and can assist disaster planners, particularly those in rural areas, in determining better ways to address issues with fewer resources. In theory, planners should be able to more accurately plan for many possible contingencies, for resource and personnel allocation, and for effective collaboration with other agencies and jurisdictions. When used in conjunction with available empirical data and what is known through the medical literature, models and simulations can help provide the evidence base for nationally consistent standards and guidelines. The simulation-based approach is depicted in Fig. 1 , our revised version of Brownson's framework for evidence-based public health, where “quantify the issue” has been replaced with “model the issue and analyze options” (Brownson et al., 1999). In this figure, we also show how modeling is an iterative process in which policy options emerge through multiple rounds of model refinement (see the feedback link, “refine analysis”) (Homer, 1996; Sterman, 2000).
Fig. 1.
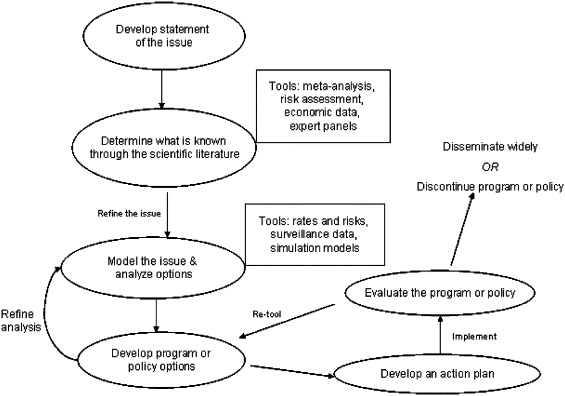
A sequential framework illustrating how simulation modeling can be used to provide an evidence-base for public health policy planning and decision-making. The figure is adapted from Brownson et al. (1999).
Modeling and simulations could focus the entire disaster preparedness process, but particularly public health practice less on individual crises and more on the broader notion “all-hazards” disaster risk and preparedness planning. This shift in approach could provide at minimum, the following advantages:
-
•
more balanced programs that address the concerns that some public health practitioners may have that disaster preparedness is a case of robbing Peter (e.g., chronic and communicable disease programs) to pay Paul (e.g., bioterrorism),
-
•
more sustainable programs, conceived in a broader way, and paid out of several funding sources that come from federal agencies and grants, and
-
•
healthier communities through greater emphasis on prevention and mitigation strategies, achieved largely through broad-based education and training programs.
Through these activities, communities would become more aware of possible risks and would work to minimize those risks or eliminate them altogether, thus creating communities that are likely to withstand any disaster they may happen to face. Computer simulation models could also assist public health in its newly prominent role in disaster and emergency planning. Epidemiological models have already proved their value in predicting epidemics outbreaks. Public health departments have now been given the additional challenge of facilitating emergency response and require tools that not only predict, but can also be useful, in the design of effective general procedures and contingency plans.
Also, public health agencies and hospitals must quickly learn to adapt and work within an environment that has, in the past, been non-collaborative and very segmented in duties and responsibilities. Within the “all-hazards” paradigm, however, collaboration and cross-cutting activities are expected and public health must now be aware of a multitude of disaster scenarios and be prepared to respond to them as a member of a response team.
With these expanded roles and responsibilities, local public health departments must consider the unique challenges and problems their community faces and assist in the creation of robust and dynamic disaster plans. Such considerations are particularly apparent in rural areas, where local emergency planners, including public health, must make the best use of limited resources. Computer models and simulations could allow local planners to develop templates or plans for the more effective allocation of resources as an event proceeds (Hupert et al., 2002). SD models and simulations, in particular, could provide robust and dynamic disaster planning and policy evaluation tools that supplement those already in place. In turn, these would support the core functions of public health: assessment, policy development, and evaluation (CDC, 2002).
Computer modeling and simulation can help to ensure that the planning and evaluation process is systematic, logical, and complete (Maheras et al., 1989), and not biased toward the re-use of past strategies that may or may not be the best ones possible.
Such an evidence-based approach will help support the disaster planning process anywhere, but will specifically assist rural emergency planners, including public health departments and hospitals, in designing plans that more effectively use resources, promote injury and disease prevention, reduce risk, and save lives.
Acknowledgements
We would like to thank Janet Williams, MD, former Director of the Center for Rural Emergency Medicine and Center for Medical Preparedness for her expertise and guidance in the conception of both this project and paper.
In addition, we would like to thank Dave Fulaytar, Senior Office Administrator, and Sanjoy Roy, Graduate Research Assistant, for their help in review and editing of this paper.
This paper was funded in part by a grant from The Rural Emergency Preparedness Program under the Health Resources and Services Administration of the U.S. Department of Health and Human Services. This grant program funds research and educational initiatives that enhance preparedness activities for rural healthcare and community providers.
References
- Altinel I.K., Ulas E. Simulation modeling for emergency bed requirement planning. Annals of Operational Research. 1996;67:183–210. [Google Scholar]
- AHA American Hospital Association . American Hospital Association; Washington, DC: 2000. Hospital preparedness for mass casualties: Final report, August 2000: Summary of an invitational forum convened on March 8–9, 2000. Available at: http://www.hospitalconnect.com/ahapolicyforum/resources/disaster.html. [Google Scholar]
- Becker S., Beitsch L., Bialek R., Fielding J., Gilchrist M., Hamburg M.A., Higginson G., Mahan C., Novick L., Plough A. Trust for America's Health; Washington, DC: 2003. Ready or not? Protecting the public's health in the age of bioterrorism. Available at: www.healthyamericans.org/state/bioterror/ [Google Scholar]
- Brownson R.C., Gurney J.G., Land G.H. Evidence-based decision making in public health. J. Public Health Manag. Pract. 1999;5:86–97. doi: 10.1097/00124784-199909000-00012. [DOI] [PubMed] [Google Scholar]
- CDC Centers for Disease Control and Prevention . U.S. Department of Health and Human Services; Atlanta: 2002. Exploring the foundations of a syndemic orientation in public health. Available at: http://www.cdc.gov/syndemics/pdfs/foundations.pdf. [Google Scholar]
- Checkland P.C. Wiley; United Kingdom: 1981. Systems Thinking, Systems Practice. [Google Scholar]
- CEPPO Chemical Emergency Preparedness and Prevention Office . U.S. Environmental Protection Agency; Washington, DC: 1998. The role of local emergency planning committees (LEPCs) and other local agencies in the risk mitigation management program (RMP) of Clean Air Act (CAA) Section 112 (r) – Subgroup #7 report. Available: http://epa.gov/swercepp/pubs/rmp-imp/lepc_rpt.html. [Google Scholar]
- Conrad, S.H., Brown, T., Beyeler, W., 2002. A dynamic simulation model of the effects of interdependent infrastructures on emergency service response. 20th International Conference of the System Dynamics Society (Albany, New York), Palermo, Italy.
- Cooke, D.L., 2003. Learning from Incidents. 21st International Conference of the System Dynamics Society (Albany, New York), New York.
- De Geus, A.P., 1994. Modeling to predict or to learn. In: Morecroft, J.D., Sterman, J.D. (Eds.), Modeling for Learning Organizations. Productivity Press, Portland, Oregon, pp. xiii–xvi.
- EPA U.S. Environmental Protection Agency . U.S. Environmental Protection Agency; Washington, DC: 2001. LEPCs and deliberate releases: Addressing terrorist activities in the local emergency plan (EPA 550-F-01-005) Available at: http://www.epa.gov/ceppo/factsheets/lepcct.pdf. [Google Scholar]
- Forrester J.W. MIT Press; Cambridge, MA: 1961. Industrial Dynamics. [Google Scholar]
- Forrester J.W. MIT Press; Cambridge, MA: 1969. Urban Dynamics. [Google Scholar]
- Forrester J.W., Senge P.M. Tests for building confidence in system dynamics models. In: Legasto A.A. Jr., Forrester J.W., Lyneis J.M., editors. vol. 14. North-Holland; New York: 1980. pp. 209–228. (System Dynamics: TIMS Studies in the Management Sciences). [Google Scholar]
- GAO General Accounting Office: Bioterrorism . General Accounting Office; Washington, DC: 2003. Preparedness varied across state and local jurisdictions (GAO-03-373) Available at: http://www.gao.gov/new.items/d03373.pdf. [Google Scholar]
- Gardner B. Managing hospital emergency capacity. The Systems Thinker. 1991;2:7–9. [Google Scholar]
- Gilmore J.S., Foresman G., Freeman M., Garrison W., Gordon E.M., Greenleaf J. The RAND Corporation; Arlington: 2003. Forging America's new normalcy: Securing our homeland, preserving our liberty. The fifth annual report to the President and Congress of the Advisory Panel to Assess Domestic Response Capabilities for Terrorism Involving Weapons of Mass Destruction. Available at: http://www.rand.org/nsrd/terrpanel/volume_v/volume_v.pdf. [Google Scholar]
- Glasziou P., Longbottom H. Evidence-based public health practice. Aust. N. Z. J. Public Health. 1999;23:436–440. doi: 10.1111/j.1467-842x.1999.tb01291.x. [DOI] [PubMed] [Google Scholar]
- Gunning-Schepers L.J. Models: Instruments for evidence based policy. J. Epidemiol. Community Health. 1999;53:263. doi: 10.1136/jech.53.5.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich J. General Accounting Office; Washington DC: 2001. Bioterrorism: Public health and medical preparedness (GAO-02-141T) Available at: http://www.gao.gov/new.items/d02141t.pdf. [Google Scholar]
- Hirsch G., Immediato C.S. Microworlds and generic structures as resources for integrating care and improving health. Syst. Dyn. Rev. 1999;15:315–330. [Google Scholar]
- Homer J.B. A system dynamics model of national cocaine prevalence. Syst. Dyn. Rev. 1993;9:49–78. [Google Scholar]
- Homer J.B. Why we iterate: Scientific modeling in theory and practice. Syst. Dyn. Rev. 1996;12:1–19. [Google Scholar]
- Homer J.B. Macro- and micro-modeling of field service dynamics. Syst. Dyn. Rev. 1999;15:139–162. [Google Scholar]
- Homer J.B., St. Clair C.L. A model of HIV transmission through needle sharing. Interfaces. 1991;21:26–49. [Google Scholar]
- Homer, J.B., Milstein, B., 2002. Communities with multiple afflictions: A system dynamics approach to the study and prevention of syndemics. 20th International Conference of the System Dynamics Society (Albany, New York), Palermo, Italy.
- Homer, J.B., Hirsch, G., Minniti, M., Pierson, M., 2004. Models for collaboration: How system dynamics helped a community organize cost-effective care for chronic illness. System Dynamics Review, in press.
- Huang X.M., Taylor C., Stewart I. Computer simulation of an A&E department: Towards shorter waiting in an accident and emergency department. OR Insight. 1995;8:18–23. [Google Scholar]
- Hupert N., Mushlin A.I., Callahan M.A. Modeling the public health response to bioterrorism: Using discrete event simulation to design antibiotic distribution centers. Med. Decis. Making. 2002;22(5 Suppl.):S17–S25. doi: 10.1177/027298902237709. [DOI] [PubMed] [Google Scholar]
- IOM Institute of Medicine . National Academy Press; Washington, DC: 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. [PubMed] [Google Scholar]
- IOM Institute of Medicine, 2002. Biological Threats and Terrorism: Assessing the Science and Response Capabilities. In: Knobler, S.I., Mahmoud, A.A., Pray, L.A. (Eds.), National Academy Press, Washington, DC. [PubMed]
- JCAHO Joint Commission on Accreditation of Healthcare Organizations . Joint Commission on Accreditation of Healthcare Organizations; Washington, DC: 2003. Health care at the crossroads: Strategies for creating and sustaining community-wide emergency preparedness systems. Available at: http://www.jcaho.org/about+us/public+policy+initiatives/emergency+preparedness.pdf. [Google Scholar]
- Kirschenbaum A. Disaster preparedness: A conceptual and empirical reevaluation. Int. J. Mass Emergencies Disasters. 2002;20:5–28. [Google Scholar]
- Landesman L.Y. American Public Health Association; Washington, DC: 2001. Public Health Management of Disasters: The Practice Guide. [Google Scholar]
- Lane D.C. Looking in the wrong place for healthcare improvements: A system dynamics study of an accident and emergency department. J. Oper. Res. Soc. 2000;51:518. [Google Scholar]
- LEPC/SERC Net., 2003. What are LEPCs? Accessed February 15, at: http://www.rtk.net/lepc/webpage/info.html.
- Levin G., Roberts E.B., Hirsch G.B. Ballinger; Cambridge, MA: 1975. The Persistent Poppy. [Google Scholar]
- Levin G., Roberts E.B., Hirsch G.B., Kligler D.S., Wilder J.F., Roberts N. Ballinger; Cambridge, MA: 1976. The Dynamics of Human Service Delivery. [Google Scholar]
- Levy B.S., Sidel V.W. Challenges that terrorism poses to public health. In: Levy B., Sidel V., editors. Terrorism and Public Health. Oxford University Press; Oxford: 2003. pp. 3–18. [Google Scholar]
- Maheras S.J., Tarapore P.S., Borak T.B., Clark G.M. Use of simulation model in occupational dose assessment at a high-level radioactive waste repository. Health Phys. 1989;57:107–116. doi: 10.1097/00004032-198907000-00013. [DOI] [PubMed] [Google Scholar]
- Meadows D.H., Robinson J.M. Wiley; Chichester, England: 1985. The Electronic Oracle: Computer Models and Social Decisions. [Google Scholar]
- Morecroft J.D.W. Rationality in the analysis of behavioral simulation models. Manage. Sci. 1985;31:900–916. [Google Scholar]
- MRHA Michigan Rural Health Association . Michigan Rural Health Association; East Lansing: 2003. The rural implication of emergency preparedness planning. Available at: http://www.miruralhealth.org/files/executive%20paper.pdf. [Google Scholar]
- Nash D.B. Being ready for an insidious threat. Managed Care. 2003;12(11 Suppl):1. [Google Scholar]
- NRC National Research Council . National Academy Press; Washington, DC: 2002. Making the nation safer: The role of technology and science in countering terrorism. Available online at: http://www.nap.edu/catalog/10415.html. [Google Scholar]
- ORHP Office of Rural Health Policy . US Department of Health and Human Services; Rockville: 2002. Rural communities and emergency preparedness. Available at: ftp://ftp.hrsa.gov/ruralhealth/RuralPreparedness.pdf. [Google Scholar]
- Oliva R. Tradeoffs in responses to work pressure in the service industry. Calif. Manage. Rev. 2001;43:26–43. [Google Scholar]
- PAHO Pan American Health Organization . PAHO; Washington, DC: 2000. Natural Disasters: Protecting the Public's Health. [Google Scholar]
- Randers J., editor. Elements of the System Dynamics Method. MIT Press; Cambridge, MA: 1980. [Google Scholar]
- Repenning N.P., Sterman J.D. Nobody ever gets credit for fixing problems that never happened: creating and sustaining process improvement. Calif. Manage. Rev. 2001;43:64–885. [Google Scholar]
- Richardson G.P. University of Pennsylvania Press; Philadelphia: 1991. Feedback Thought in Social Science and Systems Theory. [Google Scholar]
- Robards K.J. Earthquake mitigation decision making in local government: an application of system dynamics modeling. DAI. 2001;62:243. [Google Scholar]
- Rubin, J.N., 2004. Recurring pitfalls in hospital preparedness and response. Journal of Homeland Security. Available at: http://www.homelandsecurity.org/journal/Articles/rubin.html.
- Rudman W.B., Clarke R.A., Metzl J.F. Council on Foreign Relations; New York: 2003. Emergency responders: Drastically Underfunded, Dangerously Unprepared. Available at: http://www.cfr.org/pdf/Responders_TF.pdf. [Google Scholar]
- Rudolph J.W., Repenning N.P. Disaster dynamics: understanding the role of quantity in organizational collapse. Admin. Sci. Quat. 2002;47:1–30. [Google Scholar]
- Senge P.M. Doubleday; New York: 1990. The Fifth Discipline: The Art & Practice of the Learning Organization. [Google Scholar]
- Sterman J.D. A skeptic's guide to computer models. In: Grant L., editor. Foresight and National Decisions. University Press of America; Lanham, Maryland: 1988. [Google Scholar]
- Sterman J.D. Irwin/McGraw-Hill; Boston: 2000. Business Dynamics: Systems Thinking and Modeling for a Complex World. [Google Scholar]
- Sterman J.D. System dynamics modeling: tools for learning in a complex world. Calif. Manage. Rev. 2001;43:8–25. [Google Scholar]
- Tengs T.O., Osgood N.D., Lin T.H. Public health impact of changes in smoking behavior: Results from the tobacco policy model. Med. Care. 2001;10:1131–1141. doi: 10.1097/00005650-200110000-00010. [DOI] [PubMed] [Google Scholar]
- Vennix J.A.M. Wiley; Chichester, England: 1996. Group Model-building: Facilitating Team Learning using System Dynamics. [Google Scholar]
- Waters E., Doyle J. Evidence-based public health: cochrane update. J. Public Health Med. 2003;25:72–75. doi: 10.1093/pubmed/fdg015. [DOI] [PubMed] [Google Scholar]
- Wolstenholme E.F., Coyle R.G. The development of system dynamics as a methodology for system description and qualitative analysis. J. Oper. Res. Soc. 1983;7:569–581. [Google Scholar]


