CASE EXAMPLE
A newborn, from a heroin-addicted mother, is being treated for narcotic withdrawal with diluted tincture of opium. On hospital discharge, the mother is given a prescription for “DTO” and takes the prescription to the pharmacy to be filled. The prescription lacks an age or weight. The pharmacist interprets “DTO” as “deodorized tincture of opium” that is 25 times stronger than the intended “diluted tincture of opium.” The mother administers the prescription as ordered. Twenty-four hours later, the child is apneic and presents to the emergency department.
This case highlights the threat ambulatory medical mistakes pose to children. Although the majority of work in patient safety to date has focused on adult and inpatient care, there is growing awareness that ambulatory care is as paramount as inpatient care given the large volume of ambulatory care received by children. In this article, we will lay the groundwork for a patient safety research agenda for pediatric ambulatory care. In taking this first step, we will rely on and present an overview of patient safety in general, discuss issues related to pediatric patient safety, present an overview of what is known regarding ambulatory patient safety based on a systematic literature review, and finally present a framework for improving pediatric patient safety in the ambulatory setting relying on frameworks developed in other clinically relevant areas.
THE BIG PICTURE OF PATIENT SAFETY
The Institute of Medicine (IOM) report, To Err Is Human, released in 1999, shined a spotlight on preventable medical errors.1 The subsequent IOM report, Crossing the Quality Chasm: A New Health System for the 21st Century, released in 2001, reinforced that patient safety is an important goal of our nation's health care system.2 In conjunction with these reports, numerous entities have begun to tackle the patient safety problem from federal and state governments to private institutions and organizations.
Coincident with these reports, the lead federal agency for patient safety, the Agency for Healthcare Research and Quality (AHRQ) of the Department of Health and Human Services launched an initial $50 million initiative in patient safety research in 2001.3 In preparation for this initiative, AHRQ in conjunction with the federal Quality Interagency Coordination Task Force held a National Summit on Medical Errors and Patient Safety Research on September 11, 2000.4 The summit brought together users of research, funders of research, and researchers to examine needs and work collectively to develop a national research agenda on patient safety.5 The agenda they developed, which applies broadly to all types of patients and providers, comprised the following research priorities: epidemiology of errors, infrastructure to improve patient safety, role of information systems, understanding which interventions should be adopted, adoption issues, dissemination, and a special focus on transition of care issues as they relate to patient safety. But where does one begin on this far-reaching list of general priorities?
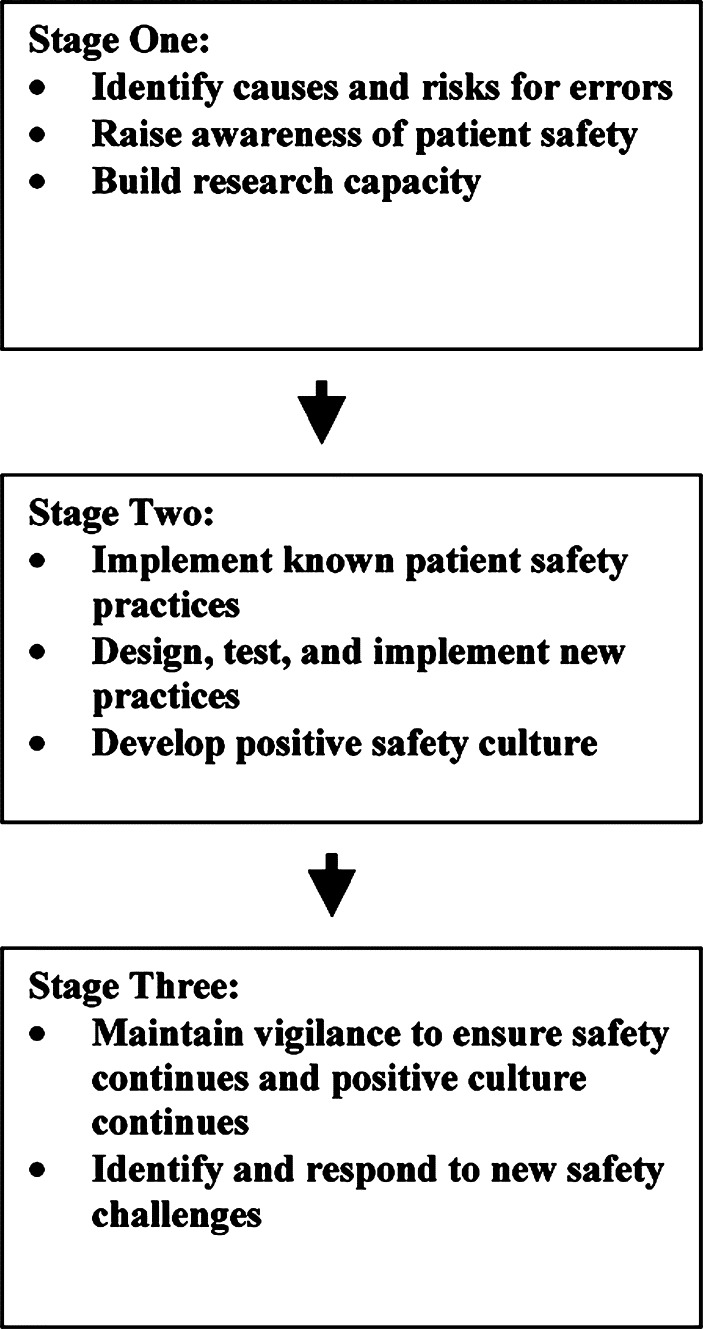
At this summit, Dr John Eisenberg, former director of AHRQ, likened the problem of medical errors to an epidemic and noted that we are currently in the first stages of understanding this epidemic. The intent of this model and its applicability to patient safety efforts lies in the fact that the field of medicine does not come from a tradition of openly discussing and collecting information on safety events. This leaves present-day groundswells to improve patient safety subject to a trap of “not being able to fix what one does not know is broken.” The epidemic notion, therefore, looks at errors not as a new phenomenon, like severe acute respiratory syndrome, but instead an “apparent” new phenomenon based on the fact that the field of medicine is just coming on board with the idea of systematic reporting and collecting of error event data. Logistically this epidemic model and the relative paucity of information and research on medical errors lend themselves to an overarching long-term plan for safety solutions that follows the traditional stages of action for epidemic response as shown the Figure .6 This model helps prioritize among the list of research agenda topics developed at the national summit. As we develop a specific agenda for patient safety for pediatric ambulatory care, we will refer back to this overarching epidemic model given the universality of its applicability.
AMBULATORY PATIENT SAFETY AND PEDIATRIC PATIENT SAFETY
The majority of current research, knowledge, and improvement efforts in patient safety are primarily focused on inpatient settings and adult patients. To begin to set an agenda specific for ambulatory care, the Medical Group Management Association Center for Research, with support from AHRQ and the Centers for Medicare and Medicaid Services and with assistance from the Partnership for Patient Safety held a multidisciplinary conference in late 2000.7 The results of this conference were twofold: 1) there is inadequate knowledge of the ambulatory care sector that severely limits our ability to understand and manage safety risks to patients; and 2) a research agenda tailored for ambulatory care.8, 9 This agenda, in line with the global patient safety agenda determined at the National Summit on Medical Errors and Patient Safety Research, can be summarized as follows:
-
•
Identify and pilot test methods to conduct a large-scale study of the epidemiology of safety in ambulatory care.
Conduct focused research examining and evaluating claim and incident data from liability insurers and determine how the rates and patterns of incidents and injuries from these sources would be expected to differ from true rates and patterns; in addition, conduct focused research on the value of case studies and focused research evaluating interventions by liability insurers.
Conduct research that builds on the experiences from risk management activities of liability insurers, provider organizations, and integrated health care systems to understand the risks and injuries in ambulatory care and identify target areas for additional focus.
Enhance research that examines the potential of administrative data for ambulatory safety research and the appropriate methods to use these data.
Explore research on the perspectives of patients and families on ambulatory care and characterize the information they can provide about safety in this setting; in addition, conduct research on the reliability and validity of that information, methods to ensure high rates of unbiased responses, and study designs to yield population-based estimates from this information.
This research agenda goes far to translate global patient safety issues into the nuances of how we begin to examine patient safety in ambulatory care. For practical implementation purposes, particularly for children, however, clearer distillation of the issues is needed.
Children's health care has not to date been a substantial focus of the current research in ambulatory care safety, let alone the overall patient safety efforts underway in this nation. To those health care providers immersed in children's health care, the rationale behind the need for targeted pediatric patient safety research is readily apparent. Children are unique in many ways related to the four Ds: developmental change, dependency on adults, different disease epidemiology, and demographic characteristics.10 Examples of how this plays out for children include the unique situation of weight-based dosing, compared with adults, whereby children can be subject to 10- to 100-fold dosing errors since children actually can come in size ranges from 300 grams to over 300 pounds, and the unique medical events such as birth.11, 12 In addition, children's health care providers are frequently separate in training and both divisional and departmental academic homes from health care providers for adults. Because both patient and provider factors combine in patient safety events, it is critical to understand how the obvious differences in pediatric patients and pediatric providers interplay with patient safety.
The overarching themes in the research agenda from the National Summit on Medical Errors and Patient Safety Research, the epidemic model of a long-term plan for patient safety, and the multidisciplinary conference on research for ambulatory care all are salient to children's health care but need tendering to make the issues and priorities clear. Collectively, these agendas and models can be synthesized and tailored. This article provides this synthesis and tailoring to pediatric patient safety in the ambulatory care setting.
PEDIATRIC PATIENT SAFETY IN AMBULATORY CARE: WHAT DO WE KNOW?
Definitions
Any discussion of patient safety and ambulatory care requires a level playing field in terms of definitional understandings and assumptions. Consistent with the IOM report To Err Is Human, patient safety in this article is defined as freedom from accidental injury because of medical care, which translates to medical errors. Such medical errors can be further defined using the definition from the federal response to To Err Is Human outlined in the report entitled Doing What Counts, as “the failure of a planned action to be completed as intended or of use of a wrong plan to achieve an aim. Errors can include problems in practice, products, procedures, and systems.”1, 13 This definition excludes acts that did not achieve their desired outcomes (as long as that was not the result of negligence), outcomes caused by the intrinsic properties of the underlying illness or additional patient comorbidities, and outcomes known to be risks of specific procedures. Inherent in this definition is the idea that the causes of the vast majority of patient safety events are not sole individuals but instead are embedded in the organizations, processes, and systems within which individuals receive care. Perhaps more so than inpatient care, ambulatory care and the resultant patient safety issues depend heavily on patients, families, providers, and organizations, and how these interact. This definition of patient safety applies broadly to all ages.
Although safety is undoubtedly a subset of quality, there is uncertainty and variability about the degree to which safety intersects with the broader issues of quality of care, in particular, whether failure to adhere to evidence-based therapies (effectiveness) should be classified as a safety or a quality problem. For example, some may argue that overprescribing antibiotics for otitis media in children is a safety issue both at a public health level because of bacterial resistance and a patient level because of side effects, whereas others may see this solely as a quality-of-care issue for the most part. This article does not attempt to draw the line between safety and quality but instead will keep a broad perspective of safety to include events that may have exposed a patient to an unnecessary risk.
Comparably, we must all appreciate what the term ambulatory care entails. In brief, ambulatory care encompasses a wide array of settings: physician offices, emergency rooms, hospital outpatient departments, home health agencies, community health centers, school-based health centers, urgent care centers, chemotherapy and radiation therapy centers, dialysis centers, diagnostic imaging centers, outpatient surgery centers, occupational health centers, mental health centers, dental centers, and other settings.8 Although inpatient care is typically more technologically and clinically complex, ambulatory care is logistically more complex, often with less elaborate infrastructure for managing care. This translates to encounters that need substantial communication and coordination, with many hand offs and transitions. The ultimate management of ambulatory care is often difficult for patients and families, not to mention that ambulatory practices often have not kept up with the rapid development of medical science and diagnostic, therapeutic, and technologic capabilities.9
Equally as important as these different settings of care is the realization that there exists multiple hand offs of patients between and within these various care settings. Providers see other colleagues' patients when needed, and providers in different ambulatory settings refer their patients to other providers in different ambulatory areas. Transitions or hand offs in care are ripe for patient safety events because of the brevity of communications between providers and between providers and families. In the emergency department setting, these transitions have been identified as potential risks for safety events.14, 15 Given the dependency of children, transitions of care takes on additional meaning when one also considers transitions of caregivers among parents, guardians, grandparents, and more distant relatives.
Literature Review
Published literature on patient safety in ambulatory care is scarce for both adult and pediatric patients. For this review we searched for published articles using the MESH terms medical errors, children, primary health care, and ambulatory care. Elder and Dovey16 published one of the most recent and comprehensive works. This study entails a systematic review and synthesis of English-language medical literature from 1965 through March 2001. In addition, this work included searches of bibliographies and web sites from patient safety and primary care organizations for unpublished reports and presentations as well as reference reviews of all identified articles. Given that this piece did not exclude children's health care, this review is very salient to our efforts to identify what is known on pediatric ambulatory patient safety. This effort identified only 7 studies, which were all primarily descriptive of the types and causes of medical error incidents.17, 18, 19, 20, 21, 22, 23 None of these studies involved primarily pediatric patients. Results of this work were synthesized into a classification scheme for preventable adverse events and process errors in primary care, which will be detailed later in this article.
In addition to these articles, other studies systematically identified on ambulatory care and patient safety can largely be described as either thought pieces or additional condition or setting specific descriptive studies that are not easily identified using search terms focused on medical errors or patient safety. For example, several thought-piece articles have been recently published talking about the broad picture of quality and safety in emergency departments in general, for children with special health care needs, and for medicine management in primary care.24, 25, 26, 27, 28, 29, 30 Taking random examples of articles one can find but not by systematic searches looking for medical errors, there are pieces that discuss the issues around conscious sedation for dentistry, examples of deaths from lipoplasty, concerns about diagnostic accuracy of pediatric echocardiograms performed in adult laboratories, and research on safe pediatric outpatient sedation.31, 32, 33, 34, 35 Likewise, the substantial body of literature on appropriate therapy and diagnosis of otitis media could also be considered a patient safety concern. Given that many articles like these do not specifically use terms such as medical errors or patient safety, a systematic identification and synthesis of these is not realistically feasible as we try to establish a research agenda for pediatric ambulatory care. Perhaps best known to most pediatricians is the wealth of information on immunizations. The clear take-home message from this body of work is that one cannot rely on vigilance and memory alone to ensure high quality care. As one recent review highlights, simplification with reminder systems and use of electronic information has been able to dramatically improve appropriate and maximal use of immunizations.36 Although it is easy to speculate on the lessons learned here and how they can apply to broader safety issues beyond immunizations, the reality is that this leap to global issues of safety in ambulatory care is not well examined in the literature.
Because one of the few recent articles identified and targeted safety, there was a recently published article specifically focused on ambulatory pediatric patient safety from the perspective of language barriers and resultant medical errors because of errors in medical interpretation to Spanish.37
Given this finding of little literature that could be systematically found regarding pediatric ambulatory patient safety, we broadened our searches to include adult health care and inpatient health care because it is likely that at least some patient safety findings in these areas will be relevant to pediatric ambulatory care. For example, one recent work on adult ambulatory patients suggests that medication errors are common. Because the rates of inpatient medication among adults and children are similar and alarmingly high, the high rates of medication errors in adult ambulatory patients should raise concern among pediatricians.11, 38, 39 In a recent study of Medicare enrollees,40 the overall rate of adverse drug events in adult ambulatory patients was 50/1000 person-years, with 14/1000 person-years considered preventable. Moreover, 38% of the adverse drug events were considered serious, life threatening, or fatal. These data highlight the need for similar studies in pediatrics. Although not in the peer-reviewed literature, recent efforts by the Institute for Safe Medication Practices have led to a new monthly publication to share lessons learned in medication safety for outpatient settings.41
Stepping for a moment to inpatient pediatric care, some research on patient safety likely translates to real issues for pediatric ambulatory care. Although this pool of literature is larger, it is still relatively scarce for broad perspectives on inpatient errors as opposed to condition-specific inpatient errors. Recent work has shown us that children in inpatient settings experience high rates of medication errors because of all the unique vulnerabilities of children, compared with adults.11, 38 This more than likely is applicable to pediatric ambulatory care because of the high rate of medication prescribing in ambulatory settings. At least 2 studies are currently underway to examine the prevalence of ambulatory medication errors for children.42, 43 Beyond medication errors, several recent studies highlight the fact that children do experience other inpatient errors and that the rates are unacceptably high.44, 45 If nothing else, these studies compel us to proactively tackle patient safety in pediatric ambulatory care because it is most likely that these findings also hold true in this setting of care. Perhaps most poignantly in terms of inpatient care for children was the recent experience involving heart surgery on children at the Bristol Royal Infirmary between 1984 and 1995.46 A recent summary document on this experience47 details how to take the lessons learned and turn them into the reality of safer patient care by vital activities such as actively involving patients in their own care, a lesson clearly applicable to ambulatory care.
Last, there is a fair amount of literature bridging both inpatient and outpatient care and both adult and pediatric patients concerning the roles of information technology and medication safety.48, 49, 50 This work is summarized in an accompanying piece in this issue by Johnson. Ongoing work on this topic will likely facilitate the wide-scale adoption of this solution for medication errors.
PEDIATRIC PATIENT SAFETY IN AMBULATORY CARE: WHAT DO WE NEED TO KNOW?
Taking what we know about patient safety as it directly or indirectly relates to pediatric ambulatory care and the previously discussed broad models and research agendas in patient safety, what can we distill as target areas to begin actively exploring and improving safety in pediatric ambulatory care? This answer has good groundwork in place from the work already done by the 2000 meeting to create a research agenda in ambulatory patient safety, which primarily focused on the science and epidemiology of errors, and in the agendas set forth in family practice and emergency medicine with regard to classification schemes and curriculums for patient safety.18, 27 More importantly, going back to the epidemic idea of patient safety, a natural extension from this involves a 3-tiered approach to research on safety comparable with how one tackles true epidemics. These 3 steps involve first understanding the basics about the environment in which the epidemic is taking place (knowing the culture of safety in ambulatory care); second, identifying the prevalence of the epidemic (knowing the magnitude, risks, and types of errors seen in ambulatory care); and last, identifying strategies to curb the spread of the epidemic (knowing successful solutions to remedy safety concerns). As the literature review and the other broader research agendas attest, the bulk of work to date has been primarily focused on the most straightforward of these tiers to examine, namely the identification of the magnitude, risks, and types of errors seen.
CULTURE AND THE SCIENCE OF SAFETY
One of the paramount needs of the ambulatory pediatric patient safety initiative is an understanding of what is current patient and provider awareness, acknowledgment, and acceptance of the reality of medical errors. Several recent works in this area found that the public and practicing physicians do not have a sense of urgency about medical errors, unlike many national organizations.51, 52 As these studies conclude, one of the largest hurdles in improving safety will be convincing providers and patients that efforts will be successful. Any efforts to change practice will need the support of the providers and patients who will be much more likely to be actively involved and ensure success if they believe true and lasting improvements will result. Flowing directly from this is a need to be able to measure the culture and strategies to improve the culture. There is a growing literature base on how to assess and change an organization's safety culture.53, 54, 55, 56 This pool of literature has several common and recurrent themes: understanding of errors as systems problems, open and full reporting of all safety events, analysis of near-miss safety events, employee education on patient safety, and management tools to promote safety. It is likely very safe to say that these issues are universal for both care of adults and children. Different medical disciplines have their own cultures and acceptable behavior. How do providers trained to take care of children stand with respect to other peers in terms of awareness, acknowledgment, and acceptance of the reality of medical errors? Where do they stand in terms of ability and success at instituting changes meant to improve safety and their ability to critically evaluate these changes? Each ambulatory care setting brings with it a unique niche in which to date little is known about how patient safety factors into everyday discussions and care practices.
Directly linked to this is a need to have a baseline understanding of the science of safety. To collectively think about and remedy medical errors, all providers need to understand basic definitions of errors and models for the analysis of errors in hopes of inducing systems changes. For example, providers need to be aware of decision-making processes that predispose one to errors such as concepts of sensitivity and specificity of tests, evidence-based medicine or a lack thereof, and the notion of inherent cognitive biases in care such as anchoring and prevalence bias. Comparably, we know little in terms of how working conditions affect ambulatory care in arenas such as sleep deprivation, visit time constraints, and patient-provider and provider-provider feedback and exchanges both proximal and distal to actual face-to-face visits to ambulatory care.
TYPES OF ERRORS
The second step in thinking of a research framework for ambulatory patient safety involves an understanding of the types of errors seen and their risk factors. Two different but interrelated classification schemas exist to categorize the types of errors likely to occur in ambulatory care.16 Within each of these schemas there exists a multitude of research questions relevant to pediatric ambulatory care. Although impossible to list each possible question, examples of types of research questions generated by these schemas are included. These sample questions are not intended to represent any prioritization of specific issues within pediatric ambulatory care patient safety research, but instead are included to only illustrate the types of concepts included in each type of error.
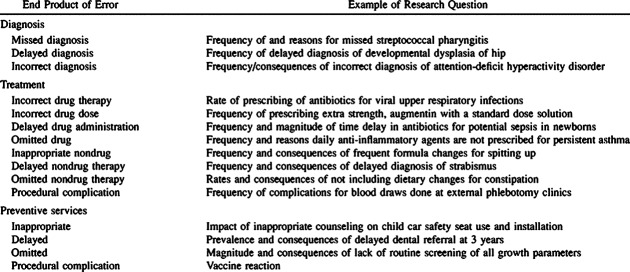
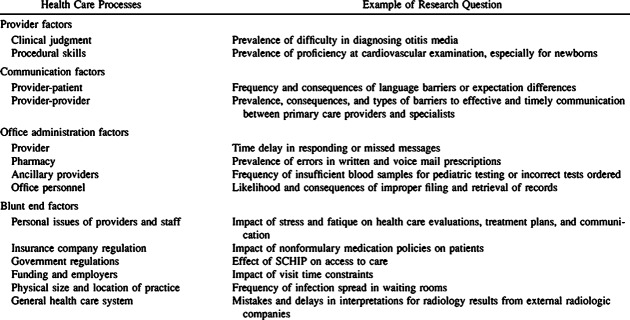
First, one can think about the end product of the error. Issues here, with pediatric-specific examples, can be summarized as indicated in Table 1 . Alternatively, one can think about the processes involved that led to an error as a classification scheme, as indicated in Table 2 .
Table 1.
Classification by the End Product of Error
Table 2.
Classification by the Processes of Health Care
Overarching both of these schemas and extending into inpatient care as well is the related need for error reporting systems. The current approach to patient safety is fragmented, often failing to identify and communicate errors to relevant parties. True to form for being in stage 1 of this epidemic, we need to focus our search for baseline data on our performance in ambulatory care with respect to medical errors. It was not by chance that the substantial portion of AHRQ's $50 million initiative in patient safety was devoted to reporting systems.57 To improve patient safety, we need to identify what is broken and then fix it.
PATIENT SAFETY SOLUTIONS
The inextricable third leg of the patient safety initiative, in addition to having a positive safety culture and a system to identify errors, is the need for solutions. Although the literature is not brimming with proven strategies in ambulatory care, substantial work does exist when one looks more broadly to other health care settings for guidance. Perhaps the largest synthesis of these solutions came from AHRQ as the evidence report entitled Making Health Care Safer: A Critical Analysis of Patient Safety Practices.58 Although the primary focus of this work related to in-hospital care, it is likely that some successful strategies from the inpatient arena will translate to outpatient care. It is also important to point out that little of this evidence comes from studies involving children and their health care providers. Although this coupled with the paucity of proven solutions in ambulatory care clearly is a significant gap and hurdle to improving safety in pediatric ambulatory care, some types of safety solutions are very likely to be generically applicable regardless of clinical setting or population. One of the most studied interventions that are likely to be generically applicable involve use of information technology. The research world is quickly accruing studies showing the benefits of information technology. For example, several evaluations of e-prescribing work have found that it creates substantial savings because of increased efficiency ($1.15 per practice member per month in pharmacy costs, $12 000 in practice savings per year because of increased operational efficiency, 30% reduction in physician to pharmacy phone calls, 1 h/d of pharmacists' time).
But information technology is not a bandage for all the ails in patient safety. This broad arena of solutions is the future of patient safety as we move to stage 2 of the epidemic. Given all the public and private focus on safety, institutions and systems are rampantly testing a wide range of solutions from low tech, no cost to high tech, high cost as the recent AHRQ report highlights. The difficulty here, however, is that many safety practices are never studied in the classical rigor of research and never published. This likely applies to both low-tech, low-cost interventions and interventions so obvious that one need not study them. Although at an institutional or health care system level this may be acceptable, this publication bias enormously hinders widespread dissemination and adoption of good safety practices. These issues are best captured in the summary document of the AHRQ report stating that “there are a number of methodologic reasons why research in patient safety is particularly challenging”:
-
•
Many practices (eg, the presence of computerized physician order entry systems, modifying nurse staffing levels) cannot be the subject of double-blind studies because their use is evident to the participants.
Capturing all relevant outcomes, including near misses (such as a nurse catching an excessive dosage of a drug just before it is administered to a patient) and actual harm, is often very difficult.
Many effective practices are multidimensional, and sorting out precisely which part of an intervention works is often quite challenging.
Many of the patient safety problems that generate the most concern (wrong-site surgery, for example) are uncommon enough that demonstrating the success of a safety practice in a statistically meaningful manner with respect to outcomes is all but impossible.
Establishing firm epidemiologic links between presumed (and accepted) causes and adverse events is critical and frequently difficult. For instance, in studying an intuitively plausible risk factor for errors, such as fatigue, analyses of errors commonly reveal the presence of fatigued providers (because many health care providers work long hours, late night hours, or both). The question is whether fatigue is overrepresented among situations that lead to errors. The point is not that the problem of long work hours should be ignored but rather that strong epidemiologic methods need to be applied before concluding that an intuitive cause of errors is, in fact, causal.58
What is clear in this evidence report on safety solutions is that health care is clearly learning from other industries leading the way in safety. Although some proven solutions are clearly health care unique (eg, use of maximum sterile barriers while placing central intravenous catheters to prevent infections, use of perioperative beta blockers), other solutions are derived from other disciplines. These solutions include ideas such as aviation-style preoperative checklists, crew resource management, and the use of simulators in training. It would be safe to say that a repertoire of safety solutions for pediatric ambulatory care should be similarly balanced with health care–specific solutions and others borrowed and translated from other disciplines.
CONCLUSION AND PRIORITY SETTING
Pediatric patient safety in ambulatory care settings should be a high research and policy priority given the unique vulnerabilities of children, the glaring lack of current knowledge, and the disproportionate reliance on ambulatory care as compared to inpatient care. Efforts to tackle patient safety in ambulatory care need to occur in parallel with efforts on inpatient care. Overall, the entire arena of pediatric ambulatory care would be well served by safety research that started with understanding the basics: 1) what is the culture of safety in ambulatory care; 2) what types of errors are seen and what is their epidemiology; and 3) how do proven safety solutions from other settings/populations work in children's ambulatory care and how can ambulatory care overcome hurdles in evaluating and disseminating a broad range of safety solutions?
ACKNOWLEDGMENTS
Research and preparation of this article was supported in part by grant 1R13HS13883-01 from the Agency for Healthcare Research and Quality and grant 20020823 from The Commonwealth fund.
The authors of this article are responsible for its contents, including any clinical treatment recommendations. No statement in this article should be construed as an official position of the Agency for Healthcare Research and Quality or the US Department of Health and Human Services.
REFERENCES
- 1.Institute of Medicine. To Err Is Human: Building a Safer Health System. National Academy Press; Washington, DC: 1999. [Google Scholar]
- 2.Committee on Quality of Health Care in America, Institute of Medicine, ed. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, DC: 2001. [Google Scholar]
- 3.Available at: www.ahrq.gov Accessed November 19, 2003
- 4.Available at: www.quic.gov Accessed November 19, 2003
- 5.Available at: www.quic.gov/summit/resagenda.htm. Accessed
- 6.Miller MR, Battles J, Dougherty D. AHRQ's pediatric patient safety agenda. Ambulatory Pediatric Association Newsletter. Spring 2003;43(3):16. [Google Scholar]
- 7.Available at: www.mgma.com Accessed November 19, 2003
- 8.Available at: www.ahrq.gov/about/cpcr/ptsafety/index.html Accessed November 19, 2003
- 9.Hammons T, Piland NF, Small SD. Ambulatory patient safety. What we know and need to know. J Ambulatory Care Manage. 2003;26:63–82. doi: 10.1097/00004479-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Forrest CF, Shipman SA, Dougherty D, Miller MR. Outcomes research in pediatric settings: recent trends and future directions. Pediatrics. 2003;111:171–178. doi: 10.1542/peds.111.1.171. [DOI] [PubMed] [Google Scholar]
- 11.Kaushal R, Bates DW, Landrigan C. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 12.Miller MR, Elixhauser A, Zhan C. Patient safety events during pediatric hospitalizations. Pediatrics. 2003;111:1358–1366. doi: 10.1542/peds.111.6.1358. [DOI] [PubMed] [Google Scholar]
- 13.Quality Interagency Coordination Task Force. Doing what counts for patient safety: federal actions to reduce medical errors and their impact. QuIC; Washington, DC: 2000. [Google Scholar]
- 14.Beach C, Croskerry P, Shapiro M. Profiles in patient safety: emergency care transitions. Acad Emerg Med. 2003;10:364–367. doi: 10.1111/j.1553-2712.2003.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 15.Karcz A, Holbrook J, Burke MC. Massachusetts emergency medicine closed malpractice claims: 1988–1990. Ann Emerg Med. 1993;22:553–559. doi: 10.1016/s0196-0644(05)81941-9. [DOI] [PubMed] [Google Scholar]
- 16.Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: a synthesis of the literature. J Fam Pract. 2002;51:927–932. [PubMed] [Google Scholar]
- 17.Bhasale AL, Miller GC, Reid S, Britt HC. Analysing potential harm in Australian general practice; an incident monitoring study. Med J Aust. 1998;169:73–76. doi: 10.5694/j.1326-5377.1998.tb140186.x. [DOI] [PubMed] [Google Scholar]
- 18.Dovey SM, Meyers DS, Phillips RL. A preliminary taxonomy of medical errors in family practice. Qual Saf Health Care. 2002;11:233–238. doi: 10.1136/qhc.11.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ely JW, Levinson W, Elder NC. Perceived causes of family physicians' errors. J Fam Pract. 1995;40:337–344. [PubMed] [Google Scholar]
- 20.Fischer G, Fetters MD, Munro AP, Goldman EB. Adverse events in primary care identified from a risk-management database. J Fam Pract. 1997;45:40–46. [PubMed] [Google Scholar]
- 21.Gandhi TK, Sittig DF, Franklin M. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15:626–631. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holden J, O'Donnell S, Brindley J, Miles L. Analysis of 1263 deaths in four general practices. Br J Gen Pract. 1998;48:1409–1412. [PMC free article] [PubMed] [Google Scholar]
- 23.Britten N, Stevenson FA, Barry CA. Misunderstandings in prescribing decisions in general practice: qualitative study. BMJ. 2000;320:484–488. doi: 10.1136/bmj.320.7233.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Croskerry P, Chisholm C, Vinen J, Perina D. Quality and education. Acad Emerg Med. 2002;9:1108–1115. doi: 10.1111/j.1553-2712.2002.tb01564.x. [DOI] [PubMed] [Google Scholar]
- 25.Burstin H. Crossing the quality chasm in emergency medicine. Acad Emerg Med. 2002;9:1074–1077. doi: 10.1111/j.1553-2712.2002.tb01560.x. [DOI] [PubMed] [Google Scholar]
- 26.Perry SJ. Profiles in patient safety: organizational barriers to patient safety. Acad Emerg Med. 2002;9:848–850. doi: 10.1197/aemj.9.8.848. [DOI] [PubMed] [Google Scholar]
- 27.Cosby KS, Croskerry P. Patient safety: a curriculum for teaching patient safety in emergency medicine. Acad Emerg Med. 2003;10:69–78. doi: 10.1111/j.1553-2712.2003.tb01981.x. [DOI] [PubMed] [Google Scholar]
- 28.Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med. 2000;7:1204–1222. doi: 10.1111/j.1553-2712.2000.tb00466.x. [DOI] [PubMed] [Google Scholar]
- 29.Sacchetti A, Sacchetti C, Carraccio C, Gerardi M. The potential for errors in children with special health care needs. Acad Emerg Med. 2000;7:1330–1333. doi: 10.1111/j.1553-2712.2000.tb00484.x. [DOI] [PubMed] [Google Scholar]
- 30.Avery AJ, Sheikh A, Hurwitz B. Safer medicines management in primary care. Br J Gen Pract. 2002;52(suppl):S17–S22. [PMC free article] [PubMed] [Google Scholar]
- 31.Jackson DL, Johnson BS. Conscious sedation for dentistry: risk management and patient selection. Dent Clin North Am. 2002;46:767–780. doi: 10.1016/s0011-8532(02)00034-4. [DOI] [PubMed] [Google Scholar]
- 32.Lapetina EM, Armstrong EM. Preventing errors in the outpatient setting: a tale of three states. Health Aff (Millwood) 2002;21:26–39. doi: 10.1377/hlthaff.21.4.26. [DOI] [PubMed] [Google Scholar]
- 33.Stanger P, Silverman NH, Foster E. Diagnostic accuracy of pediatric echocardiograms performed in adult laboratories. Am J Cardiol. 1999;83:908–914. doi: 10.1016/s0002-9149(98)01063-7. [DOI] [PubMed] [Google Scholar]
- 34.Ward CJ, Purdie J. Diagnostic accuracy of paediatric echocardiograms interpreted by individuals other than paediatric cardiologists. J Paediatr Child Health. 2001;37:331–336. doi: 10.1046/j.1440-1754.2001.00695.x. [DOI] [PubMed] [Google Scholar]
- 35.Malis DJ, Burton DM. Safe pediatric outpatient sedation: the chloral hydrate debate revisited. Otolaryngol Head Neck Surg. 1997;116:53–57. doi: 10.1016/S0194-59989770352-8. [DOI] [PubMed] [Google Scholar]
- 36.Szilagyi PG, Bordley C, Vann JC. Effect of patient reminder/recall interventions on immunization rates. JAMA. 2000;284:1820–1827. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 37.Flores G, Laws MB, Mayo SJ. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 38.Fortescue EB, Kaushal R, Landrigan CP. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003;111:722–729. doi: 10.1542/peds.111.4.722. [DOI] [PubMed] [Google Scholar]
- 39.Taxis K, Barber N. Ethnographic study of incidence and severity of intravenous drug errors. BMJ. 2003;326:684–687. doi: 10.1136/bmj.326.7391.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gurwitz JH, Field TS, Harrold LR. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- 41.Available at: http://www.ismp.org/PR/OutpatientSetting.htm Accessed November 19, 2003
- 42.Personal communication from R. Kaushal.
- 43.AHRQ Integrated Delivery System Research Network Contract No. 290-00-0015. Prevalence of and strategies for appropriate prescription medication dosing for children
- 44.Miller MR, Elixhauser A, Zhan C. Patient safety events during pediatric hospitalizations. Pediatrics. 2003;111:1358–1366. doi: 10.1542/peds.111.6.1358. [DOI] [PubMed] [Google Scholar]
- 45.Slonim AD, LaFleur BJ, Ahmed W, Joseph JG. Hospital-reported medical errors for children. Pediatrics. 2003;111:617–621. doi: 10.1542/peds.111.3.617. [DOI] [PubMed] [Google Scholar]
- 46.Bristol Royal Infirmary Inquiry. Learning from Bristol: the report of the public inquiry into children's heart surgery at the Bristol Royal Infirmary 1984–1995. Stationery Office; London: 2001. www.bristol-inquiry.org.uk [Google Scholar]
- 47.Coulter A. After Bristol: putting patients at the centre. BMJ. 2002;324:648–651. doi: 10.1136/bmj.324.7338.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaushal R, Bates DQ. Information technology and medication safety: what is the benefit? Qual Saf Health Care. 2002;11:261–265. doi: 10.1136/qhc.11.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaushal R, Barker KN, Bates DW. How can information technology improve patient safety and reduce medication errors in children's health care? Arch Pediatr Adolesc Med. 2001;155:1002–1007. doi: 10.1001/archpedi.155.9.1002. [DOI] [PubMed] [Google Scholar]
- 50.Papshev D, Peterson AM. Electronic prescribing in ambulatory practice: promises, pitfalls, and potential solutions. Am J Manag Care. 2001;7:725–736. [PubMed] [Google Scholar]
- 51.Blendon RJ, DesRoches CM, Brodie M. Views of practicing physicians and the public on medical errors. N Engl J Med. 2002;347:1933–1940. doi: 10.1056/NEJMsa022151. [DOI] [PubMed] [Google Scholar]
- 52.Robinson AR, Hohmann KB, Rifkin JI. Physician and public opinions on quality of health care and the problem of medical error. Arch Intern Med. 2002;162:186–190. doi: 10.1001/archinte.162.19.2186. [DOI] [PubMed] [Google Scholar]
- 53.Cohen MM, Eustis MA, Gribbins RE. Changing the culture of patient safety: leadership's role in healthcare quality improvement. Jt Comm J Qual Saf. 2003;29:329–335. doi: 10.1016/s1549-3741(03)29040-7. [DOI] [PubMed] [Google Scholar]
- 54.Bagian JP, Gosbee JW. Developing a culture of patient safety at the VA. Ambul Outreach. 2000:25–29. Spring. [PubMed] [Google Scholar]
- 55.Wilf-Miron R, Lewenhoff I, Benyamini Z, Aviram A. From aviation to medicine: applying concepts of aviation safety to risk management in ambulatory care. Qual Saf Health Care. 2003;12:35–39. doi: 10.1136/qhc.12.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weeks WB, Bagian JP. Developing a culture of safety in the Veterans Health Administration. Eff CLin Pract. 2000;3:270–276. [PubMed] [Google Scholar]
- 57.Available at: http://www.ahrq.gov/qual/ps2001.htm#support Accessed November 19, 2003
- 58.Available at: http://www.ahrq.gov/clinic/ptsafety/summary.htm#overview Accessed November 19, 2003