Abstract
Introduction
The therapeutic use of animals has been debated for decades, and its use explored in a variety of settings and populations. However, there is no uniformity on naming these interventions. Evidence based knowledge is essential to implement effective strategies in hospital. This review focused on the use of animal programs for hospitalized patients, and considered the potential risks.
Methods
The following databases were searched: PubMed, Scopus, PsychInfo, Ebsco Animals, PROQUEST, Web of Science, CINAHL, and MEDLINE, and PRISMA guidelines were adhered to.
Results
Out of 432 articles were identified 36 articles suitable for inclusion into the review. Data was heterogeneous in terms of age of patient, health issue, animals used and the length of interactions, which made comparison problematic. Studies on children, psychiatric and elderly patients were the most common. The animal-intervention programs suggested various benefits such as reducing stress, pain and anxiety. Other outcomes considered were changes in vital signs, and nutritional intake. Most studies used dogs, but other animals were effectively employed. The major risks outlined were allergies, infections and animal-related accidents. Zoonosis was a possible risk, as well as common infections as Methicillin-resistant Staphylococcus Aureus. The implementation of simple hygiene protocols was effective at minimizing risk. The literature suggested that the benefits outweighed by far the risks.
Conclusion
The human relationship with animals can be useful and relatively safe for inpatients with various problems. Moreover, the implementation of security precautions and the careful selection of patients should minimize the risks, particularly those infection-related. Many aspects remain unclear, further studies are required.
Keywords: Animal-assisted activity, Animal-assisted therapy, Animal-assisted intervention, Pet-therapy, Hospital, Systematic review, Risks & benefits, Benefits, Clinical guidelines
1. Introduction
The Animal Assisted Therapy (AAT) is a health intervention, meant to improve physical, social, emotional or cognitive functioning, with animals as integral part of the treatment [1]. The therapeutic use of animals was argued for decades and many associations employ this intervention in order to improve care.
The interest shown by the scientific community is proven not only by the amount of articles published, but also by the specific trainings offered by many universities and in particular by the inception of specific law to regulate this practice [2].
The “Pet Partners” (an organization dedicated to improve people’s health through the interaction with animals) pointed out the differences between AAT and Animal Assisted Activity (AAA), less structured and mainly composed by pet visitation) [3]. The AAA, as described above, is slightly structured and it includes, primarily, pet-visitation. These kind of activities are in general spontaneous, grouping several patients, and poorly standardized with regard to duration and type of activities. On the contrary, the AAT sessions are strictly organized considering both the activity type and the duration. Indeed, each AAT session presents individualized goals and is conducted by specifically trained couples (handler and animal) [3]. Unfortunately, there is no uniformity on naming these interventions and AAT, AAA and other names are used, often, in a confusing way. To make even harder to compare the studies different animals were used. Although dog is the most common, generally every species can be employed.
Animal interventions have been studied for different pathologies including mental disorders [4] and cancer [5]. In particular, some interventions focused on frail patients as elderly [6], [7] or children [5], [8]. Furthermore, AAT and AAA are implemented in different settings like hospitals, nursing homes and schools [4], [5]. The employment of Animal-Assisted Interventions (AAI) resulted increasingly popular, especially among pediatric patients. Chur-Hansen et al. conducted a critical review regarding AAI for children inpatients. This review focused primarily on the methodology of the retrieved studies. Precisely, the authors concluded that the evidences regarding AAI are scant, and more standardized studies (in particular RCTs) about this topic are required [9]. Another recent review considered only the available RCTs regarding AAT, retrieving overall eleven studies (published from 1990 to 2012). The authors outlined a relatively low quality of the recovered papers. However, the study highlighted some benefits of the AAT, especially in case of psychiatric disorders. The animals employed in these interventions were disparate, from dogs to dolphins or ferrets. The authors identified some areas requiring further insights such as costs, reasons to refuse the intervention and potential adverse effects. Moreover, the authors highlighted how the description of the intervention in terms of length, activities and settings, in the studies included in the review, was not always obvious [4].
The outcomes considered, in order to define the AAI benefits, are heterogeneous, incorporating subjective outcomes as the quality of life [10], [11], but also objective parameters as vital signs [12], hemodynamic measures [13] and nutritional intake [14]. A 2007 review and meta-analysis, firstly, assessed the quantitative effects of AAT. The meta-analysis included 49 studies, and suggested a significant improvement in the following examined areas: autism-spectrum symptoms, behavioral problems, and emotional well-being. The authors described the AAT as a worthy intervention, necessitating, however, further insights [15].
Furthermore, the risks of implementing animal therapeutic interventions especially in hospitals are not negligible, and these hazards must be considered [16], [17].
An accurate knowledge of the effectiveness and risks of animal use in hospital is essential to implement effective strategies in this setting. Nevertheless, data considering animal interventions are often heterogeneous. To our knowledge, no previous reviews estimated the evidence on the use of animal-interventions for inpatients. The aim of this review was to focus on Animal Assisted Therapy/Activity for hospitalized patients, to provide a clearer view on the status of the evidence supporting this practice, as well as the potential risks.
2. Methods
This review followed the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statements [18].
Multiple search strategies were employed to summarize the existing evidence relating to animal assisted therapy or animal assisted activity for inpatients. Searches for papers reporting data about the effectiveness or the risks of animal use in hospitals were carried out using the following databases: PubMed, Scopus, PsychInfo, Ebsco Animals, PROQUEST, Web of Science, CINAHL and MEDLINE.
Three researchers (EC, GP and GV) independently performed a systematic search using the following strings: “Animal assisted activity” AND hospital, “Animal assisted therapy” AND hospital, “Animal assisted intervention” AND hospital, “Pet therapy” AND hospital, “Animal assisted activity” AND hospitalization, “Animal assisted therapy” AND hospitalization, “Animal assisted intervention” AND hospital, “pet therapy” AND hospitalization.
Studies were considered eligible for inclusion if they:
-
•
were conducted in hospitals or in long-term care facilities
-
•
were written in English, Spanish or Portuguese
-
•
considered interventions of “Animal Assisted Therapy”, “Animal Assisted Activity” or “Animal Assisted Intervention”
No restriction was performed based on inpatient age, pathology, or type of animal used. All types of papers were included, since RCTs were few and did not give a complete overview of the topic.
Articles were excluded if they:
-
•
were conducted outside the hospital
-
•
were published before 2000
-
•
used robotic animals
-
•
were case reports or letters to the editor
Three investigators (EC, GP and GV) independently conducted a first literature search, sorting sources by title and abstract. Then, the eligible studies for full text review were selected. During the first screening, the irrelevant or duplicated papers were excluded. The search was completed through a reference list screening. Finally, the researchers independently assessed the articles considering the criteria enunciated above.
2.1. Data extraction
The investigators, solving any discrepancies by consensus, independently extracted data from the selected studies, collecting information about the country, the study design, the setting, the sample characteristics, the type of intervention, the outcomes, the results and the potential risks.
3. Results
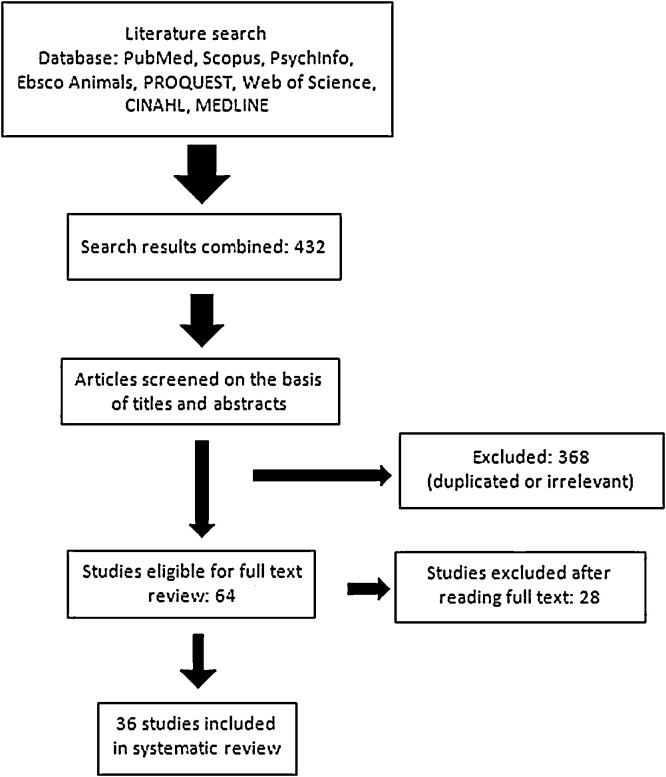
The search returned 432 results. After removing the duplicates and irrelevant results, 64 articles for full text review were obtained. The final selection obtained 36 sources (see Fig. 1 ). Eight studies were conducted on children, five referred to psychiatric population, six considered elderly patients, six were performed in the Emergency Department, Orthopedics, Internal Medicine or other wards, and eleven focused primarily on the intervention risks.
Fig. 1.
Flowchart—the figure summarizes the selection procedures of our review.
3.1. Psychiatric settings
Five studies focused on the AAT for psychiatric inpatients (See Table 1 ) [10], [11], [19], [20], [21]. All studies were published between 2009 [20], [21] and 2015[11], [19]. Nearly all the studies considered a dog-AAT (n = 4), with the exception of a study comparing four interventions: equine-assisted psychotherapy (EAP), canine-assisted psychotherapy (CAP), enhanced social skills psychotherapy, and regular hospital care [19]. Four studies were RCTs [10], [11], [19], [21] and one a controlled crossover study [20]. The total sample size ranged from 12 [20] to 90 [19].
Table 1.
Characteristics of the retrieved studies regarding animal interventions for psychiatric inpatients. The table reported information about the study design, the participant characteristics (sample size, disease, setting), the intervention type (including length and animal used), the considered outcomes and the main results.
| Authors and Year | Study Design | Sample | Disease/setting | Intervention Type | Length | Animals | Outcomes | Findings |
|---|---|---|---|---|---|---|---|---|
| Stefanini, 2015 | RCT | 34 children | Acute psychiatric diagnosis | Intervention group: structured AAT Control groups: standard therapeutic protocol |
Weekly sessions (45 min each) for 3 months | Dogs | Global functioning Format of hospital care (assessing clinical severity) Ordinary school attendance Observation of AAT (participation, socialization with peers and adults, withdrawal behaviors) |
Pre- and post-test analysis outlined an improvement in hospital care (p = 0.02), school attendance (p < 0.03) and global functioning (p < 0.0001) in the treatment group vs. control. Patients in the AAT-group showed higher participation and socialized behaviors with adults and peers (all p < 0.01), and a reduction in withdrawal behaviors (p < 0.04) |
| Nurenberg, 2015 | RCT | 90 inpatients | Psychiatric inpatients with aggressive or regressed behaviors | Equine-assisted psychotherapy (EAP) Canine-assisted psychotherapy (CAP) Environmentally enhanced social skills group psychotherapy (SSP) Regular hospital care |
10 weekly group sessions (40–60 min each) | Dogs Horses |
Aggression-related outcome measures Brief Psychiatric Rating Scale Life Skills Profile Greystone Intrusiveness Measure Staff expectations about AAT Pet Attitude Scale–Modified Visual Analog Scale |
Violent incident reports showed a significant decrease for EAP patients compared to other groups (p < 0.035), showing differences in aggressions both towards objects (p = 0.05) and persons (p = 0.053). |
| Chu, 2009 | RCT | 30 inpatients | Chronic schizophrenia | Intervention group: AAA sessions Control group: standard therapy |
AAA sessions (50 min) once a week for two-months | Dogs | A questionnaire exploring: Self-esteem, Self-determination, Extent of social support and Adverse psychiatric symptoms | There were significant improvements (p < 0.05) in self-esteem, self-determination, positive psychiatric symptoms, and emotional symptoms. The scores regarding social support and negative psychiatric symptoms did not significantly improve. |
| Hoffmann 2009 | Cross-over study | 12 inpatients | Unipolar major depression | Intervention group: interaction with a dog and a research assistant. Control group: 30-min talk with the researcher |
Two AAA 30 min sessions | Dogs | State-Trait Anxiety Inventory (STAI) | The STAI score significantly decreased after the dog-session (p = 0.016). In the control group STAI score did not significantly differ (p = 0.327) |
| Villalta 2009 | RCT | 21 patients in long-term care facilities | Chronic schizophrenia | Intervention group: AAT Control group: no AAT | 25 sessions of 45 min each | Dogs | Symptoms (Positive and Negative Syndrome Scale PANSS) Social competence (Living Skills Profile) Quality of Life Satisfaction with Treatment |
Patients in the intervention group presented significant improvements in social contact score (p = 0.04), in positive (p = 0.005) and negative symptoms (p = 0.005), in quality of life (p = 0.02). Patients in control group showed improvements in positive (p = 0.03) and general symptoms (p = 0.046). |
Chu and Villalta specifically focused on canine-assisted therapy for chronic schizophrenic inpatients (>10 years since onset) [10], [21]. Both studies underlined some positive effects of these interventions. In particular, the study of Chu, highlighted an increase in self-esteem, self-determination, and a decrease in positive psychiatric symptoms and emotional symptoms after 8 weeks of AAA (p < 0.05) [10]. The study by Villalta showed a significant improvement from baseline after a dog-program in social contact score, in positive and negative symptom dimensions and in quality of life [21]. However, no significant difference was assessed between the group experiencing AAT and the control group [21]. Nurenberg et al. considered the effectiveness of the AAT in reducing aggressiveness in chronic psychiatric inpatients, including various psychiatric diagnosis (76% presented schizophrenia or schizoaffective disorder). The authors compared two different AAT, the first using dogs and the second horses. Certified pet therapists, following the “Pet-Partners guidelines”, conducted both these interventions. The reduction of violent incidents was significantly greater in the EAP group (p < 0.035), while other generic benefits were assessed for both the AAT interventions. These positive effects were maintained for several months [19].
The effects of AAT were studied also in other psychiatric diseases as major depression (inpatients with suicidality tendencies). In this study, a dog-assisted intervention (two sessions of dog-AAA) effectively reduced anxiety (p = 0.016), as measured employing the State-Trait Anxiety Inventory (STAI). This improvement was independent from age, gender or pet possession [20].
Finally, an Italian study considered children experiencing acute psychiatric disorders. The main diagnosis were eating disorders (64.7%) and mood disorders (20.6%). In this population, the implementation of a dog-AAT program once a week resulted, compared to the control group, in an improvement of clinical severity (p = 0.02), ordinary school attendance (p < 0.03), and global functioning (p < 0.0001). In particular, the intervention group showed an improvement in socialized behaviors with adults and peers (p < 0.04). The authors adhered, for the protocol implementation, to the “Pet Partners guidelines”, and all the animals employed in the study followed strictly veterinarian sanitary protocols [11].
3.2. Childrens’ hospitals
Eight papers referred to pet therapy in pediatric hospitals (See Table 2 ) [8], [22], [23], [24], [25], [26], [27], [28]. The articles were published between 2002 [22], [28] and 2015 [23]. Two were descriptive studies [24], [25] and six trials [8], [22], [23], [26], [27], [28]. Two studies had a special focus on oncological patients [24], [25], while the others referred to general pediatric inpatients. In particular, two interested children with acute diseases [23], [26]. All papers used dogs, ranging from simple pet visitation [22], [28] to structured AAT [23], [26], [27]. The number of children involved ranged from 15 [27] to almost 150 [8].
Table 2.
Characteristics of the retrieved studies regarding animal interventions for inpatient children. The table reported information about the study design, the participant characteristics (sample size, disease, and setting), the intervention type (including length and animal used), the considered outcomes and the main results.
| Authors and Year | Study Design | Sample | Disease/setting | Intervention Type | Length | Animals | Outcome | Findings |
|---|---|---|---|---|---|---|---|---|
| Barker, 2015 | RCT | 40 hospitalized children | Children admitted to Hospital of Richmond except Pediatric Intensive Care Units | Intervention group: AAI Active control group: jigsaw puzzle |
10 min sessions | Dogs | Pain and Anxiety ratings Attachments Questionnaire for Children Family life-space Diagrams |
The AAI-group experienced lower post-intervention anxiety scores (p < 0.05). No significant within- or between-group pre-post changes in either pain or anxiety were detected. |
| Tsai, 2010 | Quasi-experimental design | 15 hospitalized children | Acute or chronic conditions | AAT (taking place in patient room) Control group: puzzle (each child did both the interventions) |
6–10 min sessions | Dogs | Blood pressure and heart rate Child Medical Fear Scale State-Trait Anxiety Inventory for Children (STAI-C) |
Systolic Blood Pressure (SBP) decreased from before, during and after AAT (p = 0.008). Children’s anxiety and medical fear did not differ after the AAT visit compared with the comparison intervention. |
| Braun 2009 | Quasi-experimental intervention study | 57 children | Acute care settings | Intervention group: AAT Control group: children sat quietly for 15 min | 15–20 min sessions | Dogs | Blood pressure, pulse rate, respiratory rate Pain level (FACE pain scale) |
The group experiencing AAT had a significantly lower post-test pain score compared to the control group (p = 0.006). Even parents perception of pain reduction was higher for the intervention group (p = 0.008). AAT group presented higher respiratory rate (p = 0.011), no differences were found in blood pressure and pulse |
| Caprilli 2006 | RCT | 138 children | Different hospital wards | AAA | Once a week for 2-h sessions | Dogs | Children participation Infection rate in the hospital Children pleasure Parents and staff level of satisfaction |
No increase in infection or in contagious disease transmitted by dogs were found. The children pleasure evaluation showed significant improvement. Parents and staff satisfaction rate was high. |
| Gagnon 2004 | Descriptive study | 16 parents and 12 nurses | Pediatric oncology wards | Dog-AAT | Each session lasted a whole day | Dogs | Satisfaction with the program and of quality of care | Beneficial role of animal therapy was underlined for physical, social, emotional, coping and self-esteem dimension |
| Bouchard 2004 | Pilot project | 27 children | Pediatric oncology wards | AAT with a dog at bed-side | / | Dogs | Client satisfaction Impact on nursing work Appropriateness of prevention measures |
Parents outlined positive aspects of the experience (as increasing children confidence, mood improvement). According to nurses, the program was well structured. They used the children’s relationship with dogs as a therapeutic tool during the intervention process. |
| Kaminski 2002 | Clinical trial on a convenience sample | 70 hospitalized children | General inpatients | Intervention group: dog-facilitated therapy Control group: Child Life group |
One session per week | Dogs | Self-reported mood, and parents and caregiver reports Clinical assessment Physiological indicators: heart rate, blood pressure, salivary cortisol |
Parents and caregivers rated their children as happier after intervention in both groups (p < 0.001). Heart rate was significantly higher in the pet therapy group (99.27 ± 16.38) than in control group (88.44 ± 12.68). |
| Moody et al. 2002 | Two cross-sectional surveys | Staff Questionnaire: 115 pre-program and 45 after | Pediatric Medical wards | Pet-visitation program | / | Dogs | Hospital staff perception (questionnaire to administrators, doctors, nursing staff and therapists; 6 weeks before and 12 weeks after the introduction of the program) | Prior to the introduction of the dog visitation, there were high staff expectations regarding the program. Healthcare workers outlined the relaxation effect, the mood improvement. Staff member generally accepted dogs. |
Four studies evaluated the satisfaction after the intervention and the effects on psychosocial behaviors [8], [22], [24], [25], instead four considered also physiological phenomena [23], [26], [27], [28]. Two studies were conducted through a survey among parents and caregivers [22], [24], while in two these data were integrated with children self-reports [8], [25]. Many different physiological parameters like pain [23], [26] or cardiovascular response [27], [28] were evaluated.
The studies involving oncological patients showed physiological benefits, like pain reduction [26], and psychological benefits like decreased loneliness, increased relaxation, socialization and self-esteem [8]. These benefits were perceived also by parents and caregivers [24], [28]. These findings are consistent with a study conducted in acute pediatric care [22].
Barker et al., in a RCT on generic pediatric inpatients, showed the consistency of these results in different diseases [23]. This study evaluated the AAI impact on anxiety and pain in acute care. A significant difference was found for anxiety, with the AAI-group experiencing lower anxiety score [23]. However, no significant differences within- or between-groups or pre-post intervention were assessed in nor pain or anxiety [23]. For the implementation of this protocol, all the hospital policies were followed, including those regarding safeguard for the dogs.
On the other hand, no differences in anxiety and medical fear were noticed in a study involving 15 hospitalized children [27]. In this study, a reduction in the systolic blood pressure (p = 0.008) was recorded and this reduction continued even after the intervention was over.
3.3. Elderly patients
Six articles evaluated the impact of the AAT in elderly inpatients (See Table 3 ) [6], [7], [13], [14], [29], [30]. These articles were published between 2002 [14] and 2012 [30]. Five studies were performed in hospitals [7], [13], [14], [29], [30], while one was conducted in a nursing home [6]. The samples ranged from 20 [30] to 76 [13] subjects.
Table 3.
Characteristics of the retrieved studies regarding animal interventions for elderly inpatients with various illness (including Alzheimer disease and heart failure). The table reported information about the study design, the participant characteristics (sample size, disease, and setting), the intervention type (including length and animal used), the considered outcomes and the main results.
| Authors and Year | Study Design | Sample | Disease/setting | Intervention Type | Length | Animals | Outcome | Findings |
|---|---|---|---|---|---|---|---|---|
| Kumasaka, 2012 | Pre-/Post- study | 20 inpatients | Oncologic patients in palliative care unit | AAA | Once per month for about 30 min | Dogs Cats Rabbits |
Quality of Life (QOL) assessed through the Lorish’s Face Scale | The study outlined a beneficial effects of AAA considering the facial scale score. Mean score was 8.10 ± 3.48 before the session and 2.66 ± 1.99 after the activity (significant decrease: p < 0.01) |
| Abate, 2011 | Prospective study | 69 inpatients | Heart failure | Intervention: Canine-assisted ambulation (CAA) Control: historical population |
/ | Dogs | Actual distance walked Patient satisfaction |
The experimental group receiving CAA walked significantly more steps than the historical group (p < 0.0001). |
| Falk et al. 2008 | Qualitative study | 35 Older people | Swedish hospital wards | Placing a bird cage in the ward lounge | September − November 2002 | Birds | Participant observation (three major themes: activity, mental experience and socializing) | The patients manifested attention and curiosity toward birds, expressing desire to take care of the birds. The birds became subject of general diversion. |
| Cole, 2007 | RCT | 76 inpatients | Advanced heart failure | Volunteer-dog team (visit from a volunteer with a therapy dog) Volunteer only Control: standard care |
12-min visits | Dogs | Blood pressure, Heart rate Pulmonary pressure and pulmonary capillary wedge pressure Right atrial pressure Epinephrine and norepinephrine Anxiety score |
The dog intervention group had significantly greater decreases in systolic pulmonary artery pressure (p = 0.03), and in pulmonary capillary wedge pressure (p = 0.001). The volunteer-dog group had the greatest decrease in anxiety score compared with volunteer-only (p = 0.02) and control group (p < 0.001). |
| Stasi, 2004 | Case-control study | 28 Subjects | Chronic age-related disabilities in a nursing home | Intervention group: cat-therapy Control group: usual activity programs |
3/week sessions of almost one-hour visit for 6 weeks | Cats | Blood pressure Cognitive impairment by mini mental state examination (MMSE). Geriatric depression scale (GDS) Self-assessment scale-geriatric (SASG). Activities of daily living (ADL) Instrumental activities of daily living (IADL) |
Patients in the intervention group presented improved depressive symptoms (not statistically significant) Significant systolic blood pressure decrease was outlined in pet-therapy group compared to control group (p = 0.01). |
| Edwards et al. 2002 | Time-series design | 62 inpatients | Alzheimer disease | Aquariums placed in the activity/dining area | 10 weeks | Fishes | Nutritional intake Change in body weight |
Following aquariums introduction, the nutritional intake significantly increased (p < 0.001) and continued to improve during follow-up. Patient weight increased significantly (p < 0.001) over the observational period |
Patients were hospitalized for different diseases including cancer [30], chronic heart failure [13], [29], Alzheimer disease [14] or chronic age-related disease [6], [7]. The animals used were dogs [13], [29], [30], cats [6], [30], rabbits [30], cage birds [7] and fishes [14].
Stasi used a cat-therapy (3 sessions per week) for 28 elderly patients in a long-term facility [6]. A significant reduction in depressive symptoms and systolic blood pressure (p = 0.01) was measured in the intervention group [6]. Similarly, a dog therapy was compared to volunteer visit and usual care in 76 patients suffering acute heart failure [13]. Compared with controls, the volunteer-dog group experienced a significant decrease in systolic pulmonary artery pressure and in pulmonary capillary wedge pressure [13]. Compared with the volunteer-only group, the volunteer-dog group presented a greater decrease in epinephrine and in norepinephrine levels during and after the intervention. Finally, the dog-group showed a greater decrease in the state anxiety score compared to both volunteer-only (p = 0.02) and control group (p < 0.001) [13].
Conversely, another study analyzed the impact of dog-therapy on patients with chronic heart failure to determine the impact of Canine Assisted Ambulation (CAA) in encouraging ambulation [29]. Additionally, patient satisfaction was assessed. The experimental group receiving CAA walked significantly more steps (p < 0.0001) than the historical control group, and all patients responded positively to this experience [29].
The benefits of AAA were investigated in a palliative care unit of a Japanese hospital, considering twenty elderly users. The considered program included a 30-min session once a month using dogs, cats or rabbits, all previously tested for health and suitability. The authors considered the effects of this intervention upon the Quality of Life of the selected inpatients, employing a validated scale (Lorish Face Scale) to assess mood changes. The study outlined the beneficial effect of similar interventions in the mood state before and after each session (p < 0.01). In particular, the positive results were higher for those who claimed to like animals or that owned a pet (especially dogs) [30].
Furthermore, we found studies using uncommon animals like fish [14] and caged birds [7]. A first study assessed the nutritional intake in individuals with Alzheimer after the introduction of an aquarium in the ward [14]. The nutritional outcomes were recorded at baseline, and, then, after 10 weeks following the aquariums introduction. The nutritional intake increased significantly (p < 0.001) after this intervention and continued increasing during follow-up. Moreover, also the weight increased significantly (p < 0.001) [14]. A second study assessed the interaction between caged-birds and older people in hospital [7]. This qualitative study investigated the patient’s reactions succeeding the introduction of caged birds in a Swedish geriatric ward. Patients manifested attention and curiosity regarding the birds and expressed desire to take care of them [7].
3.4. Emergency department, orthopedics, internal medicine and other wards
Six studies evaluated the impact of pet therapy on adult inpatients with different pathologies (See Tables 4 ) [31], [32], [33], [34], [35], [36]. Two studies investigated the dog-AAT effectiveness for orthopedic inpatients after a total joint arthroplasty intervention [31], [32]. Both studies considered the impact of this intervention on pain [31], [32]. Harper et al. inquired the subjective level of pain, using the Visual Analogue Scale (VAS) [31], while Havey et al. assessed the use of oral pain medications [32]. Harper et al. considered a dog-visitation session prior each physical session, and outlined lower VAS score in the intervention group (p < 0.001) [31]. Furthermore, the use of pain medications appeared significantly lower among the AAT group (p = 0.007) [32]. Harper investigated also the patient satisfaction regarding the hospital stay [31]. The treatment group reported a higher level of appreciation compared to the control group (p < 0.05). Moreover, the groups did not differ nor in the cleanliness items nor in quietness of hospital environment [31].
Table 4.
Characteristics of the retrieved studies regarding animal interventions for adult inpatients with various illness (including orthopedic patients, and high-risk pregnancy). The table reported information about the study design, the participant characteristics (sample size, disease, and setting), the intervention type (including length and animal used), the considered outcomes and the main results.
| Authors and Year | Study Design | Sample | Disease/setting | Intervention Type | Length | Animals | Outcome | Findings |
|---|---|---|---|---|---|---|---|---|
| Harper, 2014 | RCT | 72 patients | Orthopedic patients after Total Joint Arthroplasty intervention | Intervention Group: therapy dog and handler visitation Control group: standard physical therapy | 30 min before each physical therapy session | Dogs | Pain (VAS scale) Hospital Consumer Assessment of Healthcare Providers and Systems survey (HCAHPS) |
Patients in the intervention group had lower VAS scores after each session compared to standard care (p < 0.001). The intervention group presented higher scores regarding nursing communication (p = 0.035), pain management (p = 0.024) and overall hospital rating (p < 0.001) compared to control group. |
| Havey et al. 2014 | Retrospective study | 297 hospitalized patients | Joint replacement intervention | Hospital A: no AAT program Hospital B: AAT program (dog + handler visits) |
Visits of 5–15 minutes | Dogs | Analysis of oral pain medications usage | The cohort receiving at least one session of animal assisted therapy presented lower rate of oral pain medication use (p = 0.007) |
| Lynch et al. 2014 | Pilot study | 82 Hospitalized women | High-risk pregnancies | Non-structured session of dog in-room contact | Sessions of 15–20 min | Dogs | State-Trait Anxiety Inventory Beck Depression Inventory |
Both depression (p < 0.0001) and anxiety (p < 0.0001) significantly improved following dog contact |
| Nahm, 2012 | Survey | 125 patients, 105 staff members | Emergency Department (ED) | Therapy dogs visited the ED | 6 visits during the observation period | Dogs | Acceptance of a therapy dog among staff and patients | Most patients (93%) and staff (95%) thought that therapeutic dogs should visit the ED. Only 3.3% of patients and 1% of staff considered dog presence as a danger, while 8.6% of the staff and 4.2% of patients thought that dogs could interfered with ED work. |
| Coakley 2009 | Pre-/post quasi-experimental design | 61 inpatients | Medical 52.6% or surgical 47.4% diagnosis | Individualized pet therapy intervention based on patient preference | Session of on average 10 min | Dogs | Vital signs (blood pressure, pulse and respiratory rate) Visual Analog Scale (VAS) for pain Profile of Mood States survey (POMS) |
After pet therapy sessions, patients experienced a significant decrease in respiratory rate (p < 0.001) and pain score (p = 0.001), associated with increased energy levels (p = 0.001). Total mood disturbance scores improved significantly (p < 0.001), in particular, in anxiety (p < 0.001), anger (p = 0.001) and fatigue (p < 0.001) items. |
| Hastings et al. 2008 | Survey | 614 patients or visitors | Burn Intensive Care Unit and Burn Acute Care Unit | Dog-AAT | Bi-weekly visitation | Dogs | Total number of AAT visits Questionnaire with visitation assessments Observational summaries from patients, their families, and staff. |
Number of dog-visits increased from 2002 to 2005 (respectively 39 vs. >300). Only 3 patients (0.5%) refused dog visitation, reporting fear. Observations of patients, families, and staff were nearly all positive |
Lynch et al. studied the implementation of a dog-AAI in antepartum wards for women with complicated pregnancies [33]. The program consisted of non-structured dog-contact sessions. The authors assessed depression and anxiety symptoms prior and after each session [33]. The women recruited presented heterogeneous complications, including pre-term labor, pre-eclampsia and diabetes. Despite the lack of a control group, the results indicated that both depression and anxiety improved after the intervention (p < 0.01) [33].
Two studies considered the implementation of a dog-AAT in hospital wards [34], [35]. Nahm considered the development of similar programs in an Emergency Department, considering the opinion of patients, staff and visitors [34]. The intervention was successful among both patients and visitors ( < 5% of the patients expressed negative opinions). Furthermore, the staff appreciated the intervention (over 90% did not considered dogs as an obstacle to routine activities) [34]. Coakley et al., instead, focused on the implementation of a dog-visitation program in twelve different departments, collecting patients’ opinions [35]. The authors considered the effects on vital signs, pain perception (VAS-scale), and mood-state (exploring anxiety, depression, hostility, vigor, fatigue and confusion). The subjects participating presented a wide range of diseases. After the intervention the participants experienced a slightly, but significant, decrease in respiratory rate (p < 0.001) and in pain score (p = 0.001). The mood scale outlined a significant improvement in nearly all the items (p < 0.001), except vigor and confusion [35].
Finally, Hastings et al. investigated the use of a bi-weekly dog-visitation in a Burn Intensive Care Unit and a Burn Acute Care Unit [36]. In order to guarantee the security of these patients, all the Protection Equipment guidelines were respected. The authors collected patients, staff and visitor opinions. Nearly all comments were positive and only three patients (0.5%) refused the proposed sessions, reporting fear. The number of dog-visits significantly increased during the observation, and no infection nor issues animal-related were reported [36].
3.5. Risks and threats of animal-intervention in healthcare settings
Eleven articles focused explicitly on the risks of animal use in hospitals (see Table 5 ) [16], [17], [37], [38], [39], [40], [41], [42], [43], [44], [45]. These papers ranged from 2000 [37] to 2013 [38], and included guidelines, recommendations, clinical trials, cross-sectional surveys and reviews. Two studies investigated the prevalence of infective agents in pet-visitation animals in hospitals or in long-term care facilities [17], [44]. The first investigation is a broader survey that considered all the hospitals located in the Ontario region with a pet visitation program. In particular, this investigation analyzed aural, nasal, oral, pharyngeal and rectal swabs of over 100 visitation dogs, identifying Clostridium Difficile as the most common isolated organism [17]. Moreover, 17% of these isolates were indistinguishable from the toxigenic microorganisms responsible of the human disease. In the feces samples, the authors retrieved also Salmonella and Escherichia Coli (partly in antibiotic-resistant forms). Furthermore, some samples were positive to parasitology and mycology analysis. These microorganisms were carried asymptomatically by dogs, but can be dangerous especially for immunocompromised patients [17]. Coughlan et al. focused on Methicillin-resistant Staphylococcus Aureus (MRSA) colonization among residents animals (one dog and eleven cats) in a long-term care facility [44]. The authors considered a large long-term care facility with over 100 beds, characterized by the presence of resident animals. The researchers collected nasal swabs from the animals for overall eight weeks. Two cats presented MRSA positive swabs and the test positivity was confirmed in subsequent tests. In the meantime, human MRSA infections occurred in the facility [44].
Table 5.
Characteristics of the retrieved studies regarding animal interventions risks in healthcare settings. The table reported information about the study design, the setting, the type of intervention considered (including the assessed animals), the major risks identified and the findings.
| Authors and Year | Study design | Setting | Considered intervention | Animals | Risk considered | Findings |
|---|---|---|---|---|---|---|
| Sehr, 2013 | Guidelines | Memorial Hospital in Belleville, Illinois | Pet visitation | Private pets | Infection risks Nurse evaluation |
The authors considered as eligible all inpatients, excluding those in operating room, post-anesthesia care unit and newborn nursery. Also, immunocompromised patients were excluded. The pet was not allowed to stay in the room alone with the patient. The nurses did cleanliness check after each visitation. The authors assessed overall positive nurses’ evaluations |
| Silveira, 2011 | Protocol of AAT | A Brazilian University hospital | AAA | Dogs Cats Fish Rabbits Reptiles Rodents |
Infection risks Allergy |
Animals must be evaluated by veterinary before the admission to the program, and all the animals employed followed a specific train. Then, animals are evaluated annually. Animal’s hygiene protocols should be implemented in the 24 h prior each session. Hygiene protocols for all the surfaces after each session. Exclusion criteria for patients are post-operative, recent splenectomy, known allergy, phobia, immunocompromised oncologic patients and HIV infection in terminal stage. |
| Coughlan, 2010 | Prevalence study | One long-term care facility with 108 patients | Resident animals in long-term care facility | 11 cats 1 dogs |
Infection risk, focusing on Methicillin-resistant Staphylococcus aureus. The animals were sampled weekly for 8 weeks (total: 87 cultures) in the time period July 2006–August 2006 |
Two of 11 cats were colonized with MRSA; positivity was confirmed in repeated samples. The isolated strains were classified as healthcare-associated strains. In the meantime, human MRSA infections occurred in the facility. |
|
Kobayashi, 2009 |
Report | San Paolo Hospital | AAT | Potential animals employed in AAT | Infection risks Allergy Accidents related to animals |
The animals involved must follow repeated veterinary visits, presenting a health certificate. Both therapist and animal followed a specific train. Animals should be bathed the day before each session. Exclusion criteria for the patients included splenectomy, immunosuppression, neutropenia, allergy or respiratory problems. Each incident should be recorded and reported to a specific hospital Commission. |
| Di Salvo, 2006 | Guidelines | Hospital with specialized units | Service dogs AAT Pet visitation |
Dogs | Infection risks Accidents related to animals |
Therapy and visitation dogs are more restricted than service dogs. Health certification is required for all animals entering hospitals. Dogs are excluded to certain areas as Intensive Care Unit and isolation rooms. Adopting current regulations, risks can be minimized. A proper education to all the staff is recommended. |
| Lefebvre, 2006 | Cross-sectional study | Hospitals in Ontario (n = 231) Dog Owners (n = 90) |
AAA and Canine visitation | Dogs | Survey regarding potential risks and adherence to guidelines | Dogs were admitted in 90% of the considered hospitals. The Acute Care Hospital were more likely to disallow dogs (p < 0.001). The sanitary protocols to avoid infections resulted variable. 20% of the owner declared no infection control. 73% owners consented dogs to get on the patient’s bed and 79% let dogs lick patients. Only 14% received zoonosis information from their veterinary. 40% of the owners did not know any potential zoonosis transmitted by dogs. |
| Jofrè, 2005 | Review of Guidelines | Healthcare facilities | AAT | Dogs Cats Rabbits Birds |
Infection risks Allergy Accidents related to animals |
Animals must undergo periodic veterinary controls, avoiding the use of puppies. It is important to careful evaluate which patients to include in the interventions (exclusion in case of phobia, allergy, splenectomy, and immunocompromised patients) Rigorous hand-hygiene for patients and healthcare personnel, avoiding, as possible, any contact with animal bodily fluids. Rigorous control of the AAT sessions by trained therapists. The animal should be bathed before each session, to minimize the allergy risk. |
| Lefebvre, 2005 | Prevalence study | Hospitals in Ontario | Pet-visitation programs | Dogs (n = 102) |
Zoonosis Investigated through aural, nasal, oral, pharyngeal and rectal swabs. |
58% of the samples were positive to Clostridium Difficile (41/58 isolates were toxigenic). Three dogs were positive to Salmonella. Other samples resulted positive to Toxocara Canis, Ancylostoma Caninum, Giardia, Escherichia Choli, Malassezia Pachydermatis, Pasteurella and Trichophyton Mentagrophytes |
| Sehulster, 2003 | CDC Guidelines | Health-care facilities | AAA and Resident animals programs | All potential animals | Infection risk Animal-related accidents Allergies |
Specific guidelines to avoid the potential risks. In particular, minimize contact with animal bodily fluids, and implement hand hygiene after each contact. Avoid selection of dangerous animals for AA as primates and reptiles. Careful selection of specifically trained animals. Provide prompt response in case of animal-related accidents. Minimize allergic risks bathing and grooming the animal in the 24 h prior the visit. Use routine cleaning protocols after each session. Use all the protective measure for immunocompromised patients. |
| Brodie, 2002 | Review | Healthcare environment in Europe or North America | Pet-therapy | Dogs Cats Birds Other animals |
Infection risk Animal-related accidents Allergies |
The review concluded that infectious hazards are minimal The animal-related accidents, as bites and scratches, can be minimized following rigorous train and protocols It is recommended to incorporate intensive veterinary care. |
| Khan, 2000 | Review | Healthcare settings | AAA or AAT | All potential animal employed in AAI, especially dogs | Animal bites or accidents Zoonosis Allergies |
Infection control policies must be implemented and followed. Careful selection and suitability of the animals employed. Careful selection of eligible patients. The authors suggested to exclude: patients with splenectomy, dog allergies, positive to Mycobacterium Tuberculosis, with pyrexia of unknown origin or infected by MRSA |
Lefebvre et al. conducted a cross-sectional survey in the Ontario hospitals in order to assess the presence and characteristics of Canine Visitation Programs for inpatients. Moreover, the authors interviewed the dog handlers regarding the health protocols for AAA. Nearly all the hospitals surveyed (90%) consented the access to dogs in their facilities. Two of the selected hospitals interrupted the AAA program, during 2003, due to the onset of severe acute respiratory syndrome. The screening protocols resulted extremely variable, and eighteen dog-owners (20%) declared that they did not follow any infection control. Furthermore, over 70% of the interviewed handlers allowed the dog both to climb on patient’s bed and to lick patients. Finally, the dog owners were not aware of the potential zoonosis risks [45].
Two reviews [37], [39] considered the potential risks of animal use in healthcare settings, considering infections, allergies and bites. Precisely, Khan et al. considered the AAA or AAT implementation in healthcare settings, especially in hospitals [37]. The second review focused specifically on the healthcare environment of Europe and North America [39]. The zoonosis can be a risk especially for very young, old or immunosuppressed patients [37], [39]. All the animals mostly used in AAI can act as a source of infections. Not only zoonosis could be a risk, but also other common infections as MRSA. However, the application of hygiene protocols consented an effective risk minimization [39]. Moreover, the repeated health screenings for the animals and the careful selection of patients, using special precautions in case of open wounds and immunosuppression can help to control the risks [37]. Another risk is allergy; anyhow, the reasoned selection of patients and animals can effectively reduce this risk. Finally, animal-related accidents can be practically canceled following appropriate guidelines [39]. Therefore, the reviews concluded that the benefits overhang risks. In particular, Khan et al. recommended a careful selection of the patients, excluding patients with splenectomy, dog allergy, positive to Mycobacterium Tuberculosis, with pyrexia of unknown origin or infected with MRSA [37].
The guidelines about AAI and pet-visitation agreed over the main key points, suggesting hand hygiene after all animal contacts and avoiding as possible contacts with animal bodily fluids [16], [38], [39], [40], [41]. All animals used for AAT must be selected carefully, avoiding the most dangerous species as reptiles and primates [16]. Moreover, animals must follow strictly veterinary health screenings, vaccine programs, and be specifically trained for these activities. To minimize the allergic risk, bathing and grooming animals prior each session could be useful. After each session, routine cleaning protocols should be implemented. Finally, inclusion of patients with severe immunosuppression, known allergy or animal phobia should be carefully considered, assessing benefits and risks [16], [38], [39], [40], [41]. In particular, Sehulster et al. reported the CDC guidelines for environmental infection control in health-care facilities, including a section regarding the safety of AAA and resident animals programs in healthcare settings. On the contrary, in their guidelines [16], Sehr et al. considered exclusively a program of private pet-visitation in hospital. In this case, the authors excluded immunocompromised patients, newborns and patients in post-anesthesia care units. Moreover, the authors registered overall positive evaluations of the nurses regarding the guidelines implementation [38]. The work of Jofrè et al. consisted in a review of guidelines, in order to achieve a consensus regarding animal use in healthcare settings. As well as underlining the importance of regular veterinary checks and strict sanitary protocols, the authors recommended to avoid the use of puppies in order to minimize the infection risk [41]. Similar guidelines are adopted also in hospital implementation protocols [42], [43]. In particular, these programs excluded all patients in post-operative period, with recent splenectomy or severe immunosuppression [42]. Silveira et al. reported the implementation protocol of an AAA program in a Brazilian University hospital. This protocol included a wide range of potential employed animals, including dogs, cats, fishes, rabbits, reptiles and other rodents [42]. Similarly, Kobayashi et al. reported the Board of Nursery experience concerning the implementation of an AAT project in a University hospital. In particular, the authors adapted the CDC guidelines to their specific setting [43].
4. Discussion
Our review investigated the effectiveness and risks of animal assisted therapies in hospitals. Our search revealed extremely heterogeneous results, in terms of settings, target population, type of intervention and considered outcomes. However, most studies focused on particularly frail population groups as children [8], [22], [23], [24], [25], [26], [27], [28], psychiatric inpatients [10], [11], [19], [20], [21] and elderly patients [6], [7], [13], [14], [29]. The relationship with the animals can be extremely useful for these patients especially focusing on communication and social behaviours [7], [11], [28]. In particular, considering psychiatric diseases, schizophrenic inpatients would benefit from animal contact considering schizophrenic symptoms, social relationships and aggressiveness [10], [19], [21]. The reduction in aggressive behaviors was outlined, not only in psychiatric inpatients, but also considering general inpatients [35]. The studies regarding adults were rare, but they considered different diseases including orthopaedic surgery and high-risk pregnancies [31], [32], [33], [34], [35], [36].
Even if dogs are the most studied animals [8], [10], [11], [20], [21], [22], [23], [24], [25], [26], [27], [28], [31], [32], [33], [34], [35], [36], also other species are considered as cats [6], [44], fishes [14], cage birds [7] and horses [19]. The prevalent use of dogs is explained by the easier training for therapy; however, also other species can be potentially beneficial. Interestingly, the papers retrieved highlighted how “pet therapy” programs can be effectively implemented in a wide range of settings including Emergency Departments [34], long-term care facilities [6] and hospital wards [35]. Although all the interventions retrieved took place in hospitals or in long-term care facilities, the specific location of the interventions differed. Indeed, some interventions took place in the hospital garden [19] or in activity rooms specifically equipped [11], while others occurred directly in the ward [33], [34], or at bedside [25], [27]. Also considering the interventions’ characteristics, the results appeared variegated. In as much, the length of the sessions ranged from 5 to 10 minutes [32], [35] to different hours [24]. Moreover, some programs required multiple sessions [6], [8], [11], [21], while others included only a single session [13], [34]. These important organizational differences make extremely difficult to compare the retrieved intervention, and to draw clear conclusions. Furthermore, not all the studies exactly described the specific train and formation of the couple animal-therapist or handler. About this, some studies declared to adhere and follow the “Pet Partners Guidelines” [8], [19]. The AAT interventions resulted, in accordance to their definition, more structured, organized in limited groups and conducted by certified therapists. On the contrary, the described AAA ranged from simple pet-visitation to spontaneous activities. In this case, the specific formation of the couple dog-handler is less described, and in one case, the dogs are accompanied only by the investigators, and not by the handler [10].
Despite the wide range of outcomes considered, the studies retrieved outlined general benefits of AAT or AAA in terms of psychological and physical effects. In particular, one common outcome explored was anxiety. Positive effects on anxiety, measured using the STAI scale or the Profile of Mood States survey, were detected for various pathologies as major depression [20], hospitalized children [23], elderly patients with acute heart failure [13], high-risk pregnancies [33] and adult inpatients in different hospital departments [35]. The favorable effect of AAT upon anxiety symptoms on children was confirmed by parents and staff [8]. In conclusion, the favorable impact on inpatient anxiety seemed assessed for a wide range of age and conditions.
Another frequently assessed outcome was depression. Significant amelioration in depressive symptomatology was highlighted in psychiatric inpatients [19] and hospitalized women with at risk pregnancy [33]. In addition, an improvement in depression symptoms, even if not statistically significant, was observed for elderly institutionalized patients with age-related diseases [6]. The impact on depression required more in-depth analysis, especially considering the different scales used for its assessment.
Moreover, the pain (VAS scale, FACES scale or oral pain medication use) seemed to take advantage of animal therapeutic use in various conditions as post-orthopedic surgery [31], [32], hospitalized children in acute setting [26] and adult inpatient in different department [35]. The effective role of canine assisted therapy on pain was outlined both in surgical and medical conditions. However, not all the studies were concordant regarding this outcome. Indeed, Barker et al. did not find any difference in pain between intervention and control group in children [23].
Besides, the effects of AAI were assessed focusing on physiological parameters. The most assessed were blood pressure [6], [27], outlining a significant effect in decreasing this parameter, heart rate [13], [28], [35] and respiratory rate [13], [35]. However, the effect on blood pressure was not concordant in all studies. Indeed, Cole et al. did not identify any significant change in this parameter [13]. Another positive effect outlined was the actual distance walked in patients with chronic heart failure [29].
Therefore, the implementation of AAI can be interesting in a wide range of age and pathologies, but further and more standardized studies are required to exactly assess the pathologies mostly benefited from these interventions. The main limitations were linked to the heterogeneity of the retrieved studies considering both the outcomes and the quality, making the comparison quite difficult. Indeed, in accordance with previous reviews [4], [15], the previous cited findings are limited by the overall low quality of the retrieved studies. Indeed, only few works were RCTs. Moreover, most of the included papers presented limited samples that could affect the overall results. Therefore, more studies are required to completely describe the potential effects of AAI. In fact, some studies lacked of a control group [7], [14], [20], [33], while others were pilot studies considering limited samples [10], [11], [21]. Moreover, some papers lacked details of randomization [26], [33] or considered only parents or patients opinions [7], [8], [36]. Hospitals are particularly at risk settings, thus introducing animals has to be carefully considered. Various studies explored these risks outlining infections, allergies and animal accidents as major issues [16], [37], [38], [39], [40]. The potential risk of infections was outlined investigating the prevalence of infective agents in animals used for pet-visitation [17], [44]. These studies outlined the potential risk related not only to typical zoonosis, but also to common human infections as MRSA [17], [44]. However, reviews and guidelines suggested that the implementation of all security precautions could effectively minimize risks [16], [37], [38], [39], [40]. Therefore, the identification of patients receiving AAI should be carefully conducted. Some studies described in detail the sanitary protocols adopted for the animals involved, including regular veterinary visits, vaccination documentation and assessments of controllability and temperament [11], [23], [26], [35], [36]. On the contrary, other works did not explicitly refer to any of these procedures. This matter represents another limitation of our review. Indeed, detailed information regarding the health surveillance protocols are desirable in order to correctly evaluate the considered interventions. The extensive Canadian survey regarding dog visitation highlighted how the infection control protocols result variable and occasionally potentially inadequate. In particular, the knowledge concerning the potential risks amongst the dog-handlers seemed insufficient [45]. Consequently, a closer cooperation between hospital staff, AAI-team, and veterinarians seems necessary. In addition, stricter controls about AAI safety in the hospital are desirable.
Furthermore, the data regarding animal welfare during the intervention lacked in most of the studies. Then, it would be interesting to further deepen this topic, investigating, also, any adherence to specific guidelines. Another major concern was the acceptance of AAI programs among healthcare professional. However, all studies considering this issue identified a general acceptance by the staff [22], [34], [36].
5. Conclusions
In conclusion, AAT or AAA for hospitalized patients seem useful and safe for a wide range of diseases. However, many aspects remained unclear, in particular regarding the type of intervention, safety, economic issues and diseases that would greatly benefit of these programs. Finally, given the paucity of high quality works about this topic, it would be desirable to conduct more standardized studies considering in details outcomes and interventions in order to describe all the potential benefits and risks. Anyway, considering the intervention peculiarity, the reproducibility of randomized clinical trials could be difficult to achieve.
Ethical statement
The authors declare that they have no conflicts of interest. This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
None.
Conflict of interests
None
References
- 1.Levinson B.M. Pets and personality development. Psychol. Rep. 1978;42(June 1 (3c)):1031–1038. [Google Scholar]
- 2.Linee guida nazionali per gli interventi assistiti con gli animali (IAA) Conferenze Stato Regioni e Unificata [Internet] 2016 http://www.statoregioni.it/testo_print.asp?idprov=13952&iddoc=46922&tipoDoc=2 (cited 22.04.16) [Google Scholar]
- 3.Pet Partners.org – Therapy Pets & Animal Assisted Activities [Internet]. Available from: https://petpartners.org/learn/terminology/ (cited 22.04.16).
- 4.Kamioka H., Okada S., Tsutani K., Park H., Okuizumi H., Handa S., Oshio T., Park S.J., Kitayuguchi J., Abe T., Honda T., Mutoh Y. Effectiveness of animal-assisted therapy: a systematic review of randomized controlled trials. Complement. Ther. Med. 2014;22(April (2)):371–390. doi: 10.1016/j.ctim.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 5.Urbanski B.L., Lazenby M. Distress among hospitalized pediatric cancer patients modified by pet-therapy intervention to improve quality of life. J. Pediatr. Oncol. Nurs. 2012;29(October (5)):272–282. doi: 10.1177/1043454212455697. [DOI] [PubMed] [Google Scholar]
- 6.Stasi M.F., Amati D., Costa C., Resta D., Senepa G., Scarafioiti C., Aimonino N., Molaschi M. Pet-therapy: a trial for institutionalized frail elderly patients. Arch. Gerontol. Geriatr. 2004;9:407–412. doi: 10.1016/j.archger.2004.04.052. [DOI] [PubMed] [Google Scholar]
- 7.Falk H., Wijk H. Natural activity: an explorative study of the interplay between cage-birds and older people in a Swedish hospital setting. Int J Older People Nurs. 2008;3(March (1)):22–28. doi: 10.1111/j.1748-3743.2007.00090.x. [DOI] [PubMed] [Google Scholar]
- 8.Caprilli S., Messeri A. Animal-Assisted Activity at A. Meyer Children’s Hospital: A Pilot Study. Evid-Based Complement Altern Med ECAM. 2006;3(September (3)):379–383. doi: 10.1093/ecam/nel029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chur-Hansen A., McArthur M., Winefield H., Hanieh E., Hazel S. Animal-Assisted interventions in children’s hospitals: a critical review of the literature. Anthrozoös. 2014 Mar 1;27(1):5–18. [Google Scholar]
- 10.Chu C.-I., Liu C.-Y., Sun C.-T., Lin J. The effect of animal-assisted activity on inpatients with schizophrenia. J. Psychosoc. Nurs. Ment. Health Serv. 2009 Dec;47(12):42–48. doi: 10.3928/02793695-20091103-96. [DOI] [PubMed] [Google Scholar]
- 11.Stefanini M.C., Martino A., Allori P., Galeotti F., Tani F. The use of Animal-Assisted Therapy in adolescents with acute mental disorders: a randomized controlled study. Complement. Ther. Clin. Pract. 2015 Feb;21(1):42–46. doi: 10.1016/j.ctcp.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Orlandi M., Trangeled K., Mambrini A., Tagliani M., Ferrarini A., Zanetti L. Pet therapy effects on oncological day hospital patients undergoing chemotherapy treatment. Anticancer Res. 2007 Dec;27(6C):4301–4303. [PubMed] [Google Scholar]
- 13.Cole K.M., Gawlinski A., Steers N., Kotlerman J. Animal-assisted therapy in patients hospitalized with heart failure. Am. J. Crit. Care. 2016;6:575–585. (quiz 586; discussion 587-8) [PubMed] [Google Scholar]
- 14.Edwards N.E., Beck A.M. Animal-assisted therapy and Nutrition in Alzheimer’s disease. West. J. Nurs. Res. 2002;24(October (6)):697–712. doi: 10.1177/019394502320555430. [DOI] [PubMed] [Google Scholar]
- 15.Nimer J., Lundahl B. Animal-Assisted therapy: a meta-Analysis. Anthrozoös. 2007;20(September 1 (3)):225–238. [Google Scholar]
- 16.Sehulster L, Chinn RYW, CDC HICPAC. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep Cent Dis Control. 2003 Jun 6;52(RR-10):1-42. [PubMed]
- 17.Lefebvre S.L., Waltner-Toews D., Peregrine A.S., Reid-Smith R., Hodge L., Arroyo L.G. Prevalence of zoonotic agents in dogs visiting hospitalized people in Ontario: implications for infection control. J. Hosp. Infect. 2006 Apr;62(4):458–466. doi: 10.1016/j.jhin.2005.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J., Altman D.G. PRISMA Group: preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg Lond Engl. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Nurenberg J.R., Schleifer S.J., Shaffer T.M., Yellin M., Desai P.J., Amin R. Animal-assisted therapy with chronic psychiatric inpatients: equine-assisted psychotherapy and aggressive behavior. Psychiatr Serv Wash DC. 2015 Jan 1;66(1):80–86. doi: 10.1176/appi.ps.201300524. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann A.O.M., Lee A.H., Wertenauer F., Ricken R., Jansen J.J., Gallinat J. Dog-assisted intervention significantly reduces anxiety in hospitalized patients with major depression. Eur J Integr Med. 2009;1(3):145–148. [Google Scholar]
- 21.Victòria Villalta-Gil M.R. Dog-Assisted therapy in the treatment of chronic schizophrenia inpatients. Anthrozoos Multidiscip J Interact People Amp Anim. 2009;22(2):149–159. [Google Scholar]
- 22.Moody W.J., King R., O’Rourke S. Attitudes of paediatric medical ward staff to a dog visitation programme. J. Clin. Nurs. 2002 Jul;11(4):537–544. doi: 10.1046/j.1365-2702.2002.00618.x. [DOI] [PubMed] [Google Scholar]
- 23.Barker S.B., Knisely J.S., Schubert C.M., Green J.D., Ameringer S. The effect of an animal-Assisted intervention on anxiety and pain in hospitalized children. Anthrozoös. 2015;28(March 1 (1)):101–112. [Google Scholar]
- 24.Gagnon J., Bouchard F., Landry M., Belles-Isles M., Fortier M., Fillion L. Implementing a hospital-based animal therapy program for children with cancer: a descriptive study. Can Oncol Nurs J Rev Can Nurs Oncol. 2004;14(4):217–222. doi: 10.5737/1181912x144217222. [DOI] [PubMed] [Google Scholar]
- 25.Bouchard F., Landry M., Belles-Isles M., Gagnon J. A magical dream: a pilot project in animal-assisted therapy in pediatric oncology. Can Oncol Nurs J Rev Can Nurs Oncol. 2004;14(1):14–17. doi: 10.5737/1181912x1411417. [DOI] [PubMed] [Google Scholar]
- 26.Braun C., Stangler T., Narveson J., Pettingell S. Animal-assisted therapy as a pain relief intervention for children. Complement. Ther. Clin. Pract. 2009 May;15(2):105–109. doi: 10.1016/j.ctcp.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Tsai C.-C., Friedmann E., Thomas S.A. The effect of animal-Assisted therapy on stress responses in hospitalized children. Anthrozoös. 2010 Sep 1;23(3):245–258. [Google Scholar]
- 28.Kaminski M., Pellino T., Wish J. Play and pets: the physical and emotional impact of child-Life and pet therapy on hospitalized children. Child. Health Care. 2002;31(December 1 (4)):321–335. [Google Scholar]
- 29.Abate S.V., Zucconi M., Boxer B.A. Impact of canine-assisted ambulation on hospitalized chronic heart failure patients’ ambulation outcomes and satisfaction: a pilot study. J. Cardiovasc. Nurs. 2011 Jun;26(3):224–230. doi: 10.1097/JCN.0b013e3182010bd6. [DOI] [PubMed] [Google Scholar]
- 30.Kumasaka T., Masu H., Kataoka M., Numao A. Changes in patient mood through animal-Assisted activities in a palliative care unit. Int Med J. 2012;19(December (4)):373–377. [Google Scholar]
- 31.Harper C.M., Dong Y., Thornhill T.S., Wright J., Ready J., Brick G.W. Can therapy dogs improve pain and satisfaction after total joint arthroplasty? A randomized controlled trial. Clin. Orthop. 2015;473(January (1)):372–379. doi: 10.1007/s11999-014-3931-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Havey J., Vlasses F.R., Vlasses P.H., Ludwig-Beymer P., Hackbarth D. The effect of animal-Assisted therapy on pain medication use after joint replacement. Anthrozoös. 2014;27(September 1 (3)):361–369. [Google Scholar]
- 33.Lynch C.E., Magann E.F., Barringer S.N., Ounpraseuth S.T., Eastham D.G., Lewis S.D. Pet therapy program for antepartum high-risk pregnancies: a pilot study. J Perinatol Off J Calif Perinat Assoc. 2014;34(November (11)):816–818. doi: 10.1038/jp.2014.120. [DOI] [PubMed] [Google Scholar]
- 34.Nahm N., Lubin J., Lubin J., Bankwitz B.K., Castelaz M., Chen X. Therapy dogs in the emergency department. West J Emerg Med. 2012;13(September (4)):363–365. doi: 10.5811/westjem.2011.5.6574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coakley A.B., Mahoney E.K. Creating a therapeutic and healing environment with a pet therapy program. Complement. Ther. Clin. Pract. 2009;15(August (3)):141–146. doi: 10.1016/j.ctcp.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hastings T., Burris A., Hunt J., Purdue G., Arnoldo B. Pet therapy: a healing solution. J Burn Care Res Off Publ Am Burn Assoc. 2008;29(December (6)):874–876. doi: 10.1097/BCR.0b013e31818b9df8. [DOI] [PubMed] [Google Scholar]
- 37.Khan M.A., Farrag N. Animal-assisted activity and infection control implications in a healthcare setting. J. Hosp. Infect. 2000;46(September (1)):4–11. doi: 10.1053/jhin.2000.0785. [DOI] [PubMed] [Google Scholar]
- 38.Sehr J., Eisele-Hlubocky L., Junker R., Johns E., Birk D., Gaehle K. Family pet visitation. Am. J. Nurs. 2013;113(December (12)):54–59. doi: 10.1097/01.NAJ.0000438869.75401.21. [DOI] [PubMed] [Google Scholar]
- 39.Brodie S.J., Biley F.C., Shewring M. An exploration of the potential risks associated with using pet therapy in healthcare settings. J. Clin. Nurs. 2002;11(July (4)):444–456. doi: 10.1046/j.1365-2702.2002.00628.x. [DOI] [PubMed] [Google Scholar]
- 40.DiSalvo H., Haiduven D., Johnson N., Reyes V.V., Hench C.P., Shaw R. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am. J. Infect. Control. 2006;34(June (5)):301–307. doi: 10.1016/j.ajic.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 41.Jofré M.L. Animal- assisted therapy in health care facilities. Rev Chil Infectol érgano Of Soc Chil Infectol. 2005;22(September (3)):257–263. doi: 10.4067/s0716-10182005000300007. [DOI] [PubMed] [Google Scholar]
- 42.Silveira I.R., Santos N.C., Linhares D.R. Protocol of the animal assisted activity program at a university hospital. Rev Esc Enferm U P. 2011;45(March (1)):283–288. doi: 10.1590/s0080-62342011000100040. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi C.T., Ushiyama S.T., Fakih F.T., Robles R.A.M., Carneiro I.A., Carmagnani M.I.S. Development and implementation of Animals-Assisted Therapy in a university hospital. Rev. Bras. Enferm. 2009;62(August (4)):632–636. doi: 10.1590/s0034-71672009000400024. [DOI] [PubMed] [Google Scholar]
- 44.Coughlan K., Olsen K.E., Boxrud D., Bender J.B. Methicillin-resistant Staphylococcus aureus in resident animals of a long-term care facility. Zoonoses Public Health. 2010;57(May (3)):220–226. doi: 10.1111/j.1863-2378.2009.01302.x. [DOI] [PubMed] [Google Scholar]
- 45.Lefebvre S.L., Waltner-Toews D., Peregrine A., Reid-Smith R., Hodge L., Weese J.S. Characteristics of programs involving canine visitation of hospitalized people in Ontario. Infect. Control Hosp. Epidemiol. 2006;27(July (7)):754–758. doi: 10.1086/505099. [DOI] [PubMed] [Google Scholar]