Abstract
Coronavirus disease 2019 is an infectious disease caused by severe acute respiratory syndrome coronavirus 2. It has taken a toll of lots of lives since its outbreak. Infection prevention at present is an appropriate control measure in addition to other measure like hand hygiene and personal protective equipment (PPE). In our country with a large population, supplying PPE to all the health care workers of all hospitals definitely is an economic burden. Hence we have come up with an economic and simple solution for face mask.
Electronic supplementary material
The online version of this article (10.1007/s12070-020-01863-4) contains supplementary material, which is available to authorized users.
Keywords: COVID 19, Personal protective equipment (PPE), Face mask, Global health, Public health
Introduction
The 2019 novel coronavirus disease (COVID-19), with an epidemic centered in Wuhan, China, was declared a public health emergency on January 20, 2020, by the World Health Organization and a public health emergency by the US on January 31, 2020. A total of 463,412 cases worldwide and 20,912 deaths till now. [1] Amongst the currently Infected Patients, 328,698 a total of 314,319 (96%) have mild Condition and 14,379 (4%) are serious or critical. Amongst the closed cases of 134,714, the mortality was in 20,912 (16%) [1]. The early reported mortality rate of 4.3% [2] appears to be lower than that of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome, but this initial figure is believed likely to be an underestimation, as most of the confirmed patients are still inpatients, and their condition is not yet resolved. Common symptoms include fever, cough, and shortness of breath. Muscle pain, sputum production, diarrhea, and sore throat are less common. [3] While the majority of cases result in mild symptoms, some progress to pneumonia and multi-organ failure [4].
Based on current evidence, it is speculated that respiratory droplets and possibly feco-oral routes are culprits for the mode of transmission, similar to the SARS epidemic in 2003. [5, 6] With the outbreak of COVID 19, there has been redistribution of manpower and resources to critically meet the current and anticipated hospital service needs. Due to total lockdown announced in our country, the patients availing the medical help for minor ailments has been reduced considerably. Also all the elective surgical procedures have been postponed for a month or so as to avoid unnecessary overcrowding and possible exposure and spread of coronavirus. There has also been a reduction in elective clinics and operations to mobilize manpower to acute specialties combatting the outbreak and maximize hospital beds numbers available in anticipation of the outbreak. There is also understandably fear from the public in visiting hospitals.
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2. It has taken a lot of lives since its outbreak. This outbreak has additionally seen a high morbidity among healthcare workers, much like previous outbreaks of human coronavirus. The first fatality of a physician documented globally was that of an otolaryngology physician in Wuhan on January 25, 2020, whose situation was similar to that of an otolaryngologist who died of SARS in 2003. Thus, it is important that otolaryngologists and physicians globally stay abreast of this outbreak and realise the need for essential precautionary practices that are potentially crucial in protecting themselves and patients during this epidemic. In many regions globally, it is a very common practice for patients with upper respiratory tract infections to seek family practitioners and otolaryngologists as a primary care physician. Such a practice inadvertently poses inherent potentiall risks for physicians examining patients potentially carrying the virus.
Considering the pandemic outbreak of COVID 19, and its virility at present there is no vaccine or any other treatment for this deadly virus. Infection prevention at present is an appropriate control measure in addition to other measure like hand hygiene, personal protective equipment (PPE) and waste management materials.
An area of particular concern for use of Personal Protective Equipment (PPE) in Otolaryngolgy field is aerosol-generating procedures that would include open systems for tracheostomies and possibly the performance of flexible laryngoscopy. The Protective equipment consists of garments placed to protect the health care workers or any other persons to get infected. Personal Protective Equipment (PPE) is most important in preventing transmission of the virus. These usually consist of standard precautionary measures like gloves, mask and gown. For blood or airborne high infections, it includes: face protection, goggles and mask or face shield, gloves, gown or coverall, head cover, rubber boots.
With the current COVID-19 outbreak in our country and our region of Maharashtra, India, all outpatient clinic patients are seen by Otolaryngologists and Physicians wearing minimum an N95 mask and gloves. Considering the situation in developing countries like ours there is economic burden of providing the PPE to all the health care professionals (including doctors, nursing staff, supporting staff, ICU technicians, laboratory technicians), law handling forces (police and soldiers who manage the mobs during the Lockdown), infected and non-infected patients and their relatives. It’s a tremendous health care burden protecting all these key people who are prone to risk of exposure. We need simple solutions and it is the responsibility of the Government to take care of all the people at risk. So finding a simple economical solution is a must in all the developing countries and to provide the safety protection equipment to one and all to prevent the spread of COVID 19. In our country with a large population, supplying PPE to all the health care workers of all hospitals definitely is an economic burden. There is need for cheap, disposable face masks, eye protection, gloves and gowns, enough safety gear for medical workers, sick people and for the public. Procurement of such large amount of protection wear is difficult as it runs out of stock due to high demands. There is a tremendous need that the masks and the protection wear to be prepared by the health workers for self-protection. With a continuous and constant contemplation, we have come up with a solution, which is economic, simple solution as well as easily prepared. We have designed a face mask which will cover not only nose and mouth but also the whole of the face thereby preventing the exposure to the eyes, nose, mouth and face.
Our Solution for the Existing Crises of PPE
We recommend a very economical face protection mask as a safety barrier to prevent contact/exposure to the corona virus. It would be a better alternative other than no protection at all. It will definitely save many lives of the health care workers working selflessly for the community during the COVID 19 pandemic.
Method of Preparation of the Face Mask (Figs. 1, 2, 3 and video and sketches)
Fig. 1.

Our face mask: the design
Fig. 2.

Side view of the face mask
Fig. 3.

Front view of our mask
We propose the use of A4 size OHP transparency plastic slide and a regular cloth mask (or disposable mask) for it. It can be prepared by dividing the A4 size OHP transparency sheet across length into half (measuring 30 cm × 10 cm) and to be sewn to mask in its upper half (sketch diagrams where blue is cloth mask and red is A4 half sheet). The cloth mask can be double folded made of cloth (either cotton or polyester). Punch holes are made on the opposite two sides of the transparent plastic OHP transparency paper. Passing strings through these punched holes would help to fasten the face mask onto face and secure at the back of the head with the knotting of the strings. It would form an effective barrier protecting the exposure of eyes (corneal), nasal, buccal mucosa as well as skin of face.
We have 4 possible options for the face masks (Figs. 1, 2, 3):
Routine disposable mask attached/sewn to the transparent OHP sheet superiorly with strings to be secured posteriorly.
N95 mask attached sewn to the transparent OHP sheet superiorly with strings to be secured posteriorly.
Cotton Cloth/double layer of polyester cloth mask sewn to the transparent OHP sheet superiorly with strings to be secured posteriorly.
Mask of any type (routine disposable mask/N95 mask/cloth mask) with separate overlay of transparent OHP sheet superiorly with strings to be secured posteriorly.
OUR proposed simplest way of preparing the face shields (Figs. 4, 5, 6).
Take A4 size OHP sheet of 150 to 200 micron thickness.
With office punching machine, make 8 holes across length of OHP sheet leaving 2 cm margin.
Thread cotton ribbon gauze of 60 cm alternately through created holes for tying around head.
Fig. 4.

Our face shield
Fig. 5.

Tying of face shield behind with a knot
Fig. 6.

Front view of our face shield
Safety considerations for Face shields/masks during COVID 19 Pandemic
Snug fitting. The face shield must be snugly fitting around head without any gaps between forehead and shield. Use of sponge in between forehead and face shield gives good comfort, but such face shields should be used as disposable as sterilisation of sponge is incomplete.
Disposable/Reusable. In case of disposable face shield, removal to be done with utmost care and dispose properly. In case of reusable Face Shields, utmost care to be taken while removing the shield after use as well as sterilisation before reuse.
Quality of Material for face shield. Best thickness is OHP of 150 to 200 micron.
Methods of Handling. Never touch the front side of face shield and dispose after untying the knot from behind along with gloves.
Avoid all supplementary materials like sponge, stapler pins, sticking materials and adhesives.
Sterilisation
Two types:
Disposable: stich this to present surgical mask and throw after use.
Reusable: double cloth of polyester or Cotton with Transparent A 4 trace paper.
For Sterilisation
After use soak in 70% isopropyl alcohol. Wash it with detergent soap.
2% glutaraldehyde activated. Keep in it for 10 min. Wash it with Detergent soap.
ETO sterilisation is best and will increase longevity of masks.
1% Sodium Hypochlorite solution for minimum of 10 min.
*Strictly No Autoclave*.
Sketch Diagrams (Figs. 7, 8)
Fig. 7.
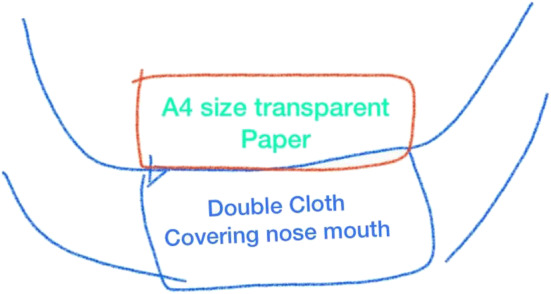
Sketch of our mask
Fig. 8.
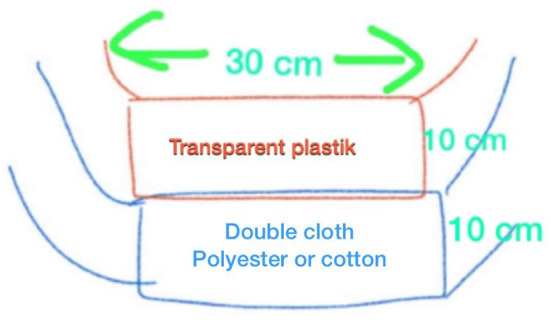
Sketch of our mask
Discussion
The mode of transmission is by respiratory droplets and by feco-oral route. The respiratory droplet transmission is very rapid if no barrier is present. It can be prevented by the use of masks. With the ongoing pandemic, there is an extreme shortage of masks not only in developing countries but also in the affluent developed countries with a demand and supply mismatch. With the disposable masks available in the market are running out of stock as the demand is more of such masks. As a result of which, the health care workers exposed to the suspected/potential COVID 19 patients are deprived of even masks. In such situations, the PPE is definitely out of question. Under these circumstances, it is of immense importance that the health care workers use at least some sort of protection or a barrier and thus prevent exposure and thus the risks. Our mask, though a simple one, definitely serves as a protection and effective barrier than no protection at all. It can be used in adjunct with the N95 mask, or a simple disposable mask or a simple double folded polyester cloth mask. Such masks can be prepared by the hospital staff within the hospital itself and can be sterilised too as mentioned in quantity as required by the staff. So it wouldn’t increase the burden on the economy of the country and makes the health care workers self-sufficient. It obviates the need for additional eye wear by the health care workers. It can also be supplemented by the wearing of disposable gowns as an additional protection.
Conclusion
With the extreme shortage of the N95 masks and other disposable masks, our simple and economic option for preparing our own effective barrier face masks and face shields by use of OHP transparent sheet and the routine masks will help to tide over the crises of the mask shortage as well as serve as a PPE.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 13,042 kb)
Funding
This study was not financially supported from external sources
Compliance with Ethical Standards
Conflict of interest
All authors declare that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.https://www.worldometers.info/coronavirus/
- 2.Wang D, Hu B, Hu C, et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. Published online February 7, 2020. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed]
- 3.Miri SM, Roozbeh F, Omrani A, Alavian SM (2020). “Panic of buying toilet papers: a historical memory or a horrible truth? systematic review of gastrointestinal manifestations of COVID-19”. Hepatitis Monthly. In Press (In Press). 10.5812/hepatmon.102729. ISSN 1735-143X.
- 4.“Q&A on coronaviruses”. World Health Organization (WHO). Archived from the original on 20 January 2020. Retrieved 27 January 2020
- 5.Chan PK, Ip M, Ng KC, et al. Severe acute respiratory syndrome-associated coronavirus infection. Emerg Infect Dis. 2003;9(11):1453–1454. doi: 10.3201/eid0911.030421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drosten C, Günther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348(20):1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1 (MP4 13,042 kb)


