Abstract
Objectives:
Ligation and excision remain the commonly recognized standard surgical modality for treating hemorrhoids. Further, impediments to surgical treatment owing to social factors and the need for minimally invasive procedures and other confounders have resulted in the adoption of the mucopexy-recto anal lifting (MuRAL) method which is associated with favorable outcomes. The objective of this study was to describe the procedure and report the outcomes in patients who underwent MuRAL.
Methods:
Between March 2016 and February 2018, 55 patients (26 males and 29 females) underwent MuRAL for hemorrhoids and rectal mucosal prolapse. The duration of the surgical procedure and hospitalization, postoperative complications, and satisfaction were evaluated.
Results:
The mean age of the male patients (n = 26) was 61.5 ± 4.9 years and that of the female patients (n = 29) was 61.5 ± 3.2 years. The mean duration of surgery was 46 ± 23 minutes for males and 53 ± 28 minutes for females, and the mean observation duration was 317 ± 186 days. Intraoperative hemorrhage was low for males and females. The mean hospitalization period was 3.2 ± 1.5 days for males and 4.3 ± 2.1 days for females. Differences in several postoperative complications were observed between male and female patients. Postoperative satisfaction was rated high by the patients.
Conclusions:
Risks of hemorrhage and pain associated with the MuRAL method were low because the procedure does not involve incision or excision. Other than ligation and excision, recurrence is favorable compared with that of other surgical modalities for the treatment of hemorrhoids.
Keywords: hemorrhoids, mucopexy-recto anal lifting, MuRAL
Introduction
Ligation and excision is the standard surgical modality for treating hemorrhoids[1]. Recently, aluminum potassium sulfate and tannic acid (ALTA) injection is being increasingly favored owing to the ease of performing this minimally invasive therapeutic modality[2-5]. In Japan, another minimally invasive procedure for treating hemorrhoids is hemorrhoidal artery ligation using a special instrument (Moricorn) developed by Morinaga et al. in 1995[6]. In Western countries, transanal hemorrhoidal dearterialisation, developed by Dal Monte et al. in 2007[7], and Doppler-guided recto anal repair, developed by Scheyer et al. in 2008, in which hemorrhoidal arteries are ligated by Doppler-guided hemorrhoidal artery ligation[8], are used in common practice. However, Doppler-guided surgeries require complicated skills, and instances of recurrence of hemorrhoids have been reported[7-10].
Since March 2016, when our institution adopted a new technique, mucopexy-recto anal lifting (MuRAL) using HemorPex SystemⓇ (HPS), we have achieved favorable outcomes for treating hemorrhoids. Here, we describe cases of patients for whom MuRAL was performed and discuss the advantages and limitations of the procedure.
Methods
Description of the MuRAL method
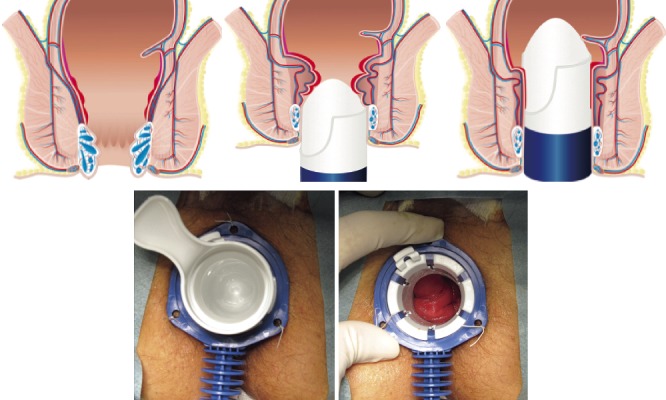
The origin of the MuRAL method traces back to when the HPS technique was reported in Italy by Iachino et al. in 2009[11]. This technique involves continuous suturing and lifting of the internal hemorrhoidal tissue containing hemorrhoidal arteries using HPS (Angiologica B.M). Thereafter, Pagano et al. improved the HPS technique and reported the MuRAL method in 2018. Currently, MuRAL is performed using the HemorPex SystemⓇ Plus, (Angiologica B.M), henceforth referred to as HPS Plus, which is an improved version of HPS. The rotor in HPS Plus can only rotate if the inner cylinder is properly inserted. This prevents a situation that is seen with the older system, wherein the rectal mucosa is damaged because it is caught in a rotating rotor without the inner cylinder inserted. Another major improvement from the HPS is that the main unit is white, which renders it easier to macroscopically observe the suture site with enhanced luminosity (Figure 1).
Figure 1.
HemorPex System®: HPS.
The procedures for the MuRAL method[12,13] are as follows. Any use of steroidal suppositories and ointments should be halted 2-3 weeks prior to surgery because their long-term use may debilitate the rectal mucosa. Suturing under a weakened condition may easily rupture the suture site, resulting in hemorrhage and insufficient suturing effects. As preoperative treatment, glycerin enema is administered. Given the possibility of intraoperative fecal contamination, irritant cathartics, such as sodium picosulfate, should not be used. For inducing anesthesia, concomitant use of local anesthetics and sedatives is recommended.
According to the HPS technique report, the recommended operative position is the jackknife position[11]. However, patients in the jackknife position are prone to drooping of the rectal mucosa toward the anus, rendering it difficult to achieve sufficient replacement of the rectal mucosa during the surgery. Therefore, the lithotomy position is preferred considering the risk of recurrence. The HPS Plus device is inserted protectively into the anal canal. With this procedure, the prolapsing hemorrhoids and rectal mucosa are lifted adorally, thereby achieving physiological mucosal replacement in the intestinal longitudinal direction (Figure 2). Then, the three fixation holes and skin are fixed with silk threads, fixing the suturing site, and the intervals are homogenized in the ensuing surgery. These procedures are difficult to perform using a slit-type proctoscope. In the basic modality, six points are lifted in the following order: 11 o'clock, 1 o'clock, 9 o'clock, 3 o'clock, 7 o'clock, and 5 o'clock. In cases with marked loosening of the rectal mucosa, such as hemorrhoids and rectal mucosal prolapse, and cases of female patients with concomitant rectocele, seven points are lifted starting in the 12 o'clock direction (Figure 3). To lift each point, for example toward the 11 o'clock direction, the rotor is first rotated toward the 1 o'clock or 9 o'clock direction and then returned to the 11 o'clock direction. This procedure reverses the ‘horizontal shift’ that occurs in the mucous membrane by one-directional rotation of the rotor to the normal position.
Figure 2.
HemorPex System Plus® insertion and rectal mucosal replacement. Image from Mucopexy-Recto Anal Lifting Clinical Applications Handbook Digital Edition, Pagano C and Serfezi C (©2018) https://www.mural-procedure.org. Reprint permission was granted.
Figure 3.
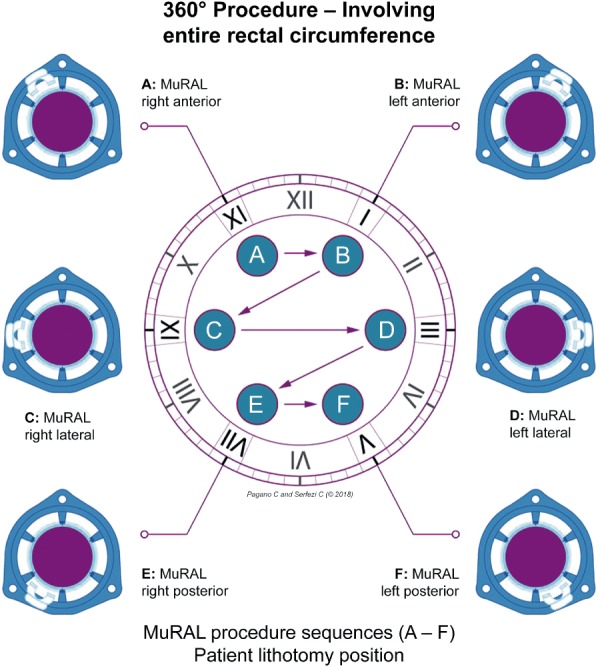
Suture sites and order of the MuRAL method. Image from Mucopexy-Recto Anal Lifting Clinical Applications Handbook Digital Edition, Pagano C and Serfezi C (©2018) https://www.mural-procedure.org. Reprint permission was granted.
The rotor is rotated to the surgical site; then, the inner cylinder is removed. Once the rectal mucosa is observed through the window, the rectal mucosa is pulled further adorally with tweezers or similar tools to securely replace the mucosal membrane. When the lower edge of the window is approximately 2 cm adorally from the dentate line, the device pierces through this site using 0-VICRYL, and the distal branch of the superior rectal artery is ligated adorally to complete the Z-suture (Figure 4).
Figure 4.
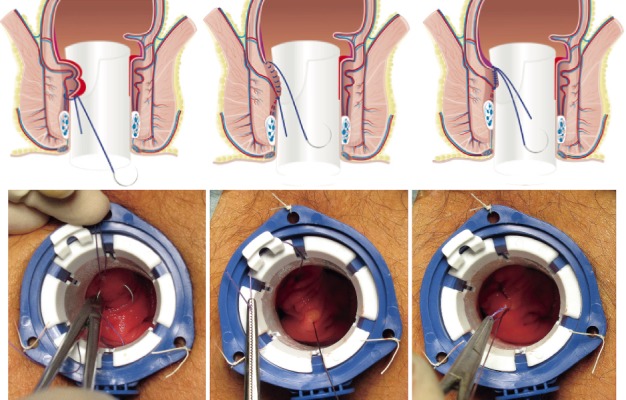
Ligation of the distal branch of the superior rectal artery and lifting of the rectal mucosa. All upper images are from Mucopexy-Recto Anal Lifting Clinical Applications Handbook Digital Edition, Pagano C and Serfezi C (©2018) https://www.mural-procedure.org. Reprint permission was granted.
Subsequently, continuous suture is performed beneath the mucous membrane of the adoral rectal mucosa. The suture width is 2-4 mm, with the footsteps being within 1 cm. If the hemorrhoids are large or are strongly loosened, the suture tends to be rough with broader suture width and footsteps. When the needle is caught in a muscle layer, the folded tissue becomes thick, resulting in insufficient suturing effects, or mucosal irregularity is caused after the wound is healed. Therefore, this part of the procedure requires utmost attention.
Proceeding with continuous suturing in the adoral direction tends to result in a reddish and rough surface of the mucous membrane after repeated prolapse, and normal intestinal mucosa tends to be whitish with clear borders. The needle should not be moved beyond the normal rectal mucosa (Figure 4). If the borders are obscure, the musculus puborectalis should roughly indicate where ligation is performed toward the anal side. This helps reduce the incidence of postoperative hypogastric pain caused by pulling of the peritoneal membrane. At this point, the rectal mucosa is lifted in the adoral direction, and finally, ligation is performed further toward the anal side than the first Z-suture site to complete the final suture (Figure 5). After six or seven points are lifted, all points are checked again to ensure that there is no hemorrhage. If there is hemorrhage, the bleeding site is Z-sutured to achieve hemostasis. However, achieving hemostasis is not required in most cases. After surgery, the patient, while at rest, is followed-up for several hours for signs of progress before being discharged home. Depending on the age and general condition of the patient, follow-up should continue overnight.
Figure 5.
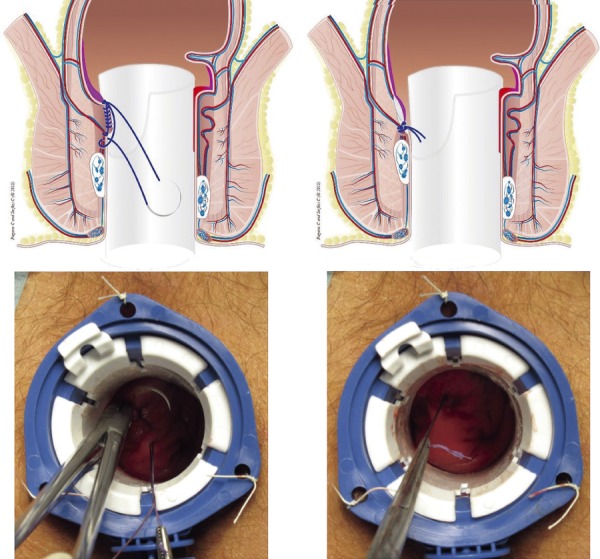
Final suture of the rectal mucosa. All upper images are from Mucopexy-Recto Anal Lifting Clinical Applications Handbook Digital Edition, Pagano C and Serfezi C (©2018) https://www.mural-procedure.org. Reprint permission was granted.
Between March 2016 and February 2018, 55 patients (26 males and 29 females) underwent MuRAL for hemorrhoids (Goligher grade III) and rectal mucosal prolapse at our institution. For these patients, the duration of the surgical procedure and hospitalization, postoperative complications, and satisfaction (satisfied, slightly satisfied, neutral, slightly unsatisfied, and unsatisfied) were evaluated.
On the day of surgery, each patient who presented at the hospital received 200 mL glycerin enema as preoperative treatment. The patient was not required to ingest a cathartic on the day prior to the surgery. General anesthesia was induced by concomitant use of saddle block, inhaled anesthetics, and intravenous anesthetics. The lithotomy position was preferred during surgery. Postoperatively, the patients were hospitalized for 2-5 days to check for pain, hemorrhage, and defecation. During the ambulatory care period, they were followed-up biweekly to examine if the suture was absorbed, if cicatricial contraction occurred, if normal defecation was restored, and if there was a relapse (Figure 6).
Figure 6.
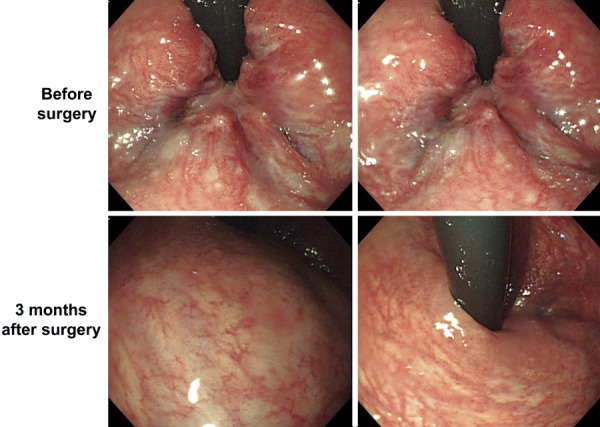
Before and after performing the MuRAL method.
The study on this surgical procedure was reviewed and approved by the Institutional Review Board of the Matsushima Hospital Colo-proctology Centre (Approval Number: 2016-011).
Results
The mean age of the male patients (n = 26) was 61.5 ± 4.9 years and that of the female patients (n = 29) was 61.5 ± 3.2 years. The mean duration of surgery was 46 ± 23 minutes in males and 53 ± 28 minutes in females, and the mean observation duration was 317 ± 186 days. Intraoperative hemorrhage was low for both males and females in the study, and the mean hospitalization period was 3.2 ± 1.5 days in males and 4.3 ± 2.1 days in females. Postoperative complications occurred in one male patient (3.8%, postoperative hemorrhage) and in no female patient; postoperative hypogastric pain occurred in 8 males (30.8%) and 26 females (89.7%); the postoperative anodyne administration period was 3.7 ± 2.3 days in males and 5.3 ± 3.1 days in females; and postoperative relapse occurred in none of the males but in 3 females (10%). The degrees of postoperative satisfaction were as follows: 17 males (65.4%) and 21 females (72.4%) were satisfied; 6 males (23.1%) and 3 females (10.3%) were slightly satisfied; 3 males (11.5%) and 2 females (6.9%) were neutral; 0 males and 1 female (3.4%) were slightly unsatisfied; and 0 males and 2 females (6.9%) were unsatisfied.
Discussion
Duration of surgery
The time required for surgery tended to be longer in females than in males because seven points (including the 12 o'clock direction) had to be lifted in all female cases. Pagano et al. performed MuRAL in 126 patients and reported the mean operation time to be 29.5 (23-60) minutes[12]. At our institution, the first case took approximately 1 hour and 20 minutes for surgery; however, the duration of surgery decreased with repeated surgeries. Currently, surgeons at our institution can complete one surgical session in approximately 30-40 minutes. Although MuRAL takes longer to complete than the three-point ligation and excision method[1,12], its duration is still within the acceptable range. It should be noted that for MuRAL, it takes longer to complete non-surgical procedures, such as introducing anesthesia and securing the lithotomy position, compared with the normal ligation and excision method.
Intraoperative hemorrhage
Because MuRAL involves neither incision nor excision, none of the patients experienced any uncontrolled bleeding and the intraoperative bleeding was minimal. Ligation and excision is usually associated with about 20-60 mL of intraoperative bleeding[14,15], which makes MuRAL more advantageous over ligation and excision.
Mean hospitalization period
Pagano et al. reported that 92 of 126 patients (73%) were able to return home on the day of surgery[12]. Our institution currently performs MuRAL by concomitantly using saddle block and general anesthesia, and therefore, discharging the patient on the same day of surgery is infeasible. Because careful postoperative observation was necessary after MuRAL was performed, all patients were hospitalized for undergoing surgery. Therefore, MuRAL has an advantage in this regard because, in comparison, the ligation and excision modality usually require the patient to be hospitalized for 7-10 days. In addition, MuRAL is possible with the use of recommended local anesthetics and intravenous anesthetics. Therefore, in the future, patients may be discharged on the same day or after an overnight stay. Therefore, MuRAL may be performed at outpatient departments in bedless proctology clinics.
Postoperative hemorrhage
Postoperative hemorrhage is relatively favorable compared with that of other modalities[1]. The male patient who experienced hemorrhage had undergone ligation and excision twice in the past and had received blood transfusion and hemostasis on both occasions owing to postoperative hemorrhage; therefore, this case was exceptional. Overall, the MuRAL method is a surgical modality associated with a lower risk of postoperative hemorrhage than the ligation and excision method.
Postoperative pain
A characteristic postoperative symptom following MuRAL is the dragging pain in the peritoneal membrane accompanied by lifting of the rectal mucosa. Because of the improvements made to HPS Plus, the boundaries between the unhealthy and healthy mucous membrane parts became relatively easier to discern. Pagano et al. reported that lifting only the unhealthy part of the mucosa rather than reaching toward the healthy part helps avoid the occurrence of postoperative hypogastric pain[12]. Nevertheless, there were many cases of patients experiencing postoperative hypogastric pain at our institution, 8 males (30.8%) and 26 females (89.7%). This may be attributed to the anatomic characteristics of the Japanese individuals or the suture of the puborectalis toward the abdominal side. Future studies are necessary to clarify this. However, patients complained of pain within 2 days of surgery at the latest, and improvement was seen in most cases by analgesic administration on the same day of surgery.
Following normal ligation and excision, analgesic administration is necessary for 2-3 weeks after surgery. Conversely, MuRAL required shorter analgesic administration periods. Therefore, the MuRAL method is advantageous from the perspective of postoperative pain management.
Postoperative recurrence
Pagano et al. reported a one-year recurrence rate of 4.1% (mean follow-up period: 554 days). At our institution, no male patients and 3 female patients (10%) experienced postoperative recurrence (in total, 3/55 [5.5%]). There were two cases of rectal prolapse and one of mass prolapse. Currently, our hospital performs the MuRAL method for hemorrhoids mainly with rectal mucosal prolapse (Goligher grades III-IV). The two patients with rectal prolapse might have had rectal prolapse prior to surgery; therefore, preoperative evaluation was insufficient. The one case with a mass prolapse had a large stitch width of the mucous membrane during surgery. The mass-like change of the suture site was caught in a part of the muscle layer, which was prolapsed by defecation. After this induration site was excised, the symptom improved. All recurrent cases would have been preventable if an accurate preoperative diagnosis had been provided and a proper modality had been selected. Based on the lessons learned, we predict a further decrease in the recurrence in the future, which will require long-term follow-up; however, the cases evaluated in this study were not postoperative long-term follow-up cases. From the above, MuRAL is indicated for Goligher grades II and grades III internal hemorrhoids and preoperative evaluation is necessary for rectal prolapse. For external hemorrhoids, additional treatment such as resection is considered necessary. And it is considered to be a good indication for rectal mucosal prolapse (including WHA). According to the hemorrhoidal artery ligation/RAR report, the recurrence rate was as high as 4%-40%[6-10], suggesting that Doppler-guided ligation is not essential. In addition, Rubber band ligation, which is one of the non-invasive treatments for hemorrhoids, has a recurrence rate as high as 30% to 49%[16,17], and Procedure for prolapsed and hemorrhoids, which has been reported in Japan before, has reported a recurrence of around 10%[18-20]. In Japan, a recurrence rate of 4%-16% was report with ALTA therapy[2-5], indicating the effectiveness of the MuRAL method.
Postoperative satisfaction
Pagano et al. reported postoperative satisfaction as follows: excellent, 31.1%; good, 57.4%; fairly good, 7.4%; and poor, 4.1%[12]. With >80% of the patients in this study responding favorably, the MuRAL method may be considered to be a modality providing a high level of satisfaction to patients.
Other complications
No noteworthy postoperative complications, including urination disorders, were observed. Conversely, Pagano et al. reported that 22 patients (18%) experienced postoperative urination disorder[12].
In conclusion, ligation and excision is the most radical surgical technique, which remains the gold standard for treating hemorrhoids[1], and is compatible with any type of hemorrhoid. However, the incidence of postoperative pain and hemorrhage associated with this modality is higher than that associated with other modalities. Moreover, advanced age and mental impairment are confounding factors that result in poor postoperative management. In Japan, the ALTA therapy is currently offered in many institutions, but because it involves drug infusion, problems arise owing to patient-specific responsivity, inferior radical cure and serious complications[2-5]. The MuRAL method can alleviate postoperative pain and hemorrhage and reduce social burdens such as long-term hospitalization, particularly when social factors prevent hospitalized care. The MuRAL method does not involve drug infusion, thereby rendering it safe. However, because the recurrence rate with the MuRAL method is higher than that with ligation and excision[1], surgical indications need to be established. Another limitation of MuRAL is the cost because the HPS Plus is an expensive apparatus (JPY: 32,000), making universal application cost-ineffective, warranting the need for insurance coverage of this highly effective procedure for a common ailment.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
All authors listed in the manuscript meet the ICMJE contribution criteria.
Approval by Institutional Review Board (IRB)
The study on this surgical procedure was reviewed and approved by the Institutional Review Board of Matsushima Hospital Colo-proctology Centre (Approval Number: 2016-011).
Disclaimer
Kosuke Okamoto and Yasuhiro Shimojima are Associate Editors of Journal of the Anus, Rectum and Colon and on the journal's Editorial Board. They were not involved in the editorial evaluation or decision to accept this article for publication at all.
Acknowledgements
The authors thank Dr. Claudio Pagano, Carmen Serfezi, and Michael Bobrove for their guidance and support, and Crimson Interactive Pvt. Ltd. (Ulatus)―www.ulatus.jp―for their assistance in manuscript translation and editing.
References
- 1.Matsushima M, Simojima Y. [Is haemorrhoid ligation and excision the gold standard? Basic techniques and evidence of ligation and excision]. J Jpn Soc Coloproctol. 2010; 63(10): 831-7. Japanese. [Google Scholar]
- 2.Saito T, Sasaki H, Tokunaga Y. [Inner haemorrhoid induration therapy]. J Clin Surg. 2008; 63: 111-7. Japanese. [Google Scholar]
- 3.Tsuji N. [Effectiveness of haemorrhoid ligation and excision and ALTA for haemorrhoids]. Surgical Therapy. 2008; 99: 301-4. Japanese. [Google Scholar]
- 4.Hachiro Y, Abe T, Kunimoto M. [ALTA induration therapy for anal diseases- after experiencing 1000 cases]. J Jpn Soc Coloproctol. 2008; 61: 216-20. [Google Scholar]
- 5.Abe T, Hachiro Y, Kunimoto M. [Comparison between ALTA therapy and ligation and excision for inner haemorrhoids]. J Jpn Soc Coloproctol. 2007; 60: 213-7. Japanese. [Google Scholar]
- 6.Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised. Am J Gastroenterol. 1995 Apr; 90(4): 610-3. [PubMed] [Google Scholar]
- 7.Dal Monte PP, Taqariello C, Sarago M, et al. Transanal haemorrhoidal dearterialization: nonexcisional surgery for the treatment of haemorrhoidal disease. Tech Coloproctol. 2007 Dec; 11(4): 333-8. [DOI] [PubMed] [Google Scholar]
- 8.Scheyer M. Doppler-guided recto-anal repair: a new minimally invasive treatment of hemorrhoidal disease of all grades according to Scheyer and Arnold. Gastroenterol Clin Biol. 2008 Jun-Jul; 32(6-7): 664. [DOI] [PubMed] [Google Scholar]
- 9.Ratto C, Parello A, Veronese E, et al. Doppler-guided transanal haemorrhoidal dearterialization for haemorrhoids: results from a multicenter trial. Colorectal Dis. 2015 Jan; 17(1): O10-9. [DOI] [PubMed] [Google Scholar]
- 10.Theodoropoulos GE, Sevrisarianos N, Paraconstantinous J, et al. Doppler-guided haemorrhoidal artery ligation, rectoanal repair, sutured Haemorrhoidopexy and minimal mucocutaneous excision for grades III-IV Haemorrhoids: a multicenter prospective study of safety and efficacy. Colorectal Dis. 2010 Feb; 12(2): 125-34. [DOI] [PubMed] [Google Scholar]
- 11.Iachino C, Guerrero Y, Sias F, et al. Hemorpex system: a new procedure for the treatment of haemorrhoids. Cir Esp. 2009 Jan; 86(2): 105-9. [DOI] [PubMed] [Google Scholar]
- 12.Pagano C, Vergani C, Invernizzi C, et al. Mucopexy-recto anal lifting: a standardized minimally invasive method of managing symptomatic hemorrhoids, with an innovative suturing technique and the HemorPex SystemⓇ. Minerva Chirurgica. 2018 Oct; 73(5): 469-74. [DOI] [PubMed] [Google Scholar]
- 13.Pagano C, Serfezi C. Mucopexy-recto anal lifting clinical applications handbook digital edition. 2018. [Google Scholar]
- 14.Teksöz S, Aytaç E, Yavuz N, et al. Comparison of a vessel sealing system with a conventional technique in hemorrhoidectoy. Balkan Med J. 2011 Jun; 15(6): 189-92. [Google Scholar]
- 15.Raul K, Seema K, Shilpi B, et al. Comparison of ligasure hemorrhoidectomy with conventional Ferguson's hemorrhoidectomy. Indian J Surg. 2010 Aug; 72(4): 294-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steven B, James T, Angus W, et al. Haemorrhoidal artery ligation versus rubber band ligation for the management of symptomatic second-degree and third-degree haemorrhoids(HuBBLe): a multicenter, open-label, randomized controlled trial. Lancet. 2016 Jul; 388(10042): 356-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andreia A. Rubber band ligation of hemorrhoids: A guide for complications. World J Gastrointest Surg. 2016 Sep; 8(9): 614-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities: A meta-analysis. Dis Colon Rectum. 1995 Jul; 38: 687-94. [DOI] [PubMed] [Google Scholar]
- 19.Sakr MF, Moussa MM. LigaSure hemorrhoidectomy versus stapled Hemorrhoidpexy: a prospective, randomized clinical trial. Dis Colon Rectum. 2010; 53: 1161-7. [DOI] [PubMed] [Google Scholar]
- 20.Khan NF, Shah SSH, Bokhari I. et al. Outcome of stapled hemorrhoidectomy versus Milligan Morgan's closed hemorrhoidectomy. J Coll Physicians Surg Pak. 2009 Sep; 19(9): 561-5. [PubMed] [Google Scholar]



