Abstract
Objectives:
In recent years, CapeOX therapy for patients with colorectal cancer is widely used. We previously reported that a multidisciplinary approach decreases the worsening of adverse events and increases patient satisfaction. In this study, we conducted a multicenter, prospective, observational study to evaluate the incidence of adverse events, health-related quality of life (HRQOL) of the patient, and efficacy of a management (intervention) according to the support system (SMILE study).
Methods:
As the interventional method, the following more than one method was carried out in each institute, 1: support with telephone, 2: dosing instruction by a pharmacist, 3: skin care instruction by a nurse, and 4: patient instruction by a doctor. The primary endpoint was the incidence of hand-foot syndrome (HFS) of more than grade 2. The secondary endpoint was the HRQOL evaluation and efficacy. The questionnaire (HADS) was administered before the start of the chemotherapy and in 1, 2, 4, 5, and 8 courses to evaluate quality of life (QOL).
Results:
From April 2011 to September 2012, 80 patients were enrolled from 14 sites, and all patients were the subjects of analysis. The demographic background was as follows: man/woman: 46/34, age median: 63 (36-75), and management interventional method 1/2/3/4: 36/68/73/78. The overall percentage of HFS that exceeded grade 2 within 6 months was 16.3%. It was 11.1% with the telephone support group and 20.5% without the telephone support group (p = 0.26).
Conclusions:
A multi-professional telephone support may reduce the deterioration of HFS. Further study which includes larger cohort is needed in the future.
Keywords: CapeOX, team management, telephone support, hand foot syndrome, chemotherapy, colorectal cancer
Introduction
Capecitabine plus oxaliplatin (CapeOX) therapy is widely used as treatment for advanced and recurrent colorectal cancer and adjuvant therapy following curative surgery, but its continuity is compromised by hand-foot syndrome (HFS) as an adverse event. We previously reported that HFS exacerbation can be prevented by treatment using a multidisciplinary approach through the formation of a team of a doctor, a pharmacist, and nurses. We also reported that patients are highly satisfied with telephone support from nurses[1]. Patient education by team support was considered useful for proficiency in self-care for the patient's HFS exacerbation. Weekly telephone support by nurses provides home care guidance for adverse toxicity and support to listen to patients' anxiety about the treatment. However, multidisciplinary intensive support for patients cannot be provided at any institution, and the support content varies by institution. Therefore, we conducted a multicenter, prospective, observational study to examine whether the support level at each institution is associated with the incidence of HFS of Blum's classification grade 2 or higher and the mental quality of life (QOL) assessed using the HRQOL questionnaire.
Methods
The present study is a prospective, nonrandomized, multicenter observational study, and it has been approved by the institutional review board of Fujita Health University. The level of support available at participating sites was confirmed and determined for patients with advanced and recurrent colorectal cancer receiving first-line therapy with CapeOX (+bevacizumab [BV]). At least one of the following levels of support was selected at enrolment: (1) telephone intervention during home care; (2) dose confirmation and explanation of supportive drugs by a pharmacist; (3) direct skin care guidance by a nurse; and (4) explanation of adverse events by a physician.
The primary endpoint of this study was HFS of Blum's classification grade 2 or higher, i.e., the frequency of HFS restricting daily living, and the secondary endpoints were the HRQOL score and the relative dose intensity of the drug. QOL was evaluated using the Hospital Anxiety and Depression Scale (HADS) questionnaire of the HRQOL score. HADS is a questionnaire consisting of 14 questions regarding anxiety and depression, with 7 questions regarding depression and 7 questions regarding anxiety, and each question is scored from 0 to 3 points. In general, a score of ≤7 points is considered normal, 8 to 10 points as borderline abnormal, and ≥11 points as abnormal. The questionnaire was administered in cycles 1, 2, 4, 5, and 8 prior to initiating treatment, collected by a nurse or administrative staff before medical examination by a doctor, sealed immediately, and mailed to the study secretariat to avoid disclosing it to the doctor. The relative dose intensity was calculated based on the actual dose administered during the treatment period.
Results
Between April 2011 and September 2012, 80 patients were enrolled from 14 institutions. Patient demographics are presented in Table 1 and the number of patients by support in Table 2. The investigation period was up to eight cycles after initiating treatment. A total of 40 patients completed 8 cycles, and 40 patients discontinued treatment. The reasons for discontinuation were switching to surgical resection in 8 patients, progressive disease in 7 patients, adverse events in 15 patients, and personal reasons in 10 patients. There was no discrepancy between the 25 (15+10) cases and the presence or absence of telephone and team support. The group in which all three professions were involved in management was designated as the team approach group (59/80), and the group receiving telephone support at home was designated as the telephone support group. The incidence rates of HFS of grade 2 or higher, the primary endpoint, were 16.9% in the team approach group and 14.3% in the non-approach group, showing no significant difference (P = 0.44). The percentage was 11.1% for the telephone support group and 20.5% without the telephone support group (p = 0.26) (Table 3). It was lower for the telephone support group, but there was no significant difference. The relative dose intensities in the telephone support and non-telephone support groups were 77.7% and 74.3%, respectively, for oxaliplatin; 80.2% and 75.3%, respectively, for capecitabine; and 78.2% and 73.9%, respectively, for bevacizumab.
Table 1.
Patient Characteristics.
| N = 80 | ||
| Age | Median | 63.5 |
| Range | (36.0-75.0) | |
| Sex | Male | 46 (57.5%) |
| Female | 34 (42.5%) | |
| PS | 0 | 73 (91.3%) |
| 1 | 7 (8.8%) | |
| Primary | Colon | 57 (71.3%) |
| Rectum | 23 (28.8%) | |
| Regimen | XELOX | 33 (41.3%) |
| XELOX+BV | 47 (58.8%) | |
| Pathological findings |
tub1 | 14 |
| tub2 | 51 | |
| others | 15 |
Table 2.
Supportive Intervention.
| Supportive Intervention | Multiple answers |
|---|---|
| A telephone follow-up (TF) | 36 (45%) |
| Instruction on dosage and administration by a pharmacist | 68 (85.0%) |
| Skin care instruction by a nurse | 73 (91.3%) |
| Patients’ education by a doctor | 78 (97.5%) |
| Management by the multidisciplinary team (Ns, doctor, pharmacist) | 59 (73.7%) |
| No team management | 21 (26.2%) |
Table 3.
Incidence of HFS Gr2<.
| All | |
|---|---|
| ≥Grade2 | 16.3% (13/80) |
| A telephone follow-up | 11.1% (4/36) |
| No telephone follow-up | 20.5% (9/44) |
| Team management | 16.9% (10/59) |
| No team management | 14.3% (3/21) |
The HRQOL scores showed no difference in both anxiety factors and depressed mood between the telephone and non-telephone support groups (P = 0.34 and P = 0.94, respectively) (Figure 1). The score of anxiety was a little lower in the telephone support group in all cycles. Although the scores of depression were lower in the telephone support group in the first half of the cycles, they were higher in the telephone support group in the second half.
Figure 1.
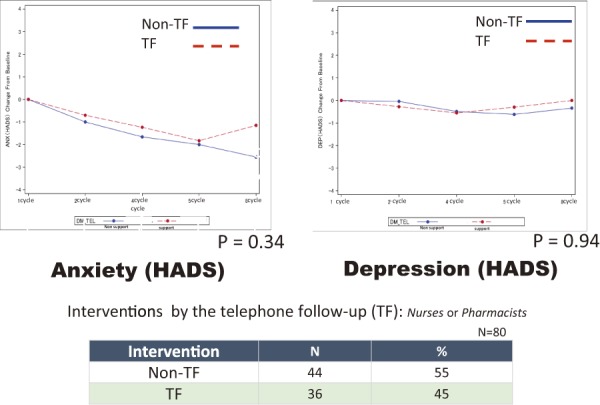
HRQOL score difference of telephone or no telephone follow-up.
As for anxiety, the score decreased with each passing course, but there was no significant difference between telephone support and non-telephone support.
Depression was also unacceptable with telephone support and non-telephone support.
In the examination of the team approach and non-team approach groups, the scores of both anxiety and depression were slightly lower in the team approach group without a significant difference (P = 0.58 and P = 0.92, respectively) (Figure 2).
Figure 2.
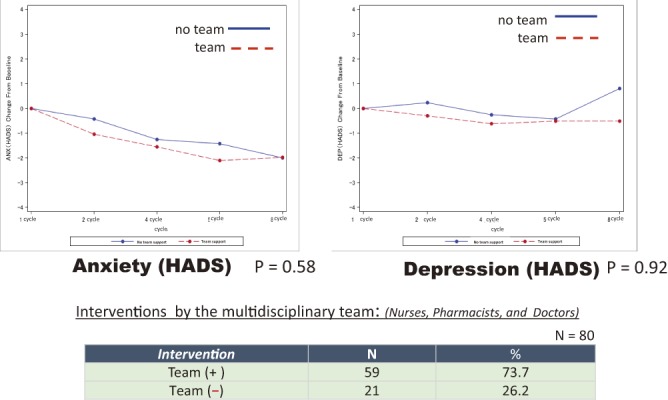
HRQOL score difference of team or no team approach.
The scores of both anxiety and depression were lower in the team approach group without a significant difference.
In changes throughout the eight cycles, the score of anxiety gradually decreased as the cycles progressed, but depression did not improve and exhibited a worsening trend in the second half.
Discussion
The median overall survival of advanced and recurrent colorectal cancer was prolonged along with drug development. On the other hand, since the survival of the patients was prolonged while continuing treatment in a tumor-bearing state, QOL impairment due to adverse toxicity gained more attention than before. We previously reported the results of the prevention of HFS exacerbation by lifestyle guidance and direct guidance by nurses and pharmacists in our hospital[1]. Favorable results of such a multidisciplinary team approach exhibited by the multicenter study are needed for the approval of health insurance coverage under circumstances in which burden on healthcare professionals is increasing. Therefore, we conducted a multicenter, prospective, observational study to examine whether there is a difference in the incidence of HFS grade 2 or higher between institutions using a team approach and those not using a team approach. At the same time, we examined whether treating patients using a multidisciplinary team approach would result in a difference in QOL using HADS.
The incidence of grade 2 or higher HFS in the group receiving telephone support by medical staff was lower than that in the non-telephone support group without a significant difference. The cause was a clinical trial scheduled to accumulate 100 cases, but 80 cases were enrolled, and it was thought that there was a possibility of underpower. Intervention or nonintervention by three professions resulted in no difference in the incidence of grade 2 HFS. Reports of incidence of grade 2 HFS of around 20% is common[2-4], which is consistent with the incidence in the non-telephone support group in this study. Since three professionals, pharmacists, nurses, and doctors, provided telephone support at the institutions, the excellent support that provided by the institutions may have stopped HFS worsening. The relative dose intensity was higher in the telephone support group for both capecitabine and L-OHP, indicating that telephone support did not result in excessively early drug suspension or dose reduction.
The mean scores of both anxiety and depression in the subjects did not achieve 8 points or more in all cycles, suggesting that the mental state was relatively stable during treatment. In addition, the contents of telephone support were examined at the participating sites providing telephone support. Although the professionals making telephone calls varied, such as nurses and pharmacists, the contents were not largely different, and the frequency of telephone calls was unified to once a week.
Sharma et al. reported that preoperative mental stability affects long-term prognosis[5]; other studies revealed that telephone support by nurses improves the anxiety of patients, and interventions by nurses who have undergone communication skills training positively affect patients' stress and stress coping[6-12]. Anxiety of the patients in the telephone support group was stronger than that of patients in the non-telephone support group. Meanwhile, both anxiety and depression exhibited a trend toward improvement in the team approach group in which all three professions provided support intervention, as compared with the non-team approach group. Based on these facts, telephone support itself is not a very effective means for improving anxiety and depression in patients who are originally mentally stable; instead, a direct support by multiple professions is considered effective. Across all eight cycles, anxiety improved as the cycle progressed, suggesting that patients became familiar with their own disease and treatment. Depression of the patients in the telephone support group worsened up to cycle 4 and improved in the telephone support group thereafter. This may suggest that depression worsened as the physical burden worsens in the anterior half of the treatment and that telephone might prevent much further worsening. White et al. reported that telephone intervention did not improve depression but was useful for improving anxiety[13], which is different from our results. In conclusion, we showed that telephone support may reduce HFS frequency; however, it may not substantially reduce psychological burden. However, many patients wished to continue receiving telephone support even after the completion of study intervention, suggesting that telephone support is helpful for the encouragement of patients' heart. In the future, a larger study, which can elucidate how to reduce psychological and physical burden using telephone support, is expected.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
H M, data acquisition and drafting of manuscript, YO, drafting and revision of manuscript, MN, acquisition of data and drafting and revision of manuscript, YS, drafting and revision of manuscript, YM, drafting and revision of manuscript, HB, drafting and revision of manuscript, KN, drafting and revision of manuscript, HO, drafting and revision of manuscript, IT, drafting and revision of manuscript and KM, drafting and revision of manuscript. All authors read and approved the final manuscript.
Approval by Institutional Review Board (IRB)
The study was approved by the Institutional Review Board of Fujita Health University (11-049).
Registration number
UMIN000007185
Acknowledgements
We would like to thank the late Dr. Genichi Nishimura, the principal investigator of this study, for his great contributions to study planning and management.
References
- 1.Matsuoka H, Katagata Y, Ohta H, et al. A multidisciplinary approach to the management of capecitabine-associated hand foot syndrome in cancer patients receiving capecitabine plus oxaliplatin and bevacizumab for advanced colorectal cancer. Fujita Medical Journal. 2017 Feb; 3(1): 1-5. [Google Scholar]
- 2.Rothenberg ML, Cox JV, Butts C, et al. Capecitabine plus oxaliplatin(XELOX) versus 5-fluorouracil/folic acid plus oxaliplatin(FOLFOX4) as second-line therapy in metastatic colorectal camcer: a randomized phase III noninferiority study. Ann Oncol. 2008 Oct; 19(10): 1720-6. [DOI] [PubMed] [Google Scholar]
- 3.Cassidy J, Clarke S, Diaz-Rubio E, et al. Randomized phase III study of capecitabine plus oxaliplatin compared with fluorouracil/folic acid plus oxaliplatin as first-line therapy for metastaic colorectal cancer. J Clin Oncol. 2008 Oct; 26(27): 2006-12. [DOI] [PubMed] [Google Scholar]
- 4.Cassidy J, Clarke S, Diaz-Rubio E, et al. XELOX vs FOLFOX4 as first-line therapy for metastatic colorectal cancer 16966 update results. Br J Cancer. 2011 Jun; 105(1): 58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma A, Walker LG, Monson J. Baseline quality of life factors predict long term survival after elective resection for colorectal cancer. Int J Surg Oncol. 2013 Oct; 2013: 1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Craven O, Hughes CA, Burton A, et al. Is a nurse-led telephone intervention a viable alternative to nurse-led home cae and standard care for patients receiving oral capecitabine? Results from a large prospective audit in patients with colorectal cancer. Eur J Cancer Care. 2013 May; 22(3): 413-9. [DOI] [PubMed] [Google Scholar]
- 7.Kornblith AB, Dowell JM, Herndon JE, et al. Telephone monitoring of distress in patients aged 65 years or older with advanced stage cancer: A cancer and leukemia group B study. Cancer. 2006 Dec; 107(11): 2706-14. [DOI] [PubMed] [Google Scholar]
- 8.MacLeod A, Branch A, Cassidy J, et al. A nurse-/pharmacy-led capecitabine clinic for colorectal cancer: results of prospective audit and retrospective survey of patient experiences. Eur J Oncol Nursing. 2006 Jul; 11(3): 247-54. [DOI] [PubMed] [Google Scholar]
- 9.Livingston PM, Craike MJ, White VM, et al. A nurse-assisted screening and referral program for depression among survivors of colorectal cancer: feasibility study. MJA. 2010 Sep; 193(S5): 83-7. [DOI] [PubMed] [Google Scholar]
- 10.Fukui S, Ogawa K, Otsuka M, et al. A Randomized study assessing the efficacy of communication skill Training on patients' phychologic distress and coping. Cancer. 2008 Sep; 113(6): 1462-70. [DOI] [PubMed] [Google Scholar]
- 11.Murugan K, Ostwal V, Carvalho MD, et al. Self-identification and management of hand-foot syndrome (HFS): effect of a structured teaching program on patients receiving capecitabine-based chemotherapy for colon cancer. Support Care Cancer. 2016 Jun; 24(6): 2575-81. [DOI] [PubMed] [Google Scholar]
- 12.Molassiotis A, Brearley S, Saunders M, et al. Effectiveness of a home care nursing program in the symptom management of patients with colorectal and breast cancer receiving oral chemotherapy: A randomized, controlled trial. J Clin Oncol. 2009 Nov; 27: 6191-8. [DOI] [PubMed] [Google Scholar]
- 13.White VM, Macvean ML, Grogan S, et al. Can tailored telephone intervention delivered by volunteers reduce the supportive care needs, anxiety and depression of people with colorectal cancer? A randomized controlled trial. Psyco-Oncol. 2012 Oct; 21(10): 1053-62. [DOI] [PubMed] [Google Scholar]


