Abstract
Etiology of rhabdomyolysis includes hereditary muscle enzyme deficiencies, trauma, viral infections, excessive exercise, hypothyroidism, and medications such as colchicine, lithium, and statins. Several studies have reported that various antiepileptic drugs may induce rhabdomyolysis. Levetiracetam is one of the antiepileptic drugs implicated in the etiology of rhabdomyolysis. Herein, we present a case of rhabdomyolysis in an adolescent treated with levetiracetam. We wanted to draw attention to the increasing trend of levetiracetam-associated rhabdomyolysis frequency in pediatric patients.
Keywords: adolescent, rhabdomyolysis, levetiracetam
Introduction
Rhabdomyolysis is a syndrome that destroys the integrity of the sarcolemma as a result of musculoskeletal damage due to traumatic or nontraumatic etiologies that include hereditary muscle enzyme deficiencies, trauma, viral infections, excessive exercise, hypothyroidism, and medications such as colchicine, lithium, and statins. 1 2 Rhabdomyolysis has been reported with various antiepileptic drugs. 3 4 Overall, levetiracetam is considered a safe and well-tolerable antiepileptic commonly used for focal and generalized seizures. In recent years, there has been an increase in the reported cases of levetiracetam-associated rhabdomyolysis. 5 6 Herein, we present a case of rhabdomyolysis in an adolescent treated with levetiracetam.
Case Report
A 15-year-old male presented to the pediatric emergency department with weakness and myalgia (especially in lower extremities) for 5 days. He was treated with several antiepileptic medications in past since his diagnosis of epilepsy 10 years ago. He has been on 10 mg/kg/day of levetiracetam for last 1 year; however, the dose was increased to 20 mg/kg/day in view of poor control of seizures. There was no history of trauma, excessive exercise, or infection. The vital signs, physical and neurological examinations were within normal limits. His complete blood count showed mild anemia with hemoglobin of 11 g/dL, slightly decreased platelet count (136.000/µL), and normal white blood cell count (6,600/µL). On chemistry, his serum blood urea nitrogen (BUN) (7.6 mg/dL) and creatinine (0.53 mg/dL) were normal with BUN/creatinine ratio of 14.3. Rest of the laboratory investigations showed uric acid: 3.9 mg/dL, sodium: 140 mmol/L, potassium: 4.2 mmol/L, phosphorus: 4 mg/dL, aspartate aminotransferase: 388 U/L, alanine aminotransferase: 89 U/L, lactic dehydrogenase: 501 U/L, creatine kinase (CK): 14,747 U/L, and blood and urine myoglobin: >3,000. Peripheral blood smear was negative for hemolysis, and platelet count did not show declining trend. History, clinical examination findings of acute onset muscle weakness along with elevated blood CK, and increased blood and urine myoglobin levels were consistent with diagnosis of rhabdomyolysis. Some laboratory tests that were performed to investigate an etiology for rhabdomyolysis were negative. These included thyroid function test and the serologies for Epstein–Barr virus, cytomegalovirus, herpes simplex virus, human immunodeficiency virus, and toxoplasma. Plasma carnitine (42 lmol/L; reference range 19–59 lmol/L) and free carnitine levels (35 lmol/L; reference range 12–46 lmol/L) were normal as acylcarnitine profile. After other causes were excluded, we considered levetiracetam as a causative factor for his rhabdomyolysis and treatment was stopped. Hydration and alkalinization therapies were started. CK continued to rise exponentially with peak of 26,798 U/L at 36th hour after the admission from emergency department. Levetiracetam treatment was stopped at the second day of hospitalization. After stopping levetiracetam, serum CK and myoglobin levels decreased gradually and returned into normal values in 5 days (7th day of admission) ( Fig. 1 ). Muscle biopsy was not performed. This patient did not need renal replacement therapy.
Fig. 1.
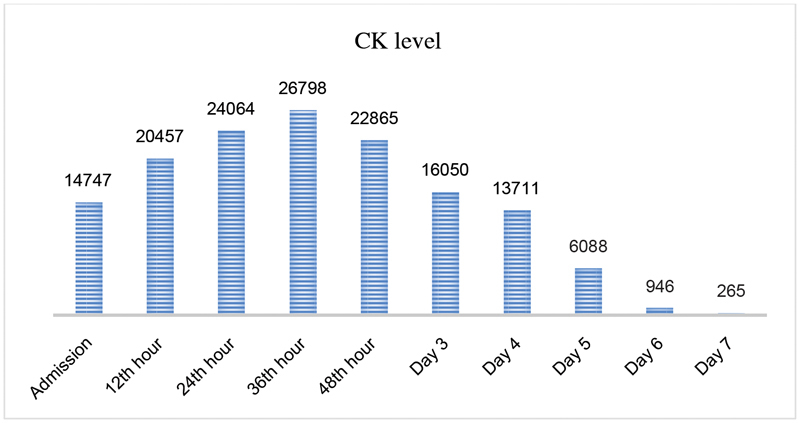
Creatine kinase (CK) levels of patient according to hours.
Discussion
Rhabdomyolysis may occur due to traumatic reasons or due to many different reasons such as alcoholism and medication use (especially statins), excessive physical activity, long-term lack of movement, epileptic seizures, hyperthermia, hypothermia, infections, and electrolyte imbalances (especially hypokalemia and hypophosphatemia). 2 7 Rhabdomyolysis is also seen in many congenital metabolic diseases, glycolytic enzyme deficiency diseases, some diseases with abnormal lipid metabolism, and malignant hyperthermia. 1 Drugs should be considered in differential for the etiology in a case of rhabdomyolysis. In our patient after the excluding other reasons of rhabdomyolysis, we associated the clinical situation of the patient with levetiracetam treatment.
In the literature, adult patients with rhabdomyolysis after levetiracetam treatment have been reported. Akiyama et al 8 reported a 29-year-old woman with epilepsy in whom rhabdomyolysis was induced with levetiracetam. The other case, a 19-year-old man, was reported by Isaacson et al. 9 There have been limited reports of levetiracetam-induced rhabdomyolysis in children. Incecik et al 5 reported a 13-year-old patient and Singh et al 10 reported this clinical situation in a 16-year-old adolescent patient. Carnovale et al 6 analyzed reports from Food and Drug Administration Adverse Event Reporting System database and they detected 48 reports of levetiracetam-induced rhabdomyolysis with an increased trend in reporting in year to year and eight of these reports involved children.
In 5 to 7% of cases that develop acute renal failure, musculoskeletal breakdown is responsible. 1 In our patient, renal functions were normal; patient was responded to the hydration and alkalinization therapy and did not require renal replacement therapy.
In conclusion, levetiracetam-induced rhabdomyolysis is quite rare but is a life-threatening condition. Rhabdomyolysis is a lesser-known adverse event of levetiracetam especially in pediatric age group; however, increased number of cases have revealed levetiracetam as a cause of rhabdomyolysis. In the present case, the most probable cause of the rhabdomyolysis was levetiracetam as symptoms and CK level resolved after stopping therapy. To the best of our knowledge, this is one of the few reports of rhabdomyolysis due to levetiracetam therapy in children. Drugs used in patients with rhabdomyolysis should be questioned and levetiracetam always should be kept in mind for etiology.
Footnotes
Conflict of Interest None declared.
References
- 1.Ward M M. Factors predictive of acute renal failure in rhabdomyolysis. Arch Intern Med. 1988;148(07):1553–1557. [PubMed] [Google Scholar]
- 2.Melli G, Chaudhry V, Cornblath D R. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine (Baltimore) 2005;84(06):377–385. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 3.Gunathilake R, Boyce L E, Knight A T. Pregabalin-associated rhabdomyolysis. Med J Aust. 2013;199(09):624–625. doi: 10.5694/mja13.10769. [DOI] [PubMed] [Google Scholar]
- 4.Santos-Calle F J, Borrás-Blasco J, Navarro-Ruiz A, Plaza Macias I. Unsuspected rhabdomyolysis associated with phenytoin. Int J Clin Pharmacol Ther. 2005;43(09):436–440. [PubMed] [Google Scholar]
- 5.Incecik F, Herguner O M, Besen S, Altunbasak S. Acute rhabdomyolysis associated with levetiracetam therapy in a child. Acta Neurol Belg. 2016;116(03):369–370. doi: 10.1007/s13760-015-0542-9. [DOI] [PubMed] [Google Scholar]
- 6.Carnovale C, Gentili M, Antoniazzi S, Clementi E, Radice S. Levetiracetam-induced rhabdomyolysis: analysis of reports from the Food and Drug Administration's Adverse Event Reporting System database. Muscle Nerve. 2017;56(06):E176–E178. doi: 10.1002/mus.25972. [DOI] [PubMed] [Google Scholar]
- 7.Grifoni E, Fabbri A, Ciuti G, Matucci Cerinic M, Moggi Pignone A. Hypokalemia-induced rhabdomyolysis. Intern Emerg Med. 2014;9(04):487–488. doi: 10.1007/s11739-013-1033-8. [DOI] [PubMed] [Google Scholar]
- 8.Akiyama H, Haga Y, Sasaki N, Yanagisawa T, Hasegawa Y. A case of rhabdomyolysis in which levetiracetam was suspected as the cause. Epilepsy Behav Case Rep. 2014;2:152–155. doi: 10.1016/j.ebcr.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Isaacson J E, Choe D J, Doherty M J. Creatine phosphokinase elevation exacerbated by levetiracetam therapy. Epilepsy Behav Case Rep. 2014;2:189–191. doi: 10.1016/j.ebcr.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh R, Patel D R, Pejka S. Rhabdomyolysis in a hospitalized 16-year-old boy: a rarely reported underlying cause. Case Rep Pediatr. 2016;2016:7.873813E6. doi: 10.1155/2016/7873813. [DOI] [PMC free article] [PubMed] [Google Scholar]


