Abstract
Obstetric palsy is classically defined as the brachial plexus injury due to shoulder dystocia or to maneuvers performed on difficult childbirths. In the last 2 decades, several studies have shown that half of the cases of Obstetric palsy are not associated with shoulder dystocia and have raised other possible etiologies for Obstetric palsy. The purpose of the present study is to collect data from literature reviews, classic articles, sentries, and evidence-based medicine to better understand the events involved in the occurrence of Obstetric palsy. A literature review was conducted in the search engine PubMed (MeSH - Medical Subject Headings) with the following keywords: shoulder dystocia and obstetric palsy , completely open, boundless regarding language or date. Later, the inclusion criterion was defined as revisions. A total of 21 review articles associated with the themes described were found until March 8, 2018. Faced with the best available evidence to date, it is well-demonstrated that Obstetric palsy occurs in uncomplicated deliveries and in cesarean deliveries, and there are multiple factors that can cause it, relativizing the responsibility of obstetricians, nurses, and midwives. The present study aims to break the paradigms that associate Obstetric palsy compulsorily with shoulder dystocia, and that its occurrence necessarily implies negligence, malpractice or recklessness of the team involved.
Keywords: paralysis, obstetric; shoulder; dystocia; birth injuries
Introduction
Obstetric palsy (OP) is defined as a partial or total flaccid paralysis that affects the upper limb of the newborn due to brachial plexus injury occurring in normal delivery, and, more rarely, in cesarean section, often associated with shoulder dystocia (SD). It is also defined as palsy due to injury received at birth, according to the Health Sciences Descriptors (DeCS, in the Portuguese acronym). 1
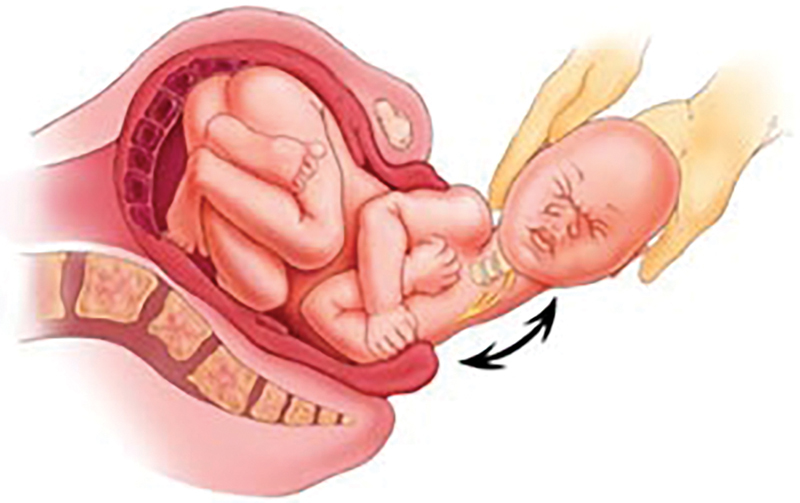
Shoulder dystocia (SD) or bisacromial dystocia occurs when the presentation is cephalic and the cephalic pole is already detached, but the shoulders do not come loose, and no other difficulties are observed 2 ( Figure 1 ).
Fig. 1.
Shoulder dystocia.
Although rare, with an incidence in < 1% of births, it is a serious complication, whose occurrence increases considerably to ∼ 6% in cases of fetuses weighing > 4,000 g. 3 4 Factors associated with this complication are maternal obesity, postdatism and gestational diabetes. 3 4 5 Importantly, even in fetuses weighing < 4,000 g, SD may occur, especially when there is some degree of disproportion between the fetus and the maternal pelvis. 2
Shoulder dystocia is associated with maternal complications, the most commonly described being birth canal lacerations, uterine atony with hemorrhage, pubic symphysis disjunction, and, occasionally, uterine rupture. 2
Fetal complications are brachial plexus injuries and clavicle and humerus fractures, which may progress to intrapartum or neonatal death. The brachial plexus is formed by joining the anterior branches of the roots of C5, C6, C7, C8 and T1, emerging between the anterior and middle scalene muscles. In many cases, it receives a contribution from C4, when it is called prefixed. The situation in which this contribution is from T2 is called postfixed. 6 The brachial plexus is usually injured by excessive traction during labor, which can occur in up to 15% of newborns with bisacromial dystocia. 7 In most cases, the lesion resolves within 6 to 12 months, but severe cases may require surgery, with risk of permanent damage in up to 10% of occurrences. 8
Galbiatti, 9 Galbiatti et al 6 and Albertoni et al, 10 in studies about OP, comment on anatomical bases and make a brief history of this lesion. The authors point out that this has been recognized since ancient times in the medical literature. It was briefly cited by Smellie in 1764. In 1872, Duchenne de Boulogne, in his “Traité de l'Électrisation Localisée”, used the term obstetric palsy and described upper root paralysis. Erb, in 1874, detailed the clinical picture of upper trunk OP (C5 and C6). In 1885, Klumpke described the rarer plasy of the lower roots (C8 and T1), which may be associated with the Claude Bernard-Horner syndrome.
The incidence of OP ranges from 0.1% to 0.4% of all live births. Despite advances in obstetric care, the incidence of OP may be increasing due to the larger number of newborns with high weight. Several risk factors were identified, including prolonged labor, high-weight newborns, difficult birth, forceps use, and previous deliveries concurrent with OP. Shoulder dystocia is the mechanical factor that results in upper trunk injury. 11 Significant risk factors are: child weight > 4,000 g, SD, and breech deliveries. 12
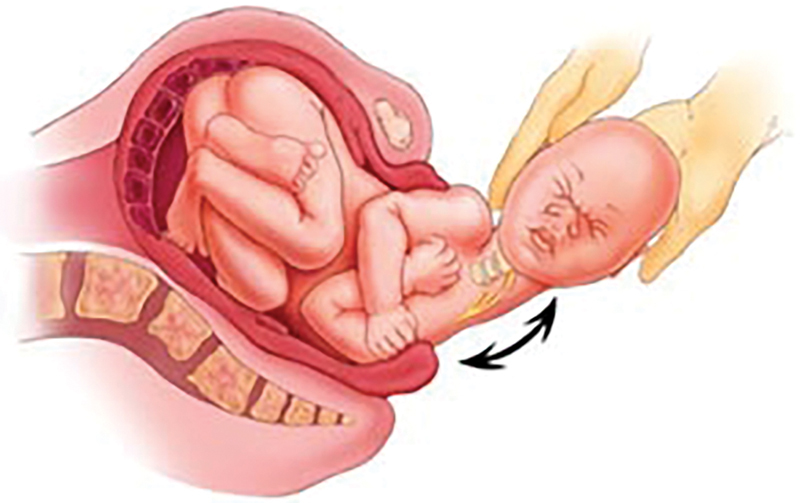
The most common type of OP and which has a better prognosis is the plasy called high, or Erb-Duchenne (90% of cases), in which the roots of C5-C6 are affected and the most frequently involved muscles are the supraspinatus and the infraspinatus ( Figure 2 ). There is also total (mixed) palsy, which presents both motor and sensory palsy of the entire extremity of the affected limb due to injury to all plexus roots; and low plasy, or Klumpke (C8-T1), in which the forearm and hand muscles are the most affected. The severity of the injury depends on the affected roots and its extent.
Fig. 2.

Erb's obstetric paralysis.
Galbiatti et al 6 present the classic brachial plexus anatomy and explain that neural lesions can be classified into three functional categories, according to Seddon 13 :
Neuropraxia: without neural morphological alteration, defined as localized conduction block due to metabolic alteration and clinically represented by motor palsy, mild sensory and sympathetic alteration, showing total recovery over a few weeks.
Axonotmesis: axonal interruption without endoneurial injury, leading to Wallerian degeneration distal to the lesion. Variable axonal regeneration occurs oriented by endoneurium preservation; the recovery time depends above all on the distance from the injury to the effectors (basically to the muscular motor plate).
Neurotmesis: determines a total nerve damage with destruction of internal and external structures. There is no spontaneous regeneration, requiring surgical treatment.
In the clinical practice, it is often difficult to classify lesions, especially axonotmesis. It must be considered also in relation to the brachial plexus injury, avulsions at the spinal cord level, also called preganglionic lesions, because they are proximal to the ganglions of motor neurons, which do not allow repair. In this situation, there is also injury to the posterior branch of the nerve root and it leads to the denervation of the paravertebral musculature of the cervical region.
The authors stress the importance of the most frequent differential diagnoses, which are cerebral palsy, clavicle and humeral shaft fractures, present in 10 to 15% of the cases with cephalic presentation. 6 Proximal humeral epiphyseal detachment, neonatal osteomyelitis, pyogenic shoulder arthritis, and congenital syphilis are also differential diagnoses.
Obstetric palsy is one of the complications associated with childbirth that needs to be better studied and understood, as it maintains its international incidence to the present day, 14 taking place all over the world, not distinguishing rich or poor countries, young obstetrician surgeons or surgeons with extensive experience, obstetric nurses or midwives.
Against this background, the medicolegal demands related to unfavorable events related to childbirth, including OP, have been increasing. In this scope, particularly obstetricians are held responsible or blamed for these events that occur during their professional activity. It is set in a classic paradigm that, in the last decade, with the evolution of evidence-based medicine (EBM), is being broken. There are currently new studies proving new etiologies as having congenital or intrauterine origins, and caused by endogenous forces of childbirth, among others. In 1997, Paradiso et al 15 had already published an important article dealing with electroneuromyography (ENMG) examination at birth, demonstrating that brachial plexus injury could have occurred inside the uterus. The authors report on an 18-day-old child with a C5-C6 lesion whose ENMG examination was compatible with an old lesion dated before birth. There are cases in which certain children are born with palsy without labor abnormality, without dystocia and without any particular maneuver.
The classic definition bears signs that the cause would be dystocic deliveries or delivery maneuvers performed by the attending physician. This paper aims to gather data from the review literature, classic articles, sentinel data and evidence-based medicine for the professionals involved in these procedures, among them the medical expert, to have sufficient scientific support to better understand the events that occur during childbirth and to identify whose responsibility the OP really is.
With this review, we will, in the light of the latest studies, change the direction, at least partially, of the causes of OP.
Methods
A literature search was performed on the PubMed search engine (Medical Subject Headings [MeSH]) with the following keywords: shoulder dystocia and obstetric palsy , completely open, with no language or date limits. We found 87 articles. Subsequently, we defined as the inclusion criterion review articles, of which 22 review articles remained associated with the themes described until March 8, 2018. We excluded 1 article because it was the same study published in a different journal in the form of a compact version, remaining, therefore, 21 articles.
These 21 articles were given order numbers according to the growing chronology of the publication. These articles were characterized according to the main relevant points, with the following descriptors: shoulder dystocia , cesarean section , prevention , history , etiopathogenesis and medicolegal . When we included in the search engine descriptors specifically related to medical expertise, such as the descriptors expert or expert testimony , in addition to a limited number of articles, they fell into themes not included in our scientific proposal.
We performed a manual review of the 21 articles that originated our review and added to our bibliography articles that were cited in most publications and the articles considered classic or sentinel data (for these, the year of publication and language were not considered). With this concept, articles with a medicolegal nature were valued.
Results
A total of 87 articles were included based on the inclusion criteria mentioned above, excluding 66 that did not have review characteristics or were repeated compact-version publications by the same authors published in another journal. Effectively, 21 articles were used, 17 in the English language, 2 in the French language, and 2 in the German language.
The results show that there are no articles with adequate levels of evidence, being mostly literature reviews.
Regarding the year of publication, there was a variable distribution from 2000 to 2016 ( Table 1 ). 14 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34
Table 1. Selected Articles.
| Order | Authorship | Journal | Year | Country | Language |
|---|---|---|---|---|---|
| 1 | Beller 14 | Z Geburtshilfe Neonatol | 2000 | Germany | German |
| 2 | Sandmire et al 35 | Birth | 2002 | USA | English |
| 3 | Sandmire et al 16 | Int J Gynaecol Obstet | 2002 | USA | English |
| 4 | Krause et al 17 | Z Geburtshilfe Neonatol | 2005 | Germany | German |
| 5 | Gherman et al 18 | Am J Obstet Gynecol | 2006 | USA | English |
| 6 | Hankins et al 19 | Semin Perinatol | 2006 | USA | English |
| 7 | Gurewitsch 20 | Clin Obstet Gynecol | 2007 | USA | English |
| 8 | Allen 21 | Clin Obstet Gynecol | 2007 | USA | English |
| 9 | Jevitt et al 22 | J Perinat Neonatal Nurs | 2008 | USA | English |
| 10 | Doumouchtsis et al 23 | Obstet Gynecol Surv | 2009 | England | English |
| 11 | O'Shea et al 24 | Semin Perinatol | 2010 | USA | English |
| 12 | Doumouchtsis et al 25 | Ann N Y Acad Sci. | 2010 | England | English |
| 13 | Anderson 26 | Prim Care Clin Office Pract | 2012 | USA | English |
| 14 | Abzug et al 27 | Orthop Clin North Am | 2014 | USA | English |
| 15 | Stitely et al 28 | Seminars in Perinatology | 2014 | New Zealand/USA | English |
| 16 | Chauhan et al 29 | Seminars in Perinatology | 2014 | USA | English |
| 17 | Ouzounian 30 | Seminars in Perinatology | 2014 | USA | English |
| 18 | Legendre et al 31 | J Gynecol Obstet Biol Reprod | 2015 | France | French |
| 19 | Schmitz 32 | J Gynecol Obstet Biol Reprod | 2015 | France | French |
| 20 | Hill et al 33 | Womens Health | 2016 | USA | English |
| 21 | Sentilhes et al 34 | Eur J Obstet Gynecol Reprod Biol | 2016 | France | English |
Data referring to the 21 review articles are described in ascending chronological order, with authorship, name of the journal, year of publication, country of origin of the authors and language of publication.
All of the major studies were literature reviews, as this is one of the premises of the method, and the number of articles in their bibliography ranged from 11 to 121 articles reviewed.
The data regarding the number order, type of study, number of bibliographies used for each article, the most important points and conclusions of the study are shown in Table 2 .
Table 2. Detailed data of the articles.
| Order | Study Type | N° of Bibliographies | Relevant points | Conclusions |
|---|---|---|---|---|
| 1 | Revision | 86 | Medicolegal | The large number of OP without dystocia does not allow us to state that OP is caused by the obstetrician. |
| 2 | Revision | 22 | Historic | OP occurs in deliveries without dystocia 36 ; the experience of the surgeon is indifferent to the incidence of OP 37 ; indirect evidence establishes that maternal driving forces are the most likely cause of Erb's palsy. |
| 3 | Revision | 17 | Shoulder Dystocia | The most likely cause of paralysis with and without SD is maternal exertion due to expulsive forces at birth. |
| 4 | Revision | 86 | Medicolegal | A clear cause-effect relationship between SD and brachial plexus injuries does not exist in all cases, although SD is usually associated with obstetric medicolegal opinions. |
| 5 | Revision | 121 | Shoulder Dystocia | There is a significantly increased risk of SD during birth related to weight, and this increases linearly; prenatal and prelabor care have no statistically significant risk factors for predicting shoulder dystocia; prophylactic cesarean delivery or drug induction of labor in nondiabetic patients due to suspected fetal macrosomia has not been shown to alter the incidence of SD. |
| 6 | Revision | 43 | Cesarean Section | Cesarean section performed in all women at 39 weeks of gestation would substantially reduce both transient and permanent brachial plexus injury, neonatal encephalopathy, intrapartum and intrauterine death. |
| 7 | Revision | 74 | Prevention | Fetal manipulation seems to be the best method for atraumatic resolution of complicated vaginal delivery, because it requires less traction to complete it. |
| 8 | Revision | 69 | Etiopathogenesis | Doctors need to be trained to slow and calibrate traction, because the natural tendency is to increase it when faced with a difficult delivery. Axial traction should be used, but lateral head flexion should be limited. |
| 9 | Revision | 27 | Prevention | SD is not predictable; perinatal nurses are useful in the prenatal period to avoid excessive weight gain and assist in glycemic control and during childbirth as a timekeeper once SD is diagnosed. |
| 10 | Revision | 99 | Etiopathogenesis | Most children with brachial plexus injuries do not have known risk factors; endogenous forces are 4- to 9-fold greater than those applied by the obstetrician during SD, according to mathematical models. |
| 11 | Revision | 95 | Shoulder Dystocia | Pregnant women with previous cesarean section, what is the best delivery option? There are no randomized studies available that directly relate to the choice of delivery method. |
| 12 | Revision | 51 | Prevention | SD is a risk factor for brachial plexus injury (increases by 100x the risk of OP) but is unpredictable; a significant proportion of plexus injury is secondary to injuries in the uterus. |
| 13 | Revision | 44 | Shoulder Dystocia | Maternal, fetal and childbirth RFs have low predictive value; SD most commonly occurs in patients without identified RFs. |
| 14 | Revision | 46 | Shoulder Dystocia | Neonatal brachial plexus paralysis can result in lifelong permanent deficits and remains common despite advances in obstetric care. The long-term results of current treatment recommendations remain unknown. |
| 15 | Revision | 28 | Shoulder Dystocia | Some maneuvers and algorithms can be used to manage shoulder dystocia. From studies among women whose delivery is complicated by SD, there is considerable scientific evidence that the all-fours maneuver is effective for releasing the fetal shoulders. |
| 16 | Revision | 80 | Shoulder Dystocia | Epidemiological knowledge of the incidence, prevalence and temporal changes of NBPP should assist the clinician, avoid unnecessary interventions, and help formulate evidence-based health policies. The extremely infrequent nature of permanent NBPP requires a multicenter study to improve our understanding of antecedent factors and reduce long-term sequelae. |
| 17 | Revision | 26 | Shoulder Dystocia | Historical risk factors for neonatal brachial plexus paralysis (NBPP), whether studied alone or in combination, have not been shown as reliable predictors. Most NBPP cases occur in women with children < 4,500g who are not diabetic and have no other identifiable RFs. In addition, caesarean section reduces but does not eliminate the risk of NBPP. |
| 18 | Revision | 23 | Shoulder Dystocia | Regarding the prevention of shoulder dystocia complications, hands-on training using dummies is associated with more improvements in SD administration than training using the video tutorial. Simulation teaching for the treatment of shoulder dystocia is encouraged for the initial and ongoing training of the various actors in the birth room (professional arrangement). |
| 19 | Revision | 55 | Prevention | To avoid SD and its complications, two measures are proposed. Induction of labor is recommended in case of imminent macrosomia, if the cervix is favorable and gestational age > 39 weeks (professional consensus). Cesarean section administration is recommended before labor in case of (I) fetus > 4,500 g if associated with maternal diabetes, (II) fetus > 5,000 g in the absence of maternal diabetes and, (III) during labor in case of fetal macrosomia and failure to progress in the second stage, when the fetal head is above a +2 position. Caesarean section should be discussed when history of shoulder dystocia has been associated with severe neonatal or maternal complications (professional consensus). |
| 20 | Revision | 94 | Shoulder Dystocia | SD can be prevented by performing preventive caesarean section in high-risk cases, but our ability to identify such cases is still limited. Rapid diagnosis and management of SD when it occurs is key to preventing permanent neurological sequelae. Management requires the coordinated efforts of a team with the necessary skills. The team leader must direct management and institute a series of maneuvers to release the fetus with minimal risk to him and the mother. A complete understanding of the relevant pelvic and fetal anatomy is needed, as well as the mechanisms by which dystocia can be resolved. |
| 21 | Revision | 11 | Shoulder Dystocia | No study has proven that correcting risk factors (except gestational diabetes) would reduce the risk of SD. Physical activity is recommended before and during pregnancy to reduce some RFs. The implementation of practical training simulation for all care providers in the delivery room is associated with a significant reduction in neonatal injury, but not in the maternal. SD remains an unpredictable obstetric emergency. All doctors and midwives should know and perform obstetric maneuvers, if necessary, quickly but calmly. |
Abbreviations: SD, shoulder dystocia; NBPP, neonatal brachial plexus paralysis; OP, obstetric paralysis; RF, risk ractor.
Data regarding order number, type of study, number of bibliographies consulted in the article, most relevant points and conclusion(s) of the study.
Discussion
Obstetric palsy is classically defined as partial or total flaccid palsy that affects the upper limb due to brachial plexus injury in childbirth. This concept is present in both orthopedic and obstetric textbooks 2 6 ; however, the literature of the last 2 decades has shown that more than half of the cases are not associated with shoulder dystocia. 14 23 35 Other etiologies have been considered, such as congenital and intrauterine origin, and those caused by endogenous forces of childbirth, among others.
We currently have ample evidence that many other factors may be involved in the cause of OP, unrelated to the delivery maneuvers performed by obstetricians.
Zaki et al, 36 in a study on congenital familial injury of brachial plexus palsy present a two-level report on Egyptian families affected at birth, characterized it as relatively uncommon and almost a sporadic disorder. Mollica et al 37 describe a Sicilian family with congenital severe brachial plexus injury and suggest that the gene has autosomal dominant inheritance with reduced penetrance. The authors report that X-linked inheritance with expression in heterozygous women cannot be ruled out.
Uterine malformations and propulsive forces in the second phase of childbirth are the main etiological factors for plexus injuries, 16 18 25 35 38 39 especially in cases without shoulder dystocia.
Among the uterine causes, we can highlight uterine malformations such as fibroids, intrauterine septum or bicornuate uterus. 25 Intrauterine maladaptation (e.g. oligohydramnios) may be related to decreased resistance of brachial plexus nerve bundles or scapular girdle structures, leading to plexus injury. 40
Regarding vaginal delivery, we can divide it didactically into three phases: the first is dilation and corresponds to the lowering of the fetus to the fitting axis of the bone pelvis. The second phase is expulsion, which lasts between 30 minutes and 2 hours.
The second phase is subdivided into two stages: the first is the completion of the descent and rotation of the presentation, and the second is the actual descent, in which the abdominal pressure must be controlled and directed with the uterine contractions to expel the fetus. 2 In the second stage, shoulder dystocia and plexus injuries may occur due to compression of the posterior shoulder against the sacral promontory during uterine contractions. According to mathematical models, the expulsive forces are four to nine times greater than the traction exerted by the obstetrician. 25 35
The third and last phase of labor begins at birth and ends when the placenta is delivered.
Due to this new knowledge, Gherman et al 39 as early as 1998, in their review, stated that indirect evidence established maternal driving forces as the most likely cause of Erb palsy, both in cases with associated SD and in cases without it, since direct fetal manipulation techniques for SD resolution were not associated with higher rates of plexus injury, humerus or clavicle fractures. Sandmire et al 16 in 2002, Gherman et al 18 in 2006, Doumouchtsis et al 25 in 2010 and Abzug et al 27 in 2014, respectively, evidenced this knowledge in their reviews, giving enough information to conclude that the recent emphasis on EBM undermined many of the myths and misconceptions surrounding shoulder dystocia. Therefore, the influence attributed to the attending physician during delivery, in relation to brachial plexus injury, needs to be revised.
The main risk factors for brachial plexus injury are: fetal macrosomia (fetal weight > 4,000 g), pelvic presentation and shoulder dystocia. 2 6 11 12 19 21 26 35 Maternal obesity, maternal or gestational diabetes, excessive weight gain during pregnancy, male fetus, prematurity, previous history of fetal macrosomia, anterior dystocic deliveries, multiparity, forceps instrumentation, advanced maternal age and post-term birth are considered secondary risk factors. 18 21 39 40 Ouzounian 30 argues that caesarean section reduces but does not completely eliminate the risk of brachial plexus injury.
Despite multiple risk factor analyses in the literature, shoulder dystocia cannot be predicted or avoided, because the precise methods to identify which fetuses will experience this complication do not exist. Prenatal and prelabor data have low predictive value. 18 22 24 26 Ultrasound examination performed late in pregnancy also has low sensitivity, with poor accuracy in estimating birthweight – there is a general tendency to overrate it. It should also be noted that SD most commonly occurs in patients without risk factors. 26
As the risk of shoulder dystocia is directly proportional to the increased fetal weight, 39 prophylactic cesarean section has been proposed in selected cases. 32 33 According to the American College of Obstetricians and Gynecologists (ACOG) and Schmitz, 32 we must consider it in fetuses of diabetic mothers with estimated weight > 4,500 g or in fetuses with > 5,000g of mothers with no risk factors. Other authors, like Hankins et al, 19 recommend it for fetuses of diabetic mothers with weight estimates between 4,000 to 4,250 g or > 4,000g in pregnancies of nondiabetic women.
A better understanding of the causes of OP is necessary, since the medicolegal demands have increased worldwide, and, in most cases where there is permanent loss of upper limb function, the attending physician is required to indemnify the family of the child for malpractice. According to the Health Insurance Association of America, from January 1985 to December 2001, the average amount paid for indemnities related to brachial plexus injury was US$301,000.00 (∼ 4x more than the average amount paid due to malpractice for other causes in the same period), in a total value of US$54 million. The indemnity values were higher for medical assistants of educational institutions. 38
To avoid these contentious situations, Noble 41 advises to make accurate and detailed records for a successful defense. However, the fundamental thing remains the doctor-patient relationship. Hickson et al 42 demonstrated in their study that 70% of the mothers who sued obstetricians for perinatal injuries in their newborns complained that these professionals did not adequately inform them about possible permanent injuries in the neuropsychomotor development of their children. Informing the risks inherent in childbirth, such as the fact that brachial plexus injuries are not necessarily due to birth trauma, and trying to understand the fears and anxieties of the patient, is essential to minimize medicolegal issues. 36
The training of the surgical team and the full understanding of the pelvic and fetal anatomy, as well as mechanisms, algorithms and maneuvers by which dystocia can be resolved, epidemiological knowledge of the incidence, prevalence and temporal changes of neonatal brachial plexus paralysis, are of fundamental importance for the proper management of an obstetric center. 19 29 32 33 34 Legendre et al, 31 advocate in their study the initial and ongoing practical training of the various actors in the birth room using mannequins, that according to the authors is associated with more improvements in shoulder dystocia management than training using a video tutorial.
Final considerations
We believe that, with this literature review, we can undoubtedly help to break the paradigm established since ancient times that this injury would be caused solely and exclusively by medical malpractice. The literature is changing its direction, demonstrating that there are other multiple causes or co-causes for the occurrence of obstetric paralysis, some of them without any involvement of the medical team.
Therefore, on the question of who is responsible for OP, there is currently indirect evidence that establishes that maternal (endogenous) driving forces may be the most likely cause of brachial plexus paralysis at birth, births without SD and children weighing < 4,000 g. Obstetric palsy may have intrauterine, genetic or postural origin, and it is important for medicolegal protection not only the fulfillment of medical records, as well as electroneuromyography examination up to 21 days after birth to determine if it occurred inside the uterus or at birth. There is still a need for new well-based and prospective publications with EBM to better define which is (or are) the real responsible for the occurrence of OP.
Conflitos de interesses Os autores declaram não haver conflitos de interesses.
Trabalho desenvolvido na Faculdade de Medicina de Marília, Marília, SP, Brasil.
Study developed at the Faculdade de Medicina de Marília, Marília, SP, Brazil.
Referências
- 1.Descritores em Ciências da Saúde (DeCS) [Internet]. ed. 2017São Paulo (SP): BIREME / OPAS / OMS. 2017 [acesso em 2017 dez 04]. Disponível em:http://decs.bvsalud.org
- 2.Francisco R P, Fonseca E S, Sapienza D S. Barueri: Manole; 2008. Parto e puerpério; pp. 307–529. [Google Scholar]
- 3.Srofenyoh E K, Seffah J D. Prenatal, labor and delivery characteristics of mothers with macrosomic babies. Int J Gynaecol Obstet. 2006;93(01):49–50. doi: 10.1016/j.ijgo.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Piasek G, Starzewski J, Chil Aet al. [Analysis of labour and perinatal complications in case of foetus weight over 4000 g] Wiad Lek 200659(5-6):326–331. [PubMed] [Google Scholar]
- 5.Seeho S K, Smith C, Mcelduff A, Morris J M. Diabetes Res Clin Pract. 2007;77(02):263–268. doi: 10.1016/j.diabres.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Galbiatti J A, Falloppa F. Porto Alegre: Artmed; 2003. Paralisia obstétrica; pp. 830–838. [Google Scholar]
- 7.Baxley E G, Gobbo R W. Shoulder dystocia. Am Fam Physician. 2004;69(07):1707–1714. [PubMed] [Google Scholar]
- 8.Athukorala C, Middleton P, Crowther C A. Intrapartum interventions for preventing shoulder dystocia. Cochrane Database Syst Rev. 2006;(04):CD005543. doi: 10.1002/14651858.CD005543.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galbiatti J A. São Paulo: Manole; 2008. Paralisia obstétrica; pp. 273–284. [Google Scholar]
- 10.Albertoni W M, Galbiatti J A, Canedo A C, Merlotti M. Estudo anatômico do plexo braquial na criança até os seis meses de idade. Rev Bras Ortop. 1994;29(03):162–169. [Google Scholar]
- 11.Sawyer J R. Philadelphia: Elsevier; 2013. Brachial plexus palsy; pp. 1323–1330. [Google Scholar]
- 12.Slooff A C.Obstetric brachial plexus lesions and their neurosurgical treatment Clin Neurol Neurosurg 199395(Suppl):S73–S77. [DOI] [PubMed] [Google Scholar]
- 13.Seddon H J. Three types of nerve injury. Brain Oxford. 1943;(66):37. [Google Scholar]
- 14.Beller F K. [Incidence and etiology of brachial plexus upper arm paralysis in newborn infants. A review and basic principles for legal assessment] Z Geburtshilfe Neonatol. 2000;204(05):163–169. doi: 10.1055/s-2000-10215. [DOI] [PubMed] [Google Scholar]
- 15.Paradiso G, Grañana N, Maza E. Prenatal brachial plexus paralysis. Neurology. 1997;49(01):261–262. doi: 10.1212/wnl.49.1.261. [DOI] [PubMed] [Google Scholar]
- 16.Sandmire H F, DeMott R K. Erb's palsy without shoulder dystocia. Int J Gynaecol Obstet. 2002;78(03):253–256. doi: 10.1016/s0020-7292(02)00131-5. [DOI] [PubMed] [Google Scholar]
- 17.Krause M, Feige A. [Shoulder dystocia from a legal standpoint] Z Geburtshilfe Neonatol. 2005;209(06):201–209. doi: 10.1055/s-2005-916243. [DOI] [PubMed] [Google Scholar]
- 18.Gherman R B, Chauhan S, Ouzounian J G, Lerner H, Gonik B, Goodwin T M. Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol. 2006;195(03):657–672. doi: 10.1016/j.ajog.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Hankins G D, Clark S M, Munn M B. Cesarean section on request at 39 weeks: impact on shoulder dystocia, fetal trauma, neonatal encephalopathy, and intrauterine fetal demise. Semin Perinatol. 2006;30(05):276–287. doi: 10.1053/j.semperi.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Gurewitsch E D. Optimizing shoulder dystocia management to prevent birth injury. Clin Obstet Gynecol. 2007;50(03):592–606. doi: 10.1097/GRF.0b013e31811eaba2. [DOI] [PubMed] [Google Scholar]
- 21.Allen R H. On the mechanical aspects of shoulder dystocia and birth injury. Clin Obstet Gynecol. 2007;50(03):607–623. doi: 10.1097/GRF.0b013e31811eb8e2. [DOI] [PubMed] [Google Scholar]
- 22.Jevitt C M, Morse S, O'Donnell Y S. Shoulder dystocia: nursing prevention and posttrauma care. J Perinat Neonatal Nurs. 2008;22(01):14–20. doi: 10.1097/01.JPN.0000311870.07958.81. [DOI] [PubMed] [Google Scholar]
- 23.Doumouchtsis S K, Arulkumaran S. Are all brachial plexus injuries caused by shoulder dystocia? Obstet Gynecol Surv. 2009;64(09):615–623. doi: 10.1097/OGX.0b013e3181b27a3a. [DOI] [PubMed] [Google Scholar]
- 24.O'Shea T M, Klebanoff M A, Signore C. Delivery after previous cesarean: long-term outcomes in the child. Semin Perinatol. 2010;34(04):281–292. doi: 10.1053/j.semperi.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Doumouchtsis S K, Arulkumaran S. Is it possible to reduce obstetrical brachial plexus palsy by optimal management of shoulder dystocia? Ann N Y Acad Sci. 2010;1205:135–143. doi: 10.1111/j.1749-6632.2010.05655.x. [DOI] [PubMed] [Google Scholar]
- 26.Anderson J E. Complications of labor and delivery: shoulder dystocia. Prim Care. 2012;39(01):135–144. doi: 10.1016/j.pop.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Abzug J M, Kozin S H. Evaluation and management of brachial plexus birth palsy. Orthop Clin North Am. 2014;45(02):225–232. doi: 10.1016/j.ocl.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Stitely M L, Gherman R B. Shoulder dystocia: management and documentation. Semin Perinatol. 2014;38(04):194–200. doi: 10.1053/j.semperi.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Chauhan S P, Blackwell S B, Ananth C V. Neonatal brachial plexus palsy: incidence, prevalence, and temporal trends. Semin Perinatol. 2014;38(04):210–218. doi: 10.1053/j.semperi.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 30.Ouzounian J G. Risk factors for neonatal brachial plexus palsy. Semin Perinatol. 2014;38(04):219–221. doi: 10.1053/j.semperi.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Legendre G, Bouet P E, Sentilhes L. Place de la simulation pour réduire la morbidité néonatale et maternelle secondaire à une dystocie des épaules. J Gynecol Obstet Biol Reprod (Paris) 2015;44(10):1285–1293. doi: 10.1016/j.jgyn.2015.09.047. [DOI] [PubMed] [Google Scholar]
- 32.Schmitz T. Modalités de l'accouchement dans la prévention de la dystocie des épaules en cas de facteurs de risque identifiés. J Gynecol Obstet Biol Reprod (Paris) 2015;44(10):1261–1271. doi: 10.1016/j.jgyn.2015.09.051. [DOI] [PubMed] [Google Scholar]
- 33.Hill M G, Cohen W R. Shoulder dystocia: prediction and management. Womens Health (Lond) 2016;12(02):251–261. doi: 10.2217/whe.15.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sentilhes L, Sénat M V, Boulogne A I et al. Shoulder dystocia: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF) Eur J Obstet Gynecol Reprod Biol. 2016;203:156–161. doi: 10.1016/j.ejogrb.2016.05.047. [DOI] [PubMed] [Google Scholar]
- 35.Sandmire H F, DeMott R K. Erb's palsy causation: a historical perspective. Birth. 2002;29(01):52–54. doi: 10.1046/j.1523-536x.2002.00156.x. [DOI] [PubMed] [Google Scholar]
- 36.Zaki M SI, el Sabbagh M H, Aglan M S. Familial congenital brachial palsy: a report of two affected Egyptian families. Genet Couns. 2004;15(01):27–36. [PubMed] [Google Scholar]
- 37.Mollica F, Li Volti S, Grasso A, De Simone D. Familial congenital brachial palsy. Am J Med Genet. 1991;41(03):322–324. doi: 10.1002/ajmg.1320410312. [DOI] [PubMed] [Google Scholar]
- 38.McAbee G N, Ciervo C. Medical and legal issues related to brachial plexus injuries in neonates. J Am Osteopath Assoc. 2006;106(04):209–212. [PubMed] [Google Scholar]
- 39.Gherman R B, Ouzounian J G, Goodwin T M. Obstetric maneuvers for shoulder dystocia and associated fetal morbidity. Am J Obstet Gynecol. 1998;178(06):1126–1130. doi: 10.1016/s0002-9378(98)70312-6. [DOI] [PubMed] [Google Scholar]
- 40.Alfonso D T. Causes of neonatal brachial plexus palsy. Bull NYU Hosp Jt Dis. 2011;69(01):11–16. [PubMed] [Google Scholar]
- 41.Noble A. Brachial plexus injuries and shoulder dystocia: medico-legal commentary and implications. J Obstet Gynaecol. 2005;25(02):105–107. doi: 10.1080/01443610500051338. [DOI] [PubMed] [Google Scholar]
- 42.Hickson G B, Clayton E W, Githens P B, Sloan F A. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992;267(10):1359–1363. [PubMed] [Google Scholar]