Abstract
Objectives
Falls are associated with several negative outcomes. Early identification of those who are at risk of falling is of importance in geriatrics and comprehensive geriatric assessment (CGA) seems to be promising in this regard. Therefore, the present study investigated whether the multidimensional prognostic index (MPI), based on a standard CGA, is associated with falls in the Osteoarthritis Initiative (OAI).
Design
Longitudinal, 8 years of follow-up.
Setting and participants
Community-dwelling older people (≥ 65 years) with knee OA or at high risk for this condition.
Methods
A standardized CGA including information on functional, nutritional, mood, comorbidities, medications, quality of life and co-habitation status was used to calculate a modified version of the MPI, categorized as MPI-1 (low), MPI-2 (moderate) and MPI-3 (high risk). Falls were self-reported and recurrent fallers were defined as ≥2 in the previous year. Logistic regression was carried out and results are reported as odds ratio (ORs), with their 95% confidence intervals (CIs).
Results
The final sample consisted of 885 older adults (mean age 71.3 years, females=54.6%). Recurrent fallers showed a significant higher MPI than their counterparts (46.1±17.2 vs. 38.2±15.8; p<0.001). Compared to those in MPI-1 category, participants in MPI-2 (OR=2.13; 95%CI: 1.53–2.94; p<0.001) and in MPI-3 (OR=5.98; 95%CI: 3.29–10.86; p<0.001) reported a significant higher risk of recurrent falls over the 8-years of follow-up. Similar results were evident when using an increase in 0.1 points in the MPI or risk of falls after one year.
Conclusions and implications
Higher MPI values at baseline were associated with an increased risk of recurrent falls suggesting the importance of CGA in predicting falls in older people.
Keywords: multidimensional prognostic index, comprehensive geriatric assessment, falls, Osteoarthritis initiative
INTRODUCTION
Falls are a major public health concern in older people, significantly associated with adverse quality of life, increased physical comorbidity, healthcare use and early mortality.1 It has been estimated that approximately 1 in 3 people aged 65 years or older fall every year in the United States.2 It has been reported that falls are a frequent cause of disability, institutionalization, and mortality, and are among the primary causes of traumatic injury in older people in the United States.1–3
Several conditions are known as potential risk factors for falls, including reduction in muscle strength4, gait imbalance5, visual and hearing deficits6, osteoarthritis7, dementia8 and depression.9 The early identification of older adults who are at risk of falling is important in order to develop tailored interventions to prevent falls10. However, the prediction of such a risk of falling remains a challenge in geriatric medicine.11
Indeed, fall risk assessment tools currently used in geriatric medicine have not shown sufficiently high predictive validity for differentiating high and low fall risks.12 For example, the timed up and go, a common test for assessing the risk of falls, has only limited specificity (0.49) to predict falls in community dwelling older people and, therefore, should not be used alone for identifying individuals at high risk of falls.13 Other tools commonly used for assessing falls risk, e.g. the Berg Balance scale and Mobility Interaction Fall chart, the Downton Fall Risk Index and the Tinetti Balance scale, showed contrasting results, particularly in terms of sensitivity.12 As summarized by a recent systematic review and meta-analysis12, rather than a single measure, two assessment tools used together would better evaluate the characteristics of falls and therefore indicating that comprehensive geriatric assessment (CGA) could be used for better predicting fall risk in older people.
The Multidimensional Prognostic Index (MPI)14 is a well-calibrated tool with a good discrimination and accuracy for short and long-term mortality, both in a hospital setting15 and in older adults at the population level.16 Among all prognostic indexes available in geriatric medicine, the MPI is the only one based on information obtained from a CGA that explores comprehensively health, functional, cognitive, and nutritional domains, as well as social aspects, using standardized and extensively validated rating scales17, usually known by the clinicians with an optimal accuracy in identifying negative outcomes, such as mortality, (re)hospitalization and institutionalization. 14, 15, 18–23
Given this background, the present study aimed to investigate the association between MPI scores at baseline and risk of recurrent falls in a large cohort of North American adults followed up over 8 years, participating to the Osteoarthritis Initiative (OAI).
MATERIALS AND METHODS
Data source and subjects
Data were obtained from the Osteoarthritis Initiative (OAI) database. Participants were recruited across four clinical sites in the United States of America (Baltimore, MD; Pittsburgh, PA; Pawtucket, RI; and Columbus, OH) between February 2004 and May 2006. Participants were included if they: (1) had knee osteoarthritis (OA) with knee pain for a 30-day period in the past 12 months or (2) were at high risk of developing knee OA (e.g. overweight/obese (body mass index, BMI ≥25kg/m2), family history of knee OA).24 The data of this longitudinal cohort study were collected at baseline and during subsequent evaluations, with a follow-up of 8 years. All participants provided written informed consent. The OAI study was given full ethics approval by the institutional review board of the OAI Coordinating Center, at the University of California in San Francisco.
Calculation of the MPI
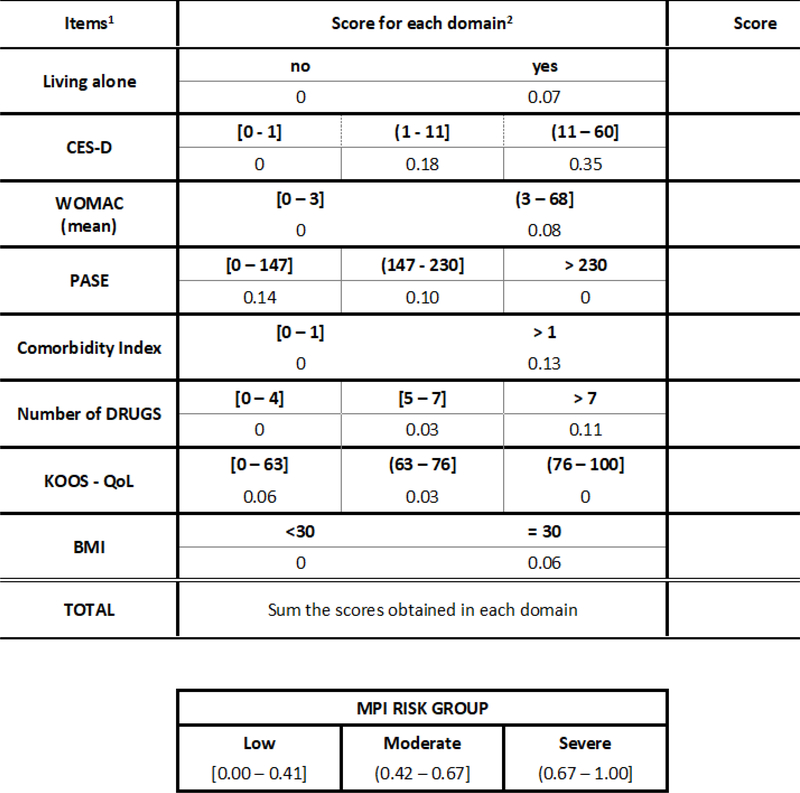
The MPI was calculated as established in previous studies, with some modification based on availability of data. Six of the original MPI domains were assessed by using standardized CGA scales: 1) physical functioning was assessed through the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) Index 25; 2) physical activity was measured through the Physical Activity Scale for the Elderly scale (PASE) 26; 3) nutritional aspects were evaluated using Body Mass Index (BMI); 4) comorbidity was assessed by the Charlson Comorbidity Index score27; 5) the number of medications used were reported; and 6) cohabitation status was reported, i.e. living alone (yes vs. no). Moreover, instead of cognitive status, the following was included in the multidimensional model: 7) the assessment of depressive symptoms by using the Center for Epidemiologic Studies Depression Scale (CES-D)28, and 8) quality of life assessed through a specific subscale of the Knee injury Osteoarthritis Outcome Score (KOOS).29 Full details are reported in Figure 1.
Fig. 1.
Multidimensional prognostic index in the Osteoarthritis Initiative.
When a categorization was not available from literature, the optimal number and location of cutoff points were determined using an iterative algorithm that maximizes the relative area under the curve (AUC).30 For each potential predictors according to the outcome in order to define different risk groups and quantify the weight of each of them in a creation of a multidimensional index from the estimates of a multivariate logistic regression (Table 1).
Table 1.
Multivariate logistic model for recurrent fallers and weight for a multidimensional score (adjusted for age and sex).
| OR (95%CI) | p-value | Weights for MPI | ||
|---|---|---|---|---|
| Living alone | no | ref. | 0.280 | 0.00 |
| Yes | 1.23 (0.85 – 1.78) | 0.07 | ||
| CES-D | [0 – 1] | ref. | 0.001 | 0.00 |
| (1 – 11] | 1.70 (1.15 – 2.50) | 0.18 | ||
| (11 – 60] | 2.82 (1.65 – 4.83) | 0.35 | ||
| WOMAC-mean | [0 – 3] | ref. | 0.247 | 0.00 |
| (3 – 68] | 1.27 (0.85 – 1.90) | 0.08 | ||
| PASE | > 230 | ref. | 0.412 | 0.00 |
| (147 – 230] | 1.34 (0.65 – 2.77) | 0.10 | ||
| [0 – 147] | 1.53 (0.76 – 3.09) | 0.14 | ||
| Comorbidity | [0 – 1] | ref. | 0.082 | 0.00 |
| >1 | 1.48 (0.95 – 2.30) | 0.13 | ||
| Number of Drugs | [0 – 4] | ref. | 0.478 | 0.00 |
| [5 – 7] | 1.10 (0.76 – 1.60) | 0.03 | ||
| > 7 | 1.39 (0.81 – 2.40) | 0.11 | ||
| KOOS – QoL | (76 – 100] | ref. | 0.770 | 0.00 |
| (63 – 76] | 1.10 (0.70 – 1.73) | 0.03 | ||
| [0 – 63] | 1.19 (0.75 – 1.88) | 0.06 | ||
| BMI | < 30 | ref. | 0.301 | 0.00 |
| ≥ 30 | 1.20 (0.85 – 1.69) | 0.06 | ||
Abbreviations: CES-D: Center for Epidemiologic Studies – Depression; WOMAC: Western Ontario and Mc Master University; PASE: Physical Activity Scale for Elderly; KOOS: Knee Injury and Osteoarthritis Outcome Score; QoL: quality of life; BMI: body mass index; MPI: Multidimensional Prognostic Index
This modified MPI, obtained as weighted sum of each domain, ranged from 0.0 (low risk of recurrent fall) to 1.0 (highest risk of recurrent fall). Moreover, as for the individual covariates that explore each domain, also MPI was categorized into three statistically different risk groups of recurrent falls: low risk 0–0.41, moderate risk 0.42 – 0.67 and severe risk 0.68 – 1.0 (Figure 1).
Definition of “recurrent fallers”
A fall is traditionally defined as “an event which resulted in a person coming to rest inadvertently on the ground or floor or other lower level.”31
The assessment of the outcome was made at baseline and during the follow-up visits at 12, 24, 36, 48, 72 and 96 months. At the end of each wave, including baseline evaluation, participants reported the number of falls experienced in the preceding year by answering this question: “Did you fall during the past year?”. The number of falls was also recorded. On the contrary, no information was available regarding the date of falling. The primary outcome for this study was categorized as: recurrent fallers (i.e. falls ≥ 2 in the previous year) vs. no recurrent fallers (0–1 falls in the previous year).
We considered as outcomes both long-term recurrent falls (i.e. any recurrence of falls during follow-up period) and short-term recurrence of falls (i.e. in the first year after the baseline evaluation).
Statistical analyses
Data on continuous variables were normally distributed according to the Kolmogorov-Smirnov test. Data were presented as means and standard deviation values (SD) for quantitative measures (if normally distributed) or as medians and interquartile ranges (if not normally distributed), and percentages for all categorical variables by recurrence of falls during follow-up period (yes vs. no). P-values were calculated with the Fisher’s Exact test for frequencies, Mann-Whitney test for medians and t-Test for means.
Logistic binary regression analysis was run, taking the MPI at admission (in categories or as increase in 0.1 points) as the exposure variable and recurrence of falls (during follow-up and after one year) as the outcome variable. The strength of the association between MPI at admission and the outcomes of interest were reported as odds ratios (ORs) with their 95 % confidence intervals (CIs). For all the outcomes, receiver operator characteristic (ROC) curves were analyzed to compare the sensitivity and specificity of MPI in predicting recurrence of falls, measuring the relative area under the curve (AUC), with the correspondent 95%CI.
A p<0.05 was deemed statistically significant. Analyses were performed using STATA® software version 14.1 (Stata Corp LP, College station, Texas).
RESULTS
Sample selection
The OAI dataset initially included a total of 4,796 individuals. At the baseline, 2974 individuals were excluded because they were not defined as older people (i.e. they were younger than 65 years), 279 since they were not White or Caucasian (race could be a possible confounder that we could not take into account for a lower number of individuals of other races) and 507 people with previous falls at baseline. Moreover, 151 subjects were excluded because they had missing data for one or more domains of interest in the creation of the MPI. Finally, 885 people were included in this analysis.
Baseline characteristics
The cohort included 483 women (54.6%), with a mean age of 71.3 years (±4.0 years; range: 60–79 years). The mean MPI at baseline was 0.40±0.16 (range: 0.0 – 1.0).
Table 2 illustrates the baseline characteristics by recurrence of falls during follow-up and in the sample as a whole. During the 8 years of follow-up, 223 participants (=25.2% of the baseline population) were classified as recurrent fallers. As shown in Table 2, no significant differences between recurrent fallers (n=223) and no recurrent fallers (n=662) were observed in terms of sex (p=0.816), mean age (p=0.458) or co-habitation (p=0.173). On the contrary, recurrent fallers were more disabled, had a higher rate of comorbidities, used more medications and were more depressed with a poorer quality of life than their counterparts (Table 2). Finally, recurrent fallers showed a significant higher MPI than non-fallers (0.46±0.17 vs. 0.38±0.16; p<0.001) (Table 2).
Table 2.
Descriptive statistics of patients’ characteristics according to fall risk.
| Recurrent fallers |
p-value | ||||
|---|---|---|---|---|---|
| Overall 885 (100.0%) |
No 662 (74.8%) |
Yes 223 (25.2%) |
|||
| Sex, n(%) | F | 483 (54.6) | 363 (54.8) | 120 (53.8) | 0.816 |
| M | 402 (45.4) | 299 (45.2) | 103 (46.2) | ||
| Age, mean(sd) | 71.3 (4.0) | 71.3 (4.0) | 71.5 (3.9) | 0.458 | |
| Living alone, n(%) | No | 674 (76.2) | 512 (77.3) | 162 (72.6) | 0.173 |
| Yes | 211 (23.8) | 150 (22.7) | 61 (27.4) | ||
| CES-D, median (IQR) | 4 (1 – 8) | 3 (1 – 7) | 5 (2 – 9) | 0.002 | |
| CES-D, n(%) | [0 – 1] | 260 (29.4) | 216 (32.6) | 44 (19.7) | < 0.001 |
| (1 – 11] | 528 (59.6) | 388 (58.6) | 140 (62.8) | ||
| (11 – 60] | 97 (11.0) | 58 (8.8) | 39 (17.5) | ||
| WOMAC-mean, median(IQR) | 3.2 (0.0 – 10.5) | 3.0 (0.0 – 10.0) | 4.8 (0.5 – 12.5) | 0.008 | |
| WOMAC-mean, n(%) | [0 – 3] | 438 (49.5) | 345 (52.1) | 93 (41.7) | 0.016 |
| (3 – 8] | 164 (18.5) | 121 (18.3) | 43 (19.3) | ||
| (8 – 68] | 283 (32.0) | 196 (29.6) | 87 (39.0) | ||
| PASE, median(IQR) | 129 (93 – 168) | 131 (93 – 170) | 126 (92 – 162) | 0.305 | |
| PASE, n(%) | [0 – 147] | 551 (62.2) | 403 (60.9) | 148 (62.3) | 0.257 |
| (147 – 230] | 274 (31.0) | 210 (31.7) | 64 (28.7) | ||
| > 230 | 60 (6.8) | 49 (7.4) | 11 (4.9) | ||
| Comorbidity, n(%) | [0 – 1] | 763 (86.2) | 583 (88.1) | 180 (80.7) | 0.009 |
| >1 | 122 (13.8) | 79 (11.9) | 43 (19.3) | ||
| Number of Drugs median(IQR) | 3 (2 – 5) | 3 (2 – 5) | 4 (2 – 5) | 0.116 | |
| Number of Drugs, n(%) | [0 – 4] | 604 (68.2) | 465 (70.2) | 139 (62.3) | 0.050 |
| [5 – 7] | 206 (23.3) | 148 (22.4) | 58 (26.0) | ||
| > 7 | 75 (8.5) | 49 (7.4) | 26 (11.7) | ||
| KOOS – QoL, median(IQR) | 75.0 (56.3 – 87.5) | 75.0 (62.5 – 87.5) | 68.8 (56.3 – 87.5) | 0.020 | |
| KOOS – QoL, n(%) | [0 – 63] | 332 (37.5) | 235 (35.5) | 97 (43.5) | 0.045 |
| (63 – 76] | 209 (23.6) | 155 (23.4) | 54 (24.2) | ||
| (76 – 100] | 344 (38.9) | 272 (41.1) | 72 (32.3) | ||
| BMI, n(%) | < 30 | 627 (70.9) | 480 (72.5) | 147 (65.9) | 0.073 |
| ≥ 30 | 258 (29.1) | 182 (27.5) | 76 (34.1) | ||
| MPI, mean(sd) | 0.40 (0.17) | 0.38 (0.16) | 0.46 (0.17) | < 0.001 | |
| MPI risk group, n(%) | Low (0–0.41) | 471 (53.2) | 389 (58.8) | 82 (36.8) | < 0.001 |
| moderate (0.42–0.67) | 362 (40.9) | 250 (37.8) | 112 (50.2) | ||
| severe (0.68–1.0) | 52 (5.9) | 23 (3.4) | 29 (13.0) | ||
Notes: p-values were referred to Fisher’s Exact test for frequencies, Mann-Whitney test for medians and t-Test for means.
Abbreviations: CES-D: Center for Epidemiologic Studies – Depression; WOMAC: Western Ontario and Mc Master University; PASE: Physical Activity Scale for Elderly; KOOS: Knee Injury and Osteoarthritis Outcome Score; QoL: quality of life; BMI: body mass index; MPI: Multidimensional Prognostic Index
Table 3 shows the logistic regression analysis and the prediction capability of the MPI in predicting recurrence of falls during the 8 years of follow-up. An increase of 0.1 on the MPI scale was associated with a significant higher risk of recurrence of falls during follow-up of 34% (OR=1.34; 95%CI: 1.22–1.48; p<0.001). We observed that those subjects in moderate (MPI-2) and severe risk (MPI-3) reported overall incidence of recurrent falls almost doubled and tripled compared to those with the lowest values of MPI-1 as reference (30.9% and 55.8% vs. 17.4%, respectively). Compared to those in MPI-1 category, participants in MPI-2 (OR=2.13; 95%CI: 1.53–2.94; p<0.001) and in MPI-3 (OR=5.98; 95%CI: 3.29–10.86; p<0.001) reported a significant higher risk of recurrent falls. The AUC of the MPI in predicting recurrent falls during the 8 years of follow-up was 62.7%, 95%CI: 58.5–66.9.
Table 3.
Logistic regression and prediction capability of MPI on a continuous scale and stratified by several groups of risk, taking recurrent fallers during 8 years of follow-up as the outcome.
| Recurrent fallers (during follow-up) | ||||
| Recurrent fallers (%) | OR (95%CI) | p-value | ||
| MPI (x 0.1 increase) | 223/885 (25.2%) | 1.34 (1.22 – 1.48) | < 0.001 | |
| MPI | Low (0–0.41) | 82/471 (17.4%) | ref. | < 0.001 |
| moderate (0.42–0.67) | 112/362 (30.9%) | 2.13 (1.53 – 2.94) | ||
| severe (0.68–1.0) | 29/52 (55.8%) | 5.98 (3.29 – 10.86) | ||
| Recurrent fallers at one year | ||||
| Recurrent fallers at 1 year (%) | OR (95%CI) | p-value | ||
| MPI (x 0.1 increase) | 49/885 (5.5%) | 1.48 (1.25 – 1.76) | < 0.001 | |
| MPI | Low (0–0.41) | 13/471 (2.8%) | ref. | < 0.001 |
| moderate (0.42–0.67) | 26/362 (7.2%) | 2.73 (1.38 – 5.38) | ||
| severe (0.68–1.0) | 10/52 (19.2%) | 8.39 (3.47 – 20.28) | ||
Abbreviations: MPI: Multidimensional Prognostic Index; OR: odds ratio; CI: confidence interval
Table 3 shows similar analyses, taking recurrence of falls after one year as the outcome. Again, MPI significantly predicts the risk of falls, using this tool as a continuous measure since an increase in 0.1 points corresponds to an increase risk of falls of 48% (increase in 0.1 point; OR=1.48; 95%CI: 1.25–1.76; p<0.001) or using groups (MPI-2: OR=2.73; 95%CI: 1.38–5.38; p<0.001; MPI-3: OR=8.39; 95%CI: 3.47–20.28; p<0.001) (Table 3). The accuracy in terms of AUC for this outcome was 68.5%; 95%CI: 60.8 – 76.2%.
DISCUSSION
In this longitudinal study, over eight years of follow-up, we found that a modified version of the MPI is able to predict the onset of recurrent falls in older people living in the community and affected by OA or at high risk for this condition. These data are confirmed both over a short- (after one year from baseline evaluation) and in long-term follow-up (up to eight years).
We observed that a high proportion of people fell during the follow-up period and about a quarter of the participants fell more than two times every year. We know that, from an epidemiological perspective, falls are the second leading cause of injury deaths worldwide, particularly in older people. 31 The present study further reinforces this epidemiological evidence.
The topic of frailty and risk of falls is of great interest in geriatric medicine. A systematic review and meta-analysis in 102,130 community-dwelling older adults found that compared with robust older adults, frail older persons demonstrated the greatest risk for falls (OR=2.50; 95%CI: 1.58–3.96), followed by prefrail older adults (OR=1.47; 1.22–1.79), being similar, also in strength, to the present findings.32 This evidence was also confirmed by a previous meta-analysis regarding this topic.33 Of importance, in these meta-analyses, frail older adults also demonstrate higher risk for recurrent falls 32, 33 and also of fractures, particularly of hip fractures. 34
The MPI has been validated in over 12,000 patients suffering from acute and chronic conditions35, 36, demonstrating in a multicentre study a significant higher mortality predictive accuracy than three other frailty instruments.37 More recently another multicentre international study confirmed that the MPI was significantly associated with a higher risk of mortality and even with re-hospitalization, higher necessity of home-care needs and institutionalization in hospitalized older patients. 38 The research proposed in this work further reinforces the utility of the MPI in predicting another negative outcome in older people, i.e. falls. Overall, the current findings suggest the importance of CGA in predicting the risk of falls.
However, the CGA seems to be important not only for the detection of future falls, but also for the management of this frequent condition, particularly when interventions include nutritional and physical activity programs.39 A recent large randomized controlled trial, for example, has reported that a home-based exercise program is able to decrease the incidence of falls in older people.40 Therefore, the present findings can add further evidence of the importance of carrying out CGA in older people in order to early identify the risk of falls in this population and to tailor specific interventions for frail older adults, if needed. In this regard, our study reported that MPI has a discrete accuracy, having an AUC of 60–70% in predicting falls during follow-up and after one year, being similar to other tools commonly used in geriatric medicine for predicting falls risk.12
The findings from this study should be interpreted in light of its limitations. First, the OAI is a cohort that includes only individuals who already have or are at high risk of knee OA. Thus, our results are not applicable to the general population. Second, falls were self-reported by the patients and not recorded with standardized diaries. It is largely known that retrospective recall of falls is not a reliable way to ascertain falls and the agreement between recall of falls and diaries is often poor since the patients often underestimate falls. 41, 42 Third, our analysis should be considered as preliminary in the context of the OAI. For example, MPI was validated only in Whites and, consequently, if our results can be applied in other populations is still to be explored that, according to the literature, have a different fall’ risk.43
CONCLUSIONS AND IMPLICATIONS
Our data suggest that, in this cohort of people affected by knee osteoarthritis or at high risk for this condition, higher MPI values at baseline may be associated with an increased risk of recurrent falls suggesting the importance of comprehensive geriatric assessment in predicting this condition in older people. Future longitudinal studies (also in other settings) are needed to confirm our findings.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age ageing 2006;35(suppl_2):ii37–ii41. [DOI] [PubMed] [Google Scholar]
- 2.Pahor M Falls in older adults: prevention, mortality, and costs. JAMA 2019;321(21):2080–2081. [DOI] [PubMed] [Google Scholar]
- 3.Hartholt KA, Lee R, Burns ER, et al. Mortality from falls among US adults aged 75 years or older, 2000–2016. JAMA 2019;321(21):2131–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reis P, Moro A, Bins Ely V, et al. Universal design and accessibility: an approach of the influence of muscle strength loss in the risk of falls in the elderly. Work 2012;41(Supplement 1):374–379. [DOI] [PubMed] [Google Scholar]
- 5.Shumway-Cook A, Baldwin M, Polissar NL, et al. Predicting the probability for falls in community-dwelling older adults. Phys ther 1997;77(8):812–819. [DOI] [PubMed] [Google Scholar]
- 6.Dhital A, Pey T, Stanford MR. Visual loss and falls: a review. Eye 2010;24(9):1437. [DOI] [PubMed] [Google Scholar]
- 7.Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age ageing 2013;42(5):561–566. [DOI] [PubMed] [Google Scholar]
- 8.Van Doorn C, Gruber-Baldini AL, Zimmerman S, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Ger Soc 2003;51(9):1213–1218. [DOI] [PubMed] [Google Scholar]
- 9.Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Ger Psych 2013;21(5):484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Callaghan B, Kerber K, Langa KM, et al. Longitudinal patient-oriented outcomes in neuropathy: importance of early detection and falls. Neurology 2015;85(1):71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hazzard WR, Halter JB. Hazzard’s geriatric medicine and gerontology, 2009. [Google Scholar]
- 12.Park S-H. Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Aging Clin Exp Res 2018;30(1):1–16. [DOI] [PubMed] [Google Scholar]
- 13.Barry E, Galvin R, Keogh C, et al. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC ger 2014;14(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pilotto A, Ferrucci L, Franceschi M, et al. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rej res 2008;11(1):151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sancarlo D, D’Onofrio G, Franceschi M, et al. Validation of a Modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging 2011;15(3):169–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angleman SB, Santoni G, Pilotto A, et al. Multidimensional Prognostic Index in Association with Future Mortality and Number of Hospital Days in a Population-Based Sample of Older Adults: Results of the EU Funded MPI_AGE Project. PloS one 2015;10(7):e0133789–e0133789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: a systematic review. JAMA 2012;307(2):182–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau ML, Liuu E, Christiaens L, et al. Using a multidimensional prognostic index (MPI) based on comprehensive geriatric assessment (CGA) to predict mortality in elderly undergoing transcatheter aortic valve implantation. Int J Cardiol 2017;236:381–386. [DOI] [PubMed] [Google Scholar]
- 19.Pilotto A, Addante F, Ferrucci L, et al. The multidimensional prognostic index predicts short- and long-term mortality in hospitalized geriatric patients with pneumonia. J Gerontol A Biol Sci Med Sci 2009;64(8):880–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pilotto A, Sancarlo D, Panza F, et al. Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short-term mortality in older patients with heart failure. Circ Heart fail 2010;3(1):191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sancarlo D, Pilotto A, Panza F, et al. A Multidimensional Prognostic Index (MPI) based on a comprehensive geriatric assessment predicts short- and long-term all-cause mortality in older hospitalized patients with transient ischemic attack. J Neurol 2012;259(4):670–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Volpato S, Bazzano S, Fontana A, et al. Multidimensional Prognostic Index predicts mortality and length of stay during hospitalization in the older patients: a multicenter prospective study. J Gerontol A Biol Sci Med Sci 2015;70(3):325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilotto A, Veronese N, Daragjati J, et al. Using the Multidimensional Prognostic Index to Predict Clinical Outcomes of Hospitalized Older Persons: a Prospective, Multicentre, International Study. J Gerontol A Biol Sci Med Sci 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Med Hypoth 2006;67(2):362–370. [DOI] [PubMed] [Google Scholar]
- 25.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J rheumat 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 26.Washburn RA, McAuley E, Katula J, et al. The physical activity scale for the elderly (PASE): evidence for validity. J clin epid 1999;52(7):643–651. [DOI] [PubMed] [Google Scholar]
- 27.Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Med care 1996;34(1):73–84. [DOI] [PubMed] [Google Scholar]
- 28.Lewinsohn PM, Seeley JR, Roberts RE, et al. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging 1997;12(2):277–287. [DOI] [PubMed] [Google Scholar]
- 29.Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J Knee Surg Sports Traumatol Arthrosc 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 30.Chang C, Hsieh M-K, Chang W-Y, et al. Determining the optimal number and location of cutoff points with application to data of cervical cancer. PloS one 2017;12(4):e0176231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Organization WH. Ageing; Life Course Unit. WHO global report on falls prevention in older age. World Health Organization 2008. [Google Scholar]
- 32.Cheng MH, Chang SF. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis. J Nurs Scholarsh 2017;49(5):529–536. [DOI] [PubMed] [Google Scholar]
- 33.Kojima G Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. JAMDA 2015;16(12):1027–1033. [DOI] [PubMed] [Google Scholar]
- 34.Chen KW, Chang SF, Lin PL. Frailty as a Predictor of Future Fracture in Older Adults: A Systematic Review and Meta-Analysis. Worldviews Evid Based Nurs 2017;14(4):282–293. [DOI] [PubMed] [Google Scholar]
- 35.Pilotto A, Sancarlo D, Daragjati J, et al. Perspective: the challenge of clinical decisionmaking for drug treatment in older people. The role of multidimensional assessment and prognosis. Frontiers med 2014;1:61–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pilotto A, Panza F, Ferrucci L A multidimensional prognostic index in common conditions leading to death in older patients. Arch Intern Med 2012;172(7):594; discussion 594–595. [DOI] [PubMed] [Google Scholar]
- 37.Pilotto A, Rengo F, Marchionni N, et al. Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS One 2012;7(1):e29090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pilotto A, Veronese N, Daragjati J, et al. Using the Multidimensional Prognostic Index to Predict Clinical Outcomes of Hospitalized Older Persons: A Prospective, Multicenter, International Study. J Gerontol A Biol Sci Med Sci 2018; doi: 10.1093/gerona/gly239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Panel on Prevention of Falls in Older Persons, AGS, Society, BG. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Ger Soc 2011;59(1):148–157. [DOI] [PubMed] [Google Scholar]
- 40.Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a home-based exercise program on subsequent falls among community-dwelling high-risk older adults after a fall: a randomized clinical trial. JAMA 2019;321(21):2092–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ganz DA, Higashi T, Rubenstein LZ . Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Ger Soc 2005;53(12):2190–2194. [DOI] [PubMed] [Google Scholar]
- 42.Griffin J, Lall R, Bruce J, et al. Comparison of alternative falls data collection methods in the Prevention of Falls Injury Trial (PreFIT). J clin epid 2019;106:32–40. [DOI] [PubMed] [Google Scholar]
- 43.Geng Y, Lo JC, Brickner L, et al. Racial-ethnic differences in fall prevalence among older women: a cross-sectional survey study. BMC ger 2017;17(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]