Abstract
Background
Coronavirus disease 2019 (COVID-19) is likely to have significant implications for the cardiovascular care of patients. In most countries, containment has already started (on 17 March 2020 in France), and self-quarantine and social distancing are reducing viral contamination and saving lives. However, these considerations may only be the tip of the iceberg; most resources are dedicated to the struggle against COVID-19, and this unprecedented situation may compromise the management of patients admitted with cardiovascular conditions.
Aim
We aimed to assess the effect of COVID-19 containment measures on cardiovascular admissions in France.
Methods
We asked nine major cardiology centres to give us an overview of admissions to their nine intensive cardiac care units for acute myocardial infarction or acute heart failure, before and after containment measures.
Results
Before containment (02–16 March 2020), the nine participating intensive cardiac care units admitted 4.8 ± 1.6 patients per day, versus 2.6 ± 1.5 after containment (17–22 March 2020) (rank-sum test P = 0.0006).
Conclusions
We confirm here, for the first time, a dramatic drop in the number of cardiovascular admissions after the establishment of containment. Many hypotheses might explain this phenomenon, but we feel it is time raise the alarm about the risk for patients presenting with acute cardiovascular disease, who may suffer from lack of attention, leading to severe consequences (an increase in the number of ambulatory myocardial infarctions, mechanical complications of myocardial infarction leading to an increase in the number of cardiac arrests, unexplained deaths, heart failure, etc.). Similar consequences can be feared for all acute situations, beyond the cardiovascular disease setting.
Keywords: COVID-19, Acute cardiac care, Intensive care unit, Acute coronary syndrome, Heart failure
Résumé
Contexte
La maladie du coronavirus 2019 (COVID-19) a des implications importantes concernant la prise en charge des problèmes cardiovasculaires. Dans la plupart des pays, le confinement a déjà commencé (en France le 17 mars) et l’isolement, la distanciation sociale, réduisent la contamination virale et sauvent des vies. Ces considérations ne pourraient être cependant que la partie émergée de l’iceberg. Parce que la plupart des ressources sont consacrées à la lutte contre le COVID-19, cette situation sans précédent pourrait compromettre la prise en charge des patients admis pour des problèmes cardiovasculaires.
Objectif
Notre objectif était d’évaluer l’impact des mesures de confinement du COVID-19 sur les admissions cardiovasculaires en France.
Méthodes
Nous avons demandé à plusieurs grands centres de cardiologie de nous donner un aperçu de leurs admissions en USIC pour infarctus aigu du myocarde ou insuffisance cardiaque aiguë.
Résultats
Avant le confinement (du 02 au 16 mars), les neuf USIC participantes ont admis 4,6 ± 1,6 patients par jour, contre 2,6 ± 1,5 après le confinement (du 17 au 22 mars) (P = 0,0006).
Conclusions
Nous confirmons ici pour la première fois une baisse spectaculaire du nombre d’admissions après la mise en place du confinement. De nombreuses hypothèses pourraient expliquer ce phénomène, mais nous pensons qu’il est temps d’alerter sur le risque pour les patients présentant une maladie cardiovasculaire aiguë, de souffrir du manque d’attention, entraînant des conséquences graves (augmentation du nombre d’infarctus du myocarde ambulatoires, conduisant à une augmentation du nombre d’arrêts cardiaques, décès inexpliqués, insuffisance cardiaque, etc.). Des conséquences similaires pourraient être craintes pour toutes les situations aiguës en dehors des maladies cardiovasculaires.
Mots clés: COVID-19, Soins cardiaques aigus ;Unité de soins intensifs, Syndrome coronarien aigu, Insuffisance cardiaque
Background
Coronavirus disease 2019 (COVID-19) is likely to have significant implications for the cardiovascular care of patients [1]. Indeed, patients with cardiovascular disease seem to experience more severe symptoms of COVID-19 infection, but the virus may also lead to direct and indirect cardiovascular complications, including acute myocardial infarction (AMI), myocarditis, arrhythmias and venous thromboembolism.
While the COVID-19 pandemic is rapidly spreading through Europe, killing people, tiring healthcare workers and filling hospitals [2], critical care units have developed effective therapeutic tools, including extracorporeal membrane oxygenation (ECMO) and respiratory assistance. In most countries, containment has already started (on 17 March 2020 in France), and isolation and social distancing are reducing viral contamination and saving lives. However, these considerations may only be the tip of the iceberg; most resources are dedicated to the struggle against COVID-19, and this unprecedented situation may compromise the management of patients admitted with cardiovascular conditions. This could be of crucial importance to bear in mind for caregivers, health system managers and, above all, patients.
Consistently, many cardiologists involved in acute cardiovascular care have noticed a reduction in patient admissions following containment measures, including for AMI. Taking these considerations into account, we hypothesized that since the onset of the containment, the number of patients admitted to intensive cardiac care units (ICCUs) for AMI or acute heart failure (AHF) could have fallen. If true, the COVID-19 pandemic might increase cardiovascular death in multiple ways, weakening patients with pre-existing cardiovascular conditions, generating inflammatory myocarditis and reducing our ability to quickly evaluate patients with acute cardiovascular disease who are not infected with COVID-19 (or concomitantly those who are infected with COVID-19) [1].
Methods
We asked several major cardiology centres to give us an overview of their ICCU admissions for AMI or AHF. To be as fair as possible in this evaluation, we considered only large centres outside the epicentre of the pandemic in France (i.e. not in the east of the country). About one-third of the university centres answered, and extensively documented the numbers of patients admitted to ICCUs in March 2020, to enable us to follow the effect of this present unprecedented situation. The mean number of admissions by centre was computed each day. These means were compared before and under containment, using a Wilcoxon-Mann-Whitney test.
Results
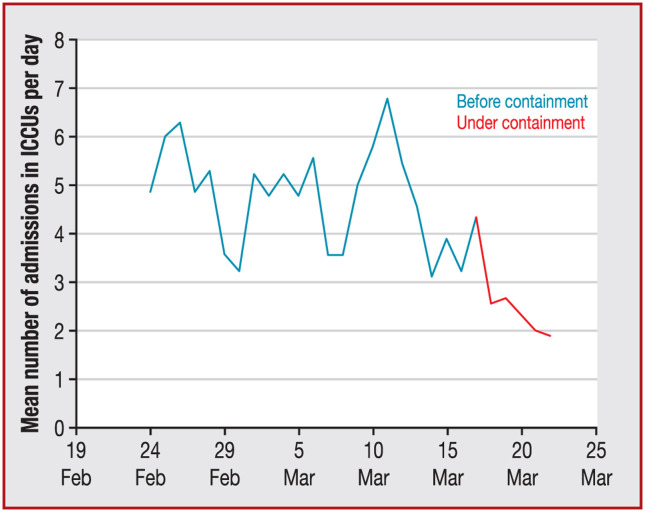
Before containment (2–16 March 2020), the nine participating ICCUs admitted 4.8 ± 1.6 patients per day, versus 2.6 ± 1.5 after containment (17–22 March 2020) (rank-sum test P = 0.0006). During the same period, ICCUs admitted 1.0 ± 0.7 patients with ST-segment elevation myocardial infarction (STEMI) per day, versus 0.6 ± 0.7 after containment (rank-sum test P = 0.02), 1.4 ± 0.8 patients with non-STEMI per day, versus 0.5 ± 0.7 after containment (rank-sum test P = 0.0009), and 1.5 ± 0.9 patients with AHF per day, versus 0.8 ± 1.0 after containment (rank-sum test P = 0.002). Details are provided in Fig. 1 , Fig. A.1 and Table 1 .
Figure 1.
Mean number of patients admitted each day to nine intensive cardiac care units (ICCUs) in France, before and after containment.
Table 1.
Mean number of patients admitted each day to nine intensive cardiac care units in France, before and after containment, with details by centre and pathology.
| Hospital | Number of beds in ICCU | Pathology of interest | Before containment | After containment |
|---|---|---|---|---|
| 1 | 15 | STEMI | 1.06 ± 0.72 | 0.00 ± 0.00 |
| NSTEMI | 1.06 ± 0.59 | 0.17 ± 0.41 | ||
| AHF | 0.69 ± 0.77 | 0.50 ± 1.22 | ||
| All admissions | 4.06 ± 0.96 | 0.83 ± 1.60 | ||
| 2 | 24 | STEMI | 2.36 ± 0.95 | 1.17 ± 1.17 |
| NSTEMI | 2.86 ± 0.91 | 1.17 ± 0.75 | ||
| AHF | 2.14 ± 0.93 | 0.83 ± 0.75 | ||
| All admissions | 7.36 ± 2.07 | 3.17 ± 1.33 | ||
| 3 | 20 | STEMI | 1.00 ± 0.63 | 0.83 ± 0.98 |
| NSTEMI | 1.25 ± 0.84 | 0.50 ± 0.55 | ||
| AHF | 1.87 ± 1.44 | 0.60 ± 0.89 | ||
| All admissions | 7.00 ± 2.13 | 3.67 ± 1.75 | ||
| 4 | 12 | STEMI | 1.05 ± 0.88 | 0.33 ± 0.52 |
| NSTEMI | 2.59 ± 1.44 | 0.67 ± 1.21 | ||
| AHF | 0.45 ± 0.58 | 0.00 ± 0.00 | ||
| All admissions | 4.09 ± 1.57 | 1.00 ± 1.10 | ||
| 5 | 16 | STEMI | 1.09 ± 0.75 | 0.83 ± 0.75 |
| NSTEMI | 1.23 ± 0.81 | 0.17 ± 0.41 | ||
| AHF | 1.32 ± 1.05 | 0.83 ± 1.60 | ||
| All admissions | 5.68 ± 1.81 | 4.00 ± 2.37 | ||
| 6 | 12 | STEMI | 0.35 ± 0.49 | 0.33 ± 0.52 |
| NSTEMI | 0.71 ± 0.68 | 0.67 ± 0.52 | ||
| AHF | 0.76 ± 0.65 | 0.83 ± 1.17 | ||
| All admissions | 2.68 ± 1.44 | 2.50 ± 1.22 | ||
| 7 | 20 | STEMI | 0.86 ± 0.63 | 1.17 ± 0.98 |
| NSTEMI | 0.64 ± 0.69 | 0.33 ± 0.82 | ||
| AHF | 2.77 ± 1.07 | 1.67 ± 0.82 | ||
| All admissions | 4.27 ± 1.41 | 3.17 ± 0.75 | ||
| 8 | 20 | STEMI | 0.82 ± 0.60 | 0.50 ± 0.84 |
| NSTEMI | 0.91 ± 0.50 | 1.00 ± 0.89 | ||
| AHF | 1.59 ± 1.01 | 1.17 ± 1.83 | ||
| All admissions | 1.68 ± 0.90 | 1.50 ± 1.52 | ||
| 9 | 20 | STEMI | 0.52 ± 0.65 | 0.17 ± 0.41 |
| NSTEMI | 0.90 ± 0.52 | 0.17 ± 0.41 | ||
| AHF | 1.48 ± 0.93 | 0.50 ± 0.55 | ||
| All admissions | 6.14 ± 2.42 | 3.83 ± 1.47 | ||
| Total | 159 | STEMI | 1.01 ± 0.70 | 0.59 ± 0.69 |
| NSTEMI | 1.35 ± 0.78 | 0.54 ± 0.66 | ||
| AHF | 1.45 ± 0.94 | 0.77 ± 0.98 | ||
| All admissions | 4.77 ± 1.63 | 2.63 ± 1.46 |
Data are expressed as mean ± standard deviation. AHF: acute heart failure; ICCU: intensive cardiac care unit; NSTEMI: non-ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction.
Discussion
We confirm here for the first time a dramatic drop in the number of admissions to ICCUs after the establishment of containment against COVID-19 in France. Many hypotheses might explain this phenomenon. Global measures and public-health messages may have created patient self-censorship, because of fear of possible in-hospital contamination or a lengthy wait before consultation in an overcrowded emergency room. Patients may also have refrained from consulting cardiologists, delaying detection of heart failure or worsening of coronary artery disease, and subsequent referral to an ICCU. Primary care physicians might not be available because of viral sickness or the reduction of non-urgent activity. The prehospital emergency system is probably unable to answer all the calls being made. Hospitals have allocated most resources to the COVID-19 challenges, so fewer resources are available for acute cardiac care. Importantly, similar considerations could be valid in all other acute situations. Finally, contained patients have probably significantly reduced their physical activity, with a possible reduction in the coronary plaque rupture that is responsible for AMI; it has been established that intense physical activity favours plaque rupture [3]. However, there are few data on the effect of a dramatic decrease in physical exertion on plaque stabilization.
Study limitations
We have to acknowledge some limitations to this work. This is only a partial view of the national situation, and there is probably high regional and local heterogeneity. We cannot exclude that at least some of the emergencies could be redirected to smaller healthcare centres reputed to be “COVID-19-free”. This is only a rapid, short survey, but we assume that a global trend could be confirmed on a large scale; we plan to confirm these results by analysing national databases that contain far more information. However, these results will be available too late, underlining the value of our approach, which facilitates a timely alert being raised. Above all, more detailed data are very important (including the delays and the main characteristics of patients, etc.).
Conclusions
We believe it is time to raise the alarm regarding the risk to patients presenting with acute cardiovascular disease, who may suffer a lack of attention, which might be inversely symmetrical to the expense of caring for patients infected with COVID-19. If true, many patients might die, in numbers that are much more difficult to quantify. The consequences could be serious, potentially resulting in an increase in the number of ambulatory myocardial infarctions, leading to an increase in the number of cardiac arrests, unexplained deaths and heart failure. For example, a recent paper found an significant increase in the time component of patients with STEMI in Hong Kong [4]. Similar consequences could be feared for all acute situations, beyond the cardiovascular disease setting.
All the available weapons in our armoury should be used. Depending on our local resources and possibilities, we could:
-
•
increase the use of teleconsultations and/or telemonitoring to better assess symptoms of high-risk patients;
-
•
use all validated apps to keep patients informed and involved in management of their cardiovascular disease;
-
•
warn healthcare workers, healthcare managers and deciders;
-
•
warn the public via all available media (social networks and more conventional media) regarding the need to contact a physician in case of signs of acute cardiovascular disease.
Funding
None.
Disclosure of interest
The authors declare that they have no competing interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.acvd.2020.04.002.
Appendix A. Supplementary data
Mean number of patients admitted each day to nine intensive cardiac care units (ICCUs) in France, before and after containment. A. Admissions for all causes. B. Admissions for ST-segment elevation myocardial infarction. C. Admissions for non − ST-segment elevation myocardial infarction. D. Admissions for acute heart failure.
References
- 1.Driggin E., Madhavan M.V., Bikdeli B., et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.03.031. Available at: http://www.onlinejacc.org/content/early/2020/03/18/j.jacc.2020.03.031 [accessed date: 26th March 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams J.G., Walls R.M. Supporting the Health Care Workforce During the COVID-19 Global Epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3972. Available at: https://jamanetwork.com/journals/jama/fullarticle/2763136 [accessed date: 27th March 2020] [DOI] [PubMed] [Google Scholar]
- 3.Kato A., Minami Y., Katsura A., et al. Physical exertion as a trigger of acute coronary syndrome caused by plaque erosion. J Thromb Thrombolysis. 2020;49:377–385. doi: 10.1007/s11239-020-02074-y. [DOI] [PubMed] [Google Scholar]
- 4.Tam C.F., Cheung K.S., Lam S., et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020 doi: 10.1161/CIRCOUTCOMES.120.006631. Available at: https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.120.006631 [accessed date: 27th March 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mean number of patients admitted each day to nine intensive cardiac care units (ICCUs) in France, before and after containment. A. Admissions for all causes. B. Admissions for ST-segment elevation myocardial infarction. C. Admissions for non − ST-segment elevation myocardial infarction. D. Admissions for acute heart failure.