Abstract
Background
In the vast majority of the laboratory-confirmed coronavirus disease 2019 (COVID-19) patients, computed tomography (CT) examinations yield a typical pattern and the sensitivity of this modality has been reported to be 97% in a large-scale study. Structured reporting systems simplify the interpretation and reporting of imaging examinations, serve as a framework for consistent generation of recommendations, and improve the quality of patient care.
Purpose
To compose a comprehensive lexicon for description of the imaging findings and propose a grading system and structured reporting format for CT findings in COVID-19.
Material and methods
We updated our published systematic review on imaging findings in COVID-19 to include 37 published studies pertaining to diagnostic features of COVID-19 in chest CT. Using the reported imaging findings of 3647 patients, we summarized the typical chest CT findings, atypical features, and temporal changes of COVID-19 in chest CT. Subsequently, we extracted a list of descriptive terms and mapped it to the terminology that is commonly used in imaging literature.
Results
We composed a comprehensive lexicon that can be used for documentation and reporting of typical and atypical CT imaging findings in COVID-19 patients. Using the same data, we propose a grading system with five COVID-RADS categories. Each COVID-RADS grade corresponds to a low, moderate, or high level of suspicion for pulmonary involvement of COVID-19.
Conclusion
The proposed COVID-RADS and common lexicon would improve the communication of findings to other healthcare providers, thus facilitating the diagnosis and management of COVID-19 patients.
Key Points
• Chest CT has high sensitivity in diagnosing the coronavirus disease 2019 (COVID-19).
• Structured reporting systems simplify the interpretation and reporting of imaging examinations, serve as a framework for consistent generation of recommendations, and improve the quality of patient care.
• The proposed COVID-RADS and common lexicon would improve the communication of findings to other healthcare providers, thus facilitating the diagnosis and management of COVID-19 patients.
Keywords: Coronavirus; Tomography, X-ray computed; Pneumonia, viral; Diagnosis; Pandemics; COVID-19
Introduction
Coronavirus disease 2019 (COVID-19) is the most recent global health emergency with more than 850,000 cases and 41,000 deaths reported in over 180 countries as of March 31, 2020 [1]. Early diagnosis of COVID-19 is crucial for patient isolation and prompt clinical interventions. Reverse transcription polymerase chain reaction (RT-PCR) is a highly specific test and the gold standard for the diagnosis of COVID-19. However, the variable sensitivity of RT-PCR and its lengthy turnaround time (24–48 h [2]) underscore the need for a complementary diagnostic approach [3–6]. Besides, multiple negative RT-PCR test results may be needed to rule out the disease in patients with a high clinical suspicion of COVID-19 [7].
Role of chest CT and its relationship with RT-PCR
Computed tomography (CT) imaging plays a key role in the diagnosis, management, and follow-up of COVID-19 patients. RT-PCR is the confirmatory test for the diagnosis of COVID-19 with high specificity. Numerous studies have endorsed the important role of CT in the management of these patients. However, several scientific societies have recommended against the routine use of CT for the screening of COVID-19 [8, 9]. Some countries have established the use of imaging as their frontline diagnostic test [2, 5, 7]. In the vast majority of the laboratory-confirmed patients, CT examinations yield a typical pattern and the sensitivity of this modality has been reported to be 97% in a study on 1014 patients [5]. The diagnostic value of this modality has been proven in clinically suspicious cases with inconclusive laboratory test results, as well as asymptomatic individuals with known exposure [3, 10]. In many healthcare settings, such as developing countries, CT imaging may be the only available diagnostic test due to a shortage of diagnostic laboratory kits, while validated COVID-19 laboratory test kits are limited in quantity even in industrialized nations [7, 11].
Need for a uniform lexicon and standardized reporting scheme
Structured reporting systems simplify the interpretation and reporting of imaging examinations, serve as a framework for consistent generation of recommendations, and improve the quality of patient care [12–16]. Our systematic review of the CT manifestations of COVID-19 showed a substantial inconsistency in description of imaging findings across the growing number of published studies [17]. We encountered the common use of several ambiguous and non-specific terms, such as fibrous stripes (or striped fibrosis), fibrotic streaks, lung fiber cord focus, vacuolar sign, bronchus distortion, patchy shadows, hazy opacities, patchy opacities, airspace disease, and interstitial disease [17–21]. While cardiothoracic radiologists may be familiar with some of these terms, the present variability in lexicon may be confusing for other radiology sub-specialties and referring healthcare providers. To ensure coherent and consistent communication between the healthcare providers, development of a standardized reporting format and lexicon is essential. It will also be vital for the ongoing clinical research, as well as an efficient organization of imaging data input for infectious disease registries.
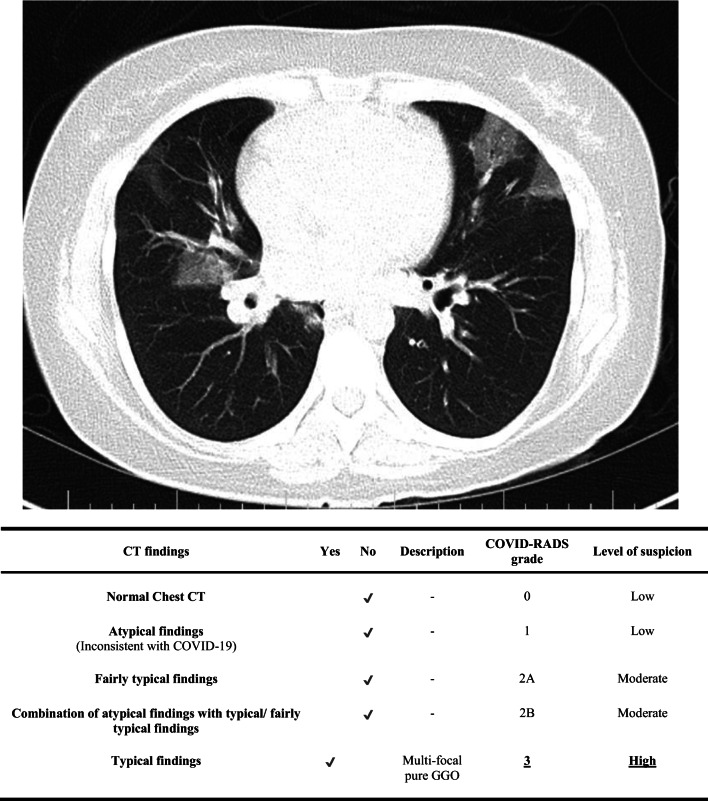
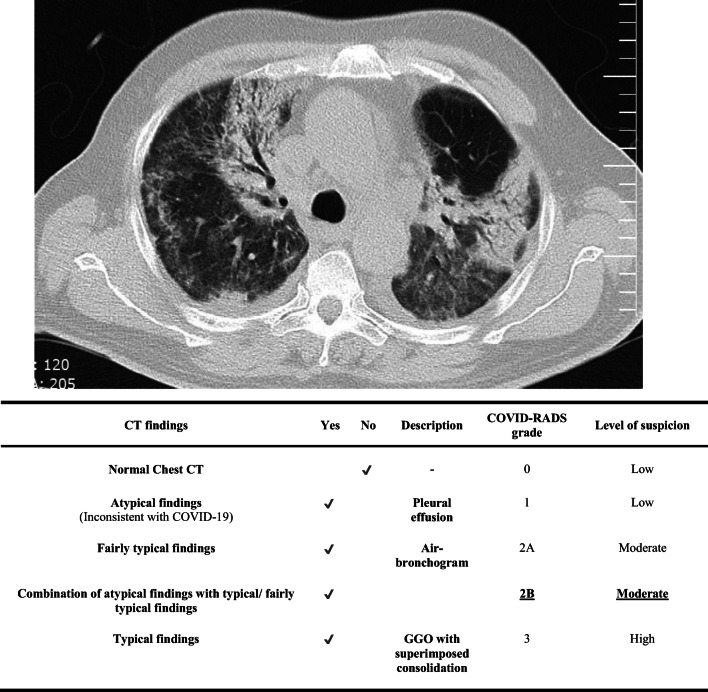
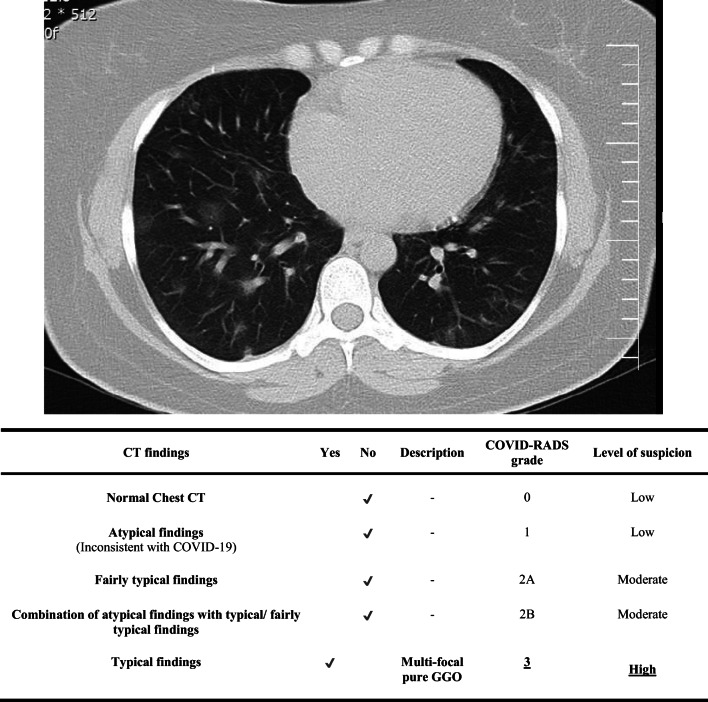
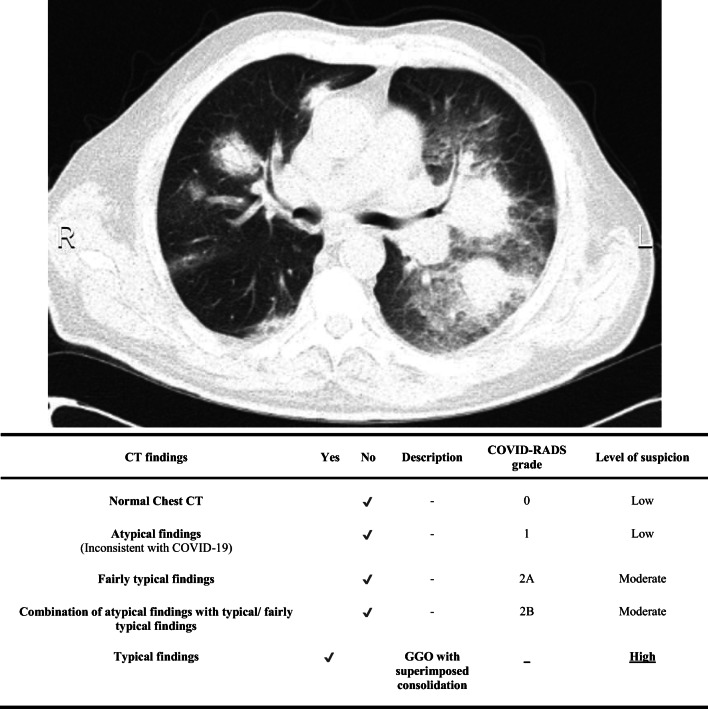
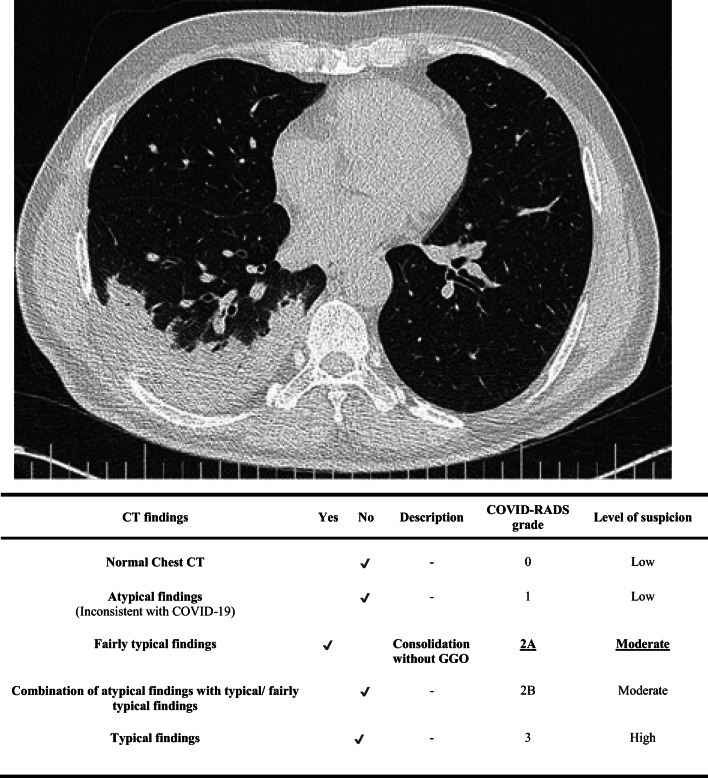
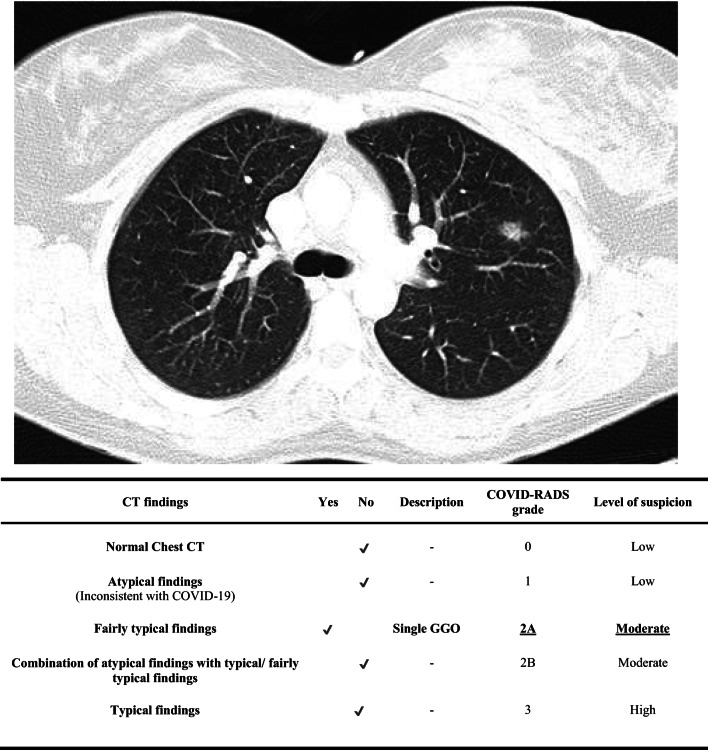
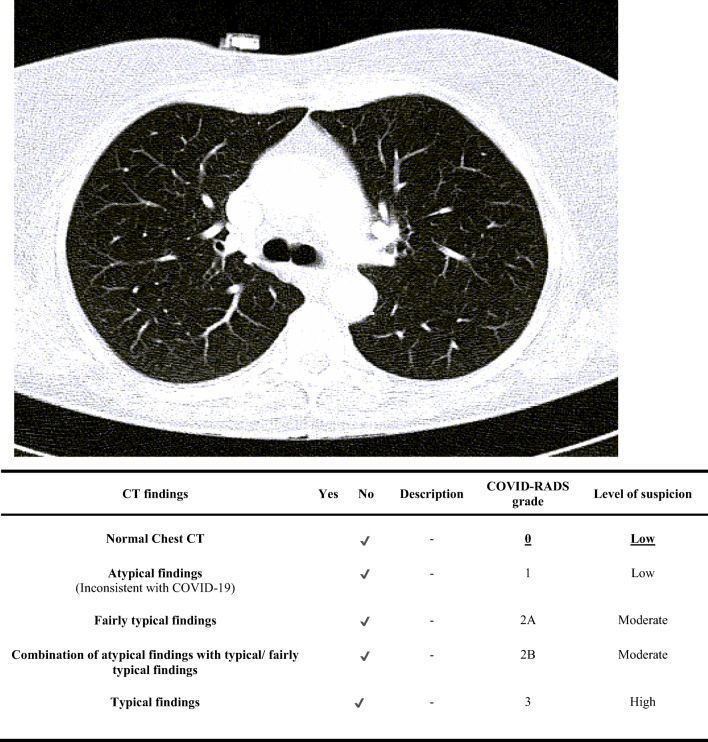
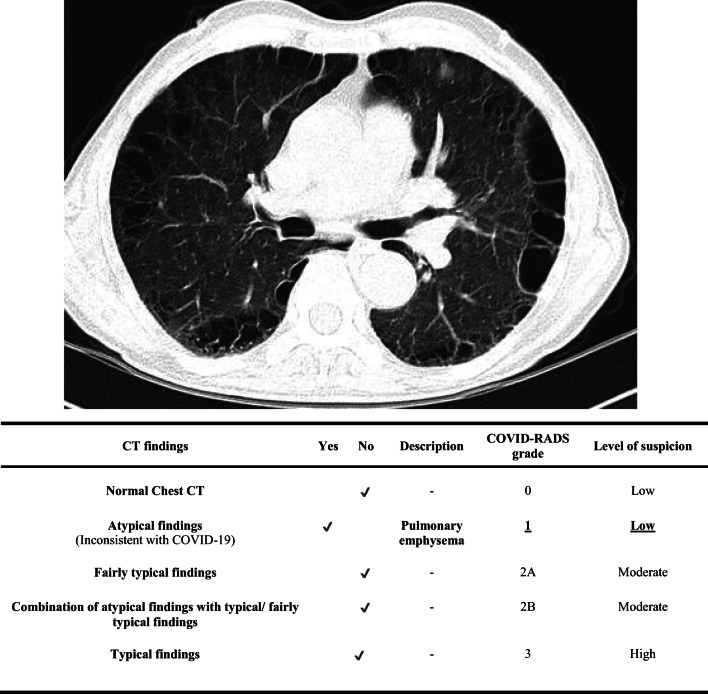
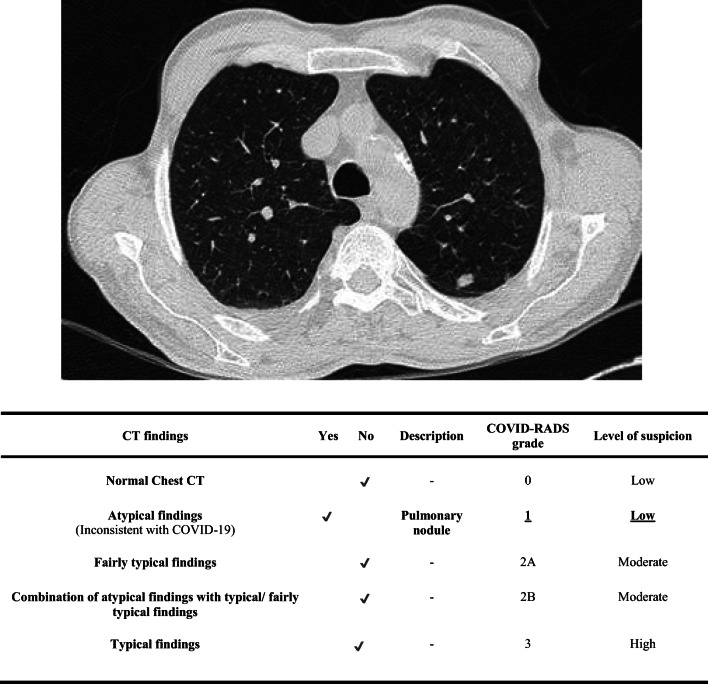
COVID-19 lexicon and imaging reporting and data system
We updated our published systematic review of chest CT manifestations of COVID-19, which was performed using a search of PubMed, Embase, Google Scholar, and the WHO database of COVID-19 literature on February 19, 2020, and included 30 studies [17]. For the purpose of the current proposal, seven studies that were published after our initial search were added, and a total of 37 studies pertaining to diagnostic features of COVID-19 in chest CT were included [5, 17, 19, 22–26]. Using the reported imaging findings of 3647 patients, we summarized the typical chest CT findings, atypical features, and temporal changes of COVID-19 in chest CT. A summary of the most common chest CT findings is reported in Table 1. Subsequently, we extracted a list of descriptive terms and mapped it to the terminology that is commonly used in imaging literature, including Fleischner Society’s Glossary of Terms for Thoracic Imaging [27]. Using this approach, we composed a comprehensive lexicon that includes the most pertinent terms and can be used for documentation and reporting of typical and atypical imaging findings in COVID-19 patients (Table 2). Using the same data, we propose the COVID-19 imaging reporting and data system (COVID-RADS), which is a grading system for CT findings with five categories (Table 3). Each COVID-RADS grade corresponds to a low, moderate, or high level of suspicion for pulmonary COVID-19 involvement. The levels of suspicion that we proposed here are based on the similarity between the findings of a given imaging exam and the typical CT manifestations of COVID-19 that are reported in the available literature. In other words, the proposed levels of suspicion are not based on the empirical data and the “true” suspicion levels are based on the clinical context and the level of pretest probability. The diagnosis should be made based on the whole clinical picture and confirmed based on the RT-PCR test results. Representative CT images along with corresponding COVID-RADS report cards are presented in Figs. 1, 2, 3, 4, 5, 6, 7, 8, and 9. Normal chest CT findings (COVID-RADS 0) or atypical features (COVID-RADS 1) are generally inconsistent with pulmonary manifestation of COVID-19. However, these features have been reported in a number of laboratory-confirmed symptomatic patients, hence indicating a low level of suspicion in our proposed grading system. Based on the current literature, the vast majority of the patients present with typical chest CT findings (COVID-RADS 3), which are commonly described as a peripheral, multifocal ground glass pattern. Typical findings are associated with the temporal stage of the disease but occasionally indicate the presence of complications. For instance, single ground glass opacity (GGO) is a fairly typical finding that may be present at the very early stages of the disease, while multifocal GGO, GGO with superimposed consolidation, and consolidation predominant pattern may be seen at progression/complicated stage. Linear opacities, crazy paving pattern, and white lung can be observed later in the course of progression/complicated stage. Imaging signs of remission, which may appear after the second week of the disease, include the melted sugar sign and parenchymal fibrotic bands [17, 18, 21, 28]. Some of the typical findings may be observed across different stages of the disease and interval changes in imaging studies should be taken into consideration for proper staging. Regardless, the typical findings denote a high level of suspicion for pulmonary involvement in COVID-19.
Table 1.
Summary of common pattern and distribution of pulmonary involvement on initial computed tomography images of coronavirus disease 2019 (COVID-19) from 37 studies
| CT finding* | Number of studies | Number of reported cases/total number of patients (%) |
|---|---|---|
| Bilateral involvement | 16 | 756/938 (80%) |
| Peripheral distribution | 16 | 467/624 (74.8%) |
| Posterior involvement | 1 | 41/51 (80%) |
| Multilobar involvement | 7 | 426/477 (89.3%) |
| Ground glass opacity | 25 | 649/749 (86.6%) |
| Consolidation | 14 | 133/403 (33%) |
| Vascular enlargement | 3 | 229/382 (60%) |
Table 2.
The proposed lexicon for description of chest CT imaging findings in coronavirus disease 2019 (COVID-19)
| Findings | Important definitions | |
|---|---|---|
| Distribution pattern of lesion |
Unilateral/bilateral Anterior/posterior Peripheral predominant/central predominant Focal/multifocal Round/linear/wedge-shaped/irregular opacity Right upper/right middle/right lower/left upper/left lower lobe One lobe/two lobes/three lobes/four lobes/five lobes involved |
The outermost one-third of the lung field is considered peripheral and the rest is considered central Posterior/anterior is determined according to the mid-axillary line |
| Type of lesion |
Pure GGO GGO with superimposed consolidation Reticulation Consolidation without GGO Predominant consolidation pattern Air bronchogram Crazy paving pattern White lung stage Melted sugar sign Parenchymal fibrotic bands Pleural effusion Cavity Pulmonary nodules Nodular pattern Lymphadenopathy Peribronchovascular distribution Bronchial wall thickening Halo sign Tree-in-bud pattern Bronchiectasis Airway secretions Interstitial emphysema Pulmonary fibrosis Pleural thickening Pneumothorax Pericardial effusion Vascular enlargement |
Pure GGO: A hazy intensification in lung attenuation without obscuration of the underlying vessels GGO with consolidation: A central opacification with obscuring the underlying vessels surrounded by GGO Melted sugar sign: Gradual decrease in density of consolidation and turning into GGO Halo sign: Pulmonary nodule surrounded by GGO, representative of hemorrhage Tree-in-bud pattern: Multiple sites of centrilobular nodules along with branching linear opacities [29] |
Table 3.
The proposed coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS)
| CT findings | Description | COVID-RADS grade | Level of suspicion |
|---|---|---|---|
| Normal Chest CT | 0 | Lowa | |
|
Atypical findings (Inconsistent with COVID-19) |
- Pleural effusion - Cavity - Pulmonary nodule(s) - Nodular pattern - Lymphadenopathy - Peribronchovascular distribution - Halo sign - Tree-in-bud sign - Bronchiectasis - Airway secretions - Pulmonary emphysema - Pulmonary fibrosis - Isolated pleural thickeningb - Pneumothorax - Pericardial effusion |
1 | Low |
| Fairly typical findings |
- Single GGO (early) - Consolidation without GGO (late/complicated)c - Focal pleural thickeningd - Vascular enlargemente - Air bronchogram - Bronchial wall thickening - White lung stage (late/complicated) - Parenchymal fibrotic bands (late/remission) |
2A | Moderate |
| Combination of atypical findings with typical/fairly typical findings | 2B | Moderate | |
| Typical findingsf |
- Multifocal GGO - GGO with superimposed consolidation - Consolidation predominant pattern (late/complicated) - Linear opacities (late/complicated) - Crazy paving pattern (late/complicated) - Melted sugar sign (late/remission) |
3 | High |
COVID-RADS, coronavirus disease imaging reporting and data system; GGO, ground glass opacity
aAlthough there is no imaging feature suggestive of COVID-19, it cannot exclude the disease
bFocal or diffused pleural thickening in the absence of GGO or consolidation
cThis finding is not highly suggestive of the COVID-19. However, in advanced stages, it may be the only present finding
dThickening of the pleura associated with the adjacent GGO or consolidation
eVascular enlargment refers to both luminal dilation and mural thickening of the pulmonary vessels [30]
fBilateral and peripheral lung involvement generally indicate a high level of suspicion for COVID-19
Fig. 1.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 3/high suspicion) for COVID-19 are underlined. GGO, ground glass opacity
Fig. 2.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion for COVID-19 are underlined (COVID-RADS 2B/moderate suspicion). GGO, ground glass opacity
Fig. 3.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion for COVID-19 are underlined (COVID-RADS 3/high suspicion). GGO, ground glass opacity
Fig. 4.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion for COVID-19 are underlined (COVID-RADS 3/high suspicion). GGO, ground glass opacity
Fig. 5.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 2A/moderate suspicion) for COVID-19 are underlined. GGO, ground glass opacity
Fig. 6.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 2A/moderate suspicion) for COVID-19 are underlined. GGO, ground glass opacity
Fig. 7.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 0/low suspicion) for COVID-19 are underlined
Fig. 8.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 1/low suspicion) for COVID-19 are underlined
Fig. 9.
An example report card for grading of the imaging based on the proposed classification. Corresponding COVID-RADS grade and the level of suspicion (COVID-RADS 1/low suspicion) for COVID-19 are underlined
Implications of COVID-RADS and lexicon
The COVID-19 outbreak is an illustrative case that emphasizes the importance of structured reporting in a scenario that requires large numbers of patients to be screened, diagnosed, and treated according to their CT imaging findings. Owing to the important burgeoning role of CT in the evaluation of COVID-19 patients, a comprehensive knowledge of imaging manifestations is crucial, and a uniform reporting format is needed to ensure effective communication between the healthcare providers.
During the current global state of emergency, some healthcare facilities around the world are experiencing historic high patient workflows. The implementation of COVID-RADS grading and lexicon would establish a structured reporting format that enables a consistent, rapid, and efficient communication between the diagnosticians and clinicians. The use of COVID-RADS will render exam reports brief yet concise and informative and in part enhance the quality of patient management and decrease the rate of missed diagnosis. The proposed structured reporting would facilitate the decision-making process, leading to timely patient isolation and prompt initiation of treatments.
Our proposed system is primarily applicable to the epidemic areas affected by the current pandemic, as well as the individuals with a high clinical suspicion for COVID-19 (high pretest probability). Our proposed lexicon is a concise list of terms required for description of chest CT findings in COVID-19, while routine CT examinations may require a more exhaustive lexicon with additional terms. Our proposed format is informed by an evidence-based systematic review of the available literature on COVID-19 and should be validated by empirical data.
It has to be emphasized that this is the first proposal for a RADS-system for COVID-19. The system is based on “interpretation” of numerous publications, but not on a very detailed statistical analysis of a huge database of COVID-19 cases. It may guide radiologists for now, but is not yet a validated system (as with other RADS). Clinicians should interpret COVID-RADS as just one part of the diagnostic puzzle and take into account the whole clinical picture. Furthermore, our understanding of the chest imaging features of COVID-19 is rapidly expanding and the current proposal is bound to the level of evidence of the studies that it is derived from, majority of which are case reports and small case series. While standardized reporting systems are intended to promote consistency, radiologists may need to adapt our proposed system based on their local or institutional policies and future guidelines. The Reporting and Data Systems (RADS) framework was developed by the American College of Radiology (ACR), aiming to standardize the radiology reports. Hence, validation and further modification of the proposed COVID-RADS grading system require the support of professional societies.
Conclusion
By introducing a standardized approach to reporting, the proposed COVID-RADS and common lexicon may improve the communication of findings to other healthcare providers, thus facilitating the diagnosis and management of COVID-19 patients.
Abbreviations
- ACR
American College of Radiology
- COVID-19
Coronavirus disease 2019
- COVID-RADS
Coronavirus disease 2019 imaging reporting and data system
- CT
Computed tomography
- GGO
Ground glass opacity
- RT-PCR
Reverse transcription polymerase chain reaction
Funding information
The authors state that this work has not received any funding.
Compliance with ethical standards
Guarantor
The scientific guarantor of this publication is Ali Gholamrezanezhad, MD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Not applicable.
This work is a proposal based on previous studies.
Ethical approval
Not applicable.
This work is a proposal based on previous studies.
Study subjects or cohorts overlap
Not applicable.
Methodology
• Evidence-based report
• Performed at one institution
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sana Salehi and Aidin Abedi contributed equally to this work.
References
- 1.Johns Hopkins Center for Systems Science and Engineering (2020) Coronavirus COVID-19 global cases. In: ArcGIS. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed 31 Mar 2020
- 2.Hare S, Rodrigues J, Nair A, Robinson G (2020) Lessons from the frontline of the covid-19 outbreak. In: BMJ Opin. https://blogs.bmj.com/bmj/2020/03/20/lessons-from-the-frontline-of-the-covid-19-outbreak/. Accessed 28 Mar 2020
- 3.Xie X, Zhong Z, Zhao W et al (2020) Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology 200343. 10.1148/radiol.2020200343 [DOI] [PMC free article] [PubMed]
- 4.Fang Y, Zhang H, Xie J et al (2020) Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 200432. 10.1148/radiol.2020200432 [DOI] [PMC free article] [PubMed]
- 5.Ai T, Yang Z, Hou H et al (2020) Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 200642. 10.1148/radiol.2020200642 [DOI] [PMC free article] [PubMed]
- 6.Huang P, Liu T, Huang L, et al. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology. 2020;295:22–23. doi: 10.1148/radiol.2020200330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanne JP, Little BP, Chung JH et al (2020) Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. Radiology 200527. 10.1148/radiol.2020200527 [DOI] [PMC free article] [PubMed]
- 8.American College of Radiology (ACR) (2020) ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed 31 Mar 2020
- 9.The American Society of Emergency Radiology (ASER) (2020) STR / ASER COVID-19 position statement. https://thoracicrad.org/wp-content/uploads/2020/03/STR-ASER-Position-Statement-1.pdf. Accessed 30 Mar 2020
- 10.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (2020) Coronavirus disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/about/testing.html. Accessed 2 Mar 2020
- 12.Assadi M, Velez E, Najafi MH, Gholamrezanezhad A. The need for standardization of nuclear cardiology reporting and data system (NCAD-RADS): learning from coronary artery disease (CAD), breast imaging (BI), liver imaging (LI), and prostate imaging (PI) RADS. J Nucl Cardiol. 2019;26:660–665. doi: 10.1007/s12350-018-01473-2. [DOI] [PubMed] [Google Scholar]
- 13.Gholamrezanezhad A, Kessler M, Hayeri SM. The need for standardization of musculoskeletal practice reporting: learning from ACR BI-RADS, liver imaging-reporting and data system, and prostate imaging-reporting and data system. J Am Coll Radiol. 2017;14:1585–1587. doi: 10.1016/j.jacr.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz LH, Panicek DM, Berk AR, et al. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260:174–181. doi: 10.1148/radiol.11101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abedi A, Tofighi S, Salehi S, et al. Reason for exam imaging reporting and data system (RI-RADS): a grading system to standardize radiology requisitions. Eur J Radiol. 2019;120:108661. doi: 10.1016/j.ejrad.2019.108661. [DOI] [PubMed] [Google Scholar]
- 16.Tofighi S, Abedi A, Salehi S et al (2020) Reason for exam imaging reporting and data system: consensus reached on quality assessment of radiology requisitions. J Patient Saf. 10.1097/PTS.0000000000000653 [DOI] [PubMed]
- 17.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A (2020) Coronavirus disease 2019 (COVID-19, 2019-nCoV): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol:1–7. 10.2214/AJR.20.23034 [DOI] [PubMed]
- 18.Pan Y, Guan H, Zhou S et al (2020) Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 10.1007/s00330-020-06731-x [DOI] [PMC free article] [PubMed]
- 19.Zhou S, Wang Y, Zhu T, Xia L (2020) CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. AJR Am J Roentgenol:1–8. 10.2214/AJR.20.22975 [DOI] [PubMed]
- 20.Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed]
- 21.Pan Y, Guan H (2020) Imaging changes in patients with 2019-nCov. Eur Radiol. 10.1007/s00330-020-06713-z [DOI] [PMC free article] [PubMed]
- 22.Bernheim A, Mei X, Huang M et al (2020) Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology 200463. 10.1148/radiol.2020200463 [DOI] [PMC free article] [PubMed]
- 23.Guan W-J, Ni Z-Y, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed]
- 24.Inui S, Fujikawa A, Jitsu M, et al. Chest CT findings in cases from the cruise ship “diamond princess” with coronavirus disease 2019 (COVID-19) Radiology Cardiothoracic Imaging. 2020;2:e200110. doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bai HX, Hsieh B, Xiong Z et al (2020) Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology 200823. 10.1148/radiol.2020200823 [DOI] [PMC free article] [PubMed]
- 26.Zhao W, Zhong Z, Xie X et al (2020) Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol :1–6. 10.2214/AJR.20.22976 [DOI] [PubMed]
- 27.Hansell DM, Bankier AA, MacMahon H, et al. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 28.Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A (2020) Coronavirus (COVID-19) outbreak: what the Department of Radiology should know. J Am Coll Radiol. 10.1016/j.jacr.2020.02.008 [DOI] [PMC free article] [PubMed]
- 29.Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G (2005) Tree-in-Bud Pattern at Thin-Section CT of the Lungs: Radiologic-Pathologic Overview. Radiographics 25 (3):789–801. 10.1148/rg.253045115 [DOI] [PubMed]
- 30.Salehi S, Abedi A, Gholamrezanezhad A (2020) Reply to vascular changes detected with thoracic CT in Coronavirus Disease (COVID-19) might be significant determinants for accurate diagnosis and optimal patient management. AJR Am J Roentgenol. 10.2214/AJR.20.23339 [DOI] [PubMed]