Abstract
Background
Type 2 diabetes (T2D) is a worldwide epidemic and a leading cause of death in Mexico, with a prevalence of 15.9%, and >70% of diagnosed adults have poor glycemic control [glycated hemoglobin (HbA1c) >7.5%]. We developed a diabetes self-management education program contextualized to the study population, including dietary preferences, health literacy, and health system.
Objectives
We aimed to evaluate the efficacy of a self-management + text message program (¡Sí, Yo Puedo Vivir Sano con Diabetes!) on primary (HbA1c), and secondary behavioral (self-management), clinical, and psychosocial outcomes in adults with T2D in Mexico City.
Methods
Participants were recruited at public primary healthcare centers (Seguro Popular), and randomly allocated to treatment (n = 26) or wait-list control groups (n = 21) with data collected at 3 and 6 mo. The program included 7 weekly sessions and 6 mo of daily text/picture messages. Descriptive statistics and a generalized linear mixed model with intent-to-treat analysis were calculated.
Results
Participants were 55.5 ± 8.8 y of age (mean ± SD), 68% female, 88.6% overweight/obese, and 57% lived in food-insecure households. Mean ± SD T2D duration was 11.9 ± 7.8 y and HbA1c was 9.2% ± 1.5%. There was 89% attendance at sessions and 6.4% attrition across both groups at 6 mo. Group-by-time effects were seen in self-monitoring of blood glucose (P < 0.01) and diabetes self-efficacy (P < 0.04); and a trend for lower HbA1c was seen in the intervention group at 6 mo (P = 0.11). Significant improvements in dietary behavior (P < 0.01) were demonstrated in the intervention group over time, but this did not reach statistical significance compared with the control group.
Conclusions
The program was associated with clinically significant improvements in T2D self-management, self-efficacy, and HbA1c over time. Thus, T2D self-management skills, including diet, were improved in a vulnerable metropolitan population.
This trial was registered at clinicaltrials.gov as NCT03159299.
Keywords: type 2 diabetes, mHealth, text message, Mexico, health disparities, self-management, low income
Evaluation of a group-based self-management + text message program for adults with type 2 diabetes on clinical (glycated hemoglobin), self-management, and psychosocial outcomes at 6 mo in Mexico City.
Introduction
The prevalence of diabetes is increasing worldwide, indicating a serious public health problem. The prevalence of diabetes in adults in Mexico is 15.8%, one of the highest in the world. This compares with 4.7% in the United Kingdom, 7.4% in Canada, 10.4% in Brazil, and 10.8% in the United States. Although these statistics include adults with type 1 diabetes and type 2 diabetes (T2D), the prevalence of type 1 diabetes is only 0.4%–1.4% in these countries (1). Globally, T2D is a major contributing factor to morbidity, mortality, and lower quality of life in adults with T2D, and has significant financial costs (2–4). In Mexico City, T2D is a leading cause of mortality and a high financial burden to the health care system (3, 4).
Meeting glycemic targets of glycated hemoglobin (HbA1c) <7.5% has been shown to decrease morbidity and mortality in adults with T2D (5). Despite improvements in access to T2D care in Mexico, the majority of adults with T2D do not meet glycemic targets (i.e., HbA1c <7.5%) (4, 6). Diabetes self-management is critical to improving HbA1c and health outcomes, yet it is complex, requiring healthy eating, physical activity, correctly taking medications, self-monitoring of blood glucose (SMBG), and quarterly health care appointments in the context of frequent problem-solving.
Diabetes self-management education (DSME) is a standard of care in many countries, providing education, skill development, and behavioral support for managing T2D (7). Considerable evidence supports the benefit of DSME on clinical, behavioral, and psychosocial outcomes globally (7, 8). However, diabetes self-management in Mexico is suboptimal. In 1 study, 12% of adults with T2D were not performing any self-management (blood glucose monitoring, dietary modifications, or physical activity), 60% were performing 1 or 2 behaviors, and only 28% were performing all behaviors (9). Limited understanding of the importance of self-management and low health literacy are contributing factors to poor self-management and glycemic control in Mexico (10).
There have been efforts to implement DSME in Mexico, such as “Mutual Help Groups” (GAM—acronym in Spanish), which were established in 2001. According to Mexico's Health Department, in 2012 there were 7059 GAM groups with 172,595 beneficiaries, yet only 30% of these groups were certified according to Health Department standards (11). Thus, the provision of DSME in Mexico City is insufficient, and there is need for evidence-based interventions. In addition, owing to the obesogeneity of the built environment in the country and food insecurity challenges (12), it is critical to design DSME interventions with a strong nutrition education component (13).
Critical to the success of DSME programs is the need to target the program to the local sociocultural context, dietary preferences, and health care system. Therefore, based on a systematic community participatory approach, that included extensive formative research and collaboration with stakeholders, we developed a DSME program for adults with T2D in Seguro Popular primary health care clinics (10, 14). These clinics are part of the Sistema de Protección Social en Salud which provides public health insurance to those without social security health coverage. Services for T2D care at Seguro Popular clinics include medical visits, referrals to specialists and nutritionists when needed, laboratory testing, and free medicines (11).
The purpose of this study was to evaluate the effect of our ¡Sí, Yo Puedo Vivir Sano con Diabetes! DSME program (¡Sí, Yo Puedo!), which included group sessions supplemented with daily text/picture messages, on our primary outcome of HbA1c and secondary clinical [BMI and blood pressure (BP)], T2D self-management (including aspects of diet and nutrition), and psychosocial outcomes (depressive symptoms, self-efficacy) at 6 mo compared with a wait-list control group. Our hypothesis was that the intervention group would demonstrate improvements in primary and secondary outcomes compared with the control group. We also hypothesized that the program would be feasible for adults with T2D at Seguro Popular clinics.
Methods
This study (NCT03159299) was a randomized wait-list control pilot study, approved by the Institutional Review Boards at Yale University and the Center for Welfare Analysis and Measurement (CAMBS—acronym in Spanish, a civil association and research center, member of the National Registry of Scientific and Technological Institutions and Companies) in Mexico City. The research was conducted in accordance with the approved protocol. Inclusion criteria were age 21–70 y, medically stable and able to exercise, diagnosed with T2D for ≥1 y with HbA1c >7.5%, receiving health care at a Seguro Popular clinic, and with access to a cell phone. Exclusion criteria included cognitive impairment, major cardiac event in the past 12 mo, uncontrolled blood pressure, renal failure, and severe peripheral neuropathy. Participants in the wait-list control group were invited to participate in the program after completion of the 6-mo data collection. Our sample size goal was 40 participants (n = 20/group). In a simulation study, 15–20 participants/group demonstrated reasonable bias-corrected estimations for a medium to large (Cohen's) effect size on the primary outcome of HbA1c (15).
The study was conducted in 5 Seguro Popular clinics in Mexico City. A coordinating official of Mexico City's Health Department recommended these clinics for the project because they had a sufficient number of adults with T2D with varying metabolic control, and these clinics lacked a certified diabetes program (GAM). Permission was obtained from clinic directors to conduct research at each clinic.
Flyers were distributed in the clinic settings and eligible adults with T2D were provided information about the study by a trained research assistant (RA). If interested, the study was explained and a screening questionnaire was completed. If eligible, an appointment was scheduled for informed consent, baseline data collection, and study enrollment. Informed consents and items on questionnaires were read to participants if needed, to ensure understanding. All study subjects signed the informed consent before study enrollment and data collection. According to the institutional review board–approved protocol, no harms, unintended effects, or serious adverse effects directly linked to the program occurred during the study follow-up time period.
Study data were collected and managed using REDCap electronic data capture tools (16, 17). RAs entered data at the time of data collection into the database via tablets. Upon completion of baseline data collection, eligible participants were randomly allocated to 1 of the 2 treatment conditions in a 1:1 allocation ratio using a computer-generated, block randomization procedure. At the end of the baseline data collection, an RA not involved in data collection told each participant their group assignment. Data collectors were blinded to treatment group assignment. All participants received a gift card for a department store after data collection; each participant received $200 Mexican pesos (∼$10 USD) at baseline, $300 Mexican pesos (∼$15 USD) at 3 mo, and $400 Mexican pesos (∼$20 USD) at 6 mo.
All participants received standard T2D care at the Seguro Popular clinic as aforementioned. Participants allocated to the treatment group also received the ¡Sí, Yo Puedo! program which was developed after formative research with adults with T2D in Mexico and health care providers of the Seguro Popular clinics (10, 14). We incorporated relevant theoretical underpinnings, educational content, and interactive strategies of 4 evidence-based programs for Hispanic adults with T2D to meet the needs of adults with T2D with limited resources, expertise of providers, and the systems of care of the Seguro Popular clinics in Mexico City. A description of the theoretical foundation for this intervention has been previously published (14). The ¡Sí, Yo Puedo! program was delivered by a registered nurse and social worker, who were provided 1 wk of interactive training and supportive supervision throughout the study. The group session leaders were closely supervised by the study leadership team who had extensive public health, nutrition, and T2D self-management expertise.
The program included 7 interactive group-based educational sessions on diabetes self-management that were culturally relevant and appropriate for adults with low health literacy (Table 1). Although the overall aim of the intervention was to strengthen diabetes self-management strategies through a multifaceted approach, the nutrition component was central in the delivery of the intervention. This component was designed to progressively increase the knowledge and abilities of participants to improve their metabolic control through healthier eating. Nutrition education was based on “the smart plate”: a plate method with modifications for T2D (18–21). Activities around the plate method allowed participants to identify foods and beverages high in carbohydrates (both simple and complex), and to build knowledge around how to combine them with other foods for balanced meals. At the same time, activities highlighted carbohydrate portions (through the fist and hand-palm method) and distribution throughout the day (22, 23). These activities were tailored to the socioeconomic and cultural context of participants.
TABLE 1.
Educational content of the ¡Sí, Yo Puedo Vivir Sano Con Diabetes! self-management program for low-income adults with T2D, Mexico City, 2018–20191
| Session number | Concepts/topics |
|---|---|
| Orientation | - Introduction to the program, expectations of participants, and class introductions |
| Session 1 | - Understanding diabetes and need for blood glucose monitoring, healthy eating, physical activity, and taking medication |
| - Common cultural misconceptions | |
| - Stress management activity | |
| Session 2 | - Self-monitoring blood glucose and relation to food and activity |
| - Stress management activity | |
| Session 3 | - Relation between carbohydrate intake and blood glucose levels |
| - The plate method for T2D | |
| - Food portion measurement | |
| - Menu planning with limited resources | |
| - Stress management activity | |
| Session 4 | - Physical activity (benefits, precautions) |
| - Stress management activity | |
| Session 5 | - Diabetes medicines and talking to health care professionals |
| - Reading food and drink nutrition labels | |
| Session 6 | - Preventing diabetes complications and taking control of diabetes |
1T2D, type 2 diabetes.
Once nutrition knowledge and abilities were established, the intervention moved on to reading food package labels. This was key, because in Mexico 29.8% of daily energy consumption is linked to ultra-processed food and 6% to other types of processed foods (24, 25). Therefore, participants were taught how to estimate portions of processed foods, to count carbohydrates, and to identify added sugars with different names. Intervention participants were provided glucometers, test strips, and lancets (Accu-Check Performa® glucometer, test strips, and lancets; Roche), with the main objective to incorporate SMBG as a key T2D self-management strategy. A secondary objective of the provision of glucometers was for participants to clearly understand how healthier diets are linked to better blood glucose values. Additional education sessions included content on stress management, physical activity, medication adherence, and prevention of complications.
Behavioral support was provided in all sessions by class leaders to assist in problem-solving barriers to change and to develop weekly goals (including follow-up phone calls every 2 wk). Empowerment-based strategies were used to promote motivation and self-efficacy. Lastly, daily text/picture messages, based on the Health Action Process Approach model (26), were sent daily for 6 mo to reinforce class content and promote participants’ intention and maintenance of behavior change. Pictures were used in text messages to enhance understanding and a positive outlook in the face of diabetes. Based on our formative research we provided text/picture message cards printed on paper secured with a binder ring in case participants could not access them via the cell phone. Classes were scheduled at the same time and day of the week, were hosted at the clinic in which patients were enrolled, and phone reminders were sent the day before each class.
Data collection and measures
Data were collected at baseline, 3 mo, and 6 mo on primary and secondary outcomes. Demographic and clinical data (age, gender, education, known diabetes duration), including food security, were collected at baseline. Household food security was measured using the Latin American and Caribbean Food Security Scale modified for use in urban older adults. This validated questionnaire contains 8 items that assess if a household has not been able to access food of adequate quality in the last 3 mo (27). Feasibility data were collected throughout study implementation.
Primary outcome
HbA1c, a gold-standard measure of glycemic control (28), was our primary outcome. HbA1c was measured using a fingerstick of blood and analyzed in situ with the A1CNow+ system (PTS Diagnostics). This point-of-care assessment of HbA1c has been validated with clinical laboratory measurement of HbA1c (29).
Secondary outcomes
Additional outcomes included clinical (BMI, BP), behavioral (T2D self-management), and psychosocial (depressive symptoms and self-efficacy) measures. BMI was calculated in kg/m2 with WHO cutoffs used to create BMI categories: ≥18.5 normal weight, ≥25 overweight, and ≥30 obesity. Body weight was measured without shoes and with minimum clothing using an electronic scale (SECA 872) registered in grams. Height was measured without shoes with a portable stadiometer (SECA model 214) registered in centimeters. Measurements for both weight and height were taken twice and averaged. Systolic and diastolic BP were measured following standard procedures using an aneroid sphygmomanometer. Two readings separated by 1 min were averaged. Results from clinical measurements were provided to participants privately. Self-management was measured by the Summary of Diabetes Self-Care Activities questionnaire (SDSCA), a multidimensional 12-item scale with items on diet (follow a healthy eating plan, fruit-vegetable and high-fat foods consumption, spacing carbohydrates through the day), SMBG, foot care, and smoking. Subscales range from 0–7 (number of days in the last 7 d each behavior was completed), with a higher score reflecting better self-management (30, 31). Physical activity was measured with the Global Physical Activity Questionnaire (32), a 16-item questionnaire that assesses physical activity (intensity, duration, and frequency) at work, during transportation and leisure time, as well as sedentary behavior (33). Depressive symptoms were measured by the Patient Health Questionnaire-8 (PHQ-8), which consists of 8 items related to the diagnostic criteria for depressive disorder. The scale range is from 0–34, with higher scores reflecting a higher number of depressive symptoms (34). Participants who scored above the cutoff for moderate depressive symptoms (≥10) were informed of their result, provided information on a mental health hotline, and recommended to make an appointment with the clinic psychologist as soon as possible. Self-efficacy was measured by the Stanford Self-Efficacy Scale, an 8-item scale that includes items on confidence in performing exercise, interpreting blood glucose concentrations, and following dietary recommendations. The scale range is from 1–10, with higher scores indicative of greater self-efficacy (35). All questionnaires have established reliability and validity in Spanish-speaking adults (31, 36–38).
Feasibility outcomes
Feasibility data included rates of recruitment, reasons for refusal, protocol implementation fidelity, attendance, and attrition. Our goal was >80% attendance across all sessions/participants and <20% attrition at 6 mo. Protocol implementation was evaluated with a 5-item fidelity checklist completed by the group session leaders. In addition, ∼35% of sessions were observed by a trained RA to also ensure protocol fidelity.
Data analysis
Sample characteristics were described using frequency distributions and summary statistics. In addition, the groups were compared to make certain that randomization procedures were adequate. To test the hypothesis that adults with T2D who received the ¡Sí, Yo Puedo! program demonstrated better outcomes than those in the control condition, a generalized linear mixed model (GLMM) with an intent-to-treat analysis was used. Before running our analyses, we examined the homogeneity of variances at baseline across the 5 clinics (39). The GLMM incorporated within-subject correlations and included the random effect of clinics when the homogeneity of variances was rejected. The correlation structure was selected using goodness-of-fit criteria such as Akaike's Information Criterion and the Bayesian Information Criterion, and residuals were assessed for normality assumptions. For repeatedly measured binary outcomes, the GLMM (also called mixed effect logistic) included a link function of logit and incorporated correlations within-subjects. In this analysis, the OR was calculated based on the estimated coefficient of time, with an OR >1 representing increased likelihood of having vigorous/moderate physical activity or moderate depressive symptoms (PHQ-8 ≥10) over 6 mo from baseline.
Because it was likely that significant main effects might not be found for all variables owing to the sample size, identification of marginally significant trends (e.g., P < 0.15) was considered. SAS software version 9.4 was used to conduct the analyses (SAS Institute Inc.). To evaluate feasibility and fidelity, a summary of the protocol implementation fidelity checklists, attendance, and attrition were calculated.
Results
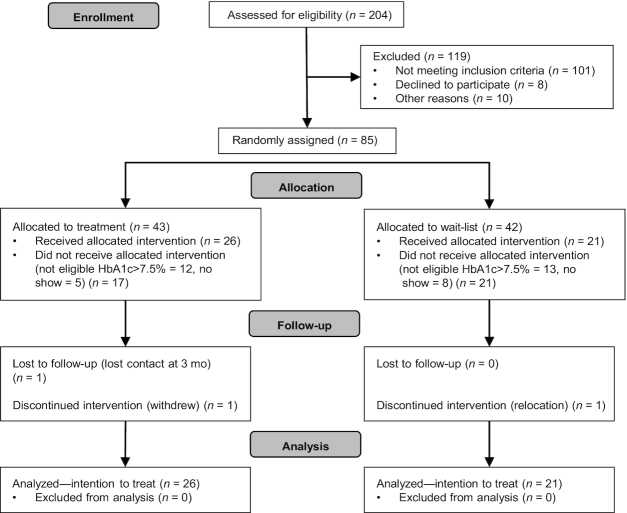
Recruitment and data collection took place from January to December 2018. A total of 204 participants expressed interest in the study. Of those, 103 were eligible and 85 were scheduled for informed consent and baseline data collection. Of those who participated in baseline data collection, 65% were eligible and enrolled in the study (Figure 1). The sample (n = 47) had a mean (± SD) age of 55.35 (± 8.75) y, 68% were female, 51% had been employed within the past week, and 57% had moderate to severe food insecurity. Mean (± SD) duration of diabetes since diagnosis was 11.85 (± 7.25) y and HbA1c was 9.20% (± 1.50%); 87% were overweight or obese and 38% had elevated depressive symptoms. No differences between the intervention (n = 26) and the control group (n = 21) were found at baseline in terms of descriptive characteristics (Table 2). Attendance was high at 89% across all sessions and attrition was low at 6.4% (n = 3) at 6 mo. The majority of participants received the text (96% at 3 mo; 100% at 6 mo) and picture messages (83% at 3 mo; 88% at 6 mo). Adherence to protocol implementation was high, with goals and objectives completely fulfilled in 91% of the sessions and mostly achieved in 7% of sessions.
FIGURE 1.
CONSORT flow diagram. Phases of a randomized controlled pilot study for diabetes self-management in low-income adults with an intervention group and a wait-list (control group) in a primary care setting in Mexico City, 2018–2019. HbA1c, glycated hemoglobin.
TABLE 2.
Baseline characteristics between intervention and control groups, ¡Sí, Yo Puedo Vivir Sano Con Diabetes! self-management program for low-income adults with T2D, Mexico City, 2018–20191
| Characteristic | Intervention (n = 26) | Control (n = 21) | Difference (P value) |
|---|---|---|---|
| Demographic characteristics | |||
| Age, y | 53.9 ± 9.2 | 56.8 ± 8.3 | 0.272 |
| Sex, F | 17 (65.4) | 14 (70.0) | 0.743 |
| Working status (worked in past week) | 14 (53.8) | 10 (47.6) | 0.673 |
| Married/partnered | 15 (57.7) | 13 (61.9) | 0.773 |
| Clinical characteristics | |||
| Duration of T2D, y | 10.2 ± 7.2 | 13.5 ± 7.3 | 0.122 |
| HbA1c, % | 9.3 ± 1.4 | 9.1 ± 1.6 | 0.612 |
| HbA1c >7.5% | 25 (96.1) | 20 (95.2) | 0.883 |
| BMI, kg/m2 | 31.0 ± 6.1 | 29.5 ± 5.0 | 0.372 |
| Overweight | 10 (38.5) | 10 (47.6) | 0.474 |
| Obese | 13 (50.0) | 8 (38.1) | |
| Overweight/obese | 23 (88.5) | 18 (85.7) | 0.783 |
| Depressive symptoms (PHQ-8) | 7.5 ± 5.0 | 10.2 ± 6.6 | 0.132 |
| Moderate depressive symptoms (PHQ-8 ≥10) | 10 (38.5) | 8 (38.1) | 0.873 |
| BP systolic, mm Hg | 126.0 ± 14.5 | 126.6 ± 14.3 | 0.902 |
| BP diastolic, mm Hg | 79.7 ± 10.9 | 79.9 ± 11.2 | 0.982 |
| ELCSA (household food insecurity) | |||
| Mild | 11 (42.3) | 9 (42.9) | 0.264 |
| Moderate | 9 (34.6) | 6 (28.6) | |
| Severe | 4 (15.4) | 6 (28.6) | |
1 n = 47. Values are means ± SDs or n (%) unless otherwise indicated. BP, blood pressure; ELCSA, Latin American and Caribbean Food Security Scale; HbA1c, glycated hemoglobin; PHQ-8, Patient Health Questionnaire-8; T2D, type 2 diabetes.
2Difference in the baseline characteristics between the 2 intervention groups examined by independent t test.
3Difference in the baseline characteristics between the 2 intervention groups examined by chi-square test.
4Difference in the baseline characteristics between the 2 intervention groups examined by Cochran–Armitage trend test.
Group-by-time effects were seen in SMBG (P < 0.001) and diabetes self-efficacy (P = 0.04); and there was a trend for lower HbA1c in the intervention group at 6 mo (−1.77% in treatment group compared with −0.96% in control group, P = 0.11). Time effects for the intervention group included improved diabetes self-care behavior (diet, exercise, SMBG), diabetes self-efficacy, depressive symptoms, and HbA1c at 6 mo. Time effects for the control group included improved HbA1c, exercise, SMBG, and depressive symptoms (see Table 3).
TABLE 3.
Longitudinal changes of outcomes between intervention and control groups over 6 mo for intent-to-treat analysis in the ¡Sí, Yo Puedo Vivir Sano Con Diabetes! self-management program for low-income adults with type 2 diabetes, Mexico City, 2018–20191
| Estimated change for 6 mo ± SE or OR [95% CI] (P value)2 | Difference of changes between intervention and control (P value)3 | ||
|---|---|---|---|
| Outcome | Intervention | Control | |
| Primary outcome | |||
| HbA1c, % | −1.77 ± 0.34 (<0.01) | −0.96 ± 0.37 (0.01) | 0.11 |
| Clinical outcome | |||
| BMI, kg/m2 (log-transformed) | 0.011 ± 0.009 (0.22) | 0.002 ± 0.009 (0.84) | 0.49 |
| Diastolic BP, mm Hg | 2.12 ± 2.71 (0.44) | 3.57 ± 2.93 (0.23) | 0.72 |
| Systolic BP, mm Hg | −1.23 ± 3.14 (0.70) | −3.09 ± 3.38 (0.36) | 0.69 |
| Behavioral outcomes | |||
| Self-care (SDSCA) subscales | |||
| General diet | 1.50 ± 0.55 (<0.01) | 0.54 ± 0.60 (0.37) | 0.24 |
| Exercise | 1.00 ± 0.58 (0.09) | 1.56 ± 0.63 (0.02) | 0.51 |
| SMBG | 4.97 ± 0.39 (<0.01) | 0.86 ± 0.43 (0.05) | <0.01 |
| Global physical activity (GPAQ) | |||
| Vigorous/moderate physical activity for work (yes vs. no) | OR: 1.42 [0.38, 5.30] (0.5989) | OR: 0.45 [0.11, 1.77] (0.2483) | 0.23 |
| Vigorous/moderate physical activity for recreation (yes vs. no) | OR: 1.27 [0.38, 4.26] (0.6985) | OR: 1.75 [0.46, 6.71] (0.4090) | 0.72 |
| Psychosocial outcomes | |||
| Depressive symptoms (PHQ-8) | −2.43 ± 1.21 (0.0476) | −3.02 ± 1.33 (0.0258) | 0.74 |
| Moderate depressive symptoms (PHQ-8 ≥10) | OR: 0.17 [0.04, 0.85] (0.0307) | OR: 0.53 [0.14, 2.07] (0.3601) | 0.28 |
| Diabetes self-efficacy | 1.24 ± 0.31 (<0.001) | 0.29 ± 0.34 (0.4030) | 0.04 |
1 n = 47. The estimates and P values were obtained from a generalized linear mixed model with a random effect of clinic (if necessary) and a specific covariance structure within-subject. BP, blood pressure; GPAQ, Global Physical Activity Questionnaire; HbA1c, glycated hemoglobin; PHQ-8, Patient Health Questionnaire-8; SDSCA, Summary of Diabetes Self-Care Activities questionnaire; SMBG, self-monitoring of blood glucose.
2Testing significant change in each group.
3Testing significant difference of changes between the 2 groups.
Discussion
Through this pilot study, we have demonstrated the potential of the ¡Sí, Yo Puedo! program for adults with T2D living with limited resources in Mexico City and enrolled in Seguro Popular. There was a significant improvement in SMBG and diabetes self-efficacy and a trend for improved HbA1c in the treatment group compared with the control group at 6 mo. Participants in the treatment group demonstrated a clinically significant decrease in HbA1c over time (−1.76% in the treatment group and −0.97% in the control group at 6 mo), supporting the critical importance of DSME in improving outcomes in a vulnerable population. Participants in the control group also improved HbA1c, SMBG, and physical activity over time. HbA1c improvement has been demonstrated in other T2D self-management clinical trials with Hispanic adults (40, 41), possibly due to systemic changes in care delivery in the clinic during the study, participants becoming more motivated in diabetes self-management owing to monitoring by the research team, and participant expectations of receiving the program after 6 mo. Alternatively, improvements in depressive symptoms in both groups may have also helped improve HbA1c through enhanced self-management (42). We would like to emphasize that the focus on healthy eating and nutrition in the program can also be reflected in 2 additional outcomes: a significant group-by-time effect in diabetes self-efficacy (which includes confidence in following dietary recommendations) and a significant time effect for better eating habits (general diet subscale of SDSCA), although the latter didn't reach statistical significance in the group-by-time analysis owing to sample size limitations.
The reported outcomes are particularly relevant when considering 2 baseline unfavorable nutrition-related indicators of the sample: a prevalence of overweight and obesity of 87% and the fact that 57% of the participants reported moderate to severe food insecurity. This highlights that well-designed and contextualized, culturally appropriate DSME plus text messaging programs can have positive outcomes even among highly vulnerable populations.
Increasing access to quality DSME programs is needed worldwide, particularly in countries like Mexico where access and delivery of DSME programs are inconsistent, with varying standards and quality (7). DSME that includes empowerment-based strategies may be particularly relevant to adults with T2D with low health literacy who may believe that they have limited control in improving their health trajectory. Empowerment-based DSME programs have demonstrated a positive effect on glycemic control in Latino adults living in the United States (41, 43). In our study, a significant improvement in diabetes self-efficacy was demonstrated in treatment group participants, which may have been a mediating factor to improved HbA1c.
Another factor that may have contributed to improved outcomes in the treatment group was improvement in SMBG. Although SMBG may not be required daily for all adults with T2D, it is recommended when adults with T2D are learning about diabetes self-management to better understand the effect of diet, exercise, medications, and stress on blood glucose concentrations (44). Teaching SMBG skills as well as how to interpret and problem-solve results is necessary to help adults with T2D, especially those with low health literacy, to make sound self-management decisions, particularly with dietary choices (26). Participants were provided SMBG supplies as part of the intervention, because coverage for SMBG supplies is critically important for those with limited resources and may be a cost-effective strategy to incorporate into future health policy initiatives. Access to SMBG supplies is limited for adults of low socioeconomic status in Mexico City (45).
High engagement with the ¡Sí, Yo Puedo! program may also have contributed to improved outcomes in this study. Elements of the intervention such as tailoring content to the local context, reinforcing content and motivation through text messages, group sessions, and follow-up phone calls from the class leaders may have contributed to the high attendance and low attrition. Attendance in group-based sessions has been shown to be an important moderator of program effectiveness (40). In addition, using evidence-based programs, adapting programs to the needs of participants and providers, providing programs in local health care settings, and aligning the program with the health care delivery system are important strategies to enhance engagement, implementation, and sustainability of programs.
The use of picture/text messages aligned with a theoretical model of behavior change was an innovative component of the ¡Sí, Yo Puedo! program. Evidence supports the use of text messages as a supplement to clinical care in improving adherence and HbA1c in adults with T2D (46). Although further research is indicated, providing theory-based behavioral support and positivity through picture/text messages may be an important strategy that enhances the effectiveness of clinical care in T2D.
In this pilot study, significant improvements in healthy eating, physical activity, depressive symptoms, BMI, and BP between groups were not demonstrated. Although there were time effects for healthy eating, physical activity, and depressive symptoms, these effects were not different between groups, possibly owing to the sample size and the psychological referral for all participants with elevated depressive symptoms. Significant effects on BMI and BP may require more intensive interventions, including adjusting pharmacologic treatment if indicated. The mild increase in BMI over time in the intervention group could be related to the lack of control the research group had over the pharmacologic treatment of the participants (i.e., hyperinsulinemia can increase adipose tissue) (47) and the focus of the ¡Sí, Yo Puedo! Program on metabolic control (meeting the HbA1c target) rather than weight loss.
Limitations of this study include its being a small pilot study, conducted in several geographic locations in Mexico City. Our sample also may represent a more motivated sample and it is important to emphasize that SMBG supplies were provided as part of the intervention in a setting where people with T2D hardly ever have access to a glucometer at home. Despite these limitations, we reached a vulnerable population with respect to income, working status, food insecurity, and elevated depressive symptoms. We also reached men with T2D (32% of the sample), who can be challenging to engage in DSME programs.
In conclusion, we have demonstrated the potential of the ¡Sí, Yo Puedo! program, developed for the sociocultural context of adults with T2D attending Seguro Popular clinics in Mexico City, to have a positive impact on self-efficacy, diabetes self-management, and HbA1c. Empowering adults with T2D self-management skills can improve health outcomes in vulnerable populations. High attendance and low attrition were also demonstrated. Providing theory-based picture/text messages may be a key strategy to support engagement in diabetes self-management over time. Future research toward scale-up of ¡Sí, Yo Puedo! is warranted.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—RW, MV-C, and RP-E: designed the research; MV-C, SDLC, RD, SB-M, MP-C, and AL-M: conducted the research; RW, MV-C, SJ, and AL-M: analyzed the data and performed the statistical analysis; RW, MV-C, RP-E, and AL-M: wrote the manuscript; RW and MV-C: had primary responsibility for the final content; and all authors: read and approved the final manuscript.
Notes
Supported by National Institute of Nursing Research grant R21NR015856 (to RW).
Author disclosures: The authors report no conflicts of interest. RW, RD, and RP-E traveled to Mexico City during study start-up. SDLC traveled to the United States during data analysis.
Abbreviations used: BP, blood pressure; DSME, diabetes self-management education; GAM, mutual help groups; GLMM, generalized linear mixed model; HbA1c, glycated hemoglobin; PHQ-8, Patient Health Questionnaire-8; RA, research assistant; SDSCA, Summary of Diabetes Self-Care Activities questionnaire; SMBG, self-monitoring of blood glucose; T2D, type 2 diabetes.
References
- 1. Organisation for Economic Co-operation and Development (OECD). Health at a glance 2017: OECD indicators. Paris: OECD Publishing; 2017. [Google Scholar]
- 2. International Diabetes Federation (IDF). IDF diabetes atlas. 8th ed Brussels (Belgium): IDF; 2017. [Google Scholar]
- 3. Alegre-Díaz J, Herrington W, López-Cervantes M, Gnatiuc L, Ramirez R, Hill M, Baigent C, McCarthy MI, Lewington S, Collins R et al.. Diabetes and cause-specific mortality in Mexico City. N Engl J Med. 2016;375(20):1961–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barquera S, Campos-Nonato I, Aguilar-Salinas C, Lopez-Ridaura R, Arredondo A, Rivera-Dommarco J. Diabetes in Mexico: cost and management of diabetes and its complications and challenges for health policy. Global Health. 2013;9(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A, Gudbjörnsdottir S, Wedel H, Clements M, Dahlqvist S, Lind M. Excess mortality among persons with type 2 diabetes. N Engl J Med. 2015;373(18):1720–32. [DOI] [PubMed] [Google Scholar]
- 6. Lerman I, Lozano L, Villa AR, Hernández-Jiménez S, Weinger K, Caballero AE, Salinas CA, Velasco ML, Gómez-Pérez FJ, Rull JA. Psychosocial factors associated with poor diabetes self-care management in a specialized center in Mexico City. Biomed Pharmacother. 2004;58(10):566–70. [DOI] [PubMed] [Google Scholar]
- 7. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, Cypress M, Faulkner P, Fischl AH, Francis T et al.. National Standards for Diabetes Self-Management Education and Support. Diabetes Educ. 2017;43(5):449–64. [DOI] [PubMed] [Google Scholar]
- 8. Silva-Tinoco R, Meza DG, García Martinez D, Orozco J, Romero-Ibarguengoitia ME, De la Torre-Saldañ VA, Ramos Garcia JA, Dolores MC, Cuatecontzi ET. Diabetes self-management education program effect on glycemic control and insulin dosing in poor diabetes literacy patients from urban areas in Mexico City—therapeutic education underuse and insulin overuse. Diabetes. 2018;67(Supplement 1):658–P. [Google Scholar]
- 9. Weller SC, Baer RD, de Alba Garcia JG, Salcedo Rocha AL. Are differences between patient and provider explanatory models of diabetes associated with patient self-management and glycemic control?. J Health Care Poor Underserved. 2013;24(4):1498–510. [DOI] [PubMed] [Google Scholar]
- 10. Whittemore R, Vilar-Compte M, De La Cerda S, Marron D, Conover R, Delvy R, Lozano-Marrufo A, Pérez-Escamilla R. Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study. Int J Equity Health. 2019;18(1):133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Secretaría de Salud. Programa de Acción Específico: prevención y control de la diabetes mellitus 2013–2018. Mexico City: D.R. Secretaría de Salud; 2014. [Google Scholar]
- 12. Access to Nutrition Initiative. Mexico's nutrition challenges: Access to Nutrition Index. [Internet] Utrecht (The Netherlands): Access to Nutrition Foundation; 2012. [cited 2019 Dec 18] Available from: https://www.accesstonutrition.org/mexicos-nutrition-challenges. [Google Scholar]
- 13. Mundo-Rosas V, Unar-Munguía M, Hernández-F M, Pérez-Escamilla R, Shamah-Levy T. [Food security in Mexican households in poverty, and its association with access, availability and consumption]. Salud Publica Mex. 2019;61(6):866–75. [DOI] [PubMed] [Google Scholar]
- 14. Whittemore R, Vilar-Compte M, Burrola-Méndez S, Lozano-Marrufo A, Roberta D, Pardo-Carrillo M, De La Cerda S, Peña-Purcell N, Pérez-Escamilla R. Development of a diabetes self-management + mHealth program: tailoring the intervention for a pilot study in a low-income setting in Mexico. Pilot Feasibility Stud. 2020;6(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–91. [DOI] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J et al.. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Raidl M, Spain K, Lanting R, Lockard M, Johnson S, Spencer M, Sant L, Welch J, Liddil A, Hartman-Cunningham M. The healthy diabetes plate. Prev Chronic Dis. 2007;4(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 19. Bowen ME, Cavanaugh KL, Wolff K, Davis D, Gregory RP, Shintani A, Eden S, Wallston K, Elasy T, Rothman RL. The diabetes nutrition education study randomized controlled trial: a comparative effectiveness study of approaches to nutrition in diabetes self-management education. Patient Educ Couns. 2016;99(8):1368–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Staum EL. Nutrition care and education of the patient with diabetes in the Joslin Clinic. Av Diabetol. 2008;24(2):157–64. [Google Scholar]
- 21. Joslin Diabetes Center, Egg Nutrition Center. Eating well with diabetes: a teaching guide for healthcare professionals. [Internet] Chicago (IL): Egg Nutrition Center; 2013; [cited 2020 Feb 18] Available from: https://www.eggnutritioncenter.org/content/uploads/Eating-well-with-diabetes-teaching-guide.pdf. [Google Scholar]
- 22. American Diabetes Association. All about carbohydrate counting. [Internet] Arlington (VA): American Diabetes Association; 2009. [cited 2020 Feb 18] Available from: https://professional.diabetes.org/sites/professional.diabetes.org/files/media/All_About_Carbohydrate_Counting.pdf. [Google Scholar]
- 23. Diabetes Care and Education Practice Group. Ready, set, start counting!. [Internet] Chicago (IL): Academy of Nutrition and Dietetics; 2016. [cited 2020 Feb 18] Available from: https://higherlogicdownload.s3.amazonaws.com/THEACADEMY/bc90d439-1a0b-4d10-8426-0d0ccc40f516/UploadedImages/DCE/Documents/1946_English_Handout_Final.pdf. [Google Scholar]
- 24. Rivera JA, Barquera S, González-Cossío T, Olaiz G, Sepúlveda J. Nutrition transition in Mexico and in other Latin American countries. Nutr Rev. 2004;62(7 Pt 2):S149–57. [DOI] [PubMed] [Google Scholar]
- 25. Arvizú Martínez O, Polo Oteyza E, Shamah Levy T. Qué y cómo comemos los Mexicanos: consumo de alimentos en la población urbana. Cuernavaca (Mexico): Instituto Nacional de Salud Pública; 2015. [Google Scholar]
- 26. Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29. [Google Scholar]
- 27. Vilar-Compte M, Bernal-Stuart A, Orta-Alemán D, Ochoa-Rivera T, Pérez-Escamilla R. Is the Latin American and Caribbean Food Security Scale an appropriate instrument for Mexican urban older adults?. J Frailty Aging. 2014;3(3):173–9. [DOI] [PubMed] [Google Scholar]
- 28. American Diabetes Association. 6. Glycemic targets: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(Suppl 1):S66–76. [DOI] [PubMed] [Google Scholar]
- 29. Moskowitz KA, Walsh B, Shipwash M, Mihane S, Mercer K, Suscha E, Shafai M, Lindke C, Xie C, Anderson J. Multicenter accuracy assessment of A1CNow+: a disposable system for monitoring hemoglobin A1c. . Diabetes. 2017;; 66:(Supplement 1):A231. [Google Scholar]
- 30. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–50. [DOI] [PubMed] [Google Scholar]
- 31. Vincent D, McEwen MM, Pasvogel A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs Res. 2008;57(2):101–6. [DOI] [PubMed] [Google Scholar]
- 32. Herrmann SD, Heumann KJ, Der Ananian CA, Ainsworth BE. Validity and reliability of the Global Physical Activity Questionnaire (GPAQ). Meas Phys Educ Exerc Sci. 2013;17(3):221–35. [Google Scholar]
- 33. World Health Organization (WHO). Global physical activity surveillance. [Internet] Geneva: WHO, 2017. [cited 2019 Dec 11] Available from:https://www.who.int/ncds/surveillance/steps/GPAQ/en/. [Google Scholar]
- 34. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–73. [DOI] [PubMed] [Google Scholar]
- 35. Ritter PL, Lorig K, Laurent DD. Characteristics of the Spanish- and English-language self-efficacy to manage diabetes scales. Diabetes Educ. 2016;42(2):167–77. [DOI] [PubMed] [Google Scholar]
- 36. Ritter PL, Lorig K. . The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J Clin Epidemiol. 2014 Nov;; 67((11):):1265–73. [DOI] [PubMed] [Google Scholar]
- 37. Hoos T, Espinoza N, Marshall S, Arredondo EM. Validity of the Global Physical Activity Questionnaire (GPAQ) in adult Latinas. J Phys Act Health. 2012;9(5):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63(4):679–86. [DOI] [PubMed] [Google Scholar]
- 39. Brown MB, Forsythe AB. Robust tests for the equality of variances. J Am Stat Assoc. 1974;69(346):364–7. [Google Scholar]
- 40. Wagner JA, Bermudez-Millan A, Damio G, Segura-Perez S, Chhabra J, Vergara C, Feinn R, Perez-Escamilla R. A randomized, controlled trial of a stress management intervention for Latinos with type 2 diabetes delivered by community health workers: outcomes for psychological wellbeing, glycemic control, and cortisol. Diabetes Res Clin Pract. 2016;120:162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pérez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Pérez S, Vega-López S, Kollannor-Samuel G, Calle M, Shebl FM, D'Agostino D. Impact of a community health workers–led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 2015;38(2):197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Oh H, Ell K. Associations between changes in depressive symptoms and social support and diabetes management among low-income, predominantly Hispanic patients in patient-centered care. Diabetes Care. 2018;41(6):1149–56. [DOI] [PubMed] [Google Scholar]
- 43. Peña-Purcell NC, Boggess MM, Jimenez N. An empowerment-based diabetes self-management education program for Hispanic/Latinos: a quasi-experimental pilot study. Diabetes Educ. 2011;37(6):770–9. [DOI] [PubMed] [Google Scholar]
- 44. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, Maryniuk MD, Siminerio L, Vivian E. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin Diabetes. 2016;34(2):70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. International Diabetes Federation (IDF). Access to medicines and supplies for people with diabetes. Brussels (Belgium): International Diabetes Federation; 2016. [Google Scholar]
- 46. Haider R, Sudini L, Chow CK, Cheung NW. Mobile phone text messaging in improving glycaemic control for patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2019;150:27–37. [DOI] [PubMed] [Google Scholar]
- 47. Erion KA, Corkey BE. Hyperinsulinemia: a cause of obesity?. Curr Obes Rep. 2017;6(2):178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]