Abstract
TDI-MPI has been shown to predict cardiovascular mortality in adults; there are a paucity of data on its use in children. We sought to determine the prognostic significance of TDI-MPI at time of DCM diagnosis in children. Patients aged ≤18 years diagnosed with DCM were included along with age- and sex-matched controls. Echo at diagnosis was analyzed to obtain standard measures of LV function, PW-MPI, and septal and LV free wall TDI-MPI. Survival analysis was used to assess the time to composite outcome of death, VAD, or transplant, stratified by TDI-MPI z-score. The study included 79 patients with DCM and 79 controls. During a median follow-up of 182 days (IQR 41–815 days), 16 underwent VAD placement, 21 underwent cardiac transplant, 6 died, and 36 had event-free survival. The median septal TDI-MPI for cases was 0.70 for patients with DCM vs 0.45 for controls (P < .001). Those with septal TDI-MPI z-scores ≥2 develop events significantly earlier than those with z-score <2 (P = .014). In multivariable analysis, TDI-MPI z-score ≥2 was significantly associated with poor outcomes (HR 2.12, 95% CI 1.06–4.23). TDI-MPI can be reliably performed in pediatric patients with DCM. A TDI-MPI z-score ≥2 at diagnosis may be associated with earlier poor outcome. Further studies evaluating the use of TDI-MPI in longitudinal follow-up of patients with DCM may be helpful in refining its clinical use.
Keywords: cardiac function, cardiomyopathy, echocardiography, heart transplant, pediatric
1 |. INTRODUCTION
DCM is a common cause of heart failure in the pediatric population. Transplant-free survival in this population is less than 70% at 5 years and has not improved significantly in the last 20 years.1,2 Several echocardiographic parameters have been used to identify patients at risk of poor outcomes to provide optimal management and counseling.3,4
MPI, the sum of the isovolumic contraction and relaxation times over the ejection time, provides the benefit of measuring systolic and diastolic function, both of which are abnormal in DCM. MPI derived from pulsed-wave Doppler measurements of mitral inflow and aortic outflow has been associated with poor prognosis in adults and children with DCM.5–8
Unlike PW-MPI, TDI-MPI is measured during one cardiac cycle, thereby avoiding discrepancies arising from variations in heart rate when measured in different cycles.9 Previous studies have examined the use of TDI-MPI in lieu of the traditional PW-MPI.10–12 TDI-MPI has shown promise as a predictor of clinical outcomes in adults with heart failure.12,13
This pediatric study aimed to evaluate the relationship between TDI-MPI, performed at the time of diagnosis of DCM, with clinical outcomes and hence explore its potential role as a prognostic marker.
2 |. METHODS
All patients aged ≤18 years who presented to our institution with a new diagnosis of DCM between 2006 and 2017 were identified using an institutional database. All patients with adequate TDI for analysis were included. Baseline clinical data collected at the time of initial echo included age, weight, BSA, sex, likely etiology of cardiomyopathy, use of milrinone, and BNP level. The following mutually exclusive outcome end-points were assigned for all patients: placement of VAD, cardiac transplantation, death, or event-free survival. Follow-up was calculated from time of presentation echo until first event or last follow-up if no event occurred.
Two independent reviewers (LW and FM) performed an off-line analysis using the measuring tool available in the Syngo Dynamics (Siemens, Mountain View, CA) digital storage system. Off-line analysis included measurement of mitral inflow and aortic outflow pulsed-wave Doppler tracings to calculate PW-MPI from an apical four-chamber view. The TDI-derived s’ and e’ velocities were measured at the LV free wall and the septum. TDI-MPI was calculated using the following formula: TDI-MPI = (isovolumic contraction time + isovolumic relaxation time)/ejection time (Figure 1) at the septum and LV free wall. M-mode derived left ventricular LV SF and LVEDD z-scores were also measured for all patients. Degree of mitral regurgitation and tricuspid regurgitation peak gradient, if present, was obtained from reports. Mitral regurgitation was assessed qualitatively and graded as none, mild, moderate, or severe. Peak gradient of tricuspid regurgitant jet was measured and reported both alone and as ratio of gradient to simultaneously measured blood pressure. Interrater reliability for TDI-MPI, PW-MPI, LVEDD, and LV SF was assessed on 17 patients (12 patients with DCM, 5 controls).
FIGURE 1.
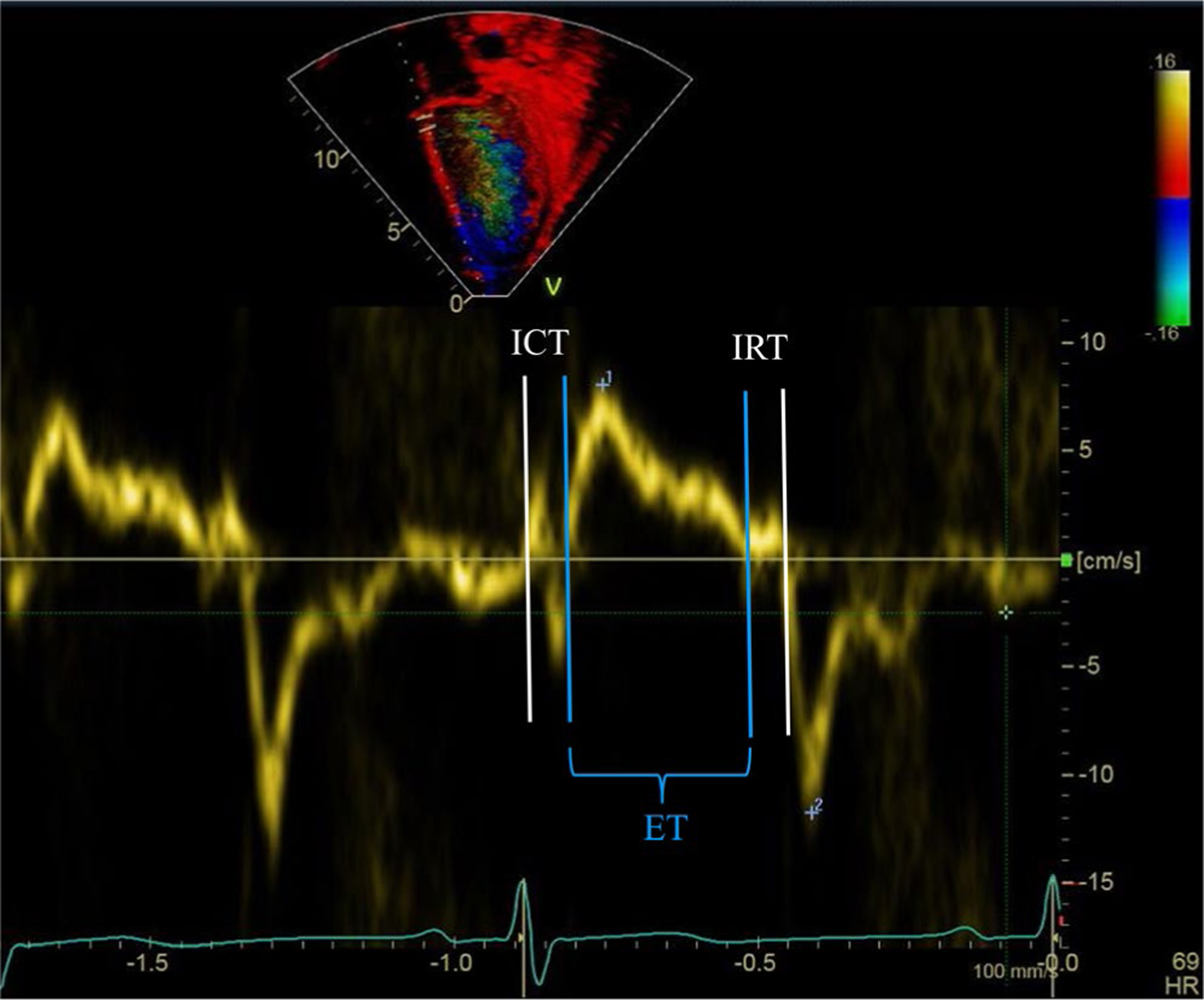
Measurement of TDI-MPI was performed as shown. ICT, ET, and IRT were measured separately, and TDI-MPI was calculated using the following formula: TDI-MPI = (ICT + IRT)/ET. ET, ejection time; ICT, isovolumic contraction time; IRT, isovolumic relaxation time
Given previously reported changes in MPI with age and lack of normal values for TDI-MPI in children, echocardiograms from an equal number of age-and sex-matched unaffected controls were analyzed. Age matching was done by month for those less than one year of age and by year for those greater than one year of age. Controls were selected from normal echocardiograms at our institution within the same time period. The indications for echocardiograms in controls were chest pain, murmur, and syncope, and these patients were determined to have no underlying cardiac condition and no family history of cardiomyopathy. TDI-MPI and PW-MPI Z-scores of +2 for our population were calculated by using the mean and standard deviation of age- and sex-matched controls. Both TDI-MPI and PW-MPI were normally distributed in the control population.
This study was approved by the Institutional Review Board of Children’s Healthcare of Atlanta.
2.1 |. Statistical analysis
Statistical analyses were conducted using SAS 9.4. Statistical significance was assessed at the 0.05 level. Descriptive statistics for all variables of interest are presented as medians and interquartile ranges or counts and percentages, as appropriate. Normality of continuous variables was assessed using histograms, normal probability plots, and the Anderson-Darling test for normality. Continuous variables were compared between those who reached primary outcome (VAD, transplant, or death) and those who did not reach primary outcome using Wilcoxon rank-sum tests, and categorical variables were compared using chi-square tests. Interrater reliability for imaging characteristics was evaluated by calculating the intraclass coefficient (ICC). The ICC ranges from 0 to 1, with a score of 0 indicating high variability between the measurements, while a score of 1 indicating no variability between the measurements. In this study, the following criteria were used to interpret measure of agreement: ICC = 0.91 to 1.00, excellent agreement; ICC = 0.81 to 0.90, substantial agreement; ICC = 0.71 to 0.80, moderate agreement; and ICC = 0.61 to 0.70 fair agreement. MPI Z-scores of +2 for our population were calculated for all MPI variables using the mean and standard deviation of age- and sex-matched controls, which were normally distributed for all MPI variables. Kaplan-Meier curves were generated to estimate freedom from death/VAD/transplant in patients with DCM stratified by <2 and ≥2 MPI z-score, and the log-rank test was used to compare survival distributions. Multivariable Cox proportional hazard model was used to evaluate the relationship between TDI-MPI z-score and time to death/VAD/transplant. All variables with P-value <.1 in univariable Cox regression (TDI-MPI z-score, LV SF, LVEDD z-score, degree of mitral regurgitation, and milrinone use) were included in multivariable Cox regression model. The proportional hazard assumption was assessed graphically using log-log survival curves and was met for all variables included in the final model.
3 |. RESULTS
Of the 125 patients presenting with a new diagnosis of DCM during the study period, 79 met the inclusion criteria (21 had no TDI, 5 had unclear TDI, and 20 were lost to follow-up after initial hospitalization). Seventy-nine age- and sex-matched controls were included. PW-MPI was available for 67 of the DCM patients and all controls; all other variables were available for all patients. The clinical characteristics and echocardiographic parameters of patients with DCM at the time of diagnosis are summarized in Table 1. The median age at diagnosis was 2 years (IQR 171 days-12 years), and the majority had a diagnosis of idiopathic DCM. At last follow-up (median follow-up 182 days, IQR 41–815), 45.6% were alive (n = 36), with the remainder having under-gone VAD placement (n = 21) or transplant (n = 16) or died (n = 6).
TABLE 1.
Clinical characteristics and echocardiographic parameters of patients with dilated cardiomyopathy (N = 79)
| N (%) or Median (IQR) | |
|---|---|
| Age | 2 y (146 d, 12 y) |
| Male sex | 37 (46.8%) |
| Cause of DCM | |
| Idiopathic | 64 (81.0%) |
| Chemotherapy associated | 8 (10.1%) |
| Muscular dystrophy associated | 2 (2.5%) |
| LV non-compaction | 3 (3.8%) |
| Pacer associated | 2 (2.5%) |
| On milrinone at time of echo | 40 (50.6%) |
| BNP on admission (N = 73) | 1094 (265, 2999) |
| Outcomes | |
| Alive at last follow-up | 36 (45.6%) |
| Death | 6 (7.6%) |
| Mechanical support | 16 (20.3%) |
| Transplant | 21 (26.6%) |
| LV shortening fraction | 13.0 (8.3, 17.9) |
| LVEDD z-score | 5.18 (2.78, 8.0) |
| PW-MPI | 0.62 (0.40, 0.77) |
| LV free wall TDI | |
| s’ | 5.00 (3.83, 6.00) |
| e’ | 9.00 (6.08, 13.00) |
| MPI | 0.74 (0.59, 0.96) |
| Septum TDI | |
| s’ | 4.25 (3.61, 5.21) |
| e’ | 7.14 (5.11, 9.05) |
| MPI | 0.67 (0.51, 0.83) |
| Mitral regurgitation | |
| None or trivial | 19 (24%) |
| Mild | 27 (34%) |
| Moderate | 17 (23%) |
| Severe | 16 (20%) |
| Peak TR gradient (mm Hg, n = 49) | 33 (22, 40) |
| TR gradient as % of systolic blood pressure (n = 40) | 32 (23,44) |
Abbreviations: BP, blood pressure; TR, tricuspid regurgitation; TR, tricuspid regurgitation.
Interrater reliability was moderate for septum and free wall TDI-MPI with an intraclass coefficient (ICC) of 0.79 (0.57, 0.92) and 0.77 (0.52, 0.91). It was fair for PW-MPI with ICC of 0.62 (0.21, 0.86). Interrater reliability was excellent for both LVEDD and SF (ICC >0.95 for both). Compared with control subjects, patients with DCM had significantly higher PW-MPI (0.62 vs 0.23, P < .001), LV free wall TDI-MPI (0.74 vs 0.43, P < .001), and septal TDI-MPI (0.70 vs 0.45, P < .001) (Figure 2). Using control data, Z-score of +2 was set at 0.47 for PW-MPI, 0.63 for septal TDI-MPI, and 0.66 for LV free wall TDI-MPI.
FIGURE 2.

Myocardial performance index (MPI) in patients with dilated cardiomyopathy (DCM) vs controls. Values were significantly higher (P < .01 for all groups) in patients with DCM compared to age- and sex-matched healthy controls
Clinical and echo characteristics of patients who reached primary outcome vs those who did not are shown in Table 2. Patients without primary outcome had higher LV SF and septal TDI s’ and lower LVEDD z-scores and PW-MPI. Septal TDI-MPI and PW-MPI z-scores ≥2 were more commonly seen in patients with primary outcome, while LV free wall TDI-MPI z-score ≥2 was not (Table 2). On Kaplan-Meier survival analysis, z-score of ≥2 on either septal TDI-MPI or PW-MPI was associated with worse event-free survival (Figure 3).
TABLE 2.
Characteristics of patients who reached primary outcome vs patients who did not reach primary outcome
| No Outcome (N = 36) N (%) or Median (IQR) | Death, VAD, or Transplant (N = 43) N (%) or Median (IQR) | P-value | |
|---|---|---|---|
| Age at presentation (years) | 2 (0,12) | 3 (0,12) | .883 |
| BNP on admission | 991 (139, 2326) | 1353 (585, 4220) | .134 |
| Male gender | 17 (47.2%) | 20 (46.5%) | .950 |
| On milrinoneat time of echo | 18 (44%) | 23 (56%) | .757 |
| LV shortening fraction | 15.7 (10.6, 20.5) | 9.72 (7.95, 14.2) | .002 |
| LVEDD z-score | 4.35 (2.38, 5.93 | 6.27 (4.01, 8.75) | .012 |
| PW-MPI | 0.58 (0.31, 0.69) | 0.67 (0.48, 0.80) | .041 |
| PW-MPI z-score ≥2 | 17 (54.8%) | 29 (80.6%) | .024 |
| LV free wall TDI | |||
| s’ | 5.06 (3.77, 7.00) | 5.00 (4.00, 5.51) | .295 |
| e’ | 9.32 (6.98, 14.2) | 9.00 (6.02, 11.0) | .170 |
| MPI | 0.69 (0.58, 0.82) | 0.77 (0.62, 1.02) | .235 |
| MPI z-score ≥2 | 21 (58.3%) | 29 (67.4%) | .403 |
| Septum TDI | |||
| s’ | 4.42 (4.00, 5.29) | 4.00 (3.00, 5.21) | .044 |
| e’ | 7.44 (5.69, 9.63) | 7.00 (5.11, 9.00) | .590 |
| MPI | 0.56 (0.50, 0.77) | 0.73 (0.52, 0.85) | .103 |
| MPI z-score ≥2 | 16 (44.4%) | 29 (67.4%) | .040 |
| Mitral regurgitation | |||
| None or trivial | 12 (63%) | 7 (37%) | .266 |
| Mild | 11 (41%) | 16 (59%) | |
| Moderate | 8 (47%) | 9 (53%) | |
| Severe | 5 (50%) | 5 (50%) | |
| Peak TR gradient (mm Hg, n = 49) | 25 (14, 35) | 34 (25,42) | .025 |
| Peak TR gradient as % of systolic blood pressure (n = 40) | 23 (16, 36) | 39 (28, 48) | .020 |
FIGURE 3.

Kaplan-Meier survival analysis stratified by MPI z-score. A, Patients with septal TDI-MPI z-score ≥2 (0.63) had earlier occurrences of death, VAD, or transplant compared to those <2 (P = .02). B, A similar pattern was observed in those patients with PW-MPI z-score ≥2 (0.47) (P = .048)
In multivariable analysis, septal TDI-MPI z-score ≥2 (HR 2.31, 95% CI 1.13–4.74) was associated with higher rates of death, transplant, or VAD placement, controlling for LV SF, LVEDD z-score, severity of mitral regurgitation, and use of milrinone at time of echo (Table 3).
TABLE 3.
Cox regression model for time to primary outcome of death, VAD placement, or transplant
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Septum TDI-MPI z-score | ||||||
| ≥2 | 2.13 | 1.12–4.04 | .02 | 2.31 | 1.13–4.74 | .02 |
| <2 | ref | - | - | ref | - | - |
| LV shortening fraction | 0.91 | 0.86–0.96 | <.01 | 0.91 | 0.86–0.98 | <.01 |
| LVEDD z-score | 1.07 | 0.99–1.17 | .09 | 1.06 | 0.95–1.218 | .29 |
| Mitral regurgitation | ||||||
| Severe | 2.83 | 1.09–7.30 | .03 | 1.16 | 0.35–3.90 | .81 |
| Moderate | 1.58 | 0.59–4.25 | .36 | 0.81 | 0.27–2.46 | .71 |
| Mild | 1.75 | 0.72–4.26 | .22 | 0.77 | 0.25–2.31 | .77 |
| None | ref | - | - | ref | - | - |
| Peak TR gradient | 1.01 | 0.99–1.03 | .21 | - | - | - |
| Peak TR gradient as % of systolic blood pressure | 1.87 | 0.44–8.02 | .40 | - | - | - |
| On milrinoneat time of echo | 2.32 | 1.24–4.36 | .01 | 1.61 | 0.75 −3.49 | .22 |
| Age at presentation | ||||||
| ≥2 y | 1.22 | 0.67–2.22 | .53 | - | - | - |
| <2 y | ref | - | - | - | - | |
| Initial BNP | 1.01 | 0.99–1.01 | .16 | - | - | - |
Abbreviations: BP, blood pressure; TR, tricuspid regurgitation.
Adjusted for TDI-MPI z-score, LV shortening fraction, LVEDD z-score, degree of mitral regurgitation, and milrinone use.
4 |. DISCUSSION
Our results point to the potential prognostic significance of septal TDI-MPI in children with newly diagnosed DCM. Both TDI-MPI and the traditional PW-MPI were significantly higher in patients with DCM than in age- and sex-matched controls. Survival analysis demonstrated earlier and more frequent occurrences of death, transplant, or VAD placement in patients with elevated septal TDI-MPI or PW-MPI at the time of diagnosis.
Measurement of TDI-MPI was reproducible in this patient population, with moderate agreement between the two reviewers for both septal TDI-MPI and LV free wall TDI-MPI. There was a much greater variation in values for LV free wall than septal TDI-MPI values, in both patients with DCM and controls, as compared to the septal TDI-MPI. Additionally, only septal TDI-MPI was significantly associated with poor outcomes. This could be explained by better alignment of Doppler during interrogation of the septum as compared to the LV free wall. This is true in patients with structurally normal hearts but is likely further exacerbated in patients with dilated ventricles and laterally displaced LV free walls. In addition to technical issues that lead to better performance of the septal TDI-MPI, this metric may be capturing some element of biventricular failure, a known predictor of poor outcomes in this population.14
In this study, both septal TDI-MPI and PW-MPI were associated with the early occurrence of poor outcomes. Patients with septal TDI-MPI ≥0.63 (Z-score ≥ + 2) and PW-MPI ≥0.47 had significantly worse event-free survival than those with Z-score <2. Septal TDI-MPI z-score >2 was associated with poor outcomes when controlling for other markers of poor ventricular function such as fractional shortening, LV size, and degree of mitral regurgitation, suggesting added utility of this measure beyond traditional metrics. Previous studies in pediatric patients with DCM have shown LVEDD to be a predictor of poor outcomes.1,3 These studies did not evaluate TDI-MPI. In a multicenter Pediatric Heart Network study, Molina and colleagues found high LVEDD and low ejection fraction are the most predictive of poor outcomes, though PW-MPI was also significantly associated with poor outcomes.3 This study included outpatients with stable chronic heart failure at enrollment, contrasting to our population many of whom were inpatient at diagnosis. In our study, higher septal TDI-MPI was more predictive of earlier poor outcomes than higher LVEDD. Our findings suggest that TDI-MPI might have additional prognostic value to the previously established measures.
Our results are consistent with a growing body of literature on the use of TDI-MPI in predicting outcomes in both children and adults with heart failure. In a cohort of adults with systolic heart failure, Olson et al found global TDI-MPI >0.67 to be a powerful predictor of cardiovascular mortality, independent of ejection fraction and LV size.12 Kim and colleagues found similar results for adults with heart failure with preserved ejection fraction; TDI-MPI >0.66 was an independent predictor of poor outcomes in this population.13 In the only previous work using this metric in the pediatric population, a TDI-MPI of >0.51 accurately predicted disease severity in 25 children with all types of heart failure.11 Taken together, our findings combined with previous ones in both adults and children with various types of heart failure point to the potential of TDI-MPI for prognostication in a variety of clinical conditions related to cardiac dysfunction. While all previous work on this metric in children has focused on patients with systolic dysfunction, the adult literature demonstrating the use in patients with preserved ejection fraction suggests promise in its application in identifying subtle changes prior to deterioration in systolic function in at-risk patients such as those receiving chemotherapy.
While both TDI- and PW-MPI were associated with poor outcomes in our cohort, it is important to note that the values were not directly comparable between the two measures, with control values for TDI-MPI higher than those seen for PW-MPI. There have been conflicting reports on the agreement between these two methods of measuring MPI in healthy controls and patients with heart disease.15–17 A recent study comparing the two with catheterization-derived hemodynamics found TDI-MPI to correlate better with hemodynamic variables.18 These data point to the need to avoid comparison between the two measures, and utilize cutoffs and normal data derived for method-specific MPI measurements, as well as to develop standardized normal values for TDI-MPI in children.
Our study was limited by its retrospective nature. As a result, images were not always optimized for measurement of MPI. Furthermore, not all studies had images needed for off-line analysis of PW-MPI and TDI-MPI, thus making direct comparisons between the two measures in the same study challenging.
Further studies are needed to characterize TDI-MPI’s application in children with heart failure of varying etiology. Serial measurements to assess longitudinal changes in TDI-MPI in individual patients with DCM may provide further insight into possible early detection of subtle changes.
5 |. CONCLUSIONS
TDI-MPI can be reliably performed in pediatric patients with DCM. A TDI-MPI z-score ≥2 at the time of diagnosis may be associated with poorer outcome and could be used in combination with other metrics of myocardial dysfunction in the identification of those at highest risk. Further studies evaluating the use of TDI-MPI in longitudinal follow-up of patients with DCM may be helpful in refining its clinical use.
Abbreviations:
- BNP
Brain natriuretic peptide
- BSA
body surface area
- DCM
Dilated cardiomyopathy
- ICC
intraclass correlation coefficient
- LV
Left ventricle
- LVEDD
Left ventricular end-diastolic dimension
- PW-MPI
Pulsed-wave Doppler-derived myocardial performance index
- SF
Shortening fraction
- TDI-MPI
Tissue Doppler imaging-derived myocardial performance index
- VAD
Ventricular assist device
REFERENCES
- 1.Alvarez JA, Orav EJ, Wilkinson JD, et al. Competing risks for death and cardiac transplantation in children with dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. Circulation. 2011;124(7):814–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexander PM, Daubeney PE, Nugent AW, et al. Long-term outcomes of dilated cardiomyopathy diagnosed during childhood: results from a national population-based study of childhood cardiomyopathy. Circulation. 2013;128(18):2039–2046. [DOI] [PubMed] [Google Scholar]
- 3.Molina KM, Shrader P, Colan SD, et al. Predictors of disease progression in pediatric dilated cardiomyopathy. Circ Heart Fail. 2013;6(6):1214–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Everitt MD, Sleeper LA, Lu M, et al. Recovery of echocardiographic function in children with idiopathic dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. J Am Coll Cardiol. 2014;63(14):1405–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function-a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26(6):357–366. [PubMed] [Google Scholar]
- 6.Dujardin KS, Tei C, Yeo TC, Hodge DO, Rossi A, Seward JB. Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic-dilated cardiomyopathy. Am J Cardiol. 1998;82(9):1071–1076. [DOI] [PubMed] [Google Scholar]
- 7.McMahon CJ, Nagueh SF, Eapen RS, et al. Echocardiographic predictors of adverse clinical events in children with dilated cardiomyopathy: a prospective clinical study. Heart. 2004;90(8):908–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995;26(2):135–136. [PubMed] [Google Scholar]
- 9.Cui W, Roberson DA. Left ventricular Tei index in children: comparison of tissue Doppler imaging, pulsed wave Doppler, and M-mode echocardiography normal values. J Am Soc Echocardiogr. 2006;19(12):1438–1445. [DOI] [PubMed] [Google Scholar]
- 10.Abd El Rahman MY, Hui W, Dsebissowa F, et al. Comparison of the tissue Doppler-derived left ventricular Tei index to that obtained by pulse Doppler in patients with congenital and acquired heart disease. Pediatr Cardiol. 2005;26(4):391–395. [DOI] [PubMed] [Google Scholar]
- 11.Sanchez Mejia AA, Simpson KE, Hildebolt CF, et al. Tissue Doppler septal Tei index indicates severity of illness in pediatric patients with congestive heart failure. Pediatr Cardiol. 2014;35(3):411–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olson JM, Samad BA, Alam M. Myocardial performance index determined by tissue Doppler imaging in patients with systolic heart failure predicts poor long-term prognosis: an observational cohort study. J Cardiac Fail. 2016;22(8):611–617. [DOI] [PubMed] [Google Scholar]
- 13.Kim H, Yoon HJ, Park HS, et al. Usefulness of tissue Doppler imaging-myocardial performance index in the evaluation of diastolic dysfunction and heart failure with preserved ejection fraction. Clin Cardiol. 2011;34(8):494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLaughlin ES, Travers C, Border WL, Deshpande S, Sachdeva R. Tricuspid annular plane systolic excursion as a marker of right ventricular dysfunction in pediatric patients with dilated cardiomyopathy. Echocardiography. 2017;34(1):102–107. [DOI] [PubMed] [Google Scholar]
- 15.Rojo EC, Rodrigo JL, Perez de Isla L, et al. Disagreement between tissue Doppler imaging and conventional pulsed wave Doppler in the measurement of myocardial performance index. Eur J Echocardiogr. 2006;7(5):356–364. [DOI] [PubMed] [Google Scholar]
- 16.Tekten T, Onbasili AO, Ceyhan C, Unal S, Discigil B. Value of measuring myocardial performance index by tissue Doppler echocardiography in normal and diseased heart. Jpn Heart J. 2003;44(3):403–416. [DOI] [PubMed] [Google Scholar]
- 17.Duzenli MA, Ozdemir K, Aygul N, Soylu A, Aygul MU, Gok H. Comparison of myocardial performance index obtained either by conventional echocardiography or tissue Doppler echocardiography in healthy subjects and patients with heart failure. Heart Vessels. 2009;24(1):8–15. [DOI] [PubMed] [Google Scholar]
- 18.Meric M, Yesildag O, Yuksel S, et al. Tissue Doppler myocardial performance index in patients with heart failure and its relationship with haemodynamic parameters. Int J Cardiovasc Imaging. 2014;30(6):1057–1064. [DOI] [PubMed] [Google Scholar]


