Abstract
Precision medicine is increasingly recognized as a promising approach to improve disease treatment, taking into consideration the individual clinical and biological characteristics shared by specific subgroups of patients. In specific fields such as oncology and hematology, precision medicine has already started to be implemented in the clinical setting and molecular testing is routinely used to select treatments with higher efficacy and reduced adverse effects. The application of precision medicine in psychiatry is still in its early phases. However, there are already examples of predictive models based on clinical data or combinations of clinical, neuroimaging and biological data. While the power of single clinical predictors would remain inadequate if analyzed only with traditional statistical approaches, these predictors are now increasingly used to impute machine learning models that can have adequate accuracy even in the presence of relatively small sample size. These models have started to be applied to disentangle relevant clinical questions that could lead to a more effective management of psychiatric disorders, such as prediction of response to the mood stabilizer lithium, resistance to antidepressants in major depressive disorder or stratification of the risk and outcome prediction in schizophrenia. In this narrative review, we summarized the most important findings in precision medicine in psychiatry based on studies that constructed machine learning models using clinical, neuroimaging and/or biological data. Limitations and barriers to the implementation of precision psychiatry in the clinical setting, as well as possible solutions and future perspectives, will be presented.
Keywords: machine learning, pharmacogenomics, predictive models, risk stratification, personalized therapy
Introduction
Coinciding with the sequencing of the human genome, and the resulting delineation of the genetic architectures of many complex diseases, precision medicine has emerged as a novel player in healthcare.1,2 Although its popularity among providers, users, and public and private stakeholders has increased constantly in the last decade, the adequate comprehension of its characteristics (and of its exact definition), as well as of the complex operational approaches accompanying its implementation, remains limited. For instance, there is consensus that precision medicine is changing the paradigm of clinical care from the traditional evidence-based approach (founded on data gathered in large populations of patients), to an individual-based deep knowledge of clinical (phenotypic) and biological characteristics.3 Yet, accurate descriptions of the potential impact of precision medicine on healthcare, even in economic terms, remain scant. In general, precision medicine “prioritizes the individualization of care and focuses attention on unique characteristics of a particular patient”.3 This is clearly in line with the traditional, clinically oriented approach that has historically permeated medicine, where physicians base their intervention on an accurate dissection of the signs and the symptoms manifested by each individual. Psychiatry, in this regard, is a perfect testament of the potential of a personalized clinical approach. Its foundations are based on descriptive psychopathology and phenomenology, which in turn originate from the accurate analysis and understanding of the internal abnormal processes expressed by each individual.4 However, even if psychiatry is deeply rooted in a personalized approach, the transition toward precision medicine, which needs other sources of information such as neuroimaging and/or biological measures, is still lagging behind compared to other fields of medicine.5 For instance, cancer and haematology have experienced tremendous advancement in this area.6,7 In oncology, the SHIVA trial assessed whether histology-agnostic use of marketed molecularly targeted agents outside their indications based on tumour molecular profiling could improve outcomes for patients with any kind of cancer for whom standard of care had failed, compared with treatment at the physician’s choice.6 Although the trial did not show a significant difference in progression-free survival between molecularly targeted agents compared with treatment at physician’s choice, it did show the potential for a precision medicine approach in oncology.6 Concerning haematology, in 2018 the US Food and Drug Administration (FDA) approved the chimeric antigen receptor T cell (CAR T) for treatment of refractory pre-B cell acute lymphoblastic leukaemia and diffuse large B cell lymphoma.7 This treatment is based on the application of sophisticated ex vivo culture and cellular engineering approaches to autologous T cells that can then express a CAR specific for the CD19 B lymphocyte molecule.7 Thus, CAR T is the perfect exemplification of an intervention designed according to individual biological characteristics.
These are more optimistic scenarios than the one observable in psychiatry. However, it was not so long ago that psychiatry saw attempts to implement precision medicine approaches. One of the examples was the dexamethasone suppression test, which showed a moderate sensitivity (50–65%) but a high specificity (96%) in the prediction, not only of future episodes of depression, but also of response to antidepressant treatment.8 However, the presence of an altered function of the hypothalamus–pituitary–adrenal (HPA) axis is a feature shared by almost all severe psychiatric disorders, limiting the clinical utility of these findings in terms of precision medicine.
One additional introductory remark should be made before starting our exposition. This concerns the need to use proper terminology, and methodology, in precision medicine in general, and even more so in psychiatry. Although a detailed review of these aspects lies outside the scope of this paper, we believe that a general overview of the terms might help the reader in familiarizing with the concepts of precision psychiatry. A list of the main terms is outlined in Table 1. Of particular relevance here is the concept of clinical significance. This is strictly related to, but somewhat independent, from statistical significance. Indeed, a statistically significant finding can or cannot be clinically relevant.9 Conversely, clinical significance relates precisely to its own impact and importance for a patient population.10 Findings with clinical significance are starting to being applied to dosing recommendations for psychotropic drugs, including selective serotonin reuptake inhibitors (SSRI),11 tricyclic antidepressants (TCAs),12 atomoxetine,13 and carbamazepine,14 based on genetic information. Specifically, information on genotypes of CYP2D6 (atomoxetine) and/or CYP2C19 (SSRIs and TCAs), two genes encoding enzymes that contribute to the metabolism of several antidepressants, can be used to adjust the dosage or select an alternative treatment based on the recommendations made by the Clinical Pharmacogenetics Implementation Consortium (CPIC)15 or the Dutch Pharmacogenetics Working Group (DPWG).16 Although translation of CYP2D6 genotype to metabolizing phenotypes is not standardized across laboratories, CPIC and DPWG have recently started to adopt a standardized system in order to develop more consistent dosing guidelines.17 In the case of carbamazepine, recommendations based on HLA genotypes were formulated on the basis of a large body of evidence supporting an association between specific alleles and the risk of severe adverse drug reactions.14 These initiatives represent a precious effort to overcome one of the barriers to precision psychiatry, ie, the difficulty in translating pharmacogenetic results into actionable treatment decisions.
Table 1.
Glossary of Relevant Terms in Precision Psychiatry
| Term | Definition |
|---|---|
| Accuracy | Metric used to evaluate the classification performance of a machine learning model defined by the ratio of the number of correct predictions over the total number of predictions. |
| Precision | Ability of an algorithm to return substantially more relevant results than irrelevant ones |
| AUC | Measure of how well a binary classifier system can distinguish between two groups |
| Sensitivity | Proportion of actual positives that are correctly identified as such |
| Specificity | Proportion of actual negatives that are correctly identified as such |
| PPV | Proportions of positive results in statistics that are true positive |
| NPV | Proportions of negative results in statistics and true negative results |
| Statistical significance | Expresses whether an observed difference is more likely to be a real difference rather than a chance occurrence |
| Clinical significance | Expresses the impact and importance of a finding for a patient population |
Abbreviations: AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value.
However, despite the aforementioned examples, while there is a general consensus on the definition of statistical significance, clinical significance remains a vague concept, relying heavily on the subjective interpretations and assumptions made by the researchers.10 This quandary has started to be resolved with the implementation of data analysis methods, such as machine learning, that allow to make inferences even in the presence of non-linear correlations between the independent variables of a specific outcome, and of relatively small sample sizes, using supervised and unsupervised methods.18 Indeed, machine learning deals with the creation and evaluation of algorithms that facilitate pattern recognition, classification, and prediction, based on models derived from existing data.19 Two main approaches, supervised and unsupervised learning, can be used when applying this analytical method.19 While in supervised learning, specific set of attributes are used to classify data, unsupervised learning discovers the similarity patterns existing in the datasets allowing to identify distinct clusters of objects.19 Although there are challenges, including reproducibility, management of missing data, and overfitting,20,21 that might dampen the enthusiasm for machine learning approaches, these have shown their utility in building clinically relevant predictive models. The classification performance of these models is typically measured using area under the receiver operating characteristic curve (ROC-AUC), accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). As we will show in the following sections, precision medicine, including precision psychiatry, is increasingly relying on the application of this methodology.
In this context, we reckon timely a narrative review of the most significant findings in precision psychiatry on predictive models based on clinical (and partly neuroimaging) data, and on biological measures. We will then discuss the barriers that are still present in the implementation of precision psychiatry, concluding with its potential and future perspectives.
Clinical Predictive Models in Precision Psychiatry
Precision medicine in psychiatry can be enriched by deep knowledge of the biological characteristics of each individual. Yet, there have been several attempts, partly successful, to implement predictive models of specific outcomes (for instance treatment response) based purely on clinical data (Table 2). These studies have mainly focused on: 1) response to lithium,22–24 the mainstay of treatment of bipolar disorder (BD), a recurrent mood disorder characterized by alternating episodes of depression and mania; 2) prediction of resistance to antidepressants in major depressive disorder;25,26 and 3) stratification of the risk27 and outcome prediction28–30 in schizophrenia.
Table 2.
Clinical Predictive Models in Precision Psychiatry
| Outcome | Sample | Classification Methods | Best Performance | Most Relevant Predictors | Reference |
|---|---|---|---|---|---|
| BD | |||||
| Response to lithium (CGI-BP for overall BD illness at 6 months) | 240 outpatients with BD-I or BD-II receiving adjunctive personalized treatment plus either lithium or quetiapine | ENR | Accuracy: 17% | Non-suicidal self-injurious behaviour, ADHD, high levels of mania, of social phobia/anxiety disorder, suicide risk | Kim et al (2019)22 |
| Long-term lithium response (minimum duration of treatment: 1 year) | 1266 patients with BD from seven international specialist clinics | RF | Sensitivity: 0.53 Specificity: 0.90 |
Episodic clinical course | Nunes et al (2020)23 |
| Short-term lithium response (8 weeks) | 20 patients with first-episode bipolar mania | Genetic fuzzy tree | Accuracy: 80% | fMRI and 1H-MRS scans | Fleck et al (2017)24 |
| MDD | |||||
| Treatment-resistant depression | 2555 patients with MDD included in the STAR*D study | Naïve Bayes classifier, RF, SVM | ROC AUC: 0.71 | QIDS score, demographic variables, comorbidity with PTSD, recurrent episodes, psychosis screen positive | Perlis (2013)25 |
| Treatment-resistant depression | 2782 patients with MDD included in the STAR*D study; 225 patients with MDD included in the RIS-INT-93 study | K-means clustering, penalized LR RF, GBDT, XGBoost ENR | Accuracy: 0.70 | Items from QIDS, SHFS, PDSQ, PRISE and WSAS | Nie et al (2018)26 |
| SCZ | |||||
| Subgroups of patients with homogeneous characteristics | 104 patients with SCZ | Hierarchical clustering, LR, SVM, RM | ROC AUC: 0.81 | T1-weighted MRI data, items from SAPS/SANS | Talpalaru et al (2019)27 |
| First episode psychosis or conversion to psychosis within 12 months | 347 participants from eight early psychosis clinics | Spectral clustering analysis, SVM | PPV: 76.5% | Items from EPSI and SIPS | Brodey et al (2019)28 |
| Psychotic relapse | 315 patients included in the included in the FondaMental Expert Centers for Schizophrenia network and followed up for two years | Classification and regression trees | Sensitivity: 0.71 Specificity: 0.45 |
High anger (Buss&Perry subscore), high physical aggressiveness (Buss &Perry scale subscore), high lifetime number of hospitalizations in psychiatry, low education level, PANSS positive subscore at baseline | Fond et al (2019)29 |
| Treatment outcome (GAF score) at 4 weeks and 1 year | 334 patients included in the European First Episode Schizophrenia Trial | Cross validation, SVM | Accuracy: 75% | Unemployment, poor education, functional deficits, unmet psychosocial needs predicted both endpoints; previous depressive episodes, male sex, and suicidality predicted poor 1-year outcomes | Koutsouleris et al (2016)30 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BD, bipolar disorder; BD-I, BD type I; BD-II, BD type 2; CGI-BP, Clinical global impressions scale‐bipolar version; ENR, Elastic net regularization; EPSI, Early Psychosis Screener for Internet; fMRI, functional magnetic resonance imaging; GAF, Global Assessment of Functioning; LR, logistic regression; MDD, major depressive disorder; MRS, magnetic resonance spectroscopy; PANSS, Positive and Negative Syndrome Scale; PDSQ, Psychiatric Diagnostic Screening Questionnaire; PPV, positive predictive value; PRISE, The Patient Rated Inventory of Side Effects; QIDS, Quick Inventory of Depressive Symptomatology; Ref, reference; RF, random forest; ROC AUC, area under the receiver operating characteristic curve; SANS, Scale for the Assessment of Negative Symptoms; SAPS, Scale for the Assessment of Positive Symptoms; SCZ, schizophrenia; SFHS, Short Form Health Survey; SIPS, Structured Interview for Psychosis-Risk Syndromes; STAR*D, Sequenced Treatment Alternatives to Relieve Depression; SVM, support vector machine; WSAS, The Work and Social Adjustment Scale.
The prediction of response to lithium therapy is a clear example of the significance of precision psychiatry. One-third of lithium-treated patients shows a pattern of complete clinical response, with absence of mood recurrences and, importantly, return to normal levels of functioning as well as to good quality of life.31,32 Thus, lithium modifies substantially the trajectory of illness in BD patients, a characteristic that makes this drug a unique therapeutic tool in the field of psychiatry. The identification of reliable clinical predictors of lithium response has therefore gained attention. Quantitative data synthesis has pointed to several clinical factors as possible predictors.33,34 Among these are the presence of an episodic clinical course, the absence of psychotic symptoms, a positive family history of BD and later age of onset.33,34 However, the predictive power of these variables, either singularly or cumulatively, remains inadequate if based only on standard univariate statistical approaches. Proper analytical methods, such as machine learning, could be instrumental in determining, even in the presence of relatively small sample sizes, the accuracy of predictive models and their eventual clinical significance. In this context, Kim et al used data from a randomized clinical trial of outpatients with BD type I or II who received adjunctive personalized treatment plus either lithium or quetiapine.22 In the analysis of lithium response data, the authors split the total sample (n = 240) in a training set (n = 192) and a test set (n = 48), finding that the predictive accuracy of the model was around 17%.22 The most significant predictors of lithium response were the presence of non-suicidal self‐injurious behavior, of attention‐deficit/hyperactivity disorder, of high level of mania, of social phobia/social anxiety disorder, and of suicide risk.22 Although potentially clinically relevant, these findings were based on a clinical outcome (response to lithium with a concomitant evidence-based stabilizing treatment) different from monotherapy efficacy, making the comparison with previous literature difficult. In addition, the model was based on data collected in a trial with a limited duration, which differs from the classical phenotypic definition of long-term lithium response and included also nonclinical features such as serum levels of laboratory markers (creatinine, sodium, potassium, and so on). More recently, a collaborative initiative led by Canadian investigators,23 made use of data from seven international specialist clinics, with a minimum duration of lithium treatment of 1 year, using a validated scale for the assessment of clinical response to lithium.35 This study suggested that lithium response could be predicted with a low rate of false positives (specificity 0.9), although the sensitivity was comparatively less strong (0.53).23 Importantly, even considering the substantial between-site heterogeneity, completely episodic clinical course was the most informative feature in the prediction model of lithium response,23 in line with prior evidence.33,34 It should be noted that attempts of predicting lithium response have been made also using neuroimaging data.24 The proof of concept study of Fleck et al showed that a machine learning system applied to functional magnetic resonance imaging (fMRI) and proton magnetic resonance spectroscopy (1H-MRS) inputs were able to predict post-treatment symptom reductions at 8 weeks of lithium treatment with at least 88% accuracy in training and 80% accuracy in validation.24 However, the outcome chosen for the analysis (short-term lithium response) was again different from the one typically used in clinical and genetic studies.
Another set of findings concerns the testing of predictive algorithms of treatment resistance to antidepressants.25,26 Treatment-resistant depression is a common clinical phenomenon, with about 30% of patients with major depressive disorder showing lack of clinical improvement.36 In addition, a much larger proportion of antidepressant-treated patients show suboptimal responses.36 Predicting with adequate accuracy treatment-resistant depression could translate into a more effective management of the disorder, with a more expedite relief of the symptoms, and a reduction of the costs determined by long-term disability. Using data drawn from the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, Perlis applied different analytical approaches (logistic regression and machine learning algorithms) to test the predictive power of a series of clinical variables selected on the basis of manual and automated approaches.25 Both approaches led to a comparable performance in the prediction of treatment resistance depression with an area under the curve (AUC) of 0.7 in training, testing, and validation datasets.25 Specifically, several variables, such as years of education, presence of recurrent illness, presence of psychosis, African-American ethnicity, presence of Post-Traumatic Stress Disorder, and higher total score at the Quick Inventory of Depressive Symptoms, increased the risk of treatment-resistant depression.25 These findings suggest that it is possible to rely solely on patient self-reported measures to identify at least a subset of individuals at greatest risk for treatment resistance.25 More recently, Nie and coauthors applied five different machine learning approaches to clinical and socio-demographic data from the STAR*D cohort and an independent cohort, the latter used as an external test dataset to predict treatment-resistant depression after two trials of treatment regimens.26 The authors found that, using the top 30 clinical predictors, the gradient boosting decision tree (GBDT) model was able to predict both treatment resistance and non-treatment resistance with comparable accuracy (about 0.7).26 Several variables, including more severe 16-item Quick Inventory of Depressive Symptomatology, clinician-rated (QIDS-C16) symptom severity total score at week 2, presence of anxiety/chronicity as identified with the Psychiatric Diagnostic Screening Questionnaire (PDSQ) questions, lower levels of Physical Health Composite Scores (PCS), presence of nervous system symptom (PRISE question) and Work and Social Adjustment Scale (WSAS) total score were associated with increased odds of being treatment resistant to antidepressants.26
Finally, a few studies focused 1) on the ability of machine learning algorithms to identify subgroups of patients affected by schizophrenia with more homogenous characteristics, that could be targeted by ad hoc interventions, either pharmacological or non-pharmacological, and 2) on the predictive accuracy of diagnostic conversion in at-risk subjects or of symptomatic recurrences.27–30 The implementation of accurate deep phenotyping is a necessary condition to reduce the impact of heterogeneity on prediction accuracy.37 But this might not be sufficient if adequate analytical approaches are not implemented. The work of Talpalaru et al used different classifiers, logistic regression, random forest and support vector machine (SVM), to identify subgroups of schizophrenic patients on the basis of symptomatic and magnetic resonance imaging (MRI) data of 167 subjects were used.27 The subgroups included patients at 1) high symptom burden, 2) predominantly positive symptom burden, and 3) mild symptom burden. These authors found that all three classifiers predicted the high symptom burden group with an AUC higher than the case–control comparison. Additionally, the RF classifier also outperformed the case–control study in predicting the mild symptom burden group.27 Even if not including solely clinical information, these findings show the ability of machine learning algorithms to perform clinical prediction. Furthermore, they demonstrate how the integration of different types of data can increase the performance of predictive algorithms even with relatively small sample sizes. The study of Brodey et al28 tested whether machine learning analysis of data from a self-report screener for early psychosis was able to predict with accuracy the diagnostic conversion to psychosis. The SVM algorithm applied on data from 353 participants showed that this assessment tool had cross-validated PPV of 76.5% at separating individuals who would not convert to psychosis within 12 months from those who either would convert within 12 months or who had already experienced a first-episode psychosis.28 Fond et al showed the ability of a classification and regression tree to predict psychotic relapse in a cohort of 315 patients followed up for 2 years.29 Several clinical characteristics, such as high anger and/or physical aggressiveness, the number of lifetime hospitalizations in psychiatry, low education level, and high positive symptoms at baseline were found to be the best predictors of psychotic relapse at 2 years.29 The work of Koutsouleris et al applied non-linear SVM machine learning to clinical data from 334 patients in the European First-Episode Schizophrenia Trial to predict outcome after 4 weeks and 52 weeks of treatment.30 The accuracy of the predictive models was adequate (75% for 4-week outcomes and 73.8% for 52-week outcomes), showing the feasibility of generalizable, individual-patient prediction of treatment outcomes in first-episode psychosis using pre-treatment clinical information.30 Importantly, the most useful predictors of poor 4-week and 52-week treatment outcome were unemployment, unmet needs in the Camberwell Assessment of Needs (CAN) questionnaire about relationships, daytime activities, and psychological distress.30 Educational difficulties were predictive at 52-week, and low educational status of the patient and the patient’s mother at 4-weeks.30 Poor 1-year outcome was predicted by a series of variables including the Mini-International Neuropsychiatric Interview (MINI) diagnostic items [recurrent major depression, schizophrenia (present and lifetime)], suicidality, male sex, and lower baseline scores on the PANSS positive subscale, presence of conceptual disorganization and hyperactivity (P2 and P4 items of PANSS, respectively).30 Poor 4-week outcome was predicted by higher clinical global impression (CGI) and lower global assessment of functioning (GAF) score at baseline, haloperidol treatment, and unmet needs in the CAN’s accommodation, information, money, and sexual expression domains.30
In summary, these findings show that precision psychiatry have a solid base on clinical data, provided that accurate phenotyping, preferably in a longitudinal perspective, is performed. This can be empowered by the integration of other sources of data, such as neuroimaging and, as we will discuss below, biological measures.
Biological Predictive Models in Precision Psychiatry
The majority of studies assessing whether biological variables are able to increase the accuracy of predictive models of treatment response to psychotropic medications focused on antidepressants (Table 3). A recent meta-analysis evaluated previous studies using machine learning-devised models to predict therapeutic outcomes in unipolar and bipolar depression.38 The quantitative evaluation of 20 studies showed an overall accuracy, clinically relevant, of 0.82. Importantly, the models with the best performance were those informed by multiple data types which included neuroimaging, genetic and clinical predictors.38 In particular, the latter included overall mood symptom severity, anxiety, anhedonia, global functioning, and the number of previous mood episodes.38 In addition, socio-demographic variables, such as employment status, level of education, and household income, contributed significantly to the performance of the predictive models.38 This evidence highlights the importance of including multiple source of data to increase the accuracy of predictive models.
Table 3.
Biological Predictive Models in Precision Psychiatry
| Outcome | Sample | Classification Methods | Best Performance | Most Relevant Predictors | Ref. |
|---|---|---|---|---|---|
| MDD | |||||
| Response to fluvoxamine at 6 weeks (HAMD-21 ≤ 8) | 121 patients with MDD | Neural networks | ROC AUC: 0.73 | 5-HTTLPR and TPH promoter polymorphism | Serretti and Smeraldi (2004)39 |
| Response to antidepressants (HAMD score < 17) | 225 patients with MDD included in the GSRD study | RF, K-means clustering | NA | rs6265 (BDNF), rs7430 (PPP3CC), rs6313 (HTR2A), absence of melancholy | Kautzky et al (2015)41 |
| Remission after duloxetine (MADRS ≤ 10) at 8 weeks | 186 patients with MDD treated with duloxetine | LASSO regression, classification -regression trees, SVM | Accuracy: 0.52 Sensitivity: 0.58 Specificity: 0.46 |
92 SNPs located in various genes | Maciukiewicz et al (2018)42 |
| Remission after citalopram (HDRS-17 ≤ 7) at 12 weeks | 34 patients with MDD and anxiety treated with citalopram + psychotherapy for 12 weeks and 33 controls; validation cohort including 63 patients with MDD treated with citalopram for 8 weeks | SVM | Accuracy: 0.79 Sensitivity: 0.86 Specificity: 0.90 |
mRNA levels of six genes (IFITM3, RPL5, GZMA, RPL24, MATR3, RPL17) | Guillox et al (2015)43 |
| Response to citalopram/escitalopram at 4 and 8 weeks (QIDS-C) | 290 patients with MDD included in the Mayo Clinic PGRN-AMPS SSRI trial | SVM, GLM, RF | Accuracy: 0.80 Sensitivity: 0.83 Specificity: 0.77 |
65 variables including levels of selected metabolites (eg serotonin, kynurenine and tryptophan) SNPs (eg located in DEFB1, AHR, TSPAN5 and ERICH3), psychometric measures and sociodemographic factors | Athreya et al (2018)44 |
| Response to antidepressants (50% reduction of HDRS-6) | 98 patients with MDD treated with SSRI or SNRI | SVM | Accuracy: 0.86 | rsfMRI and 13 SNPs located in 12 genes (ATP6V1B2, PCLO, MTHFR, HTR5A, CLOCK, HTR2C, DRD5, TPH2, SLC6A3, MAOB, TOR1A, PER3) | Pei et al (2019)45 |
| Response to antidepressants (HAMD score at 1, 4, 8 and 24 weeks) | 121 patients with MDD | ENR | Accuracy: 0.85 Sensitivity: 0.80 Specificity: 0.87 |
Brain MRI data, genetic variants and methylation status of different genes | Chang et al (2019)47 |
| SCZ | |||||
| Treatment-resistant schizophrenia | 5554 patients with treatment-resistant schizophrenia, 6299 healthy controls included in the CLOZUK sample | SVM, PRS | ROC AUC SVM: 0.63 ROC AUC PRS: 0.64 |
4998 SNPs located in various genes | Vivian-Griffiths et al (2019)49 |
| Antipsychotic-induced extrapyramidal symptoms | 131 patients with SCZ treated with risperidone and two replication cohorts of 113 patients each, treated with various antipsychotics | Naïve Bayes learner | Sensitivity: 0.39 Specificity: 0.81 |
Four SNPs located in genes of the mTOR signaling pathway (AKT1 and RPTOR) | Boloc et al (2018)52 |
Abbreviations: 5-HTTLPR, serotonin transporter gene-linked functional polymorphic region; ARPnet, antidepressant response prediction network for major depressive disorder; CLOZUK, clozapine UK; ENR, elastic net regularization; GLM, generalized linear model; GRSD, European Group for the Study of Resistant Depression; HAMD, Hamilton Depression Rating Scale; HAMD-21, HAMD, Hamilton Depression Rating Scale 21 items; HDRS-6, Hamilton Depressive Rating Scale 6 items; HDRS-17, Hamilton Depressive Rating Scale 17 items; MADRS, Montgomery–Asberg Depression Rating Scale; MDD, major depressive disorder; MRI, magnetic resonance imaging; mRNA, messenger RNA; NA, not available; rsfMRI, resting state functional MRI; PGRN-AMPS, Mayo Clinic Pharmacogenomics Research Network Antidepressant Medical Pharmacogenomic Study; PRS, polygenic risk score; QIDS-C, quick inventory of depressive symptoms; ROC AUC, area under the receiver operating characteristic curve; SCZ, schizophrenia; SNP, single nucleotide polymorphism; SNRI, serotonin and norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors.
Among the first studies using genetic data to predict response to antidepressants, Serretti and Smeraldi (2004) applied a neural network approach in a sample of 121 patients with major depressive disorder treated with fluvoxamine for 6 weeks.39 Although this study only included genotypic data for two variants [serotonin transporter gene-linked functional polymorphic region (5-HTTLPR) and a polymorphism located in the promoter of the TPH gene, it reached a promising accuracy equal to 0.71 in predicting response to fluvoxamine defined as an Hamilton Depression Rating Scale (HAMD) 21 items (HAMD-21) ≤8.39 An important effort to define algorithms for treatment-resistant depression is currently being made by the European Group for the Study of Resistant Depression (GSRD).40 In a recent work, using random forest and k-means clustering, the authors identified a signature of three genetic variants related to treatment outcome [rs6265 in the gene encoding for the brain-derived neurotrophic factor (BDNF), rs7430 in the Protein Phosphatase 3 Catalytic Subunit Gamma (PPP3CC) gene, and rs6313 in the gene encoding for the serotonin transporter receptor 2A (HTR2A)] that, combined with the absence of melancholy, were associated with a decline in the HAMD score <17 (62% of the patients with this combination compared to 34% in the whole study population).41 A more comprehensive list of genetic variants was investigated by Maciukiewicz et al (2018).42 The authors used LASSO regression to identify the most promising predictors and SVM to predict treatment outcome in a sample of 186 major depressive disorder patients treated with duloxetine for 8 weeks and for which genome-wide association data (GWAS) were available.42 Response was defined as a 50% increase in the Montgomery–Asberg Depression Rating Scale (MADRS) score from baseline, while remission was reached with a MADRS score ≤10 at end point. While no model showed a good performance for response, a slightly better performance was achieved for remission, although substantially below the threshold for clinical applicability (accuracy=0.52, sensitivity=0.58, and specificity=0.46).42 Although innovative in its approach, the limited number of participants and the choice not to apply any filter or weight according to the biological relevance of the variants might have influenced the results of this study. Besides genotypic data, peripheral messenger RNA (mRNA) levels of selected genes might also inform machine learning models. This approach was applied by a recent study showing that baseline expression levels of six genes (IFITM3, RPL5, GZMA, RPL24, MATR3 and RPL17) selected from genome-wide transcriptome data reached 0.76 accuracy in predicting non-remission after 8 weeks of treatment with citalopram.43
Other studies investigated the use of genetic variants together with imaging or metabolomic information.44,45 Specifically, an SVM model integrating clinical variables with resting-state fMRI and 13 selected single nucleotide polymorphisms (SNPs) was used to predict early response to antidepressants defined as a 50% reduction of the 6-item HAMD (HAMD-6) score after 2 weeks in a sample of 98 Chinese patients with major depressive disorder treated with SSRI (n=63) or SNRI (n=35).45 In this study, the model based on multimodal features achieved a better performance (accuracy = 0.86) compared to models including only fMRI (accuracy = 0.81) or genetic (accuracy = 0.73) data. Another recent study was conducted by Athreya et al (2018), who developed a learning-augmented clinical assessment workflow.44 The aim of this model was to integrate metabolomics and genomics measures derived from peripheral blood with clinical data, to increase the accuracy in the prediction of treatment outcomes. The workflow was designed using data from about 300 patients with major depressive disorder treated with citalopram/escitalopram for 8 weeks and included in the Mayo Clinic Pharmacogenomics Research Network Antidepressant Medical Pharmacogenomic Study (Mayo PGRN-AMPS) and for whom biological measures were available. Response to SSRIs at 4 and 8 weeks was evaluated using the QIDS-C.46 In this study, the analysis of GWAS data and plasma metabolomic concentrations for 31 metabolites, integrated with psychometric measures and sociodemographic factors, increased the prediction accuracy of treatment response from around 52% to 64% compared to a model using only clinical predictors.44 In the first step, unsupervised learning techniques were used to identify the cluster of patients and metabolites associated with symptom severity (eg, serotonin, kynurenine and tryptophan). GWAS data were also used to identify SNPs associated with concentrations of the previously identified metabolites (such as SNPs located in the DEFB1, AHR, TSPAN5 and ERICH3 genes). The final model included 65 variables among SNPs, metabolites and clinical predictors.44 Along this line of research, recently, Chang et alproposed the Antidepressant Response Prediction Network for Major Depressive Disorder (ARPNet) initiative, a platform aiming to predict whether the patient will reach clinical remission as well as the degree of response to antidepressants (expressed as the HAM-D score).47 In this model, elastic net was used to select the most informative features among clinical and biological predictors including demographic variables, brain MRI features, genetic (35 genes related to antidepressants) and epigenetic data (136 CpG sites). The model was applied to predict response to antidepressants (HAMD scores of the patients measured at 1, 4, 8 and 24 weeks after the initial visit) in a sample of 121 Korean patients with major depressive disorder treated with various antidepressants. From a methodological point of view, the novelty of this model consisted of being composed of three distinct layers (a patient representation, an antidepressant prescription representation and a prediction layer).47 The first two layers capture informative features to create the patient and antidepressant representation vectors, respectively, which are used by the prediction layer based on a linear regression approach. ARPNet reached high sensitivity (0.80), specificity (0.87) and accuracy (0.85), being able to outperform six other machine learning models, including SVM regressor with a linear kernel and random forest regressor.47
Fewer studies applied machine learning models including biological features to predict response to antipsychotics. Rather than focusing on response to single antipsychotics, most studies focused on predicting treatment-resistant schizophrenia.48 A recent study from Vivian-Griffiths et al (2019) used an SVM model to compare its predictive performance to that of a polygenic risk score (PRS) prediction in discriminating patients with treatment-resistant schizophrenia from healthy controls.49 The study was conducted in the CLOZUK sample, including 5554 patients with treatment-resistant schizophrenia and 6299 healthy controls50 and the PRS included 4998 SNPs from the Psychiatric Genomics Consortium (PGC) wave 2 GWAS meta-analysis.51 In this study, the SVM model showed a worse accuracy compared to PRS, with neither of the two approaches showing a prediction accuracy adequate for clinical implementation [median area under the receiver operating characteristics curve (AUC-ROC): PRS = 0.644, SVM = 0.634].49
Based on the high heritability of antipsychotics-induced side effects (0.60–0.80), a recent study developed a model based on genetic data to predict extrapyramidal symptoms induced by antipsychotics,52 which represented a refinement of a previous model proposed by the same authors.53 In light of the evidence implicating the mTOR signaling pathway in antipsychotics-induced extrapyramidal symptoms53 as well as in L-DOPA-induced dyskinesia,54 Boloc et al evaluated 12 functional SNPs located in four genes of the mTOR signaling pathway (AKT1, FCHSD1, RPTOR and DDIT4). Four of these SNPs (rs33925946 and rs1130214 in the AKT1 gene; rs3476568 and rs9915667 in the RPTOR gene) were selected on the basis of their nominal association with extrapyramidal symptoms in a discovery sample including 131 patients treated with risperidone (of which 48 with and 83 without extrapyramidal symptoms). Naive Bayes learner achieved the best performance among three machine learning algorithms applied to the discovery sample and was therefore used to predict the extrapyramidal symptoms status in two replication samples, showing good specificity (0.81 and 0.79) but low sensitivity (0.39 and 0.38).52 Taken together, these data show that, although still falling short of the clinical significance threshold, predictive models based on purely biological data, or integrating them with clinical information, are: 1) starting to reach the accuracy needed to become implantable in clinical settings; 2) showing in general low sensitivity, but high specificity, implying that, at least for predictive models of treatment response, it may be of importance to avoid a premature suspension of a drug trial given that an eventual response would be highly probable.
Barriers to Precision Medicine in Psychiatry
There are great expectations for the successful implementation of precision psychiatry. However, a series of hurdles might delay or even impede this paradigm shift. These involve ethical aspects, the impact of stigma and the possible lack of cost-effectiveness. Ethical components of a correct application of precision psychiatry include self-determination (autonomy), nonmaleficence, clinician competency, justice and veracity.55,56 For instance, self-determination implies that a patient, duly informed on the development of novel diagnostic and prognostic approaches, can freely exert his right to choose (or refuse) them.56 To guarantee this, a clinician should be properly informed on the methodology, and should not have any conflict of interest (such as personal financial benefit) related to it.56 In addition, given that precision psychiatry is strongly related to the analysis of massive datasets (either phenotypic, neuroimaging, or biological), confidentiality and privacy concerns are becoming increasingly relevant. In this context, it is crucial to develop an appropriate ethical-legal framework, which would facilitate safe data sharing. Closely related to the concept of self-determination is the essential need of an active role of the patient to access precision psychiatry instruments (electronic monitoring tools, neuroimaging, genotyping, laboratory tests in general). While this is easily achievable in less severe psychiatric disorders (anxiety disorders, persistent depressive disorder), patients with severe depression, and presenting social withdrawal and/or disorganized behaviour, as in schizophrenia, might self-exclude from precision psychiatry. This should be taken into account in the organization of future mental health services when precision psychiatry will be implemented. Another aspect which has a fundamental impact on mental healthcare in general, and in precision psychiatry specifically, is stigma. Both public (the prejudice disseminated in the general population toward patients affected by mental illness) and self-stigma (occurring when this prejudice is internalized by the patient) can impact on the implementation of precision psychiatry. Public stigma could negatively orient public health policies diminishing the relevance of mental health as a potential target for precision medicine. In addition, self-stigmatized patients could withdraw their participation in precision psychiatry approaches to avoid the spotlight. The influence of stigma should not be neglected, as it is known to influence several important outcomes in psychiatry, such as, for instance, suicide.57
A final remark concerns the possibility that precision psychiatry tools may not be cost-effective, at least in the first phases of their implementation. Although there are examples of cost-effectiveness, such as in pharmacogenetic testing of polymorphisms within the HLA region for the onset of Stevens–Johnson syndrome/toxic epidermal necrolysis in Asian patients treated with carbamazepine (HLA-A*31:01), or agranulocytosis/neutropenia in clozapine treated patients [HLA-B (158T) and HLA-DQB1 (126Q)],58 these remain limited to the prediction of side effects with lack of evidence with regard to the prediction of clinical response. For instance, CAR-T is extremely effective but is priced amongst the most expensive cancer therapies to date, up to $475,000 per treatment.59 This raises doubts on the long-term sustainability of these approaches for public healthcare. However, promising preliminary considerations can be drawn from studies investigating cost savings associated with available pharmacogenetics panels, such as the Assurex GeneSight Psychotropic test.60 Recent studies suggested significant cost savings in medication costs for patients whose antidepressant and antipsychotic prescribing was congruent with the test recommendations.61–63 However, as these studies were funded by Assurex Health, further independent investigations are needed to draw definitive conclusions. In addition, the presence of economic disparities at a global level might also impact the implementation of precision medicine approaches in mental health.
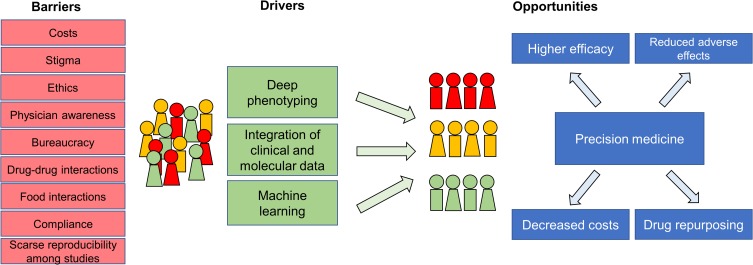
Other obstacles can hinder the implementation of precision psychiatry in clinical settings. Among these are the lack of an adequate knowledge of precision medicine tools, including pharmacogenetics/pharmacogenomics, in clinicians and mental health operators, and compliance toward precision medicine tools. There are extensive data on the impact that inadequate education and training can exert on the proper implementation of precision medicine.64,65 It has been proposed that to realize the translation of precision medicine concepts and instruments into clinical care, specific training packages should be implemented at undergraduate and graduate levels.66 Furthermore, a specific set of skills are needed in healthcare providers involved in precision medicine implementation.67 In this context, initiatives such as those spearheaded by the Electronic Medical Records and Genomics Network show the relevance of ongoing education to ensure provider acceptance and adoption of precision medicine tools.68 Another relevant component that might delay the implementation of precision psychiatry is users’ adherence to tests and procedures. It is conceivable that adherence to precision medicine tools can be as common as that for pharmacological treatment in individuals with mental illness. As several factors, including access to scientifically reliable and valid evidence,69 might substantially influence adherence, disseminating information and involving patients in shared decision-making could favor the implementation of precision psychiatry tools.70 Figure 1 illustrates some of the main barriers and opportunities for precision psychiatry.
Figure 1.
Barriers and drivers of a precision medicine approach in mental health.
Finally, a concluding remark should be made on the protagonists of the implementation of precision psychiatry. As the primary responsibility for the care of patients, psychiatrists will need to take the lead in the implementation of precision psychiatry tools. As previously mentioned, adequate training and education will be key to achieve successful results. In addition, the involvement of patients in specific brief training activities might be an achievable and useful objective, as recent evidence shows that brief community educational program can improve knowledge of complex genomic concepts in the general population.71
In summary, stakeholders will need to assess the impact of these barriers on the application of precision psychiatry. Changes in the organization of mental healthcare as well as of funding policies and creation of proper legislation will be crucial to address them.
Perspectives and Potential of Precision Medicine in Psychiatry
We have argued that precision psychiatry has its foundation in accurate deep phenotyping. However, this can be achieved only if a dynamic longitudinal perspective is taken fully into account. Indeed, most severe psychiatric disorders show developmental trajectories that start in childhood or early adolescence. Antecedents of the disorders are not only psychopathological but also neurocognitive, neuroanatomical, and biological.72 In this context, precision psychiatry might have also a preventative value. The integration of omics approach with neuroimaging and phenotypic data can increase the accuracy in the prediction of diagnostic conversion in at-risk population. Attempts of implementing these approaches have been made in the population at clinical high risk for psychosis.73 Yet, the longitudinal component in psychiatric disorders remains neglected. This is of relevance if we think that even genetic associations with a specific disorder might differ according to different trajectories or patterns of antecedents.74 Even in well-characterized phenotypes, such as lithium response, there is scarce knowledge on the temporal dynamics of those neurobiological changes that underscore the onset of a long-term efficacy of the treatment. And it remains to be established whether immediate neurobiological changes correspond to long-term changes and whether the latter are predictable from the former. In this context, an ongoing large EU funded research initiative is attempting to answer these sensible research and clinical questions.75 Other approaches, again applying a longitudinal perspective, are attempting to disentangle the interaction of several biological components, including the microbiome, on the risk of recurrences in bipolar disorder.76 In conclusion, the potential for precision psychiatry is large, but can be realized only by taking into account the temporal dynamics of mental disorders.
Conclusions
In summary, we have described the intensification of precision approaches in psychiatry. There is a strong expectation that the implementation of precision psychiatry, even if challenging, will ultimately improve the standard of care for patients suffering from mental illness. It remains to be seen whether precision psychiatry will cause the expected paradigm shift, or if it will just prove to be the next in a long line of disillusionments.
Acknowledgment
The authors wish to thank all patients affected by mental illness who make our research possible and most importantly, meaningful. This paper was partly funded by Fondo Integrativo per la Ricerca (FIR)-2018 granted to AS.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
- 1.Jameson JL, Longo DL. Precision medicine — personalized, problematic, and promising. N Engl J Med. 2015;372(23):2229–2234. doi: 10.1056/NEJMsb1503104 [DOI] [PubMed] [Google Scholar]
- 2.Ashley EA. Towards precision medicine. Nat Rev Genet. 2016;17(9):507. doi: 10.1038/nrg.2016.86 [DOI] [PubMed] [Google Scholar]
- 3.Tonelli MR, Shirts BH. Knowledge for precision medicine: mechanistic reasoning and methodological pluralism. JAMA. 2017;318(17):1649–1650. doi: 10.1001/jama.2017.11914 [DOI] [PubMed] [Google Scholar]
- 4.Häfner H. Descriptive psychopathology, phenomenology, and the legacy of Karl Jaspers. Dialogues Clin Neurosci. 2015;17(1):19–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alda M. Personalized psychiatry: many questions, fewer answers. J Psychiatry Neurosci. 2013;38(6):363–365. doi: 10.1503/jpn.130221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Le Tourneau C, Delord J-P, Gonçalves A, et al. Molecularly targeted therapy based on tumour molecular profiling versus conventional therapy for advanced cancer (SHIVA): a multicentre, open-label, proof-of-concept, randomised, controlled phase 2 trial. Lancet Oncol. 2015;16(13):1324–1334. doi: 10.1016/S1470-2045(15)00188-6 [DOI] [PubMed] [Google Scholar]
- 7.June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359(6382):1361–1365. doi: 10.1126/science.aar6711 [DOI] [PubMed] [Google Scholar]
- 8.Carroll B. Clinical applications of the dexamethasone suppression test for endogenous depression. Pharmacopsychiatry. 1982;15(01):19–25. doi: 10.1055/s-2007-1019504 [DOI] [PubMed] [Google Scholar]
- 9.Barlow DH. On the relation of clinical research to clinical practice: current issues, new directions. J Consult Clin Psychol. 1981;49(2):147. doi: 10.1037/0022-006X.49.2.147 [DOI] [PubMed] [Google Scholar]
- 10.LeFort SM. The statistical versus clinical significance debate. Image J Nurs Sch. 1993;25(1):57–62. doi: 10.1111/j.1547-5069.1993.tb00754.x [DOI] [PubMed] [Google Scholar]
- 11.Hicks JK, Bishop JR, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98(2):127–134. doi: 10.1002/cpt.147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hicks J, Sangkuhl K, Swen J, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37–44. doi: 10.1002/cpt.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown JT, Bishop JR, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium guideline for cytochrome P450 (CYP)2D6 genotype and atomoxetine therapy. Clin Pharmacol Ther. 2019;106(1):94–102. doi: 10.1002/cpt.1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phillips EJ, Sukasem C, Whirl-Carrillo M, et al. Clinical pharmacogenetics implementation consortium guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharmacol Ther. 2018;103(4):574–581. doi: 10.1002/cpt.1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caudle K, Klein T, Hoffman J, et al. Incorporation of pharmacogenomics into routine clinical practice: the clinical pharmacogenetics implementation consortium (CPIC) guideline development process. Curr Drug Metab. 2014;15(2):209–217. doi: 10.2174/1389200215666140130124910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lunenburg CATC, van der Wouden CH, Nijenhuis M, et al. Dutch Pharmacogenetics Working Group (DPWG) guideline for the gene–drug interaction of DPYD and fluoropyrimidines. Eur J Hum Genet. 2020;28(4):508–517. doi: 10.1038/s41431-019-0540-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caudle KE, Sangkuhl K, Whirl-Carrillo M, et al. Standardizing CYP2D6 genotype to phenotype translation: consensus recommendations from the clinical pharmacogenetics implementation consortium and Dutch pharmacogenetics working group. Clin Transl Sci. 2020;13(1):116–124. doi: 10.1111/cts.12692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Chen PHC, Krause J, Peng L. How to read articles that use machine learning: users’ guides to the medical literature. JAMA. 2019;322(18):1806–1816. doi: 10.1001/jama.2019.16489 [DOI] [PubMed] [Google Scholar]
- 19.Tarca AL, Carey VJ, Chen XW, Romero R, Drǎghici S. Machine learning and its applications to biology. PLoS Comput Biol. 2007;3(6):e116. doi: 10.1371/journal.pcbi.0030116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beam AL, Manrai AK, Ghassemi M. Challenges to the reproducibility of machine learning models in health care. JAMA. 2020;323(4):305. doi: 10.1001/jama.2019.20866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doshi-Velez F, Perlis RH. Evaluating machine learning articles. JAMA. 2019;322(18):1777–1779. doi: 10.1001/jama.2019.17304 [DOI] [PubMed] [Google Scholar]
- 22.Kim TT, Dufour S, Xu C, et al. Predictive modeling for response to lithium and quetiapine in bipolar disorder. Bipolar Disord. 2019;21(5):428–436. doi: 10.1111/bdi.12752 [DOI] [PubMed] [Google Scholar]
- 23.Nunes A, Ardau R, Berghöfer A, et al. Prediction of lithium response using clinical data. Acta Psychiatr Scand. 2020;141(2):131–141. doi: 10.1111/acps.13122 [DOI] [PubMed] [Google Scholar]
- 24.Fleck DE, Ernest N, Adler CM, et al. Prediction of lithium response in first-episode mania using the LITHium Intelligent Agent (LITHIA): pilot data and proof-of-concept. Bipolar Disord. 2017;19(4):259–272. doi: 10.1111/bdi.12507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perlis RH. A clinical risk stratification tool for predicting treatment resistance in major depressive disorder. Biol Psychiatry. 2013;74(1):7–14. doi: 10.1016/j.biopsych.2012.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nie Z, Vairavan S, Narayan VA, Ye J, Li QS. Predictive modeling of treatment resistant depression using data from STAR*D and an independent clinical study. PLoS One. 2018;13(6):e0197268. doi: 10.1371/journal.pone.0197268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talpalaru A, Bhagwat N, Devenyi GA, Lepage M, Chakravarty MM. Identifying schizophrenia subgroups using clustering and supervised learning. Schizophr Res. 2019;214:51–59. doi: 10.1016/j.schres.2019.05.044 [DOI] [PubMed] [Google Scholar]
- 28.Brodey BB, Girgis RR, Favorov OV, et al. The Early Psychosis Screener for Internet (EPSI)-SR: predicting 12 month psychotic conversion using machine learning. Schizophr Res. 2019;208:390–396. doi: 10.1016/j.schres.2019.01.015 [DOI] [PubMed] [Google Scholar]
- 29.Fond G, Bulzacka E, Boucekine M, et al. Machine learning for predicting psychotic relapse at 2 years in schizophrenia in the national FACE-SZ cohort. Prog Neuropsychopharmacol Biol Psychiatry. 2019;92:8–18. doi: 10.1016/j.pnpbp.2018.12.005 [DOI] [PubMed] [Google Scholar]
- 30.Koutsouleris N, Kahn RS, Chekroud AM, et al. Multisite prediction of 4-week and 52-week treatment outcomes in patients with first-episode psychosis: a machine learning approach. Lancet Psychiatry. 2016;3(10):935–946. doi: 10.1016/S2215-0366(16)30171-7 [DOI] [PubMed] [Google Scholar]
- 31.Alda M. Who are excellent lithium responders and why do they matter? World Psychiatry. 2017;16(3):319–320. doi: 10.1002/wps.20462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alda M. Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry. 2015;20(6):661–670. doi: 10.1038/mp.2015.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kleindienst N, Engel R, Greil W. Which clinical factors predict response to prophylactic lithium? A systematic review for bipolar disorders. Bipolar Disord. 2005;7(5):404–417. doi: 10.1111/j.1399-5618.2005.00244.x [DOI] [PubMed] [Google Scholar]
- 34.Hui TP, Kandola A, Shen L, et al. A systematic review and meta analysis of clinical predictors of lithium response in bipolar disorder. Acta Psychiatr Scand. 2019;140(2):94–115. doi: 10.1111/acps.13062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grof P, Duffy A, Cavazzoni P, et al. Is response to prophylactic lithium a familial trait? J Clin Psychiatry. 2002;63(10):942–947. doi: 10.4088/JCP.v63n1013 [DOI] [PubMed] [Google Scholar]
- 36.Thase ME. Treatment-resistant depression. J Clin Psychiatry. 2011;72(05):e18. doi: 10.4088/JCP.8133tx4c [DOI] [PubMed] [Google Scholar]
- 37.Manchia M, Cullis J, Turecki G, Rouleau GA, Uher R, Alda M. The impact of phenotypic and genetic heterogeneity on results of genome wide association studies of complex diseases. PLoS One. 2013;8(10):e76295. doi: 10.1371/journal.pone.0076295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee Y, Ragguett R-M, Mansur RB, et al. Applications of machine learning algorithms to predict therapeutic outcomes in depression: a meta-analysis and systematic review. J Affect Disord. 2018;241:519–532. doi: 10.1016/j.jad.2018.08.073 [DOI] [PubMed] [Google Scholar]
- 39.Serretti A, Smeraldi E. Neural network analysis in pharmacogenetics of mood disorders. BMC Med Genet. 2004;5(1):27. doi: 10.1186/1471-2350-5-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bartova L, Dold M, Kautzky A, et al. Results of the European Group for the study of resistant depression (GSRD) - basis for further research and clinical practice. World J Biol Psychiatry. 2019;20(6):427–448. doi: 10.1080/15622975.2019.1635270 [DOI] [PubMed] [Google Scholar]
- 41.Kautzky A, Baldinger P, Souery D, et al. The combined effect of genetic polymorphisms and clinical parameters on treatment outcome in treatment-resistant depression. Eur Neuropsychopharmacol. 2015;25(4):441–453. doi: 10.1016/j.euroneuro.2015.01.001 [DOI] [PubMed] [Google Scholar]
- 42.Maciukiewicz M, Marshe VS, Hauschild A-C, et al. GWAS-based machine learning approach to predict duloxetine response in major depressive disorder. J Psychiatr Res. 2018;99:62–68. doi: 10.1016/j.jpsychires.2017.12.009 [DOI] [PubMed] [Google Scholar]
- 43.Guilloux J-P, Bassi S, Ding Y, et al. Testing the predictive value of peripheral gene expression for nonremission following citalopram treatment for major depression. Neuropsychopharmacology. 2015;40(3):701–710. doi: 10.1038/npp.2014.226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Athreya A, Iyer R, Neavin D, et al. Augmentation of physician assessments with multi-omics enhances predictability of drug response: a case study of major depressive disorder. IEEE Comput Intell Mag. 2018;13(3):20–31. doi: 10.1109/MCI.2018.2840660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pei C, Sun Y, Zhu J, et al. Ensemble learning for early-response prediction of antidepressant treatment in major depressive disorder. J Magn Reson Imaging. 2019. doi: 10.1002/jmri.27029 [DOI] [PubMed] [Google Scholar]
- 46.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/S0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- 47.Chang B, Choi Y, Jeon M, et al. ARPNet: antidepressant response prediction network for major depressive disorder. Genes (Basel). 2019;10(11):907. doi: 10.3390/genes10110907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pisanu C, Squassina A. Treatment-resistant schizophrenia: insights from genetic studies and machine learning approaches. Front Pharmacol. 2019;10:617. doi: 10.3389/fphar.2019.00617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vivian-Griffiths T, Baker E, Schmidt KM, et al. Predictive modeling of schizophrenia from genomic data: comparison of polygenic risk score with kernel support vector machines approach. Am J Med Genet B Neuropsychiatr Genet. 2019;180(1):80–85. doi: 10.1002/ajmg.b.32705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamshere ML, Walters JTR, Smith R, et al. Genome-wide significant associations in schizophrenia to ITIH3/4, CACNA1C and SDCCAG8, and extensive replication of associations reported by the Schizophrenia PGC. Mol Psychiatry. 2013;18(6):708–712. doi: 10.1038/mp.2012.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schizophrenia Working Group of the Psychiatric Genomic Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511(7510):421–427. doi: 10.1038/nature13595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boloc D, Gortat A, Cheng-Zhang JQ, et al. Improving pharmacogenetic prediction of extrapyramidal symptoms induced by antipsychotics. Transl Psychiatry. 2018;8(1):276. doi: 10.1038/s41398-018-0330-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mas S, Gassó P, Ritter MA, Malagelada C, Bernardo M, Lafuente A. Pharmacogenetic predictor of extrapyramidal symptoms induced by antipsychotics: multilocus interaction in the mTOR pathway. Eur Neuropsychopharmacol. 2015;25(1):51–59. doi: 10.1016/j.euroneuro.2014.11.011 [DOI] [PubMed] [Google Scholar]
- 54.Martín-Flores N, Fernández-Santiago R, Antonelli F, et al. MTOR pathway-based discovery of genetic susceptibility to L-DOPA-induced dyskinesia in Parkinson’s disease patients. Mol Neurobiol. 2019;56(3):2092–2100. doi: 10.1007/s12035-018-1219-1 [DOI] [PubMed] [Google Scholar]
- 55.Juengst E, McGowan ML, Fishman JR, Settersten Jr RA. From “personalized” to “precision” medicine: the ethical and social implications of rhetorical reform in genomic medicine. Hastings Cent Rep. 2016;46(5):21–33. doi: 10.1002/hast.614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ball TM, Kalinowski A, Williams LM. Ethical implementation of precision psychiatry. Pers Med Psychiatry. 2019;19:100046. [Google Scholar]
- 57.Carpiniello B, Pinna F. The reciprocal relationship between suicidality and stigma. Front Psychiatry. 2017;8:35. doi: 10.3389/fpsyt.2017.00035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Plumpton CO, Pirmohamed M, Hughes DA. Cost effectiveness of panel tests for multiple pharmacogenes associated with adverse drug reactions: an evaluation framework. Clin Pharmacol Ther. 2019;105(6):1429–1438. doi: 10.1002/cpt.1312 [DOI] [PubMed] [Google Scholar]
- 59.Hay AE, Cheung MC. CAR T-cells: costs, comparisons, and commentary. J Med Econ. 2019;22(7):613–615. doi: 10.1080/13696998.2019.1582059 [DOI] [PubMed] [Google Scholar]
- 60.Health Quality Ontario. Pharmacogenomic testing for psychotropic medication selection: a systematic review of the assurex genesight psychotropic test. Ont Health Technol Assess Ser. 2017;17(4):1–39. [PMC free article] [PubMed] [Google Scholar]
- 61.Tanner J-A, Brown LC, Yu K, Li J, Dechairo BM. Canadian medication cost savings associated with combinatorial pharmacogenomic guidance for psychiatric medications. Clinicoecon Outcomes Res. 2019;11:779–787. doi: 10.2147/CEOR.S224277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brown LC, Lorenz RA, Li J, Dechairo BM. Economic utility: combinatorial pharmacogenomics and medication cost savings for mental health care in a primary care setting. Clin Ther. 2017;39(3):592–602.e1. doi: 10.1016/j.clinthera.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 63.Jablonski MR, Lorenz R, Li J, Dechairo BM. Economic outcomes following combinatorial pharmacogenomic testing for elderly psychiatric patients. J Geriatr Psychiatry Neurol. 2019;891988719892341. [DOI] [PubMed] [Google Scholar]
- 64.Squassina A, Manchia M, Manolopoulos VG, et al. Realities and expectations of pharmacogenomics and personalized medicine: impact of translating genetic knowledge into clinical practice. Pharmacogenomics. 2010;11(8):1149–1167. doi: 10.2217/pgs.10.97 [DOI] [PubMed] [Google Scholar]
- 65.Anaya J-M, Duarte-Rey C, Sarmiento-Monroy JC, Bardey D, Castiblanco J, Rojas-Villarraga A. Personalized medicine. Closing the gap between knowledge and clinical practice. Autoimmun Rev. 2016;15(8):833–842. doi: 10.1016/j.autrev.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 66.Ta R, Cayabyab MAS, Coloso R. Precision medicine: a call for increased pharmacogenomic education. Per Med. 2019;16(3):233–245. doi: 10.2217/pme-2018-0107 [DOI] [PubMed] [Google Scholar]
- 67.Kohane IS. Ten things we have to do to achieve precision medicine. Science. 2015;349(6243):37–38. doi: 10.1126/science.aab1328 [DOI] [PubMed] [Google Scholar]
- 68.Rohrer Vitek CR, Abul-Husn NS, Connolly JJ, et al. Healthcare provider education to support integration of pharmacogenomics in practice: the eMERGE network experience. Pharmacogenomics. 2017;18(10):1013–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zavorotnyy M, Ehrlich F, Nenadic I. Health-related Internet use and treatment adherence: a transdiagnostic comparison of outpatients with major depressive disorder and schizophrenia. Psych J. 2020. doi: 10.1002/pchj.355 [DOI] [PubMed] [Google Scholar]
- 70.Arandjelovic K, Eyre HA, Lenze E, Singh AB, Berk M, Bousman C. The role of depression pharmacogenetic decision support tools in shared decision making. J Neural Transm. 2019;126(1):87–94. doi: 10.1007/s00702-017-1806-8 [DOI] [PubMed] [Google Scholar]
- 71.Hillyer GC, Schmitt KM, Reyes A, et al. Community education to enhance the more equitable use of precision medicine in Northern Manhattan. J Genet Couns. 2020;29(2):247–258. doi: 10.1002/jgc4.1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sandstrom A, Sahiti Q, Pavlova B, Uher R. Offspring of parents with schizophrenia, bipolar disorder, and depression. Psychiatr Genet. 2019;29(5):160–169. doi: 10.1097/YPG.0000000000000240 [DOI] [PubMed] [Google Scholar]
- 73.Oliver D, Radua J, Reichenberg A, Uher R, Fusar-Poli P. Psychosis polyrisk score (PPS) for the detection of individuals at-risk and the prediction of their outcomes. Front Psychiatry. 2019;10:174. doi: 10.3389/fpsyt.2019.00174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Iorfino F, Scott EM, Carpenter JS, et al. Clinical stage transitions in persons aged 12 to 25 years presenting to early intervention mental health services with anxiety, mood, and psychotic disorders. JAMA Psychiatry. 2019;76(11):1167. doi: 10.1001/jamapsychiatry.2019.2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Scott J, Hidalgo-Mazzei D, Strawbridge R, et al. Prospective cohort study of early biosignatures of response to lithium in bipolar-I-disorders: overview of the H2020-funded R-LiNK initiative. Int J Bipolar Disord. 2019;7(1):20. doi: 10.1186/s40345-019-0156-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Manchia M, Squassina A, Pisanu C, et al. Investigating the relationship between melatonin levels, melatonin system, microbiota composition and bipolar disorder psychopathology across the different phases of the disease. Int J Bipolar Disord. 2019;7(1):27. doi: 10.1186/s40345-019-0163-y [DOI] [PMC free article] [PubMed] [Google Scholar]