Summary
Background
Atopic dermatitis (AD) is associated with high disease burden, with a significant physical and social impact. However, the association between disease severity and burden of disease, with work productivity and daily activities being one aspect, has not been well characterized.
Objectives
To investigate the impact of disease severity on work productivity and daily activities among adults with AD in Europe (France, Germany and the U.K.) and the U.S.A.
Methods
The survey panel participants for this cross‐sectional internet‐based survey on AD were sourced from the population‐based National Health and Wellness Survey (Europe 2016, U.S.A. 2015 and 2016). AD severity was determined by Patient‐Oriented Scoring Atopic Dermatitis (PO‐SCORAD). Work productivity and work activity impairment were assessed using the Work Productivity and Activity Impairment (WPAI) – Specific Health Problem questionnaire for AD.
Results
The study survey was completed by 1098 respondents with moderate‐to‐severe AD and 134 with mild AD. Overall, the negative impact on work productivity (all WPAI items) was suggested to increase with increasing AD severity (PO‐SCORAD) at the regional level (Europe and U.S.A.) and in the total sample. For overall work impairment due to AD, respondents with mild AD reported a mean of 2·4 h per week of potential work productivity lost, respondents with moderate AD 9·6 h and respondents with severe AD 19·0 h.
Conclusions
Higher AD severity was associated with a greater negative impact on work productivity in adults. This impact is a burden not only for the patient but also for society and may provide incentives for treatment optimization and more effective management of AD.
What's already known about this topic?
Atopic dermatitis (AD) is associated with a high disease burden.
AD has a negative impact on several aspects of health‐related quality of life, one of which is work productivity.
What does this study add?
By using a population of participants with AD recruited from the National Health and Wellness Survey, which collects broad and representative data from the general population, survey data could be obtained from U.S. and European populations of patients with AD.
The present study suggests an increasingly negative impact on work productivity with increasing severity of AD.
The data indicate no regional differences in the impact of AD severity on work productivity.
Short abstract
https://doi.org/10.1111/bjd.18913 available online
Atopic dermatitis (AD) is a complex inflammatory skin condition. Its worldwide geographical occurrence varies enormously. Prevalence data on AD in adults are limited and variable. The results of an international, cross‐sectional, web‐based survey in adults with AD published recently (2018) reported a prevalence of 4·9% in the U.S.A. and 4·4% in Europe, with values in individual countries ranging from 2·2% (Germany) to 8·1% (Italy).1 Earlier studies reported prevalence rates in the U.S.A. between 3·2% and 10·7%, depending on the definition of AD and population studied.2, 3, 4, 5 In Europe, the European Community Respiratory Health Survey II reported AD prevalence based on self‐report, and measured rates of atopy from 0·3% to 6·2% in different countries.5
Being a chronically relapsing condition, AD is associated with a high disease burden, with a significant physical and social impact. AD has been reported to have a detrimental effect on health‐related quality of life, including aspects such as sleep disturbance and reductions in work productivity.6, 7 However, the burden of AD in adult patients has still not been well characterized.7, 8 Very recently, results from a real‐world survey of patient‐reported data showed that adults with AD reported significantly higher rates of anxiety, depression and sleep disorders than controls without AD, as well as a high worsening impact on health‐related quality of life (measured by the 36‐Item Short Form Health Survey, mental component summary and physical component summary scores and the Short Form 6‐Dimension utility score), work productivity and daily activities.7 The nonfatal disease burden across all chronic diseases has AD alone as being the skin disease that causes the greatest population‐level disability within the skin disease subcategories.9, 10
The current study was conducted to increase knowledge about the relationship between disease severity and burden of AD. The objective of the presented analyses was to investigate the possible relationship between patient‐reported severity of AD and self‐reported impairment of work productivity and daily activities. Impairment was measured by the Work Productivity and Activity Impairment (WPAI) – Specific Health Problem (SHP) questionnaire in adults with moderate‐to‐severe AD in Europe (France, Germany and the U.K.) and the U.S.A.
Patients and methods
This was a cross‐sectional, internet‐based, self‐reported survey investigating the burden of AD among adults with AD in France, Germany, the U.K. and the U.S.A. The survey panel participants for this survey were sourced from the larger population‐based National Health and Wellness Survey (NHWS), from which selected participants were recontacted to participate in the 35‐min online survey used in this study. The European respondents included in this study had participated in the 2016 European NHWS, and the U.S. respondents in either the 2015 or 2016 U.S. NHWS. The random, stratified sampling framework on which the NHWS is designed ensures that this survey is representative of the demographic composition of the general population.
The sample of patients with moderate‐to‐severe AD was the focus of this study, and constituted the major part of the study sample. A subgroup of people with mild AD was also included to provide some baseline context for the moderate‐to‐severe subgroup results. However, due to resource constraints, this last group was smaller as it was not the main focus of the study.
All respondents provided informed consent electronically prior to answering any survey questions. Participants were compensated for participation, and were required not to have participated in more than 12 surveys per year, to reduce the likelihood of respondent fatigue. People who were unable or unwilling to provide informed consent, or who had no internet access to complete the survey, were excluded.
The first four inclusion criteria defined the participants from NHWS who were invited to participate. They were (i) adult age; (ii) report of having experienced AD, dermatitis or eczema in the past 12 months; (iii) report that this was physician diagnosed and (iv) report of having treatment prescribed by a dermatologist, allergist or immunologist for their condition. In this study's survey, a series of additional questions was then applied as inclusion criteria to ensure a current physician diagnosis of AD, with participants seen recently by dermatologist, allergist or immunologist. The respondent needed (i) to report doctor‐diagnosed ‘atopic dermatitis or atopic eczema’ or ‘eczema or dermatitis (nonspecific)’ from among a list of dermatitis and nondermatitis conditions; (ii) to confirm that they only had the other specific dermatitis conditions specified (e.g. contact dermatitis, nummular dermatitis etc) and (iii) to indicate whether they had other specific dermatitis conditions in addition to AD.
Based on this first screening, they had (iv) again to confirm specifically that they meant AD, defined back to them as ‘atopic dermatitis, also known as atopic eczema, which typically includes itching, especially at night, and reddish patches on the skin. Raised bumps on the skin may leak fluid, and your skin may be cracked or scaly. Symptoms tend to flare (suddenly appear or worsen) periodically and then decrease’ and (v) to confirm that if they had indicated multiple dermatitis conditions, that any other condition was in fact in addition to their AD. Additionally, they should (vi) report that they had seen a dermatologist, allergist or immunologist for their AD in the last year.
Next, current status of mild, moderate or severe AD was determined using Patient‐Oriented Scoring Atopic Dermatitis (PO‐SCORAD). Severity categories were determined by the PO‐SCORAD scores (< 25 mild, 25–50 moderate, > 50 severe).11, 12, 13
Work impairment and activity impairment were assessed using the WPAI‐SHP questionnaire for AD.14 The WPAI, a validated instrument used to measure impairment in work productivity and daily activities over the past 7 days, has been validated across multiple languages including English, German and French, and includes the following items: absenteeism (percentage of time missed from work due to health in the past 7 days), presenteeism (percentage of impairment while at work due to health in the past 7 days), overall work impairment (aggregate of absenteeism and presenteeism) and activity impairment (percentage of impairment in daily activities due to health in the past 7 days). Data on absenteeism, presenteeism and overall work impairment were obtained only from employed participants, whereas activity impairment data were obtained from all participants. The SHP version of the WPAI uses the name of the health problem, in this case AD, instead of health problems in general.
Statistical analysis
For the descriptive analyses, continuous variables are presented as the number of observations (n), mean, SD and range, while categorical variables are presented as frequencies and percentages. χ2‐Tests, Cochran–Armitage trend tests or t‐tests were used to assess any statistically significant differences between groups based on their baseline characteristics.
For the adjusted statistical analysis, multivariable regression models were used to examine associations between severity of AD (as predictor) and patient‐reported work and activity impairment (dependent variables), assuming negative binomial distribution of outcomes and controlling for potential confounding. PO‐SCORAD was the main independent variable treated as a categorized variable, with mild < 25, moderate 25–50 and severe > 50, as well as the subgroups severe 1 (51–60), severe 2 (61–70) and severe 3+ (≥ 71). Country, age, sex, alcohol use, smoking, body mass index categories, household income, Charlson Comorbidity Index (CCI; used here as a summary measure of comorbidity and general health) and years since AD diagnosis were included as covariates. This list was the result of a priori inclusion of age, sex, CCI, alcohol use, smoking and body mass index categories, and evaluation of additional significant predictors resulting in this total model.
Analyses were conducted at a regional level (Europe and the U.S.A.) and for the total sample (all respondents). A statistical significance of 0·05 was adopted. All statistical analyses and data management were conducted using SAS software (version 9·4; SAS Institute Inc., Cary, NC, U.S.A.).
Results
Sample characteristics
In total, 21 852 respondents to the NHWS were invited. The total response rate was 39·7%. Among those responding to the study survey, after excluding a majority who did not meet the inclusion criteria, 1232 respondents were finally included in the analysed study sample. Excluded respondents did not meet the criteria of having physician‐diagnosed current AD and having recently (i.e. within the previous year) seen a dermatologist, allergist or immunologist. Also excluded were patients with mild AD beyond our predefined quota.
In total 1098 participants had moderate‐to‐severe AD, of whom 221 were recruited in France, 209 in Germany, 118 in the U.K. and 550 in the U.S.A. PO‐SCORAD scores ranged from 25·0 to 103·0, with a mean ± SD of 42·8 ± 13·4. Of the participants with mild AD (n = 134), 31 were recruited in France, 30 in Germany, 23 in the U.K. and 50 in the U.S.A. PO‐SCORAD scores ranged from 0·3 to 24·8, with a mean ± SD of 16·9 ± 6·2.
The sociodemographic and clinical characteristics of participants with moderate‐to‐severe AD presented by region and total population are summarized in Tables 1 and 2. The total study sample (pooled across regions and all four countries) comprised 69% female and 31% male participants, with a mean ± SD age of 48·3 ± 14·7 years. The mean ± SD age at diagnosis of AD was 30·4 ± 19·4 years. Generally, the characteristics were similar in the European (France, Germany and the U.K.) and U.S. populations.
Table 1.
Sociodemographic characteristics of participants with moderate‐to‐severe atopic dermatitis (AD), presented by region and total population
| Europea | U.S.A. | Total | P‐value | |
|---|---|---|---|---|
| n = 548 | n = 550 | n = 1098 | ||
| Age (years), mean ± SD | 45·3 ± 13·5 | 51·3 ± 15·3 | 48·3 ± 14·7 | < 0·001 |
| Sex | 0·88 | |||
| Female | 378 (69·0) | 377 (68·5) | 755 (68·8) | |
| Male | 170 (31·0) | 173 (31·5) | 343 (31·2) | |
| Age at AD diagnosis (years), mean ± SD | 27·3 ± 17·5 | 33·2 ± 20·5 | 30·4 ± 19·4 | < 0·001 |
| PO‐SCORAD total score, mean ± SD | 43·4 ± 13·7 | 42·2 ± 13·1 | 42·8 ± 13·4 | 0·16 |
| Body mass index (kg m−2) | < 0·001 | |||
| Underweight (≤ 18·4) | 37 (6·8) | 13 (2·4) | 50 (4·6) | |
| Normal weight (18·5–25) | 234 (42·7) | 166 (30·2) | 400 (36·4) | |
| Overweight (25–30) | 164 (29·9) | 169 (30·7) | 333 (30·3) | |
| Obese (≥ 30) | 105 (19·2) | 197 (35·8) | 302 (27·5) | |
| Declined to answer | 8 (1·5) | 5 (0·9) | 13 (1·2) | |
| Smoking behaviour | < 0·001 | |||
| Currently smokes | 178 (32·5) | 93 (16·9) | 271 (24·7) | |
| Formerly smoked | 156 (28·5) | 173 (31·5) | 329 (30·0) | |
| Never smoked | 214 (39·1) | 284 (51·6) | 498 (45·4) | |
| Exercise (≥ 20 min) in past months | 394 (71·9) | 400 (72·7) | 794 (72·3) | 0·76 |
| Marital status | 0·34 | |||
| Not married or living with partner | 197 (35·9) | 213 (38·7) | 410 (37·3) | |
| Never married | 131 (23·9) | 119 (21·6) | 250 (22·8) | |
| Divorced or separated | 56 (10·2) | 68 (12·4) | 124 (11·3) | |
| Widowed | 9 (1·6) | 25 (4·5) | 34 (3·1) | |
| No answer | 1 (0·2) | 1 (0·2) | 2 (0·2) | |
| Married or living with partner | 351 (64·0) | 337 (61·3) | 688 (62·7) | |
| Committed relationship but not married | 108 (19·7) | 51 (9·3) | 159 (14·5) | |
| Married | 243 (44·3) | 286 (52·0) | 529 (48·2) | |
| Employment status | < 0·001 | |||
| Employed | 367 (67·0) | 300 (54·5) | 667 (60·7) | |
| Part time (≤ 20 h per week) | 91 (16·6) | 62 (11·3) | 153 (13·9) | |
| Full time (> 20 h per week) | 276 (50·4) | 238 (43·3) | 514 (46·8) | |
| Unemployed | 181 (33·0) | 250 (45·5) | 431 (39·3) | |
| Not employed | 50 (9·1) | 51 (9·3) | 101 (9·2) | |
| Retired | 84 (15·3) | 149 (27·1) | 233 (21·2) | |
| Homemaker | 39 (7·1) | 48 (8·7) | 87 (7·9) | |
| No answer | 8 (1·5) | 2 (0·4) | 10 (0·9) |
Data are presented as n (%) unless stated otherwise. PO‐SCORAD, Patient‐Oriented Scoring Atopic Dermatitis. aFrance, Germany and the U.K.
Table 2.
Clinical characteristics of participants with moderate‐to‐severe atopic dermatitis, presented by region and total population
| Europea | U.S.A. | Total | P‐value | |
|---|---|---|---|---|
| n = 548 | n = 550 | n = 1098 | ||
| Treatment (ever)b | < 0·001 | |||
| Nonprescription only | 45 (8·2) | 20 (3·6) | 65 (5·9) | |
| TCSc | 234 (42·7) | 259 (47·1) | 493 (44·9) | |
| TCI | 25 (4·6) | 31 (5·6) | 56 (5·1) | |
| Oral or injectable CS | 108 (19·7) | 157 (28·5) | 265 (24·1) | |
| Phototherapy | 41 (7·5) | 25 (4·5) | 66 (6·0) | |
| Immunosuppressants | 90 (16·4) | 56 (10·2) | 146 (13·3) | |
| None | 5 (0·9) | 2 (0·4) | 7 (0·6) | |
| Treatment (past 12 months)b | 0·0031 | |||
| Nonprescription only | 80 (14·6) | 62 (11·3) | 142 (12·9) | |
| TCSc | 250 (45·6) | 308 (56·0) | 558 (50·8) | |
| TCI | 31 (5·7) | 27 (4·9) | 58 (5·3) | |
| Oral or injectable CS | 93 (17·0) | 101 (18·4) | 194 (17·7) | |
| Phototherapy | 20 (3·6) | 11 (2·0) | 31 (2·8) | |
| Immunosuppressants | 54 (9·9) | 32 (5·8) | 86 (7·8) | |
| None | 20 (3·6) | 9 (1·6) | 29 (2·6) |
Data are presented as n (%). CS, corticosteroids; TCI, topical calcineurin inhibitors; TCS, topical corticosteroids. aFrance, Germany and the U.K. bMultiple answers were possible; the highest level of treatment is given. cTCS as needed and/or proactively.
The sociodemographic and clinical characteristics of participants with mild, moderate and severe AD presented by severity are summarized in Table 3. The mean ± SD age across severity subcategories ranged from 45·5 ± 12·4 to 49·3 ± 13·1 years, and the mean ± SD age at diagnosis of AD ranged from 23·9 ± 17·7 to 31·0 ± 19·9 years (Table 3). Generally, the characteristics were similar in participants with mild, moderate or severe AD in the total study sample.
Table 3.
Sociodemographic and clinical characteristics of participants with mild and moderate‐to‐severe AD, presented by level of severity (total population)
| AD severity (PO‐SCORAD) | Mild (< 25) | Moderate (25–50) | Severe 1 (51–60) | Severe 2 (61–70) | Severe 3+ (≥ 71) |
|---|---|---|---|---|---|
| n = 134 | n = 825 | n = 141 | n = 83 | n = 49 | |
| Age (years), mean ± SD | 47·7 ± 17·2 | 48·5 ± 15·3 | 49·3 ± 13·1 | 46·7 ± 12·6 | 45·5 ± 12·4 |
| Country | |||||
| U.S.A. (n = 600) | 50 (37·3) | 412 (49·9) | 79 (56·0) | 37 (45) | 22 (45) |
| Europe (n = 632) | 84 (62·7) | 413 (50·0) | 62 (44·0) | 46 (55) | 27 (55) |
| France (n = 252) | 31 (23·1) | 169 (20·5) | 19 (13·5) | 24 (29) | 9 (18) |
| Germany (n = 239) | 30 (22·4) | 167 (20·2) | 24 (17·0) | 10 (12) | 8 (16) |
| U.K. (n = 141) | 23 (17·1) | 77 (9·3) | 19 (13·5) | 12 (14) | 10 (20) |
| Sex, n (%) | |||||
| Female (n = 830) | 75 (56·0) | 573 (69·5) | 90 (63·8) | 55 (66) | 37 (76) |
| Male (n = 402) | 59 (44·0) | 252 (30·5) | 51 (36·2) | 28 (34) | 12 (24) |
| Age at AD diagnosis (years), mean ± SD | 31·0 ± 19·0 | 31·0 ± 19·9 | 30·3 ± 18·1 | 28·2 ± 16·3 | 23·9 ± 17·7 |
| Population (area of residence) | |||||
| > 500 000 (major metropolitan area) (n = 205) | 17 (12·7) | 146 (17·7) | 17 (12·1) | 18 (22) | 7 (14) |
| 100 000–500 000 (urban area) (n = 221) | 19 (14·2) | 135 (16·4) | 39 (27·7) | 17 (20) | 11 (22) |
| > 100 000 (suburb of a large city) (n = 248) | 28 (20·9) | 154 (18·7) | 33 (23·4) | 17 (20) | 16 (33) |
| 30 000–100 000 (small city) (n = 203) | 19 (14·2) | 149 (18·1) | 17 (12·1) | 11 (13) | 7 (14) |
| < 30 000 (rural or small town) (n = 355) | 51 (38·1) | 241 (29·2) | 35 (24·8) | 20 (24) | 8 (16) |
| Marital status | |||||
| Not married/not living with partner (n = 452) | 42 (31·3) | 313 (37·9) | 54 (38·3) | 22 (27) | 21 (43) |
| Married/living with partner (n = 780) | 92 (68·7) | 512 (62·1) | 87 (61·7) | 61 (73) | 28 (57) |
| Employment status | |||||
| Not employed (n = 485) | 54 (40·3) | 335 (40·6) | 48 (34·0) | 25 (30) | 23 (47) |
| Employed (n = 747) | 80 (59·7) | 490 (59·4) | 93 (66) | 58 (70) | 26 (53) |
| Household income | |||||
| France, < €30 000 (n = 111) | 11 (8·2) | 78 (9·4) | 5 (3·5) | 11 (13) | 6 (12) |
| France, ≥ €30 000 (n = 126) | 19 (14·2) | 80 (9·7) | 12 (8·5) | 13 (16) | 2 (4) |
| France, no answer (n = 15) | 1 (0·7) | 11 (1·3) | 2 (1·4) | 0 (0) | 1 (2) |
| Germany, < €40 000 (n = 114) | 12 (9·0) | 87 (10·5) | 9 (6·4) | 3 (4) | 3 (6) |
| Germany, ≥ €40 000 (n = 96) | 13 (9·7) | 63 (7·6) | 15 (10·6) | 3 (4) | 2 (4) |
| Germany, no answer (n = 29) | 5 (3·7) | 17 (2·1) | 0 (0·0) | 4 (5) | 3 (6) |
| U.K., < €30 000 (n = 64) | 10 (7·5) | 35 (4·2) | 12 (8·5) | 2 (2) | 5 (10) |
| U.K., ≥ €30 000 (n = 64) | 10 (7·5) | 35 (4·2) | 5 (3·5) | 9 (11) | 5 (10) |
| U.K., no answer (n = 13) | 3 (2·2) | 7 (0·8) | 2 (1·4) | 1 (1) | 0 (0) |
| U.S.A., < €60 000 (n = 303) | 21 (15·7) | 215 (26·1) | 39 (27·7) | 19 (23) | 9 (18) |
| U.S.A., ≥ €60 000 (n = 275) | 26 (19·4) | 181 (21·9) | 39 (27·7) | 17 (20) | 12 (24) |
| U.S.A., no answer (n = 22) | 3 (0·2) | 16 (1·9) | 1 (0·7) | 1 (1) | 1 (2) |
Data are presented as n (%) unless stated otherwise. PO‐SCORAD, Patient‐Oriented Scoring Atopic Dermatitis.
Severity of atopic dermatitis and impact on work productivity
Overall, reported work productivity decreased with increasing severity of AD (PO‐SCORAD). This was observed for the total study sample (for all items, Table 4). Similar results were obtained analysing at a regional level for Europe and the U.S.A.
Table 4.
Comparison of work productivity outcomes, presented by level of severity in respondents with atopic dermatitis (AD) and regions and total population
| Outcome variable | AD severity (PO‐SCORAD) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Severe 1 | Severe 2 | Severe 3+ | |||||||
| PO‐SCORAD < 25 | PO‐SCORAD 25–50 | PO‐SCORAD > 50 | PO‐SCORAD 51–60 | PO‐SCORAD 61–70 | PO‐SCORAD 71+ | |||||||
| n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | |
| Absenteeism (%) | ||||||||||||
| Europe | 48 | 2·0 ± 9·9 | 255 | 5·1 ± 15·1 | 87 | 10·9 ± 18·6 | 43 | 7·0 ± 13·7 | 31 | 12·1 ± 19·0 | 13 | 21·1 ± 27·4 |
| U.S.A. | 22 | 2·4 ± 10·7 | 208 | 3·2 ± 12·4 | 81 | 9·7 ± 20·4 | 47 | 6·1 ± 15·7 | 23 | 16·6 ± 28·1 | 11 | 10·5 ± 17·1 |
| Total | 70 | 2·1 ± 10·1 | 463 | 4·2 ± 14·0 | 168 | 10·3 ± 19·5 | 90 | 6·5 ± 14·7 | 54 | 14·0 ± 23·2 | 24 | 16·3 ± 23·4 |
| Presenteeism (%) | ||||||||||||
| Europe | 48 | 2·9 ± 7·7 | 255 | 22·1 ± 24·2 | 87 | 43·5 ± 30·2 | 43 | 38·4 ± 28·9 | 31 | 45·8 ± 29·6 | 13 | 54·6 ± 34·3 |
| U.S.A. | 22 | 6·4 ± 12·9 | 208 | 22·0 ± 22·9 | 81 | 43·3 ± 26·7 | 47 | 41·3 ± 26·3 | 23 | 47·7 ± 28·1 | 11 | 42·7 ± 26·9 |
| Total | 70 | 4·0 ± 9·7 | 463 | 22·0 ± 23·6 | 168 | 43·4 ± 28·5 | 90 | 39·9 ± 27·4 | 54 | 46·6 ± 28·8 | 24 | 49·2 ± 31·1 |
| Overall work impairment (%) | ||||||||||||
| Europe | 48 | 4·8 ± 12·7 | 255 | 24·4 ± 27·4 | 87 | 47·6 ± 30·7 | 43 | 41·2 ± 29·4 | 31 | 51·6 ± 28·6 | 13 | 59·0 ± 36·8 |
| U.S.A. | 22 | 8·7 ± 15·9 | 208 | 23·7 ± 25·1 | 81 | 47·4 ± 28·7 | 47 | 44·1 ± 27·0 | 23 | 54·8 ± 31·5 | 11 | 46·3 ± 29·7 |
| Total | 70 | 6·0 ± 13·8 | 463 | 24·1 ± 26·4 | 168 | 47·5 ± 29·7 | 90 | 42·7 ± 28·1 | 54 | 53·0 ± 29·6 | 24 | 53·2 ± 33·6 |
| Activity impairment (%) | ||||||||||||
| Europe | 84 | 6·6 ± 12·0 | 413 | 26·3 ± 24·4 | 135 | 52·4 ± 27·4 | 62 | 44·2 ± 24·4 | 46 | 52·8 ± 24·9 | 27 | 70·4 ± 30·2 |
| U.S.A. | 50 | 12·0 ± 18·3 | 412 | 24·8 ± 24·8 | 138 | 52·5 ± 26·7 | 79 | 47·5 ± 25·1 | 37 | 54·9 ± 29·5 | 22 | 66·4 ± 22·8 |
| Total | 134 | 8·6 ± 14·8 | 825 | 25·5 ± 24·6 | 273 | 52·4 ± 27·0 | 141 | 46·0 ± 24·8 | 83 | 53·7 ± 26·9 | 49 | 68·6 ± 26·9 |
PO‐SCORAD, Patient‐Oriented Scoring Atopic Dermatitis. Europe represents France, Germany and the U.K.
Absenteeism
A comparison of work productivity outcomes by level of AD severity and by region and total population is shown in Table 4. In respondents with mild AD, assuming a 5‐day working week with 40 h per week, the past week's working hours missed due to AD (absenteeism) correspond to an average of 0·1 days per week lost in the total study sample, and the European and U.S. samples. For respondents with moderate AD this corresponds to an average of 0·2 days per week lost due to AD in the total study sample, 0·3 days per week in the European sample and 0·2 days per week in the U.S. sample.
However, the highest proportions of time lost due to AD were reported in the severe groups severe (Table 4). In the total study sample in the severe 3+ respondents this was 16·3 ± 23·4%, corresponding to 0·8 days per week; in the European sample, also in the severe 3+ respondents, it was 21·1 ± 27·4%, corresponding to 1·1 days per week; and in the U.S. sample it was in the severe 2 respondents, at 16·6 ± 28·1%, corresponding to 0·8 days per week. The proportion of lost time of 10·5 ± 17·1%, corresponding to 0·5 days per week, in the severe 3+ respondents in the U.S.A. was lower than in the U.S. severe 2 and in the Europe severe 3+ groups; however, the statistical variability is high. Taking the respondents with severe AD together in a consolidated severe group, the past week's working hours lost due to AD correspond to an average of 0·5 days per week (total study sample, Europe and the U.S.A.).
Presenteeism
For respondents with mild AD, the reported impairment while at work (presenteeism) corresponds to an average of 1·6 h per week being unproductive or ineffective due to AD while at work for the total study sample, 1·1 h per week for Europe and 2·6 h per week for the U.S.A. Impact on work productivity in respondents with moderate AD was much higher and corresponds to an average of 8·8 h per week being unproductive or ineffective due to AD while at work (total study sample: Europe and the U.S.A.). Respondents in the severe subcategories reported an impairment while at work that was, with some variation across severity subcategories, approximately twice as high as in the moderate subcategory. The highest impairment due to AD while at work was reported in the severe 3+ respondents in Europe and overall (Table 4). The proportion of presenteeism was 49·2 ± 31·1% (corresponding to 19·7 h per week) for the total study sample and 54·6 ± 34·3% (corresponding to 21·8 h per week) for Europe. In the U.S. population the highest impairment due to AD while at work was 47·7 ± 28·1% (corresponding to 19·1 h per week), seen in the severe 2 respondents.
Work impairment
Overall work impairment due to AD in respondents with mild AD (Table 4) corresponds to an average of 2·4 h (total study sample), 1·9 h (Europe) and 3·5 h (U.S.A.) per week of potential work productivity lost due to AD. For respondents with moderate AD, it corresponds to an average of 9·6 h (total study sample), 9·8 h (Europe) and 9·5 h (U.S.A.) per week of potential work productivity lost due to AD. For the total study sample and Europe, the highest overall work impairment due to AD was reported by the severe 3+ respondents: mean ± SD 53·2 ± 33·6% overall (corresponding to 21·3 h per week) and 59·0 ± 36·8% in Europe (corresponding to 23·6 h per week). In the U.S. population the highest overall work impairment due to AD was 54·8 ± 31·5% (corresponding to 21·9 h per week), in the severe 2 respondents. Overall, respondents with severe AD reported a mean ± SD overall work impairment due to AD of 47·5 ± 29·7%, corresponding to 19·0 h per week. The total study sample and European and U.S. subgroups were very similar (Table 4).
Activity impairment
The mean ± SD activity impairment among participants with mild AD was 8·6 ± 14·8% in the total study sample, 6·6 ± 12·0% for Europe and 12·0 ± 18·3% for the U.S.A. (Table 4). In participants with moderate AD it was 25·5 ± 24·6% for the total study sample, 26·3 ± 24·4% for Europe and 24·8 ± 24·8% for the U.S.A. In the total study sample respondents with the most severe AD (severe 3+) reported the highest activity impairment, at 68·6 ± 26·9%. This was similar for the European sample (70·4 ± 30·2%) and the U.S. sample (66·4 ± 22·8%) (Table 4).
Adjusted impact of atopic dermatitis
When the analysis was adjusted for confounding, the trend across the severity 1–3 categories was lost, and these were grouped together into a joint ‘severe’ category. Apart from this, the results for mild vs. moderate vs. severe were similar to the those in the unadjusted analyses (Table 5 and Figure 1).
Table 5.
Adjusted means of work productivity outcomes, presented by level of severity in respondents with atopic dermatitis (AD) and regions and total population
| AD severity (PO‐SCORAD) | |||
|---|---|---|---|
| Outcome variable | Mild | Moderate | Severe |
| PO‐SCORAD < 25 | PO‐SCORAD 25–50 | PO‐SCORAD > 50 | |
| Absenteeism | |||
| Europe (n = 316) | 0·3 (0·0–2·7) | 2·8 (0·6–13·5) | 10·8 (1·8–64·6) |
| U.S.A. (n = 256) | NA | NA | NA |
| Total (n = 572) | 2·1 (0·3–12·5) | 1·7 (0·5–6·2) | 8·6 (2·1–34·6) |
| Presenteeism | |||
| Europe (n = 316) | 1·3 (0·6–2·6) | 21·2 (12·4–36·2) | 39·6 (21·5–72·8) |
| U.S.A. (n = 255) | 2·2 (0·7–6·8) | 13·2 (6·2–27·9) | 24·6 (11·0–55·0) |
| Total (n = 571) | 2·0 (1·1–3·5) | 20·0 (13·4–29·8) | 37·4 (23·8–58·7) |
| Overall work impairment | |||
| Europe (n = 316) | 2·1 (1·0–4·4) | 28·0 (15·9–49·2) | 49·9 (26·4–94·5) |
| U.S.A. (n = 256) | 4·6 (1·5–13·7) | 12·8 (6·1–27·2) | 25·6 (11·5–57·3) |
| Total (n = 572) | 4·2 (2·4–7·3) | 22·1 (14·8–33·0) | 42·2 (26·7–66·7) |
| Activity impairment | |||
| Europe (n = 508) | 5·9 (3·9–9·1) | 34·1 (24·6–47·2) | 62·8 (42·8–92·1) |
| U.S.A. (n = 508) | 7·1 (4·0–12·6) | 15·2 (10·2–22·7) | 30·4 (19·2–48·3) |
| Total (n = 1016) | 7·6 (5·4–10·6) | 26·7 (20·9–34·0) | 51·6 (38·9–68·3) |
Data are shown as geometric means with corresponding 95% confidence intervals in brackets. The values represent the estimate of outcome at the mean of the covariates. In addition to Patient‐Oriented Scoring Atopic Dermatitis (PO‐SCORAD) categories, regressions included country, age, sex, alcohol use, smoking, body mass index category, household income, Charlson Comorbidity Index and years since AD diagnosis as predictors. NA, not available: absenteeism results could not be obtained as they could not converge. Europe represents France, Germany and the U.K.
Figure 1.
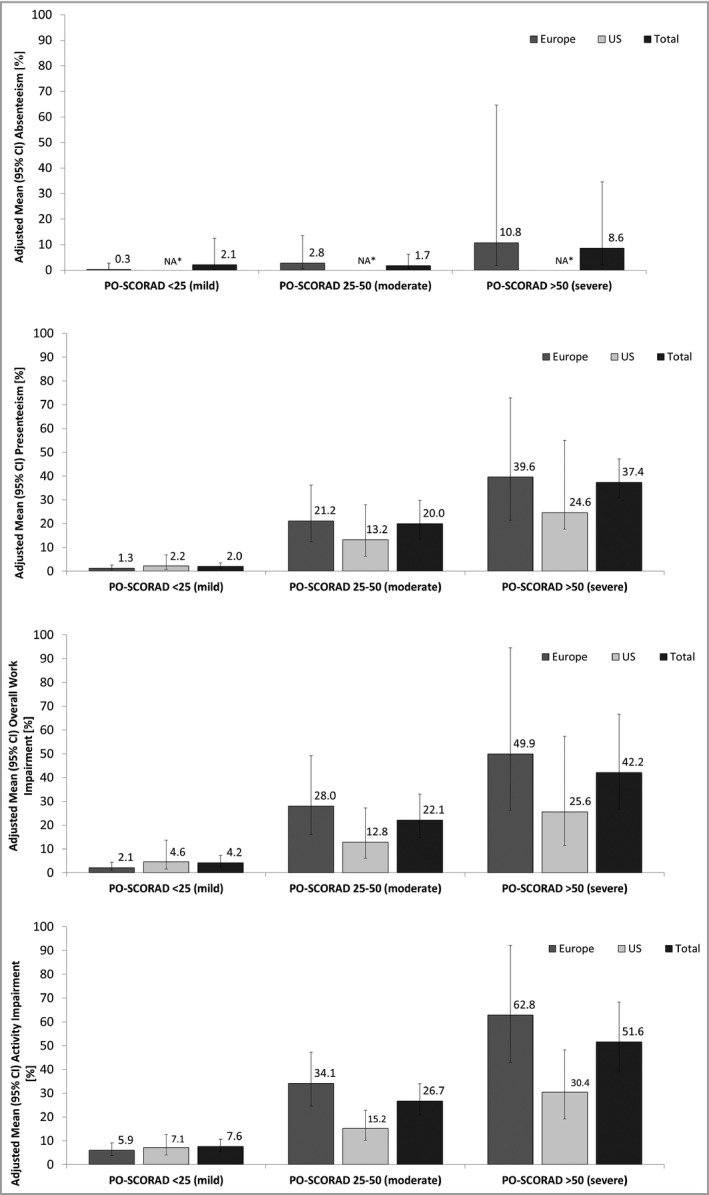
Adjusted means of work productivity outcomes, presented by level of severity in respondents with atopic dermatitis (AD) and regions and total population. The values represent the estimate of outcome at the mean of the covariates. Data are shown as geometric means, with the corresponding 95% confidence intervals (CIs) represented by whiskers. In addition to Patient‐Oriented Scoring Atopic Dermatitis (PO‐SCORAD) categories, regressions included country, age, sex, alcohol use, smoking, body mass index category, household income, Charlson Comorbidity Index and years since AD diagnosis as predictors. *NA, not available: absenteeism results could not be obtained as they could not converge. For absenteeism (data from employed respondents): Europe: n = 316, U.S.A.: n = 256, total: n = 572. For presenteeism (data from employed respondents): Europe: n = 316, U.S.A.: n = 255, total: n = 571. For overall work impairment (data from employed respondents): Europe: n = 316, U.S.A.: n = 256, total: n = 572. For activity impairment: Europe: n = 508, U.S.A.: n = 508, total: n = 1016. Europe represents France, Germany and the U.K.
The adjusted mean (95% confidence interval) impairment while at work (presenteeism) in the mild AD group was 2·0% (1·1–3·5) for the total sample, 1·3% (0·6–2·6) for Europe and 2·3% (0·7–6·8) for the U.S.A. In the moderate AD group it was much higher, with 20·0% (13·4–29·8) for the total sample, 21·2% (12·4–36·2) for Europe and 13·2% (6·2–27·9) for the U.S.A. In participants with severe AD the mean level of impairment at work was approximately twice as high as in the moderate group.
The adjusted mean (95% confidence interval) activity impairment among those with mild AD was 7·6% (5·4–10·6) for the total sample, 5·9% (3·9–9·1) for Europe and 7·1% (4·0–12·6) for the U.S.A. In participants with moderate AD it was 26·7% (20·9–34·0) for the total sample, 34·1% (24·6–47·2) for Europe and 15·2% (10·2–22·7) for the U.S.A. For respondents with severe AD, the mean level of activity impairment was approximately twice as high. Moreover, the mean level of activity impairment was approximately twice as high in respondents from the Europe than in those from the U.S.A.
Discussion
This real‐world, internet‐based, patient‐reported survey study investigated the burden of AD among a sample of adults mainly with moderate‐to‐severe AD. Participants were from Europe and the U.S.A., recruited from a survey panel sourced from the 2016 European NHWS and the 2015 or 2016 U.S. NHWS. The presented results demonstrate a significant impact of AD on work productivity. In general, higher AD severity was associated with a greater negative impact on work productivity. As expected, the work impairment was lowest in the participants with mild AD. This is in line with previous reports based on data from the 2013 U.S. NHWS, where respondents with moderate‐to‐severe AD generally showed a higher disease burden than respondents with mild AD.7, 15 This is now also shown to be consistent across regions.
We had no within‐study data on work productivity in the general population without AD, and thus we were unable to compare directly the loss of productivity in people with AD against that in the general population. However, in the U.S. NHWS studies it was shown that respondents with AD overall had higher work impairment than those without AD,7, 15 and that respondents with mild AD had higher work impairment than those without.15 Similarly, comparing the moderate with the severe AD groups, a greater negative impact was reported in our study for each WPAI item across each of the more severe AD subcategories. After adjustment for covariates, the trend across mild – moderate – severe remained strong, but the trend across severe subgroups disappeared, suggesting that once the disease reaches a certain severity level, little additional impairment occurs. It should be noted that the overall variation of the data was high.
The impact on work impairment in participants with moderate‐to‐severe AD was similar in the European and U.S. populations, and the observed unadjusted impact on work impairment in participants with moderate‐to‐severe AD was similar in the European and U.S. populations. However, activity impairment after adjusting for potential confounding was approximately twice as high in the European than in the U.S. population. A hypothesis for this observation could be the different social systems in Europe and the U.S.A., which may result in people in the U.S.A. being more concerned about losing their job and therefore being more likely to go to work even if they do not feel well.
The reported mean 2–16% of the past week's working hours missed due to AD (absenteeism) across all severity levels from mild to severe 3+ in the total study sample corresponds to an average of 0·1–0·8 days per assumed 5‐day working week lost, indicating an associated economic burden to society. This negative impact is likely to be influenced further by the 4–49% reported impairment due to AD while at work (presenteeism), which corresponds to 1·6–19·7 h per week being unproductive or ineffective while at work. However, it cannot be clearly determined whether or not an employee is truly 100% unproductive or ineffective when experiencing presenteeism.
For most severity subcategories the reported loss of work days was considerably higher than in two other studies, which reported 5·8 days in a 6‐month period and 2·7 days per year, respectively.16, 17, 18 In the European Union, the related indirect costs due to reduced performance at work and working time missed were estimated at €2 billion per year.18 However, the results of the present study are consistent with a previous report, based on data from the 2013 U.S. NHWS, concluding that lost work productivity is driven mainly by presenteeism.15 Together with the results for activity impairment, the present findings indicate an extensive negative impact of AD on peoples’ work and daily life. Overall, the results for impact on work productivity in patients with AD in the present study confirm what has previously been suggested with respect to this impact.6, 7
Compared with previous reports also using participants from the U.S. NHWS database,7, 15 this study adds data from the European NHWS, greater detail across the severe AD subgroup, and a more thorough assessment of current severity level using the PO‐SCORAD (administered in our specific survey). We also implemented a more thorough and specific definition of AD based on multiple survey questions to identify respondents with current physician diagnosis of clearly stated AD, who had been seen recently by a dermatologist, allergist or immunologist. In addition, whereas those studies used the general WPAI (measuring total activity impairment) as administered in the NHWS, this study used the disease‐specific WPAI‐SHP for AD as administered in our survey, measuring activity impairment related to the specific condition.
A limitation of this study is that the data were self‐reported. Diagnoses and other clinical variables were not verified via alternative data sources (e.g. medical records). However, the specific questionnaires used (PO‐SCORAD and WPAI) are validated instruments. Furthermore, as the design of the present study is cross‐sectional, causality cannot be directly inferred, but the alternatives of reverse causality (work impairment causing higher AD severity) or a random finding are less likely. Although potential bias always remains a possibility, the results were adjusted for multiple covariates to eliminate confounding. Additionally, although the study sample was sourced from the NHWS, which is designed to be representative of the general adult population in the U.S.A. and participating European countries, there is a risk that some subpopulations of patients with AD were under‐represented due to age, technology, willingness to participate in a follow‐up survey and/or severity‐related limitations. The sample in the current study is likely to favour younger and/or healthier adults.
In conclusion, the present study suggests an association between AD severity and work productivity among people with AD, with increasing AD severity being associated with a greater negative impact on work productivity. Reducing AD severity is expected to reduce the patient burden and thereby reduce the negative impact on work productivity. Consequently, this is also likely to reduce the economic burden of AD to society. Future research could help further to increase insights into the burden of AD and unmet treatment needs.
Acknowledgments
The authors would like to thank the survey participants with AD for their participation in this study, and Kantar Health for input into the study design and data analysis. Manuscript writing support was provided by Wiebke Griemberg, PhD and Emili Gonzalez‐Perez, PhD also from TFS Trial Form Support GmbH and by Copentown Healthcare Consulting, with financial support provided by LEO Pharma. The study was sponsored by AstraZeneca. We would like to thank Nebibe Varol from AstraZeneca for participation in the study design and conduct as a health economist.
Funding sources This study was supported by AstraZeneca and LEO Pharma.
Conflicts of interest L.A. and M.E.N. are employees of LEO Pharma; F.N. is an employee of AstraZeneca.
References
- 1. Barbarot S, Auziere S, Gadkari A et al Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy 2018; 73:1284–93. [DOI] [PubMed] [Google Scholar]
- 2. Hanifin JM, Reed ML. A population‐based survey of eczema prevalence in the United States. Dermatitis 2007; 18:82–91. [DOI] [PubMed] [Google Scholar]
- 3. Silverberg JI, Hanifin JM. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population‐based study. J Allergy Clin Immunol 2013; 132:1132–8. [DOI] [PubMed] [Google Scholar]
- 4. Silverberg JI, Garg NK, Paller AS et al Sleep disturbances in adults with eczema are associated with impaired overall health: a US population‐based study. J Invest Dermatol 2015; 135:56–66. [DOI] [PubMed] [Google Scholar]
- 5. Harrop J, Chinn S, Verlato G et al Eczema, atopy and allergen exposure in adults: a population‐based study. Clin Exp Allergy 2007; 37:526–35. [DOI] [PubMed] [Google Scholar]
- 6. DaVeiga SP. Epidemiology of atopic dermatitis: a review. Allergy Asthma Proc 2012; 33:227–34. [DOI] [PubMed] [Google Scholar]
- 7. Eckert L, Gupta S, Amand C et al Impact of atopic dermatitis on health‐related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol 2017; 77:274–9. [DOI] [PubMed] [Google Scholar]
- 8. Simpson EL, Bieber T, Eckert L et al Patient burden of moderate to severe atopic dermatitis (AD): insights from a phase 2b clinical trial of dupilumab in adults. J Am Acad Dermatol 2016; 74:491–8. [DOI] [PubMed] [Google Scholar]
- 9. Hay RJ, Johns NE, Williams HC et al The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol 2014; 134:1527–34. [DOI] [PubMed] [Google Scholar]
- 10. Karimkhani C, Boyers LN, Prescott L et al Global burden of skin disease as reflected in Cochrane Database of Systematic Reviews. JAMA Dermatol 2014; 150:945–51. [DOI] [PubMed] [Google Scholar]
- 11. Oranje AP. Practical issues on interpretation of Scoring Atopic Dermatitis: SCORAD index, objective SCORAD, patient‐oriented SCORAD and Three‐Item Severity score. Curr Probl Dermatol 2011; 41:149–55. [DOI] [PubMed] [Google Scholar]
- 12. Stalder J‐F, Barbarot S, Wollenberg A et al Patient‐Oriented SCORAD (PO‐SCORAD): a new self‐assessment scale in atopic dermatitis validated in Europe. Allergy 2011; 66:1114–21. [DOI] [PubMed] [Google Scholar]
- 13. Severity scoring of atopic dermatitis: the SCORAD index . Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology 1993; 186:23–31. [DOI] [PubMed] [Google Scholar]
- 14. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993; 4:353–65. [DOI] [PubMed] [Google Scholar]
- 15. Whiteley J, Emir B, Seitzman R, Makinson G. The burden of atopic dermatitis in US adults: results from the 2013 National Health and Wellness Survey. Curr Med Res Opin 2016; 32:1645–51. [DOI] [PubMed] [Google Scholar]
- 16. Holm EA, Esmann S, Jemec GBE. The handicap caused by atopic dermatitis – sick leave and job avoidance. J Eur Acad Dermatol Venereol 2006; 20:255–9. [DOI] [PubMed] [Google Scholar]
- 17. Torrelo A, Ortiz J, Alomar A et al Atopic dermatitis: impact on quality of life and patients’ attitudes toward its management. Eur J Dermatol 2012; 22:97–105. [DOI] [PubMed] [Google Scholar]
- 18. Zuberbier T, Orlow SJ, Paller AS et al Patient perspectives on the management of atopic dermatitis. J Allergy Clin Immunol 2006; 118:226–32. [DOI] [PubMed] [Google Scholar]


