Abstract
Aim
To assess the relationship of malnutrition risk and in‐hospital falls in a patient group of older hospitalized patients (65–79 and ≥80 years).
Methods
A cross‐sectional, multicenter, point‐prevalence study was conducted in 68 Austrian hospitals with 3702 hospitalized older patients. The relationship between malnutrition risk and falls was analyzed using univariate and multivariate binary logistic regression analyses. Data were analyzed separately for two age groups, patients were aged 65–79 years (n = 2320) and ≥80 years (n = 1382).
Results
Prevalence of hospital‐acquired falls was 5.2%, and prevalence of risk of malnutrition was 24.3% (Malnutrition Universal Screening Tool) and 16.2% (definition using body mass index and weight loss). The univariate analysis showed significant associations of malnutrition risk and in‐hospital falls for patients aged ≥80 years (odds ratio 2.1; 95% confidence interval 1.2–3.6) but not for patients aged 65–79 years. The multivariate logistic regression analysis did not show significant associations between malnutrition risk and hospital‐acquired falls.
Conclusions
The results of this study show that malnutrition risk is a predictor for in‐hospital falls in very old patients (≥80 years). In this patient group, the screening and assessment of nutritional status as well as nutritional interventions for the prevention/treatment of malnutrition risk should be considered as one important factor for successful fall prevention. Studies are necessary to assess the effect of nutritional interventions as part of a multifaceted fall‐prevention program. Geriatr Gerontol Int 2020; 20: 348–353.
Keywords: association, falls, malnutrition, predictor, prevention
Introduction
Falls are common in older adults and represent a major threat to the sense of independence and health of older persons.1 A recently published study shows that about 28% of hospitalized patients report that they had fallen during the last 12 months, and about 15% of these patients experienced a fall in hospital.2 More than half of the falls lead to fall‐related injuries,3, 4 >20% of the falls in older adults require a hospital visit,4 and falls even represent a major cause of death among very old persons.5 Fall‐related injuries can have a considerable negative impact on the patients' quality of life1 and studies have confirmed high costs related to fall events and consequences, ranging from about 2000 to 26 000 USD per fallen person.6
Commonly mentioned risk factors for in‐hospital falls, for example, are having a positive fall history, fear of falling, agitated confusion, urinary incontinence, psychotropic medication or instability while walking.7, 8 Walking difficulties in older adults are strongly related to muscle strength impairment, and several studies have shown that sarcopenia, which is defined as loss of muscle mass, strength and function, increases the risk of falls and fractures.9 Sarcopenia is related to malnutrition, as many malnourished patients are concurrently sarcopenic.10 These facts strongly suggest that malnutrition may be a predictor for in‐hospital falls.
However, previous studies and systematic reviews that have summarized the risk factors for in‐hospital falls and falls in general rarely mention malnutrition.3, 7, 11 Some authors examined the association of malnutrition and falls in the community setting12 or in long‐term care institutions,13 but the predictive value of malnutrition or malnutrition risk on hospital‐acquired falls is still unclear.
Therefore, the aim of this study was to assess the relationship of malnutrition risk and in‐hospital falls in a patient group of older hospitalized patients (≥65 years). The research questions asked were:
Is the presence of malnutrition risk a predictor for in‐hospital falls in older patients?
Is there a difference among the predictors of in‐hospital falls in older patients aged 65–79 and very old patients ≥80 years?
Methods
Design, participants and ethical considerations
This is a secondary data analysis of cross‐sectional, multicenter, point‐prevalence studies conducted during 2017 and 2018. All Austrian hospitals with >50 beds were invited to participate in the study, either with all or some of the wards in the respective hospitals. Participation in the study was voluntary. All patients who were admitted on the day of measurement (November 14, 2017 and November 13, 2018) were informed about the study and asked to participate. If they agreed, they received detailed information about the study, and they had to provide written informed consent. If the patient was not able to provide informed consent, the legal representatives were asked to decide whether the patient should participate in the study. The ethics committee for each participating hospital approved the study (20–192 ex 08/09), and the study was conducted in accordance with the Code of Ethics issued by the World Medical Association and the Declaration of Helsinki.
Data collection
Each hospital nominated a coordinator who was responsible for the measurements. Furthermore, each participating ward appointed one person that organized the measurements on the respective ward. The coordinators and persons responsible at the ward level received training from members of the research team. Data were collected by two persons: one who was familiar to the patients and one who worked on another ward to ensure objectivity. Data were collected by questioning the patients and accessing relevant data in the patient records. All data was entered into a specifically programmed, password‐protected data entry program with online security (https://at.lpz-um.eu/).
A standardized questionnaire was used to collect data on fall incidence and potential predictors of in‐hospital falls, such as demographic characteristics, medical diagnoses, care dependency, use of psychotropic drugs, pain prevalence, incontinence and the patients' fall and malnutrition risk levels.2, 14 The patients' medical diagnoses were assessed by referring to the International Classification of Diseases (ICD‐10). A fall was defined as an event that resulted in the person coming to rest inadvertently on the ground or floor or other lower level.15 To evaluate the fall incidence, the persons responsible for the study on the participating wards documented all falls that had occurred during the 30 days before the measurement. They also documented whether the most severe fall in the institution had caused physical injuries to the patient and, if so, indicated the severity of the injury or injuries. A risk of falling was considered present if the patient had experienced at least one fall during the last 12 months.
The Care Dependency Scale (CDS) was used to assess the care dependency of the patients.16 The capabilities of patients were assessed on a five‐point Likert scale, ranging from completely dependent to completely independent. The lower the total score, the more care‐dependent the patients are. The CDS shows good validity and reliability in older hospitalized patients.16
To assess whether the patients were at risk of malnutrition, two methods were applied: the Malnutrition Universal Screening Tool (MUST)17 and a malnutrition definition. The MUST is a valid tool that is very easy to use and requires about 3–5 min to complete.18 The malnutrition definition included the body mass index (BMI) and unintentional weight loss; in particular, unintentional weight loss was considered >10% body weight over the previous 6 months or >5% body weight during the previous month with or without a BMI <18.5 kg/m2 in patients <65 years and <20 kg/m2 for patients ≥65 years.19
Data analysis
We analyzed the data using SPSS version 25 (IBM Corp., Armonk, NY, USA). For this study, we analyzed data collected from patients aged ≥65 years. Two persons performed the data cleaning and deleted invalid values (e.g., BMI >60). Patient characteristics were analyzed using descriptive statistics. The χ2 and Student's t‐test were used to show differences between the age groups as well as between fallers and non‐fallers. The association between malnutrition risk, other patient characteristics and hospital‐acquired falls was calculated using univariate and multivariate binary logistic regression analyses. Experiencing a fall in the hospital (yes/no) was used as the dependent variable. Fallers and non‐fallers were compared based on the following variables: gender, age, number of medical diagnoses, CDS scale, different diagnoses (dementia, diseases of the nervous system, diseases of the spinal cord, diseases of the musculoskeletal system and connective tissue, diseases of the eye, stroke), use of psychotropic medication, pain during the last 7 days, incontinence, BMI, risk of malnutrition according to MUST and risk of malnutrition according to the definition, including BMI and weight loss. The significance level was set at P < 0.05. Variables that differed significantly between fallers and non‐fallers in the univariate logistic regression analysis were included in the multivariate binary logistic regression analysis.
Results
Sample characteristics
In total, 68 Austrian hospitals participated in the study and 8637 hospitalized patients were asked to participate in the measurement during 2017 and 2018; 6271 patients accepted the invitation. Of those patients, 3702 were ≥65 years, 2320 were aged 65–79 years and 1382 were aged ≥80 years. The most frequently indicated reasons for non‐participation were refusal (42.2%), cognitive impairment (16.8%), unavailability during the measurement (12.3%) or insufficient understanding of the German language (10.9%). Most of the patients were admitted to a surgical or internal ward (see Fig. 1).
Figure 1.
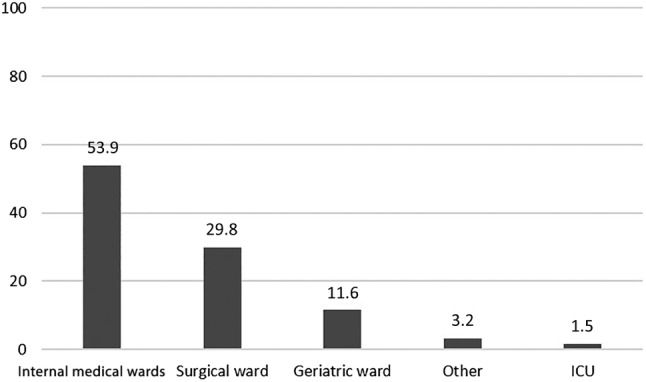
Percentage of patients admitted to the different types of wards on the day of measurement.
The mean age of the patients was 77.6 years, and more than half were female (Table 1). In total, 54% were completely independent from care, whereas 4.1% were completely care dependent and 8.5% were to a great extent care dependent. More detailed patient characteristics are shown in Table 1.
Table 1.
Characteristics and differences between patients 65–79 and ≥80 years†
| Characteristics | Total (n = 3702) | Patients 65–79 years old (n = 2320) | Patients ≥80 years (n = 1382) | P‐value |
|---|---|---|---|---|
| Female | 2026 (54.7) | 1171 (50.5) | 855 (61.9) | 0.000 |
| Age, years | 77.6 ± 7.6 | 72.76 ± 4.3 | 85.6 ± 4.3 | 0.000 |
| Number of ICD‐10 diagnosis | 3.2 ± 1.8 | 3.1 ± 1.7 | 3.5 ± 1.9 | 0.000 |
| Patients completely dependent from care (CDS score ≤24) | 153 (4.1) | 69 (3.0) | 84 (6.1) | 0.000 |
| Patients completely independent from care (CDS score >69) | 2000 (54.0) | 1461 (63) | 539 (39.0) |
0.000 |
| CDS sum score | 63.8 ± 15.2 | 66.5 ± 13.5 | 59.4 ± 16.7 | 0.000 |
| BMI, kg/m2 | 26.2 ± 5.2 | 26.8 ± 5.5 | 25.3 ± 4.6 | 0.000 |
| Patients with a fall during last 30 days in hospital | 193 (5.2) | 110 (4.7) | 83 (6.0) | 0.094 |
| Fallers with a fall injury | 81 (2.2%) | 42 (1.8) | 39 (2.8) | 0.220 |
| Patients with a risk of falling | 1165 (31.6) | 621 (26.8) | 544 (39.5) | 0.000 |
| Use of psychotropic drugs | 1317 (35.9) | 767 (33.2) | 550 (40.4) | 0.000 |
| Patients with malnutrition risk, MUST | 793 (24.3) | 524 (25.2) | 269 (22.7) | 0.107 |
| Patients with malnutrition risk due to BMI and weight loss | 541 (16.2) | 343 (16.1) | 198 (16.3) | 0.895 |
| Most frequent ICD‐10 diagnoses | ||||
| Circulatory diseases | 2273 (61.4) | 1295 (55.8) | 978 (70.8) | 0.000 |
| Musculoskeletal diseases | 1096 (29.6) | 511 (26.3) | 485 (35.1) | 0.000 |
| Genitourinary diseases | 999 (27.0) | 555 (23.9) | 444 (32.1) | 0.000 |
| Respiratory diseases | 937 (25.3) | 602 (25.9) | 335 (24.2) | 0.248 |
| Digestive diseases | 900 (24.3) | 551 (23.8) | 349 (25.3) | 0.302 |
BMI, body mass index; CDS, Care Dependency Scale; MUST, Malnutrition Universal Screening Tool.
†Values presented are n (%) for categorical data and mean (± SD) for metric data, according to the distribution.
Prevalence of falls, fall‐related injuries and malnutrition risk
The overall prevalence of falls within the 30 days before the measurement in the hospital was 5.2% (n = 193). The highest prevalence rate of hospital‐acquired falls was observed in geriatric wards (8.4%, 36) followed by internal medicine wards (6.2%, 124). The prevalence of the risk of falling, defined by the rate that a fall had been experienced within the last 12 months, was 31.6% (n = 1165) in the total sample and significantly higher in patients ≥80 years (39.5%, 544). The fall experienced in the hospital caused physical injuries to the patient in 42.0% (n = 81) of the cases. Of these injuries, 67.9% were minor injuries that did not need medical interventions, such as bruises or abrasion. The injuries were moderate in 18.5% of the cases, including injuries such as contusions, cuts that needed stitching and abrasions that required wound care, while 13.6% were severe injuries, such as serious head injuries or fractures.
According to the MUST, 24.3% of the patients were at risk of malnutrition and according to the definition using the BMI and weight loss, 16.2% were at risk of malnutrition. The prevalence of the malnutrition risk did not significantly differ between old and very old patients (Table 1).
Predictors for in‐hospital falls
In patients ≥80 years a risk of malnutrition using the definition with the BMI and weight loss as well as a low BMI were significantly associated with falls during the hospital stay. Table 2 presents the association of potential predictors with hospital‐acquired falls using univariate analysis.
Table 2.
Predictors for hospital‐acquired falls in patients aged 65–79 and ≥80 years, analyzed with univariate analysis (χ2 tests and Mann–Whitney U‐tests)†
| Patients 65–79 years old (n = 2320) | Patients ≥80 years old(n = 1382) | |||||
|---|---|---|---|---|---|---|
| Fallers | Non‐fallers | P‐value | Fallers | Non‐fallers | P‐value | |
| Risk of malnutrition, BMI and weight loss | 19 (20.4) | 324 (16.0) | 0.251 | 20 (28.2) | 178 (15.6) | 0.005 |
| Risk of malnutrition, MUST | 29 (31.9) | 495 (24.9) | 0.137 | 19 (27.5) | 250 (22.4) | 0.325 |
| BMI | 26.1 ± 4.8 | 26.8 ± 5.5 | 0.254 | 24.0 ± 4.3 | 25.3 ± 4.6 | 0.016 |
| Female | 50 (45.5) | 1121 (50.7) | 0.281 | 49 (59.0) | 806 (62.0) | 0.584 |
| Dementia | 9 (8.2) | 60 (2.7) | 0.001 | 20 (24.1) | 122 (9.4) | 0.000 |
| Disease of the nervous system | 20 (18.2) | 274 (12.4) | 0.075 | 19 (22.9) | 165 (12.7) | 0.008 |
| Disease of the spinal cord | 1 (0.9) | 10 (0.5) | 0.496 | 0 (0.0) | 6 (0.5) | 0.535 |
| Disease of the eye | 8 (7.3) | 130 (5.9) | 0.547 | 10 (12.0) | 157 (12.1) | 0.992 |
| Stroke | 23 (20.9) | 178 (8.1) | <0.001 | 16 (19.3) | 120 (9.2) | 0.003 |
| Musculoskeletal disease | 31 (28.2) | 580 (26.2) | 0.653 | 30 (36.1) | 455 (35.0) | 0.836 |
| Use of psychotropic drugs | 66 (60.0) | 701 (31.8) | <0.001 | 54 (65.9) | 496 (38.8) | 0.000 |
| Pain in the last 7 days | 64 (58.2) | 1330 (60.2) | 0.647 | 48 (57.8) | 766 (59.0) | 0.838 |
| Incontinence | 31 (28.2) | 439 (19.9) | 0.034 | 35 (42.2) | 506 (39.0) | 0.561 |
| Number of medical diagnosis | 3.9 ± 2.0 | 3.0 ± 1.7 | <0.001 | 3.9 ± 1.7 | 3.5 ± 1.9 | 0.036 |
| CDS sum score | 60.2 ± 15.0 | 66.7 ± 13.4 | <0.001 | 54.3 ± 15.3 | 59.7 ± 16.67 | 0.000 |
BMI, body mass index; CDS, Care Dependency Scale; MUST, Malnutrition Universal Screening Tool.
†Values presented are n (%) for categorical data and mean ± SD for metric data.
The results of the univariate logistic regression analysis did not show significant associations between hospital‐acquired falls and malnutrition risk for patients aged 65–79 years according to MUST or the definition including the BMI and weight loss. The analysis showed associations of hospital‐acquired falls with the presence of dementia, stroke, incontinence, use of psychotropic drugs, incontinence, number of medical diagnoses and care dependency (Table 3).
Table 3.
Predictors of hospital‐acquired falls in patients aged 65–79 and ≥80 years, analyzed with univariate and multivariate binary regression analyses
| Patients 65–79 years old (n = 2320) | ||||||
|---|---|---|---|---|---|---|
| Univariate linear regression | Multivariate linear regression | |||||
| OR | 95% CI | P‐value | OR | 95% CI | P‐value | |
| Dementia | 3.2 | 1.5–6.6 | 0.002 | 1.4 | 0.6–3.2 | 0.400 |
| Stroke | 3.0 | 1.9–4.9 | 0.000 | 2.2 | 1.3–3.7 | 0.002 |
| Use of psychotropic drugs | 3.2 | 2.2–4.7 | 0.000 | 2.6 | 1.8–4.0 | 0.000 |
| Incontinence | 1.6 | 1.0–2.4 | 0.036 | 0.8 | 0.5–1.4 | 0.500 |
| Number of medical diagnoses | 1.3 | 1.2–1.4 | 0.000 | 1.2 | 1.1–1.3 | 0.007 |
| CDS sum score | 0.9 | 0.964–0.985 | 0.000 | 0.9 | 0.9–1.0 | 0.067 |
| Patients ≥80 years (n = 1382) | ||||||
|---|---|---|---|---|---|---|
| Univariate linear regression | Multivariate linear regression | |||||
| OR | 95% CI | P‐value | OR | 95% CI | P‐value | |
| Risk of malnutrition, definition with BMI and weight loss | 2.1 | 1.2–3.6 | 0.006 | 1.6 | 0.84–3.21 | 0.150 |
| BMI | 0.9 | 0.88–0.98 | 0.012 | 0.98 | 0.92–1.04 | 0.510 |
| Dementia | 3.1 | 1.8–5.2 | 0.000 | 1.8 | 0.9–3.7 | 0.103 |
| Disease of the nervous system | 2.0 | 1.2–3.5 | 0.009 | 2.0 | 1.1–3.6 | 0.026 |
| Stroke | 2.3 | 1.3–4.2 | 0.004 | 1.7 | 0.85–3.41 | 0.131 |
| Use of psychotropic drugs | 3.0 | 1.9–4.9 | 0.000 | 2.2 | 1.3–3.7 | 0.004 |
| Number of medical diagnosis | 1.1 | 1.0–1.2 | 0.091 | 1.0 | 0.87–1.16 | 0.902 |
| CDS sum score | 0.9 | 0.97–0.99 | 0.005 | 1.0 | 0.97–1.0 | 0.360 |
BMI, body mass index; CI, confidence interval; CDS, Care Dependency Scale; OR, odds ratio.
The results of the univariate analysis showed significant associations of in‐hospital falls and malnutrition risk for patients aged ≥80 years according to the definition using the BMI and weight loss (P < 0.01). Further significant associations were found for lower BMI, presence of dementia, diseases of the nervous system, stroke, use of psychotropic drugs, number of medical diagnoses and higher care dependency (see Table 3).
The results of the multivariate logistic regression analysis did not show significant associations between malnutrition risk and hospital‐acquired falls. The final model of the multivariate regression analysis for the 65–79‐year age group revealed previous stroke (odds ratio [OR] 2.2, 95% confidence interval [CI] 1.3–3.7), use of psychotropic drugs (OR 2.6, 95% CI 1.8–4.0) and number of medical diagnoses (OR 1.2, 95% CI 1.1–1.3) as the strongest predictors for in‐hospital falls. The strongest predictors for in‐hospital falls among patients aged ≥80 years in the final multivariate regression model were the presence of a disease of the nervous system (OR 2, 95% CI 1.1–3.6) and the use of psychotropic drugs (OR 2.2, 95% CI 1.3–3.7) (Table 3).
Discussion
In our sample, we found significant differences between fallers and non‐fallers in terms of the risk of malnutrition, BMI, degree of care dependency, number of diagnoses, presence of incontinence, use of psychotropic drugs and some diseases, such as dementia or stroke. Malnutrition risk was identified as a predictor for hospital‐acquired falls in the univariate analysis among very old patients, but not for patients in the 65–79‐year age group. This means that hospitalized patients who are aged ≥80 years and at risk of malnutrition have a two‐fold higher chance of experiencing a fall during their hospital stay than older hospitalized patients who are not at risk of malnutrition. Hence, the results of our study provide evidence that an impaired nutritional status is not only associated with falls in the community12 or falls in the nursing home20 but also in the hospital. Our results also showed that a low BMI was significantly associated with hospital‐acquired falls in very old patients. In our sample, these associations were not found in patients aged 65–79 years.
The strength of the association between malnutrition risk and falls may be affected by several confounding factors that correlate with the occurrence of both malnutrition and falls. It is important to consider these factors in a multivariate analysis, which is underlined by the discrepancy of the results of the univariate and multivariate regression analyses in the current study.
Physical function, such as the balance function, muscle strength, muscle power or muscle mass, is one of the most important factors influencing the occurrence of falls in older adults, which we did not assess in this study.21 Ramsey et al. showed an association of malnutrition and physical performance by means of dynamic measures such as the timed up and go test or chair stand test. This indicates that the nutritional status of older adults is more likely to be affected by muscle power than by muscle strength.22
In clinical practice, multifaceted interventions for fall prevention in older persons should be individualized to address the individual patient's risks.23 If a person is at risk of malnutrition, it may be beneficial to include nutritional interventions such as energy and protein supplementation or dietary counseling in the prevention program for the respective patient. If a vitamin D deficiency or osteoporosis is diagnosed, supplementation with vitamin D and calcium should be considered. The relevance of vitamin D supplementation in fall and injury prevention is currently the subject of controversy in the scientific community, but the benefit of (moderate) vitamin D supplementation has been demonstrated in several recently published, randomized, controlled trials.24, 25
Recent studies in which the effectiveness of fall prevention programs was assessed, revealed that interventions that cover multiple components are the most promising for preventing falls.26 This is not surprising, as falls are a geriatric syndrome, and the causes for these are mostly multifactorial. The advantage of multifaceted interventions has also been reported in guidelines for fall prevention in older adults.27, 28, 29 However, the administration of vitamin D is mentioned in some of the guidelines, but nutrition in general and the maintenance of a good nutritional status is usually not included in the recommendations.27, 29
The best practice guideline published by the Registered Nurses' Association of Ontario includes recommendations for dietary intervention in fall prevention,28 i.e., to optimize bone health in adults at risk for falls or fall injuries, and particularly those at risk for fractures. A recommendation is also made to refer the persons to dietitians so they can receive advice and individualized nutritional interventions. However, nutritional interventions are not only important to optimize bone health but also for muscle strength and physical function, as several studies have shown.30 Nutritional interventions should be additionally carried out to provide exercise, environmental adjustments and education for patients and staff. These are fundamental interventions for fall prevention and should be recommended in several guidelines.
In conclusion, the results of this study show that malnutrition risk is a predictor for in‐hospital falls in very old patients (≥80). Knowledge of this relationship is important for planning adequate interventions to prevent hospital‐acquired falls. In this patient group, the screening and assessment of nutritional status as well as nutritional interventions for the prevention/treatment of malnutrition risk should be considered as one important factor for successful fall prevention. Referrals to nutrition experts such as dietitians so patients can receive advice and individualized interventions should be considered. High‐quality studies are necessary to assess the effect of nutritional interventions as part of a multifaceted fall‐prevention program. We recommend that researchers conduct pragmatic clinical trials in the future in real‐world settings, individualizing the interventions to the patients' risk factors and needs.
Strengths and limitations
This was a cross‐sectional study that included data collected at two time points. Therefore, the analyses of the data‐generated information on associations between different risk factors rather than causalities of these. Participation in the study was voluntary and required the informed consent of the patients. This may have led to a selection bias in that patients with a very poor health status may have been more likely to refuse to participate in the study. Furthermore, >18% of the patients did not participate because of cognitive impairment. These patients are at particularly high risk of experiencing a fall or being malnourished; therefore, because these patients may not have participated in the study, the prevalence rates may be underestimated. The independent variables for the regression analysis were chosen based on the literature, but some other important variables may have been missed. However, we conducted the analysis using a rather large sample of older hospitalized patients and used standardized questionnaires and a standardized data collection procedure. The distinction made between old (65–79 years) and very old (≥80) patients allowed a deeper understanding of different risk factors for the different subgroups of fallers in the hospital setting to be obtained.
Disclosure statement
The authors declare no conflict of interest.
Eglseer D, Hoedl M, Schoberer D. Malnutrition risk and hospital‐acquired falls in older adults: A cross‐sectional, multicenter study. Geriatr. Gerontol. Int. 2020;20:348–353. 10.1111/ggi.13885
References
- 1. Hartholt KA, van Beeck EF, Polinder S et al Societal consequences of falls in the older population: injuries, healthcare costs, and long‐term reduced quality of life. J Trauma 2011; 71: 748–753. [DOI] [PubMed] [Google Scholar]
- 2. Eglseer D, Hodl M, Lohrmann C. Six nursing care problems in hospitals: a cross‐sectional study of quality of care. J Nurs Care Qual 2019; 34(1): E8–E14. 10.1097/NCQ.0000000000000307. [DOI] [PubMed] [Google Scholar]
- 3. Gazibara T, Kurtagic I, Kisic‐Tepavcevic D et al Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics 2017; 17: 215–223. [DOI] [PubMed] [Google Scholar]
- 4. Milat AJ, Watson WL, Monger C, Barr M, Giffin M, Reid M. Prevalence, circumstances and consequences of falls among community‐dwelling older people: results of the 2009 NSW falls prevention baseline survey. N S W Public Health Bull 2011; 22: 43–48. [DOI] [PubMed] [Google Scholar]
- 5. Alamgir H, Muazzam S, Nasrullah M. Unintentional falls mortality among elderly in the United States: time for action. Injury 2012; 43: 2065–2071. [DOI] [PubMed] [Google Scholar]
- 6. Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH. Cost of falls in old age: a systematic review. Osteoporos Int 2010; 21: 891–902. [DOI] [PubMed] [Google Scholar]
- 7. Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in‐patients: a systematic review. Age Ageing 2004; 33: 122–130. [DOI] [PubMed] [Google Scholar]
- 8. Dhargave P, Sendhilkumar R. Prevalence of risk factors for falls among elderly people living in long‐term care homes. J Clin Gerontol Geriatr 2016; 7: 99–103. [Google Scholar]
- 9. Schaap LA, van Schoor NM, Lips P, Visser M. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the longitudinal aging study Amsterdam. J Gerontol A Biol Sci Med Sci 2018; 73: 1199–1204. [DOI] [PubMed] [Google Scholar]
- 10. Eglseer D, Eminovic S, Lohrmann C. Association between sarcopenia and nutritional status in older adults: a systematic literature review. J Gerontol Nurs 2016; 42: 33–41. [DOI] [PubMed] [Google Scholar]
- 11. Deandrea S, Bravi F, Turati F, Lucenteforte E, La Vecchia C, Negri E. Risk factors for falls in older people in nursing homes and hospitals. A systematic review and meta‐analysis. Arch Gerontol Geriatr 2013; 56: 407–415. [DOI] [PubMed] [Google Scholar]
- 12. Trevisan C, Crippa A, Ek S et al Nutritional status, body mass index, and the risk of falls in community‐dwelling older adults: a systematic review and meta‐analysis. J Am Med Dir Assoc 2019; 20: 569‐82.e7. [DOI] [PubMed] [Google Scholar]
- 13. Meijers JM, Halfens RJ, Neyens JC, Luiking YC, Verlaan G, Schols JM. Predicting falls in elderly receiving home care: the role of malnutrition and impaired mobility. J Nutr Health Aging 2012; 16: 654–658. [DOI] [PubMed] [Google Scholar]
- 14. van Nie‐Visser NC, Schols JM, Meesterberends E, Lohrmann C, Meijers JM, Halfens RJ. An international prevalence measurement of care problems: study protocol. J Adv Nurs 2013; 69: e18–e29. [DOI] [PubMed] [Google Scholar]
- 15. Group KIW . The prevention of falls in later life. A report of the Kellogg international work group on the prevention of falls by the elderly. Dan Med Bull 1987; 34 (Suppl 4): 1–24. [PubMed] [Google Scholar]
- 16. Lohrmann C, Dijkstra A, Dassen T. The care dependency scale: an assessment instrument for elderly patients in German hospitals. Geriatr Nurs 2003; 24: 40–43. [DOI] [PubMed] [Google Scholar]
- 17. Elia M. Screening for Malnutrition: a Multidisciplinary Responsibility. Development and Use of the Malnutrition Universal Screening Tool (MUST) for Adults. Wallingford, England: Malnutrition Advisory Group (MAG), a Standing Committee of BAPEN, 2003. [Google Scholar]
- 18. Stratton RJ, Hackston A, Longmore D et al Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr 2004; 92: 799–808. [DOI] [PubMed] [Google Scholar]
- 19. Lohrmann C. Nursing Quality Measurement 2.0. Graz: Medical University Graz, 2018. [Google Scholar]
- 20. Neyens J, Halfens R, Spreeuwenberg M et al Malnutrition is associated with an increased risk of falls and impaired activity in elderly patients in Dutch residential long‐term care (LTC): a cross‐sectional study. Arch Gerontol Geriatr 2013; 56: 265–269. [DOI] [PubMed] [Google Scholar]
- 21. Van Ancum JM, Pijnappels M, Jonkman NH et al Muscle mass and muscle strength are associated with pre‐ and post‐hospitalization falls in older male inpatients: a longitudinal cohort study. BMC Geriatr 2018; 18: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ramsey KA, Meskers CGM, Trappenburg MC et al Malnutrition is associated with dynamic physical performance. Aging Clin Exp Res 2019. 10.1007/s40520-019-01295-3. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rimland JM, Abraha I, Dell'Aquila G et al Effectiveness of non‐pharmacological interventions to prevent falls in older people: a systematic overview. The SENATOR project ONTOP series. PLoS One 2016; 11: e0161579–e0161579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Uusi‐Rasi K, Patil R, Karinkanta S et al A 2‐year follow‐up after a 2‐year RCT with vitamin D and exercise: effects on falls, injurious falls and physical functioning among older women. J Gerontol A Biol Sci Med Sci 2017; 72: 1239–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smith LM, Gallagher JC, Suiter C. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. J Steroid Biochem Mol Biol 2017; 173: 317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cameron ID, Dyer SM, Panagoda CE et al Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018; 9: CD005465–CD005465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. NICE NIfHaCE . Falls in Older People: Assessing Risk and Prevention. National Institute for Health and Care Excellence (NICE); 2013. https://www.nice.org.uk/guidance/cg161/resources/falls-in-older-people-assessing-risk-and-prevention-pdf-35109686728645. [PubMed] [Google Scholar]
- 28. Ontario RNo . Preventing Falls and Reducing Injury from Falls, 3rd edn. Toronto: Registered Nurses' Association of Ontario; 2017. [Google Scholar]
- 29. Schoberer D, Findling E, Breimaier H et al Evidence‐Based Guideline. Fall Prevention for Older People in Hospitals and Nursing Homes. Graz: Medical University Graz, 2018. [Google Scholar]
- 30. Cruz‐Jentoft AJ, Landi F, Schneider SM et al Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS). Age Ageing 2014; 43: 748–759. [DOI] [PMC free article] [PubMed] [Google Scholar]


