Abstract
Aims
To test the efficacy of a therapist‐guided high‐intensity internet intervention compared with an unguided low‐intensity internet intervention among individuals with alcohol use disorder.
Design
A three‐group randomized controlled trial with follow‐up assessments post‐treatment (12 weeks) and 6 months post‐randomization (primary end‐point).
Settings
General population sample in Sweden.
Participants
A total of 166 on‐line self‐referred adults (49% males) with a score of 14 (females)/16 (males) or more on the Alcohol Use Disorders Identification Test, a preceding week alcohol consumption of 11 (females)/14 (males) or more standard drinks and an alcohol use disorder according to a diagnostic interview.
Interventions and comparators
Both the high‐ (n = 72) and low‐intensity internet interventions (n = 71) consisted of modules based on relapse prevention. Controls were on a waiting‐list (n = 23), and were only followed until the post‐treatment follow‐up. Participants were randomized at a 7 : 7 : 2 ratio.
Measurements
Primary outcome was self‐reported alcohol consumption in the preceding week measured as (1) number of standard drinks and (2) number of heavy drinking days at the 6‐month follow‐up.
Findings
Alcohol use disorders were largely in the severe category (74.7%), with the majority of participants having had alcohol problems for more than 5 years. Attrition was 13 and 22% at the post‐treatment and 6‐month follow‐up, respectively. At the 6‐month follow‐up, an intent‐to‐treat analysis showed no significant differences in alcohol consumption between the high‐ and low‐intensity interventions [standard drinks d = −0.17, 95% confidence interval (CI) = −0.50 to 0.16; heavy drinking days: d = −0.07, 95% CI = −0.40 to 0.26]. Prevalence of negative effects was somewhat low (8–14%) in both intervention groups, as was deterioration (3–5%).
Conclusions
At 6‐month follow‐up, there were no significant differences between a therapist‐guided high‐intensity internet intervention and an unguided low‐intensity internet intervention in reducing alcohol consumption among individuals with an alcohol use disorder.
Keywords: Alcohol, alcohol use disorder, internet intervention, randomized controlled trial, treatment; cognitive behavior therapy, cognitive behavior therapy
Introduction
Individuals with alcohol use disorders (AUD) 1 account for a substantial part of the global disease burden caused by alcohol 2, but fewer than 20% seek help within regular services 3. Reasons for this vary. People may doubt that treatment will be effective, may think that they should be able to deal with the problem on their own and/or may deny having a problem altogether 4. Importantly, AUD is severely stigmatized 5, provoking more social rejection and negative emotions than other psychiatric conditions 6. Internet interventions have been heralded as a way to attract some of those who hesitate seeking help within regular services. Aside from the obvious advantages of radically increasing access and eliminating geographical barriers, these interventions could hypothetically circumvent the stigma associated with physically visiting a clinic 7.
Internet interventions can be conceptualized in two main ways: public health‐oriented low‐intensity internet interventions (LIII) characterized by brief treatment content and minimal or no therapist contact, and clinically oriented high‐intensity internet interventions (HIII) characterized by extensive treatment content akin to bibliotherapy and guidance by an active therapist 8. The central argument for the low‐intensity concept has been its potential to radically increase treatment accessibility to the public at a small cost, while the main argument for the high‐intensity concept has been increase of patient access to manual‐based therapy while minimizing therapist time. Although internet interventions targeting alcohol problems are not new 9, most have been LIII, typically single‐module ‘brief interventions’ 10 aimed at undiagnosed individuals with hazardous, rather than severe, drinking problems 11. HIII have been extensively studied for depression and anxiety, and with meta‐analyses showing no differences in outcome between these interventions and face‐to‐face therapy 12 these interventions have been successfully implemented within psychiatric care in several countries 13. However, studies investigating HIII for people with alcohol problems, especially among those with levels of severity similar to the population seen in clinics (i.e. individuals with AUD), are rare 11. Two studies on alcohol problems directly compared a cognitive–behavioral therapy (CBT) internet program with and without therapist guidance 14, 15. In both, groups receiving therapist guidance reported significantly lower alcohol consumption at varying follow‐ups compared to the group not receiving therapist guidance, with small and medium differential effect sizes respectively. In a third study, a CBT internet program with therapist guidance was compared to a waiting‐list, rendering large between‐group effect sizes 16. An important limitation of these studies is the absence of interview‐based diagnostic assessments, hampering generalizations to the AUD population 11. Another limitation is that none of the studies investigated negative effects, a critical but neglected component when evaluating internet interventions 17.
We conducted a randomized controlled trial among individuals with AUD to compare the effects of a HIII compared with a LIII and a waiting‐list (WL). We hypothesized that:
participants in HIII would have reduced their alcohol consumption more than participants in LIII at a 6‐month follow‐up (primary end‐point); and
participants in HIII and LIII would have reduced their alcohol consumption more than participants in WL at post‐treatment (treatment response).
A secondary aim was to evaluate negative effects of the internet interventions.
Methods
Design
We conducted a parallel, three‐group randomized, controlled trial with recruitment ongoing between January 2016 and February 2017 with follow‐ups at post‐treatment and 6 months post‐randomization. Participants were randomized without stratification by an independent third party, using an on‐line tool with a random number generator function (http://www.randomizer.org). A waiting‐list was added to contrast the two intervention groups. The effective randomization ratio was 7 : 7 : 2. Participants randomized to either of the interventions were blinded and were not informed about study hypotheses. The trial was prospectively registered (https://clinicaltrials.gov/ct2/show/NCT02645721). The Regional Ethics Vetting Board in Stockholm approved the trial (2015/2014–31; amendment 2016/295–32). All participants provided informed consent.
Participants
Inclusion criteria were being aged ≥ 18 years, having a score of ≥ 14 (females)/ ≥ 16 (males) on the Alcohol Use Disorders Identification Test (AUDIT) 18, a preceding week consumption of ≥ 11 (females)/≥ 14 (males) standard drinks of alcohol and an AUD, defined as two or more positive DSM‐5 criteria for AUD. Exclusion criteria were insufficient skills in Swedish language, reading/writing difficulties, concurrent psychological treatment, severe depression, acute suicidal ideation, illicit drug use problems and severe psychiatric comorbidity. Participants were recruited throughout Sweden through Google Adwords, Facebook and the Remente smartphone application (app). Interested individuals could register on the study website and complete an on‐line screening. Those potentially eligible underwent a structured psychiatric telephone interview with a clinical psychologist (69% of the interviews) or a clinical psychology master's level student under supervision from a clinical psychologist. All interviewers had undergone basic training in structured diagnostic interviewing. To establish an AUD diagnosis, the Structured Clinical Interview for DSM‐IV axis I disorders (SCID‐I) was used 19, adapted to DSM‐5 criteria. Comorbid psychiatric disorders were assessed with the Mini International Neuropsychiatric Interview (MINI) 20. Figure 1 shows participant flow throughout the trial.
Figure 1.
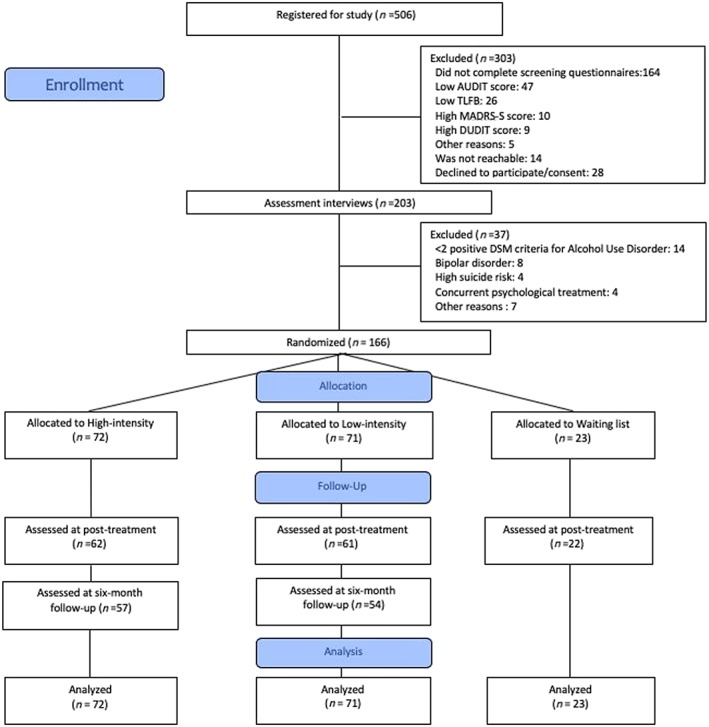
Study flow diagram. TLFB = time‐line follow‐back; AUDIT = Alcohol Use Disorders Identification Test; MADRS‐S = Montgomery–Åsberg Depression Rating Scale – Self‐report; DUDIT = Drug Use Disorders Identification Test [Colour figure can be viewed at http://wileyonlinelibrary.com]
Interventions
Both interventions were based on a CBT model of alcohol problems and delivered over 12 weeks. The platform was hosted on a server with encrypted traffic and authentication login function to guarantee participant confidentiality.
High‐intensity internet intervention
In the HIII, the ePlus program was used (see Supporting information, Appendix S7). This program has been previously evaluated in a pilot trial 21, and is intended for use alongside approximately 15 minutes of therapist guidance per week via written messages. It consists of 13 modules with three to four pages of text and a video clip reflecting the theme. All participants had contact with a therapist using a secure built‐in message system. Participants were notified via SMS when they had a new message from the therapist. For each module, participants were instructed to complete homework assignments on work‐sheets, after which the therapist granted access to the next module. Therapists logged in two to three times a week to provide feedback on and encourage participants’ work. Of the 10 therapists, six were clinical psychologists treating 75% of the participants and four were clinical psychology students at master's level, with basic clinical training and experience of providing therapy in milder cases. There was no randomization of participants at the therapist level. Clinical issues were discussed as needed with the senior author, a licensed clinical psychologist and psychotherapist. To ensure treatment integrity and adherence to protocol, the first author monitored messages sent by therapists, and provided weekly or biweekly supervision to therapists.
Low‐intensity internet intervention
In the LIII, the eChange program was used (see Supporting information, Appendix S6). This program has been evaluated in several trials 14, 15 and consists of nine modules and one to two pages of text; in this trial, an extra summary module was added to more accurately conform to the length of the ePlus program. Participants were instructed to complete homework assignments, and were consecutively granted access to new modules each week. Participants were notified via text messages when new modules were accessible on the intervention platform, but there was no therapist guidance or other contact with the research team. During weeks 8–11 participants received no new modules, but weekly text messages reminded participants to log in.
Participants in the WL condition had no contact with the research team during their waiting period except being requested to complete primary outcomes every 4 weeks, for which they received text reminders. Directly after the 12‐week waiting period, participants were offered the ePlus program with a choice of proactive, reactive or no therapist guidance.
Measures
Baseline measures
At screening, participants responded to a number of demographic and clinically relevant questions.
Outcome measures
All participants completed outcome measures five times: at screening (all outcome measures), before treatment initiation (primary outcome only), at 4 and 8 weeks during treatment (primary outcome only) and after treatment; i.e. at 12 weeks (all outcome measures). In addition, the two intervention groups completed all outcome measures again at 6 months post‐randomization (primary end‐point).
Primary outcome
At all assessment points, participants were asked about number of standard drinks (12 g of ethanol) consumed during each of the preceding 7 days according to the time‐line follow‐back method 22. Two primary outcomes were considered: (1) total number of drinks and (2) number of heavy drinking days (HDD), defined as ≥ 5 (men) or ≥ 4 (women) standard drinks on a single day.
Secondary outcomes
Three alcohol‐related questionnaires were used: the AUDIT 18 to assess changes in alcohol problems, the Alcohol Abstinence Self Efficacy Scale (AASES) 23 to assess changes in self‐efficacy and the Penn Alcohol Craving Scale (PACS) 24 to assess changes in cravings. The Montgomery–Åsberg Depression Rating Scale–self‐report (MADRS‐S) 25 was used to assess changes in depression, the Generalized Anxiety Disorder Scale (GAD‐7) was used to assess changes in anxiety 26 and Euroqol‐5D (EQ‐5D) 27 was used to assess changes in quality of life. The Drug Use Disorders Identification Test (DUDIT) 28 was used to assess illicit substance use.
Treatment credibility, treatment satisfaction and other forms of help
The Treatment Credibility Scale (TCS) 29 was administered once during the third week of the intervention, and the Client Satisfaction Scale‐8 (CSQ‐8) 30 was administered post‐treatment, complemented with other evaluation questions. In addition, questions about whether participants had recently accessed any other forms of help for alcohol problems were administered at both follow‐ups.
Negative effects
Negative effects were assessed halfway through treatment and immediately post‐treatment with the question: ‘During the treatment, have you encountered any unwanted event that you feel was a result of the treatment or experienced any undesired effect of the treatment?’. Participants were then asked to describe the event/effect. Deterioration, defined as having a higher alcohol consumption (standard drinks/HDD) post‐treatment compared to screening, was also calculated.
Analyses
The study was powered to detect a medium differential effect size in terms of standard drinks between intervention groups (Cohen's d = 0.5). Power calculations were based on results from previous trials of HIII 21 and LIII 15. A sample size of 72 per group was deemed required for 80% power with a two‐sided 5% significance level. A large differential effect size was expected between HIII and the waiting‐list, and for this reason a small waiting‐list (≤ 25) was considered sufficient. All participants randomized were included in the outcome analysis according to intention‐to‐treat principles. Missing data were deemed missing at random with Little's MCAR test (P = 0.263). Multiple imputation with five imputed data sets (SPSS) was performed to manage missing data. Generalized estimating equations (GEE) with an unstructured working correlation matrix and a 3 (intervention) × 5 (pre‐treatment, mid‐treatment 1, mid‐treatment 2, post‐treatment, 6‐month follow‐up) design was used to assess intervention effects on primary outcomes with the screening measure included as a covariate. To evaluate effects on secondary outcomes, a 3 (intervention) × 3 (screening, post‐treatment, 6‐month follow‐up) was used. For primary outcomes, a negative binomial model with log‐link was used 31, while a normal model was used for secondary outcomes. Planned two‐sided contrast tests were used to test between‐group differences. Analyses were performed using SPSS version 24 (IBM Corp., Armonk, NY, USA). In addition, Bayes factors (B) were calculated to assess strength of evidence of primary outcomes (drinks and HDD). A B of 3 or more indicates evidence for the alternative hypothesis (H1) over the null hypothesis (H0); a B below 1/3 indicates evidence for H0 over H1, while B between 1/3 and 3 indicates insensitive data. BH[0, standard deviation (SD)] refers to a Bayes factor in which the predictions of H1 are modeled as a half‐normal distribution with a peak at 0 (indicating no effect) and an SD equal to the expected effect size 32. As with our power calculation, we expected a Cohen's d of 0.5 for our Bayes factor calculation when comparing HIII and LIII, suggesting a difference of 6.1 in number of drinks and 0.75 in number of HDD. Thus, we modeled H1 as a half‐normal with an SD of 6.1 and 0.75, respectively. Further, we used 0.8 as expected Cohen's d effect size when comparing HIII and WL, modeling H1 as half‐normal with an SD of 10.0 (drinks) and 1.12 (HDD), and a Cohen's d of 0.3 when comparing LIII and WL, modeling H1 as half‐normal with an SD of 3.9 (drinks) and 0.43 (HDD). To assess all Bayes factors, we used an on‐line calculator 33.
Results
Mean participant age was 52.9 years (SD = 10.7), and 49% were male. Seventy‐five per cent of participants had a severe AUD and 44% had a psychiatric comorbidity. There were no significant differences between groups on baseline characteristics (see Table 1). At post‐treatment and at 6‐month follow‐up attrition was 13 and 22%, respectively, with no significant differences between the three groups at post‐treatment (χ2 = 1.67, P = 0.45) or between the two groups at 6‐month follow‐up (χ2 = 0.26, P = 0.61). Four participants (one in HIII and three in LIII) did not complete pre‐treatment measures, and subsequently made no attempts to access the treatment.
Table 1.
Baseline descriptive and clinical characteristics.
| High‐intensity (n = 72) | Low‐intensity (n = 71) | Waitlist (n = 23) | Total (n = 166) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | P | |
| Age (years) | 51.9 | 11.5 | 53.7 | 10.7 | 54.1 | 8.4 | 52.9 | 10.7 | 0.671 | 0.513 |
| Standard drinks | 34.2 | 17.3 | 33.8 | 16.4 | 32.0 | 15.9 | 33.8 | 16.7 | 0.156 | 0.856 |
| Heavy drinking days | 4.00 | 1.94 | 3.99 | 2.12 | 3.35 | 1.94 | 3.90 | 2.02 | 1.013 | 0.365 |
| AUDIT | 23.2 | 5.1 | 23.9 | 4.9 | 22.1 | 4.5 | 23.3 | 4.9 | 1.217 | 0.299 |
| Self‐efficacy | 2.31 | 0.66 | 2.40 | 0.73 | 2.61 | 0.47 | 2.39 | 0.67 | 1.792 | 0.170 |
| Craving | 17.2 | 4.7 | 17.9 | 5.2 | 15.3 | 5.0 | 17.2 | 5.0 | 2.423 | 0.092 |
| Depression | 17.2 | 6.6 | 15.9 | 7.3 | 16.4 | 7.3 | 16.5 | 7.0 | 0.631 | 0.534 |
| Anxiety | 6.97 | 4.17 | 6.86 | 4.96 | 6.13 | 3.76 | 6.81 | 4.46 | 0.316 | 0.729 |
| Quality of life | 0.50 | 0.32 | 0.51 | 0.38 | 0.60 | 0.28 | 0.52 | 0.34 | 0.855 | 0.427 |
| Quality of life scale 1–100 | 59.9 | 17.2 | 63.7 | 19.7 | 63.7 | 17.6 | 62.0 | 18.3 | 0.794 | 0.454 |
| n | % | n | % | n | % | n | % | χb | P | |
| Male | 32 | 44.4 | 35 | 49.3 | 14 | 60.9 | 81 | 48.8 | 1.895 | 0.388 |
| Highest educational level | ||||||||||
| University | 44 | 61.1 | 38 | 53.5 | 12 | 52.2 | 94 | 56.6 | 2.184 | 0.702 |
| High school | 24 | 33.3 | 26 | 36.6 | 10 | 43.5 | 60 | 36.1 | ||
| Basic education | 4 | 5.6 | 7 | 9.9 | 1 | 4.3 | 12 | 7.2 | ||
| Marital status | ||||||||||
| Married/partner | 50 | 69.4 | 53 | 74.6 | 19 | 82.6 | 122 | 73.5 | 3.211 | 0.523 |
| Divorced/widowed | 8 | 11.1 | 10 | 14.1 | 2 | 8.7 | 20 | 12.0 | ||
| Single | 14 | 19.4 | 8 | 11.3 | 2 | 8.7 | 24 | 14.5 | ||
| Occupational statusa | ||||||||||
| 100% | 47 | 65.3 | 40 | 56.3 | 14 | 60.9 | 101 | 60.8 | 4.285 | 0.831 |
| 75% | 6 | 8.3 | 4 | 5.6 | 2 | 8.7 | 12 | 7.2 | ||
| 50% | 3 | 4.2 | 7 | 9.9 | 1 | 4.3 | 11 | 6.6 | ||
| 25% | 5 | 6.9 | 6 | 8.5 | 3 | 13.0 | 14 | 8.4 | ||
| 0% | 11 | 15.3 | 14 | 19.7 | 3 | 13.0 | 28 | 16.9 | ||
| Self‐perceived economic situationb | ||||||||||
| Very good | 12 | 16.7 | 15 | 21.1 | 3 | 13.0 | 30 | 18.1 | 4.915 | 0.767 |
| Good | 31 | 43.1 | 34 | 47.9 | 9 | 39.1 | 74 | 44.6 | ||
| Neither good nor bad | 18 | 25.0 | 15 | 21.1 | 3 | 21.7 | 38 | 22.9 | ||
| Bad | 10 | 13.9 | 6 | 8.5 | 5 | 21.7 | 21 | 12.7 | ||
| Very bad | 1 | 1.4 | 1 | 1.4 | 1 | 4.3 | 3 | 1.8 | ||
| Years with alcohol problemsc | ||||||||||
| Less than 1 year | 1 | 1.4 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 8.086 | 0.425 |
| 1–2 years | 11 | 15.3 | 11 | 15.5 | 1 | 4.3 | 23 | 13.9 | ||
| 3–5 years | 20 | 27.8 | 16 | 22.5 | 8 | 34.8 | 44 | 26.5 | ||
| 6–10 years | 20 | 27.8 | 13 | 18.3 | 5 | 21.7 | 38 | 22.9 | ||
| More than 10 years | 20 | 27.8 | 31 | 43.7 | 9 | 39.1 | 60 | 36.1 | ||
| Previously sought alcohol treatment (yes) | 28 | 38.9 | 29 | 40.8 | 12 | 52.2 | 69 | 41.6 | ||
| Alcoholics Anonymous | 4 | 6.1 | 7 | 10.4 | 5 | 23.8 | 16 | 9.6 | 1.293 | 0.524 |
| Psychotherapy | 7 | 10.6 | 10 | 14.9 | 5 | 23.8 | 22 | 13.3 | ||
| Pharmacological treatment | 16 | 24.2 | 13 | 19.4 | 7 | 33.3 | 36 | 21.7 | ||
| Alcohol use disorders (SCID‐IV)d | ||||||||||
| Mild alcohol use disorder | 4 | 5.6 | 9 | 12.9 | 0 | 0.0 | 13 | 7.8 | 6.145 | 0.189 |
| Moderate alcohol use disorder | 15 | 20.8 | 10 | 14.3 | 3 | 13.0 | 28 | 16.9 | ||
| Severe alcohol use disorder | 53 | 73.6 | 51 | 72.9 | 20 | 87.0 | 124 | 74.7 | ||
| Any psychiatric comorbidity (MINI) | 30 | 41.7 | 31 | 44.3 | 12 | 52.2 | 73 | 44.2 | 0.780 | 0.677 |
| Depression | 19 | 26.4 | 14 | 20.0 | 9 | 39.1 | 42 | 25.5 | 3.398 | 0.183 |
| Agoraphobia | 9 | 12.5 | 10 | 14.3 | 3 | 13.0 | 22 | 13.3 | 0.100 | 0.951 |
| Generalized anxiety disorder | 6 | 8.3 | 7 | 10.0 | 4 | 17.4 | 17 | 10.3 | 1.560 | 0.458 |
| Social phobia | 5 | 6.9 | 6 | 8.6 | 3 | 13.0 | 14 | 8.5 | 0.836 | 0.658 |
| Other | 4 | 5.6 | 9 | 12.7 | 1 | 4.3 | 14 | 8.4 | 2.924 | 0.232 |
Occupational status = ‘To what degree are you presently occupied with work, studies or self‐employed?’
Self‐perceived economic situation = ‘How would you describe your current economic situation?’
Years with alcohol problems = ‘For about how long would you say that you have had alcohol problems?’
Diagnostic interview information (SCID and MINI) collected from one participant in the low‐intensity group was lost. Thus, diagnostic information about the low‐intensity group only consists of 70 participants. AUDIT: = Alcohol Use Disorders Identification Test; SCID = Structured Clinical Interview for DSM‐IV axis I disorders; MINI = Mini International Neuropsychiatric Interview.
Adherence, treatment credibility and therapist–participant interaction
At post‐treatment, participants in HIII had completed 8.4 (SD = 3.9; 64.6%) of 13 module work‐sheets, while participants in LIII had completed 5.9 (SD = 2.8; 65.5%) of nine module work‐sheets. There were no significant differences between groups in credibility ratings during the third week of intervention (HIII = 34.2; LIII = 33.5; t = 0.01, P = 0.617). The average number of messages sent from therapists to participants in HIII was 15.4 (SD = 6.8). The corresponding number of messages sent from participants to therapists was 13.1 (SD = 8.3). Therapists in HIII spent 13.5 (SD = 8.1) minutes a week per participant.
Primary outcomes
To control for chance imbalances on demographic and clinical characteristics in the three conditions, we tentatively added each characteristic as a covariate to the treatment model. None of these were significant and none were thus added in the final model (see Supporting information, Appendix S1).
At the 6‐month follow‐up, there were no significant differences between HIII and LIII either in number of standard drinks [HIII = 16.6 versus LIII = 14.5, t (141) = 0.986, P = 0.326, d = −0.17, 95% CI: −0.50 − 0.16, BH(0, 6.1) = 0.16] or in number of HDD [HIII = 1.77 versus LIII = 1.66, t (141) = 0.419, P = 0.676, d = −0.07, 95% CI: −0.40 − 0.26, BH(0, 0.75) = 0.23] (see Table 2). At the post‐treatment follow‐up, participants in HIII had a significantly greater reduction compared to WL both in number of standard drinks [HIII = 10.9 versus WL = 20.6, t (93) = 3.209, P = 0.002; d = 0.78, BH(0, 10.0) = 67.86] and in number of HDD per week [HIII = 1.22 versus WL = 2.51, t (93) = 3.867, P = 0.0002; d = 0.92, BH(0, 1.12) = 456.16] and so did participants in LIII [drinks: LIII = 14.4 versus WL = 20.6, t (92) = 2.012, P = 0.047; d = 0.48, BH(0, 3.9) = 4.00], HDD: (LIII = 1.69 versus WL = 2.51, t (92) = 2.334, P = 0.022; d = 0.57, BH(0, 0.43) = 7.47]. There was no significant difference between HIII and LIII in number of standard drinks [HIII = 10.9 versus LIII = 14.4, t (141) = 1.704, P = 0.091, d = 0.29, BH(0, 6.1) = 2.14], but participants in HIII had significantly fewer HDD than participants in LIII [HIII = 1.22 versus LIII = 1.69, t (141) = 2.003, P = 0.047; d = 0.34, BH(0, 0.75) = 3.62] ,2
Table 2.
Primary and secondary outcomes across time × group.
| High‐intensity | Low‐intensity | Wait list | Cohen's d | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | HIII versus LIII | HIII versus WL | LIII versus WL | |
| Standard drinks | |||||||||
| Pre‐treatment | 22.3 | 1.4 | 22.9 | 1.6 | 22.6 | 2.9 | |||
| Mid‐treatment 1 | 16.6 | 1.5 | 17.3 | 1.4 | 27.0 | 3.1 | |||
| Mid‐treatment 2 | 13.1 | 1.3 | 15.9 | 1.5 | 26.5 | 2.8 | |||
| Post‐treatment | 10.9 | 1.4 | 14.4 | 1.5 | 20.6 | 2.7 | 0.29 | 0.78* | 0.48* |
| 6‐month follow‐up | 16.6 | 1.5 | 14.5 | 1.5 | NA | NA | 0.17 | – | – |
| Heavy drinking days | |||||||||
| Pre‐treatment | 2.57 | 0.14 | 2.51 | 0.19 | 2.43 | 0.32 | |||
| Mid‐treatment 1 | 1.81 | 0.17 | 1.98 | 0.18 | 2.94 | 0.36 | |||
| Mid‐treatment 2 | 1.59 | 0.17 | 1.79 | 0.19 | 3.17 | 0.36 | |||
| Post‐treatment | 1.22 | 0.16 | 1.69 | 0.17 | 2.51 | 0.30 | 0.34* | 0.92** | 0.57* |
| 6‐month follow‐up | 1.77 | 0.17 | 1.66 | 0.19 | NA | NA | 0.07 | – | – |
| AUDIT | |||||||||
| Post‐treatment | 15.3 | 0.8 | 16.5 | 0.9 | 18.6 | 1.2 | 0.17 | 0.51* | 0.32 |
| 6‐month follow‐up | 15.5 | 0.9 | 14.4 | 1.0 | NA | NA | 0.14 | – | – |
| Self‐efficacy (AASES) | |||||||||
| Post‐treatment | 3.06 | 0.10 | 3.12 | 0.11 | 2.96 | 0.19 | 0.07 | 0.12 | 0.17 |
| 6‐month follow‐up | 3.15 | 0.11 | 3.34 | 0.11 | NA | NA | 0.20 | – | – |
| Craving (PACS) | |||||||||
| Post‐treatment | 10.8 | 0.7 | 11.5 | 0.8 | 11.8 | 1.3 | 0.11 | 0.17 | 0.05 |
| 6‐month follow‐up | 11.2 | 0.7 | 10.3 | 0.8 | NA | NA | 0.14 | – | – |
| Depression (MADRS) | |||||||||
| Post‐treatment | 9.2 | 0.9 | 9.6 | 0.9 | 13.2 | 1.7 | 0.05 | 0.49* | 0.45 |
| 6‐month follow‐up | 10.5 | 1.0 | 9.8 | 0.9 | NA | NA | 0.09 | – | – |
| Anxiety (GAD‐7) | |||||||||
| Post‐treatment | 4.53 | 0.45 | 4.14 | 0.52 | 5.47 | 0.89 |
0.09 |
0.23 |
0.31 |
| 6‐month follow‐up | 4.67 | 0.60 | 3.95 | 0.50 | NA | NA | 0.16 | – | – |
| Quality of life (EQ 5D) | |||||||||
| Post‐treatment | 0.60 | 0.04 | 0.64 | 0.05 | 0.53 | 0.07 | 0.09 | 0.21 | 0.28 |
| 6‐month follow‐up | 0.56 | 0.05 | 0.65 | 0.05 | NA | NA | 0.20 | – | – |
| Quality of life scale (EQ 5D‐VAS) | |||||||||
| Post‐treatment | 68.1 | 2.0 | 73.6 | 2.0 | 69.9 | 2.7 | 0.37 | 0.12 | 0.25 |
| 6‐month follow‐up | 66.9 | 2.2 | 72.4 | 2.1 | NA | NA | 0.30 | – | – |
HIII = high‐intensity internet intervention, LIII = low‐intensity internet intervention; WL = waiting‐list; AUDIT = Alcohol Use Disorders Identification Test; MADRS = Montgomery–Åsberg Depression Rating Scale; GAD‐7 = Generalized Anxiety Disorder Scale; PACS = Penn Alcohol Craving Scale; AASES = Alcohol Abstinence Self Efficacy Scale; NA = not available; SE = standard error.
≤ 0.05,
≤ 0.01.
As we noted a sharp decrease in alcohol consumption between screening and pre‐treatment, we assessed these within‐group changes; they were significant for all three groups (P = ≤ 0.01). Measures of alcohol consumption before, during and after treatment in the three groups are shown in Fig. 2.
Figure 2.
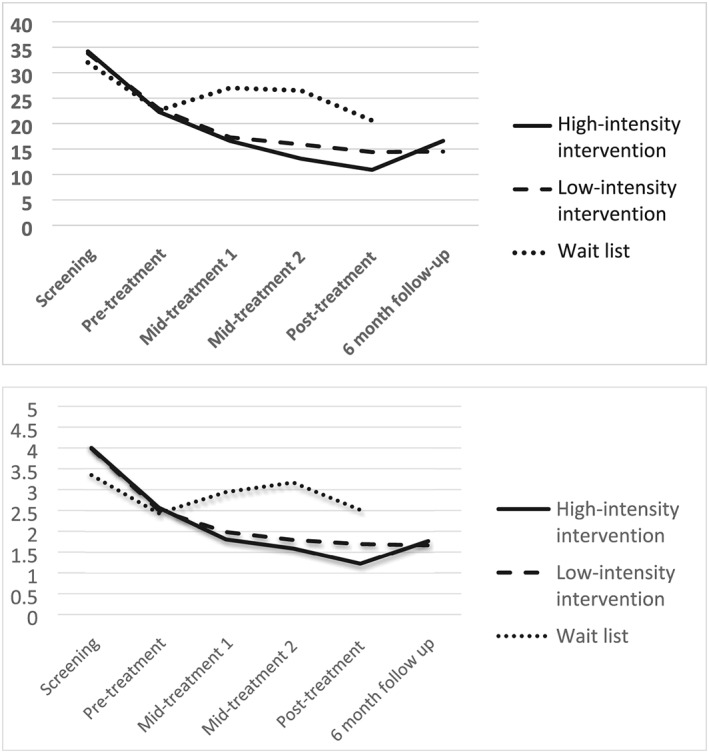
Number of standard drinks consumed (panel 1) and number of heavy drinking days (panel 2) during preceding calendar week before, during, after treatment and at 6‐month follow‐up
We explored AUD severity, psychiatric comorbidity and having accessed other forms of help as predictors of alcohol outcomes. None of these factors affected outcomes significantly (see Supporting information, Appendices S2–S4).
Secondary outcomes
At post‐treatment, participants in HIII had reduced their AUDIT and MADRS‐S scores significantly compared to WL (AUDIT: HIII = 15.3 versus WL = 18.6, t (93) = 2.249, P = 0.027; d = 0.51; MADRS‐S: HIII 9.2 versus WL = 13.2, t (93) = 2.06, P = 0.042; d = 0.49), but there was no significant difference between HIII and LIII or between LIII and WL in these two measures or in any other measures. At 6‐month follow‐up, there were no significant differences between intervention groups. At post‐treatment, three participants, two in HIII and one in LIII, had positive DUDIT scores, with total scores of ≤ 6. At 6‐month follow‐up, six participants, five in HIII and one in LIII, had DUDIT scores over 0 (range = 19).
Treatment satisfaction and other forms of help
Participants in HIII were significantly more satisfied than participants in LIII according to their CSQ‐8 total score (HIII = 24.8 versus LIII = 22.0, t (121) = 3.51, P = 0.001), see Table 3. Participants were also asked additional questions; see Supporting information, Appendix S5.
Table 3.
Client satisfaction questionnaire.
| High‐intensity n = 63 | Low‐intensity n = 60 | ||||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | χ2 | P | ||
| 1. How would you rate the quality of the service you received? | Good/excellent | 51 | 80.9 | 33 | 55.0 | 9.559 | 0.002 |
| 2. Did you get the kind of service that you wanted? | Yes, generally/yes, definitely | 44 | 69.8 | 28 | 46.7 | 6.800 | 0.009 |
| 3. To what extent has our program met your needs? | All/most of my needs have been met | 43 | 68.3 | 39 | 65.0 | 0.146 | 0.702 |
| 4. If a friend were in need of similar help, would you recommend our program to him/her? | Yes, generally/yes, definitely | 57 | 90.4 | 48 | 80.0 | 2.700 | 0.100 |
| 5. How satisfied are you with the amount of help that you received? | Mostly/very satisfied | 59 | 93.7 | 43 | 71.7 | 10.490 | 0.001 |
| 6. Have the services you received helped you to deal more effectively with your problems? | Yes, they helped somewhat/a great deal | 60 | 95.2 | 47 | 78.3 | 7.761 | 0.005 |
| 7. In an overall, general sense, how satisfied are you with the service you have received? | Mostly/very satisfied | 55 | 87.3 | 41 | 68.3 | 6.454 | 0.011 |
| 8. If you were to seek help again, would you come back to our program? | Yes, I think so/yes, definitely | 48 | 76.2 | 38 | 63.3 | 2.415 | 0.120 |
At post‐treatment, 10 (15.8%) of participants in HIII and 12 (16.6%) of participants in LIII reported having received some other form of help. At 6‐month follow‐up, 14 (24.5%) of participants in HIII and 15 (27.7%) of participants in LIII reported having received some other form of help (details provided in Supporting information, Appendix S3). There were no significant differences between groups.
Negative effects and deterioration
Halfway through the program, 10 (13.8%) participants in HIII and 14 (19.7%) in LIII reported a negative effect, while at post‐treatment, six (9.5%) participants in HIII and five (8.3%) in LIII reported a negative effect. When analyzing content of the comments, four distinct categories emerged: first, some participants reported experiencing alcohol‐related changes during treatment, such as increased craving, having more intense thoughts about alcohol or even an increase in alcohol consumption. Secondly, some participants reported negative social consequences, such as being questioned by an intimate partner or no longer being able to spend time with friends who drink. Thirdly, some participants reported experiencing feelings of distress; for example, stress about the intervention or feeling depressed due to the intervention constantly reminding them of their alcohol problems. Fourthly, some participants reported somatic, possibly abstinence‐related, symptoms such as headache and sleeping problems (some, but not all, were abstinent at the time of reporting this). Regarding deterioration, two (3.2%) participants in HIII, three (4.9%) participants in LIII and four (18%) participants in WL showed a deterioration in relation to standard drinks, while one participant (1.6%) in HIII, six participants (10%) in LIII and four (18%) participants in WL showed deterioration in relation to HDD.
Discussion
The high‐intensity internet intervention did not result in significantly greater alcohol reductions at the 6‐month follow‐up compared to the low‐intensity internet intervention. Both the high‐ and low‐intensity interventions were significantly more effective in reducing alcohol consumption than the waiting‐list. Adherence was high in both intervention groups, while few negative effects were reported and deterioration was rare. Although we found a significant difference with a small effect size between interventions in HDD at the post‐treatment follow‐up (P = 0.047), this finding should be interpreted with caution, as we did not correct for multiple testing. At the 6‐month follow‐up, mean consumption in the high‐intensity internet intervention had increased since last follow‐up, in contrast to the low‐intensity internet intervention where mean consumption had remained at virtually the same level. A speculation is that therapist guidance functioned as a temporary motivation booster, which for some participants resulted in relapse when the guidance eventually ended. The low‐intensity group, in contrast, did not experience the ending of any guidance as they had to guide themselves through the intervention. Most AUD patients relapse within the first year 34, and continuing care, i.e. regular check‐ups on patients after treatment, has a demonstrable effect on alcohol consumption 35. A possible way to extend the short‐term effects of the high‐intensity internet intervention would be to provide therapist check‐ups after treatment has ended. Although differences in outcomes were small or non‐significant, participants in HIII were significantly more satisfied with the treatment, implying that therapist‐guided interventions may be more appreciated by users than unguided ones.
Our results differ from findings in previous studies where guided internet interventions have been found more effective than unguided internet interventions 14, 15. Notably, differences between a guided and an unguided intervention were larger in a previous pilot trial 15, mainly because the unguided group in the present trial reduced their alcohol consumption to a greater degree than the unguided group in the previous trial, despite the two groups receiving the same program (eChange). A probable explanation is that the comprehensive inclusion process in this study (i.e. use of diagnostic interview) increased motivation among those randomized to the low‐intensity intervention. The phenomenon of assessment reactivity 36 is well documented, and diagnostic assessment has been associated with pre‐treatment change 37. This explanation is corroborated by evaluation questions confirming that participants perceived the diagnostic interview as therapeutic (see Supporting information, Appendix S5. Thus, an unexpected, clinically relevant finding is that assessment‐related human contact may augment the effects of a low‐intensity internet intervention. Further, attrition in the unguided group was surprisingly low. In a previous trial comparing guided to unguided internet interventions, we had major differential attrition 15. However, we found no differential attrition in this trial. A possible explanation is that the diagnostic interview contributed positively to participants’ engagement and adherence in the trial, including completion of follow‐up assessments.
This is the first time, to our knowledge, that systematic diagnostic assessment was used as an inclusion criterion in an alcohol trial where a therapist‐guided internet intervention is tested against an unguided internet intervention. Although some internet intervention trials have included diagnosed participants, these studies have tended to also include users of cannabis 38 and other substances 39. This study thus makes generalizations to the clinical population more valid than previous studies 11. The low attrition implies high internal validity 40. Another contribution to the literature is our exploration of negative effects. Prevalence of negative effects was similar to other studies 17 indicating that internet interventions are safe for people with AUD (although negative reactions may occur and should be monitored). Almost half of participants had psychiatric comorbidity, with depression affecting more than 25% of participants. AUD and depression commonly occur, and although international guidelines suggest addressing both conditions in integrated, dual‐focus interventions to improve both alcohol and depression outcomes, a recent review indicates that evidence for this is sparse 41. Research into how internet interventions might best be tailored to fit different psychiatric profiles could contribute significantly to identifying necessary adaptations of future clinical practice.
This study has limitations. First, participants were recruited by self‐referral and may have had high initial motivation to change. Secondly, the diagnostic assessment interview may have further sorted out less motivated individuals. Thirdly, all data collection was based on self‐report and may thus reflect recall bias and/or social desirability. Although reliance on self‐report measures is standard in alcohol treatment trials, corroboration with objective ways of measuring alcohol consumption (i.e. blood tests) would strengthen future evaluations. Lastly, participants in the waiting‐list first decreased their alcohol consumption after the interview, but then increased it again after having been randomized to the waiting‐list. This pattern may thus partly reflect disappointment after participants realized that they had been randomized to a waiting‐list instead of a natural progression.
High‐ and low‐intensity internet interventions seem effective, acceptable and safe and may have potential as alternatives to traditional treatment forms for people with AUD who, for varying reasons, are reluctant or unable to visit a clinic. Further research is needed to elucidate the differential contributions of high‐ versus low‐intensity internet interventions to recovery from AUD. The field is mature for trials conducted in clinical settings.
Declaration of interests
C.S. has consulted for the software company My Indicators and has received a grant from the Swedish Alcohol Monopoly Research Council. A.H.B. is co‐owner of a company, TeleCoach AB, aiming to disseminate digital interventions for problematic behaviors, including hazardous and harmful alcohol use. The company is not currently active. N.E. is co‐founder of the mental well‐being application Remente. All other authors declare no competing interests or financial relationships with commercial interests.
Clinical trials registration
Supporting information
Appendix S1 Demographic and clinical characteristics separately added as covariates of drinks/heavy drinking days in the treatment model.
Appendix S2 AUD severity as predictor of drinks/heavy drinking days among participants randomized to interventions.
Appendix S3 Access to other help.
Appendix S4 Psychiatric comorbidity as predictor of drinks/heavy drinking days among participants randomized to interventions.
Appendix S5 Evaluation questions about the internet interventions at the post‐treatment follow‐up.
Appendix S6 eChange (low‐intensity intervention).
Appendix S7 ePlus (high‐intensity intervention).
Acknowledgements
The authors wish to thank Mariana Dufort for preparing and executing the randomization schedule, Ingvar Rosendahl for conducting the power analysis and Sanna Beijnoff, Caroline Erkers, Alexander Kolga, Martina Thörnquist for acting as student therapists in the high‐intensity intervention. This study was supported by grants to A.H.B. from the Swedish Research Council, nr K2012‐61X‐22 132–01‐6 and grant no. K2012‐61P‐22 131–01‐6.
Sundström, C. , Eék, N. , Kraepelien, M. , Fahlke, C. , Gajecki, M. , Jakobson, M. , Beckman, M. , Kaldo, V. , and Berman, A. H. (2020) High‐ versus low‐intensity internet interventions for alcohol use disorders: results of a three‐armed randomized controlled superiority trial. Addiction, 115: 863 10.1111/add.14871.
References
- 1. Connor J. P., Haber P. S., Hall W. D. Alcohol use disorders. Lancet 2016; 387: 988–998. [DOI] [PubMed] [Google Scholar]
- 2. Rehm J., Baliunas D., Borges G. L., Graham K., Irving H., Kehoe T., et al The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction 2010; 105: 817–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Probst C., Manthey J., Martinez A., Rehm J. Alcohol use disorder severity and reported reasons not to seek treatment: a cross‐sectional study in European primary care practices. Subst Abuse Treat Prev Policy 2015; 10: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grant B. F. Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. J Stud Alcohol 1997; 58: 365–371. [DOI] [PubMed] [Google Scholar]
- 5. Keyes K. M., Hatzenbuehler M. L., McLaughlin K. A., Link B., Olfson M., Grant B. F., et al Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol 2010; 172: 1364–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schomerus G., Lucht M., Holzinger A., Matschinger H., Carta M. G., Angermeyer M. C. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol 2011; 46: 105–112. [DOI] [PubMed] [Google Scholar]
- 7. Cunningham J. A., Kypri K., McCambridge J. The use of emerging technologies in alcohol treatment. Alcohol Res Health 2011; 33: 320–326. [PMC free article] [PubMed] [Google Scholar]
- 8. Andersson G. Using the internet to provide cognitive behaviour therapy. Behav Res Ther 2009; 47: 175–180. [DOI] [PubMed] [Google Scholar]
- 9. Riper H., Hoogendoorn A., Cuijpers P., Karyotaki E., Boumparis N., Mira A., et al Effectiveness and treatment moderators of internet interventions for adult problem drinking: an individual patient data meta‐analysis of 19 randomised controlled trials. PLOS Med 2018; 15: e1002714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sundström C., Blankers M., Khadjesari Z. Computer‐based interventions for problematic alcohol use: a review of systematic reviews. Int J Behav Med 2017; 24: 646–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dedert E. A., McDuffie J. R., Stein R., McNiel J. M., Kosinski A. S., Freiermuth C. E., et al Electronic interventions for alcohol misuse and alcohol use disorders: a systematic review. Ann Intern Med 2015; 163: 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided internet‐based versus. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta‐analysis. World Psychiatry 2014; 13: 288–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Titov N., Dear B., Nielssen O., Staples L., Hadjistavropoulos H., Nugent M., et al ICBT in routine care: a descriptive analysis of successful clinics in five countries. Internet Interv 2018; 13: 108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Blankers M., Koeter M. W., Schippers G. M. Internet therapy versus internet self‐help versus no treatment for problematic alcohol use: a randomized controlled trial. J Consult Clin Psychol 2011; 79: 330–341. [DOI] [PubMed] [Google Scholar]
- 15. Sundström C., Gajecki M., Johansson M., Blankers M., Sinadinovic K., Stenlund‐Gens E., et al Guided and unguided internet‐based treatment for problematic alcohol use—a randomized controlled pilot trial. PLOS ONE 2016; 11: e0157817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Postel M. G., de Haan H. A., ter Huurne E. D., Becker E. S., de Jong C. A. Effectiveness of a web‐based intervention for problem drinkers and reasons for dropout: randomized controlled trial. J Med Internet Res 2010; 12: e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rozental A., Andersson G., Boettcher J., Ebert D. D., Cuijpers P., Knaevelsrud C., et al Consensus statement on defining and measuring negative effects of internet interventions. Internet Interv 2014; 1: 12–19. [Google Scholar]
- 18. Saunders J. B., Aasland O. G., Babor T. F., Delafuente J. R., Grant M. Development of the alcohol‐use disorders identification test (AUDIT)—WHO collaborative project on early detection of persons with harmful alcohol‐consumption–II. Addiction 1993; 88: 791–804. [DOI] [PubMed] [Google Scholar]
- 19. Kranzler H. R., Kadden R. M., Babor T. F., Tennen H., Rounsaville B. J. Validity of the SCID in substance abuse patients. Addiction 1996; 91: 859–868. [PubMed] [Google Scholar]
- 20. Sheehan D. V., Lecrubier Y., Sheehan K. H., Amorim P., Janaversus J., Weiller E., et al The Mini‐international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM‐IV and ICD‐10. J Clin Psychiatry 1998; 59: 22–33; quiz 4–57. [PubMed] [Google Scholar]
- 21. Sundström C., Kraepelien M., Eek N., Fahlke C., Kaldo V., Berman A. H. High‐intensity therapist‐guided internet‐based cognitive behavior therapy for alcohol use disorder: a pilot study. BMC Psychiatry 2017; 17: 197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sobell L. C., Maisto S. A., Sobell M. B., Cooper A. M. Reliability of alcohol abusers’ self‐reports of drinking behavior. Behav Res Ther 1979; 17: 157–160. [DOI] [PubMed] [Google Scholar]
- 23. Berman A. H., Forsberg L., Durbeej N., Kallmen H., Hermansson U. Single‐session motivational interviewing for drug detoxification inpatients: effects on self‐efficacy, stages of change and substance use. Subst Use Misuse 2010; 45: 384–402. [DOI] [PubMed] [Google Scholar]
- 24. Flannery B. A., Volpicelli J. R., Pettinati H. M. Psychometric properties of the Penn alcohol craving scale. Alcohol Clin Exp Res 1999; 23: 1289–1295. [PubMed] [Google Scholar]
- 25. Svanborg P., Asberg M. A comparison between the Beck Depression Inventory (BDI) and the self‐rating version of the Montgomery Asberg Depression Rating Scale (MADRS). J Affect Disord 2001; 64: 203–216. [DOI] [PubMed] [Google Scholar]
- 26. Spitzer R. L., Kroenke K., Williams J. B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 27. Herdman M., Gudex C., Lloyd A., Janssen M., Kind P., Parkin D., et al Development and preliminary testing of the new five‐level version of EQ‐5D (EQ‐5D‐5L). Qual Life Res 2011; 20: 1727–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Berman A. H., Bergman H., Palmstierna T., Schlyter F. Evaluation of the Drug Use Disorders Identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res 2005; 11: 22–31. [DOI] [PubMed] [Google Scholar]
- 29. Borkovec T. D., Nau S. D. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry 1972; 3: 257–260. [Google Scholar]
- 30. Larsen D. L., Attkisson C. C., Hargreaves W. A., Nguyen T. D. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann 1979; 2: 197–207. [DOI] [PubMed] [Google Scholar]
- 31. Horton N. J., Kim E., Saitz R. A cautionary note regarding count models of alcohol consumption in randomized controlled trials. BMC Med Res Methodol 2007; 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Beard E., Dienes Z., Muirhead C., West R. Using Bayes factors for testing hypotheses about intervention effectiveness in addictions research. Addiction 2016; 111: 2230–2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dienes Z. Bayes factor calculator [Available at: http://www.lifesci.sussex.ac.uk/home/Zoltan_Dienes/inference/Bayes.htm. Date accessed: 2019-10-14
- 34. Miller W. R., Walters S. T., Bennett M. E. How effective is alcoholism treatment in the United States? J Stud Alcohol 2001; 62: 211–220. [DOI] [PubMed] [Google Scholar]
- 35. McLellan A. T., McKay J. R., Forman R., Cacciola J., Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow‐up to concurrent recovery monitoring. Addiction 2005; 100: 447–458. [DOI] [PubMed] [Google Scholar]
- 36. Clifford P. R., Maisto S. A., Davis C. M. Alcohol treatment research assessment exposure subject reactivity effects: part I. alcohol use and related consequences. J Stud Alcohol Drugs 2007; 68: 519–528. [DOI] [PubMed] [Google Scholar]
- 37. Epstein E. E., Drapkin M. L., Yusko D. A., Cook S. M., McCrady B. S., Jensen N. K. Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol‐dependent women. J Stud Alcohol 2005; 66: 369–378. [DOI] [PubMed] [Google Scholar]
- 38. Kay‐Lambkin F. J., Baker A. L., Lewin T. J., Carr V. J. Computer‐based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: a randomized controlled trial of clinical efficacy. Addiction 2009; 104: 378–388. [DOI] [PubMed] [Google Scholar]
- 39. Kiluk B. D., Nich C., Buck M. B., Devore K. A., Frankforter T. L., LaPaglia D. M., et al Randomized clinical trial of computerized and clinician‐delivered CBT in comparison with standard outpatient treatment for substance use disorders: primary within‐treatment and follow‐up outcomes. Am J Psychiatry 2018; 175: 853–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Postel M. G., de Haan H. A., ter Huurne E. D., van der Palen J., Becker E. S., de Jong C. A. Attrition in web‐based treatment for problem drinkers. J Med Internet Res 2011; 13: e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hobden B., Bryant J., Carey M., Baker A. L., Farrell M., Oldmeadow C., et al Finding the optimal treatment model: a systematic review of treatment for co‐occurring alcohol misuse and depression. Aust NZ J Psychiatry 2018; 52: 737–750. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Demographic and clinical characteristics separately added as covariates of drinks/heavy drinking days in the treatment model.
Appendix S2 AUD severity as predictor of drinks/heavy drinking days among participants randomized to interventions.
Appendix S3 Access to other help.
Appendix S4 Psychiatric comorbidity as predictor of drinks/heavy drinking days among participants randomized to interventions.
Appendix S5 Evaluation questions about the internet interventions at the post‐treatment follow‐up.
Appendix S6 eChange (low‐intensity intervention).
Appendix S7 ePlus (high‐intensity intervention).


