Abstract
OBJECTIVES:
The American Academy of Pediatrics recommends that all pediatricians screen for social determinants of health to identify families in need and connect them to available resources. We examined pediatric residents’ screening practices for social needs in different clinical settings and explored the influence of electronic health record (EHR) prompts on screening.
METHODS:
In this cross-sectional study, pediatric residents participated in a brief electronic survey assessing (1) screening practices for unmet social needs and (2) perceived barriers to and facilitators of routine screening in the inpatient and outpatient settings. The differences in screening by care setting were assessed by using Fisher’s exact test. Mixed-effects logistic regression was used to examine the association between EHR prompts and resident screening practices.
RESULTS:
Ninety-two pediatric residents (64% of the residency program) responded to the survey. Respondents reported significantly higher rates of social needs screening in the outpatient as compared with the inpatient setting (98% vs 37%; P < .001). Residents cited time constraints, lack of knowledge about available resources, and discomfort with screening questions as barriers to screening in both settings. Residents were more likely to screen for social needs when screening questions were embedded in the EHR (odds ratio = 9.6; 95% confidence interval: 6.7–13.9).
CONCLUSIONS:
Pediatric residents were more likely to screen for unmet social needs in the outpatient than in the inpatient setting despite reporting similar barriers to screening in both settings. EHR-based social needs screening templates could be used to increase rates of screening and reach additional families in need.
Poverty and associated social determinants of health, such as food insecurity and housing instability, can adversely affect children’s health and development.1–5 In 2016, the American Academy of Pediatrics (AAP) released a policy statement encouraging community pediatricians to screen for unmet social needs in order to identify families in need and connect them to community resources.6 However, implementing successful screening and referral programs has been challenging. In previous surveys of primary care pediatricians across the United States, fewer than half reported routinely screening for social needs in their practice.7–9
These previous studies were focused predominantly on social needs screening practices in the primary care setting, but there is evidence to suggest that families are also receptive to screening in the inpatient setting.10 Pediatric residents often serve as frontline providers for children living in poverty in both inpatient and outpatient settings and can therefore play an important role in identifying and addressing families’ social needs across care settings. In this study, we aimed to (1) examine residents’ self-reported social needs screening practices in inpatient and outpatient settings, (2) identify barriers to and facilitators of screening in each setting, and (3) assess whether residents reported screening more frequently when prompts were embedded in the electronic health record (EHR).
Methods
This cross-sectional study was conducted at a large academic pediatric health system in which residents provide inpatient care at a tertiary care children’s hospital and outpatient care at 1 of 3 urban primary care practices serving a predominantly Medicaid-insured, minority population. In both the inpatient and outpatient settings, on-site social workers are available to address families’ social needs.
Pediatric residents (N = 144) received e-mail invitations to participate in an electronic survey assessing (1) social needs screening practices in the inpatient and outpatient settings and (2) perceived barriers to and facilitators of screening. The survey instrument (Supplemental Fig 3) was developed on the basis of a review of the literature, pilot tested with a subset of residents, and then administered from April 2017 to June 2017.
For each included social need (educational support needs, food insecurity, housing issues, intimate partner violence, legal needs, and maternal depression), residents were asked to indicate whether they screened never (≤25% of the time), rarely (25%–50% of the time), often (50%–75% of the time), or always (≥75% of the time) in the inpatient and outpatient setting. A response of “often” or “always” was classified as routinely screening, whereas a response of “never” or “rarely” was classified as not routinely screening. Residents were asked to select their 2 most significant barriers to and facilitators of screening in each setting from a list of potential barriers and facilitators initially generated through a literature review and then refined when the survey was piloted. Outpatient clinic visit and inpatient admission EHR templates were reviewed, and social needs were classified as included in the EHR if at least 1 social needs screening question related to that domain was present in any EHR template (Supplemental Table 1).
Fisher’s exact test was used to compare screening rates by care setting. Multivariable mixed-effects logistic regression was used to examine associations between screening rates and the presence of screening questions in EHR-based templates. We examined whether each resident reported screening for each social need as a binary outcome, with age, race and/or ethnicity, sex, level of training, care setting, and the presence of screening questions in an EHR template as fixed effects. A resident identifier was included as a random effect because screening behaviors may have clustered by survey participant. Survey data were analyzed using Stata 15.0 (Stata Corp, College Station, TX).11
Results
Ninety-two pediatric residents completed the survey, for a response rate of 64% (92 of 144 residents). Most respondents were women (74%). Residents ranged in age from 26 to 39, with a median age of 29 years. Most respondents (75%) identified as white, 13% as Asian American, 8% as Hispanic, and 4% as African American.
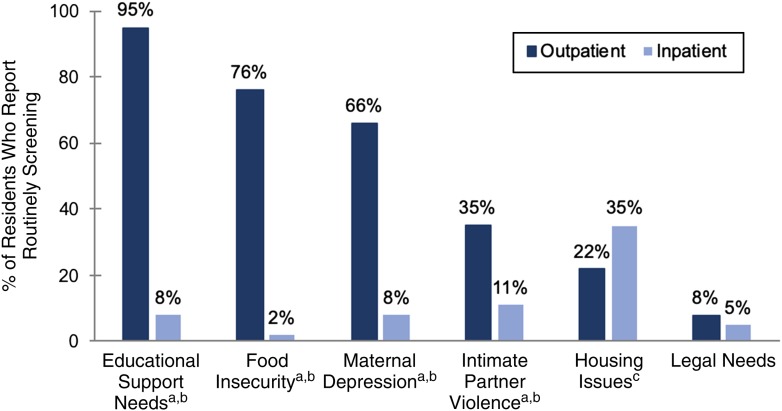
Social needs screening rates are summarized in Fig 1. Overall, a significantly greater proportion of residents reported routinely screening for at least 1 social need in the outpatient setting compared with the inpatient setting (98% vs 37%; P < .001). In the outpatient setting, residents most frequently screened for educational support needs (95%), food insecurity (76%), and maternal depression (66%). In the inpatient setting, residents most frequently screened for housing issues (35%) and intimate partner violence (11%). In mixed-effects multivariable analysis, residents were more likely to screen for individual social needs in the outpatient setting (odds ratio = 4.4; 95% confidence interval: 3.0–6.4) and if screening questions were embedded in EHR-based templates (odds ratio = 9.6; 95% confidence interval: 6.7–13.9). There were no significant associations between screening and resident age, sex, race and/or ethnicity, or level of training.
FIGURE 1.
Resident rates of social needs screening by setting. a Significant differences between inpatient and outpatient screening rates at P < .001. b Social needs included in EHR-based templates in the outpatient setting. c Social needs included in EHR-based templates in the inpatient setting.
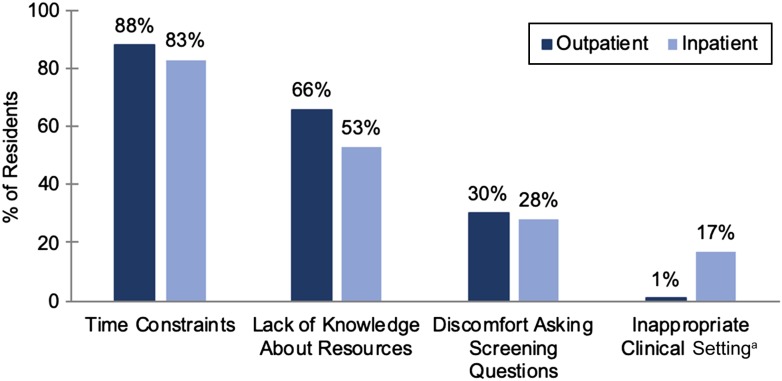
In both settings, residents cited time constraints, lack of knowledge about resources available to families, and discomfort with asking screening questions as the most common barriers to screening (Fig 2). The suggested interventions to facilitate screening included support staff to facilitate referrals (88%), EHR-based screening templates (72%), accessible information about resources for families (61%), and education regarding how to discuss social needs with families (38%).
FIGURE 2.
Resident-reported barriers to screening by setting. a Significant difference between inpatient and outpatient rates of reporting each barrier at P < .001.
Discussion
With this study, we are the first to examine differences in residents’ rates of social needs screening by care setting and describe the influence of EHR-based templates on screening rates across care settings. Our screening rates in the outpatient setting are higher than those reported in previous studies.7–9 This could reflect both the impact of the AAP’s 2016 policy statement encouraging screening and the high prevalence of poverty at our resident clinics; one recent study revealed an association between pediatricians’ social needs screening rates and the proportion of their patients experiencing financial hardship.7
The comparatively low rate of social needs screening we observed in the inpatient setting indicates an opportunity for improvement. The burden of competing demands for outpatient provider visits is well documented.12 The inpatient setting offers more time to target social needs, and previous work suggests that most caregivers view in-hospital screening favorably.10 Given the demonstrated relationships between social determinants of health and hospitalization costs, lengths of stay, and preventable readmissions, inpatient screening programs that address social risks could provide synergy with hospital systems’ institutional priorities.13–16 For families living in poverty, who often face barriers to accessing preventive care, hospital-based programs could provide an additional opportunity to connect with resources targeted to their social needs.
In our study, we also found a strong positive association between social needs screening rates and the presence of screening questions in EHR templates. Previous studies have revealed that EHR-based reminders can be strategically deployed to promote desired physician behaviors such as prescribing generic medications and administering influenza vaccinations.17–19 One previous study revealed that an asthma-specific admission note template led to increased documentation of families’ housing issues.20 Our results suggest that this methodology could be used to increase social needs screening rates more broadly by including multiple domains in EHR templates and incorporating prompts that promote screening across care settings. However, given the potential adverse consequences of social needs screening if conducted in a way that is insensitive to families’ preferences,21 hospital systems must be thoughtful in selecting which social needs to include in screening, particularly in the inpatient setting, in which individuals administering a screen may not have longitudinal relationships with caregivers.
Residents must also receive education on how to discuss social needs with families and engage them in shared decision-making around referrals to community resources.22,23 Attending hospitalists should explicitly emphasize and model strategies for identifying and addressing social needs in the inpatient setting because attending feedback and expectations can be a powerful driver of resident behavior. Social needs screening and referral programs are likely to be most effective if they incorporate resident and attending physician education regarding the importance of screening, EHR reminders that promote screening in practice, and support staff to facilitate referrals for families.
This study has several limitations. It was conducted at a single urban academic health system in a residency program with a longitudinal advocacy curriculum spanning at least 4 weeks each year, including modules focused on social determinants of health, which may limit the generalizability of our results. We relied on self-reported rates of screening, and social desirability or recall bias may have influenced participant reporting. Additionally, although our study was focused on residents, it is crucial to also consider the perspectives of other members of the care team, including attending physicians, nurses, social workers, and caregivers, when determining the feasibility of inpatient social needs screening. In future studies, authors should more comprehensively evaluate feasibility, acceptability, and impact of social needs screening and referral programs in the inpatient setting, with a focus on ensuring that families are connected with resources targeted to their needs.
Conclusions
Pediatric residents reported screening for social needs more frequently in the outpatient setting than in the inpatient setting and were more likely to screen when questions were incorporated into EHR templates. There may be an opportunity to reach additional families in need by implementing screening in the inpatient setting, and linking EHR screening templates to community resources may help the next generation of pediatricians more effectively identify and address families’ unmet social needs.
Footnotes
Dr Vasan conceptualized and designed the study, designed the data collection instrument, conducted the data analysis, and drafted the initial manuscript; Drs Kenyon and Palakshappa supervised conceptualization and design of the study, assisted in the data analyses, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr. Kenyon was supported by a K-award from the National Institutes of Health’s National Heart, Lung, and Blood Institute (5K23HL136842-02). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72 [DOI] [PubMed] [Google Scholar]
- 2.Alaimo K, Olson CM, Frongillo EA., Jr Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development [published correction appears in Pediatrics. 2001;108(3):824b]. Pediatrics. 2001;108(1):44–53 [PubMed] [Google Scholar]
- 3.Peltz A, Garg A. Food insecurity and health care use. Pediatrics. 2019;144(4):e20190347. [DOI] [PubMed] [Google Scholar]
- 4.Drennen CR, Coleman SM, Ettinger de Cuba S, et al. Food insecurity, health, and development in children under age four years. Pediatrics. 2019;144(4):e20190824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandel M, Sheward R, Ettinger de Cuba S, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2):e20172199. [DOI] [PubMed] [Google Scholar]
- 6.Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339. [DOI] [PubMed] [Google Scholar]
- 7.Garg A, Cull W, Olson L, et al. Screening and referral for low-income families’ social determinants of health by US pediatricians. Acad Pediatr. 2019;19(8):875–883 [DOI] [PubMed] [Google Scholar]
- 8.Morgenlander MA, Tyrrell H, Garfunkel LC, Serwint JR, Steiner MJ, Schilling S. Screening for social determinants of health in pediatric resident continuity clinic. Acad Pediatr. 2019;19(8):868–874 [DOI] [PubMed] [Google Scholar]
- 9.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558 [DOI] [PubMed] [Google Scholar]
- 10.Colvin JD, Bettenhausen JL, Anderson-Carpenter KD, Collie-Akers V, Chung PJ. Caregiver opinion of in-hospital screening for unmet social needs by pediatric residents. Acad Pediatr. 2016;16(2):161–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. StataCorp. Stata Statistical Software: Release 15 [computer program]. College Station, TX: Stata Corp LLC; 2017.
- 12.Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1592 [DOI] [PubMed] [Google Scholar]
- 14.Beck AF, Riley CL, Taylor SC, Brokamp C, Kahn RS. Pervasive income-based disparities in inpatient bed-day rates across conditions and subspecialties. Health Aff (Millwood). 2018;37(4):551–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sills MR, Hall M, Colvin JD, et al. Association of social determinants with children’s hospitals’ preventable readmissions performance. JAMA Pediatr. 2016;170(4):350–358 [DOI] [PubMed] [Google Scholar]
- 16.McKay S, Parente V. Health disparities in the hospitalized child. Hosp Pediatr. 2019;9(5):317–325 [DOI] [PubMed] [Google Scholar]
- 17.Patel MS, Day SC, Halpern SD, et al. Generic medication prescription rates after health system-wide redesign of default options within the electronic health record. JAMA Intern Med. 2016;176(6):847–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel MS, Volpp KG, Small DS, et al. Using active choice within the electronic health record to increase influenza vaccination rates. J Gen Intern Med. 2017;32(7):790–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burkhardt MC, Beck AF, Conway PH, Kahn RS, Klein MD. Enhancing accurate identification of food insecurity using quality-improvement techniques. Pediatrics. 2012;129(2). Available at: www.pediatrics.org/cgi/content/full/129/2/e504 [DOI] [PubMed] [Google Scholar]
- 20.Beck AF, Sauers HS, Kahn RS, Yau C, Weiser J, Simmons JM. Improved documentation and care planning with an asthma-specific history and physical. Hosp Pediatr. 2012;2(4):194–201 [DOI] [PubMed] [Google Scholar]
- 21.Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316(8):813–814 [DOI] [PubMed] [Google Scholar]
- 22.Klein MD, Schumacher DJ, Sandel M. Assessing and managing the social determinants of health: defining an entrustable professional activity to assess residents’ ability to meet societal needs. Acad Pediatr. 2014;14(1):10–13 [DOI] [PubMed] [Google Scholar]
- 23.Klein MD, Kahn RS, Baker RC, Fink EE, Parrish DS, White DC. Training in social determinants of health in primary care: does it change resident behavior? Acad Pediatr. 2011;11(5):387–393 [DOI] [PubMed] [Google Scholar]