Abstract
Despite the prevalence of vertical integration, data and research focused on identifying and describing health systems are sparse. Until recently, we lacked an enumeration of health systems and an understanding of how systems vary by key structural attributes. To fill this gap, the Agency for Healthcare Research and Quality developed the Compendium of U.S. Health Systems, a data resource to support research on comparative health system performance. In this article, we describe the methods used to create the Compendium and present a picture of vertical integration in the United States. We identified 626 health systems in 2016, which accounted for 70% of nonfederal general acute care hospitals. These systems varied by key structural attributes, including size, ownership, and geographic presence. The Compendium can be used to study the characteristics of the U.S. health care system and address policy issues related to provider organizations.
Keywords: health systems, vertical integration, hospital–physician affiliations, delivery system organization
Introduction
Payment and delivery reforms have encouraged changes to the organization of the U.S. health care system, resulting in greater integration of hospitals and physicians into health systems. Horizontal and vertical consolidation of hospitals and physicians has occurred rapidly for more than two decades. The percentage of U.S. hospitals in a health system rose from 53% in 2001 to 60% in 2011, and hospital ownership of physician practices increased from 24% in 2004 to 49% in 2011 (Cutler & Scott Morton, 2013). More recently, the share of physicians who own their own practice declined from 53% in 2012 to 47% in 2016 (Kane, 2017). Given these trends, more research is needed on the organization of care and the extent to which providers are organized into integrated systems.
Prior data and research on vertical integration has predominantly taken the perspective of the physician, practice, or hospital—not the system. Data and research typically focus on the components of integrated systems such as hospital ownership of physicians (Baker, Bundorf, Devlin, & Kessler, 2018) or physician employment by hospitals (Burns, Goldsmith, & Sen, 2013). However, less data and research have focused on vertically integrated entities at the system level, emphasizing the parent organizations that include hospitals and physicians under common ownership and management (Burns, Gimm, Nicholson, & Muller, 2005; Burns & Pauly, 2002; Goldsmith, Burns, Sen, & Goldsmith, 2015). In fact, despite the prevalence of vertical integration, we lack an enumeration of health systems in the United States and an understanding of how systems vary by key structural attributes (Casalino, 2014; Cohen et al., 2017). Research on systems extends beyond the hospital-physician relationship to focus on the institutions that can potentially support functions, such as sharing electronic health records, establishing standard care guidelines, taking on risk in contracts, and, in some cases, offering an insurance product.
To advance research on this topic, the Agency for Healthcare Research and Quality (AHRQ) created the Comparative Health System Performance (CHSP) Initiative to study how health care systems promote evidence-based practices in delivering care. As part of the initiative, AHRQ developed the Compendium of U.S. Health Systems as a data resource to identify health systems and describe key system attributes (AHRQ, 2017a).1
The Compendium can be used by researchers, policymakers, and other stakeholders to address a range of policy issues, such as assessing the diversity of health care structures underlying alternative payment models and understanding how system attributes affect cost and quality outcomes (Post, Buchmueller, & Ryan, 2018). As payment and delivery reforms encourage vertical integration through accountable care organizations and bundled payments, accounting for how health care is structured may inform the design of new policies.
For this article, we use the Compendium to characterize health systems in the United States as of 2016. Our study (1) enumerates the number of health systems in the United States; (2) characterizes systems by key structural attributes such as size, ownership, system type, and geographic presence; and (3) reports system penetration among hospitals, beds, and physicians.
New Contribution
Our study differs from prior work on vertical integration in three ways. First, our study examines vertical integration at the system level, whereas prior studies have focused on physicians, practices, and hospitals. Focusing on the hospital-physician relationship within health systems allows us to distinguish between vertical integration that is and is not part of a health system. Second, our study is the first to identify and enumerate the number of health systems in the United States, delineate system composition, and describe variation across systems. This contribution allows us to describe the landscape of hospitals and physicians at the system level rather than at the hospital or physician level. Third, we introduce the Compendium of U.S. Health Systems, the first publicly available data resource that identifies and describes health systems that have formed from the dramatic consolidation of physicians and hospitals into vertically integrated arrangements. We describe the construction of the Compendium and use it to characterize the landscape of the U.S. health care systems. By linking the Compendium to other data sources, stakeholders will be able to answer important policy questions about systems’ impact on care delivery, health care costs and quality, and how different system characteristics affect comparative health system performance.
Method and Data
Defining Health Systems
We used the definition of a health system that a group of experts developed under the CHSP Initiative. According to this definition, a health system is
an organization that includes at least one hospital and at least one group of physicians that provides comprehensive care (including primary and specialty care) who are connected with each other and with the hospital through common ownership or joint management. (AHRQ, 2017c)
This definition does not explicitly include other provider types and other common forms of integration between providers. For example, this definition does not explicitly include health system ownership/management of post–acute care providers and nonownership contractual relationships such as accountable care organizations or physician hospital organizations. It also excludes multihospital systems (without sufficient outpatient capacity) and multispecialty group practices (without an inpatient presence).
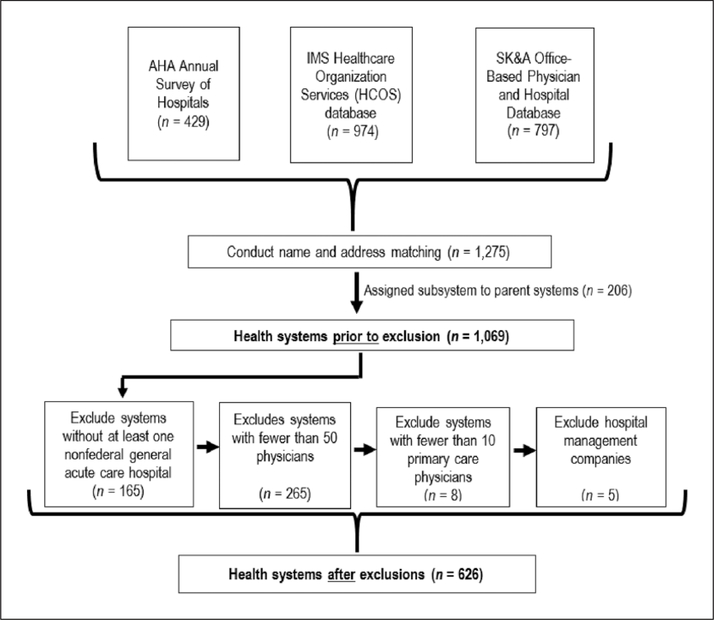
Prior work on the extent of vertical integration has compared two national surveys to assess ownership patterns (Baker et al., 2018); however, we were not aware of a gold standard on health systems by which to validate our estimates. No single data source enumerates or describes the health systems that meet the CHSP definition (Cohen et al., 2017). To construct the Compendium, we selected three data sources that identify health systems: the American Hospital Association (AHA) Annual Survey, Quintiles IMS Healthcare Organization Services Database (HCOS), and SK&A’s Office-Based Physician and Hospital Databases (the latter two now make up IQVIA). These data sources rely on different techniques for surveying organizations and providers, and they rely on different definitions of health systems (Table 1). For example, AHA surveys hospitals and asks respondents to self-report the characteristics and attributes of their hospitals, including counts of affiliated physicians. Their definition of a system includes either a multihospital system or a diversified single hospital system. SK&A surveys outpatient practices, enumerates providers, and asks for their hospital affiliations. Their definition of a health system emphasizes ownership or management of health care providers, including hospitals, medical offices, group practices, and nursing homes. HCOS uses secondary data from industry sources—including the National Plan and Provider Enumeration System, the Drug Enforcement Agency, and the Drug Distribution Database—to identify providers and organizations. Linkages are made using proprietary matching algorithms. Because of these differences in definition, each data source identifies a different number of total systems (Figure 1).
Table 1.
Health System Definition, by Data Source.
| Data source | Health system definition |
|---|---|
| American Hospital Association annual survey | Either a multihospital or a diversified single hospital system. A multihospital system is two or more hospitals owned, leased, sponsored, or contract managed by a central organization. |
| HCOS | An organization that has direct responsibility for centralizing the purchasing or contracting of its affiliated hospitals and ancillary care facilities; it also offers a continuum of care through services at acute and non-acute sites. An integrated delivery network owns, leases, manages, or establishes a purchasing affiliation with two or more health care delivery sites. Integrated delivery networks include at least one acute care hospital and one non-acute organization. |
| SK&A | Health care organizations that own or manage a complex delivery network of health care providers, including hospitals, medical offices, group practices, and nursing homes. |
Note. HCOS = Healthcare Organization Services.
Figure 1.
Flowchart describing the construction of the Agency for Healthcare Research and Quality’s (AHRQ) Compendium of U.S. Health Systems, 2016.
Developing a List of Health Systems
We constructed the Compendium in four steps: (1) conducting name and address matches across contributing data sources, (2) aggregating regional subsystems into their parent systems, (3) applying exclusion criteria to help identify systems delivering comprehensive care, and (4) removing hospital management companies (Figure 1). Each step is described below. For a complete description of the methods we used to construct the Compendium, see the technical documentation on the AHRQ website (AHRQ, 2017b).
First, we applied a series of automated matching techniques using the names and addresses of systems to create a deduplicated list of health systems across the three data sources. Specifically, we conducted character-string matching and distance-based matching using geocoding in SAS. In addition, we manually reviewed a set of matches identified in the automated process as potential matches to determine if they were in fact matches. The process resulted in a list of 1,275 unique health systems.
Next, we sought to aggregate regional subsystems into their parent systems. That is, some medium and large health systems have smaller, regional subsystems nested within them. These types of nested relationships are explicitly defined in the SK&A data. We identified possible additional subsystems by reviewing discrepancies across data sources in how entities are classified. For example, an entity that is classified as a system in one source but as a hospital linked to a larger system in another source might represent a nested relationship. We aggregated the information for identified regional subsystems under their parent systems (n = 206) and reported only the parent subsystems.2 This approach does not address whether systems deliver comprehensive care that would qualify them as health systems in all of their local or regional markets.
Third, we applied exclusion criteria to remove health systems that did not appear to meet the requirement that a system provide comprehensive care. We excluded systems that (1) lacked at least one general acute care hospital (n = 165), (2) had fewer than 50 physicians (n = 265), or (3) had fewer than 10 primary care physicians (n = 8). We chose these thresholds based on the requirement that a system include a sufficient number of physicians to plausibly offer a reasonably comprehensive range of services to their patients.
Finally, we removed systems that were hospital management companies that did not appear to own or tightly manage comprehensive physician services and thus did not meet the criteria used to identify health systems. To identify systems that might be hospital management companies, we reviewed the corporate website of entities for which either the AHA data indicated that they had a hospital under contract management and the management organization name matched the system name or the entity was classified as primarily investor owned. To be retained as a system on the list, the corporation website had to document either (1) common ownership of at least one general acute care hospital and one group of physicians providing comprehensive primary care and specialty care or (2) tight joint management of at least one general acute care hospital and one group of physicians providing comprehensive primary and specialty care. We defined tight joint management as a foundation model, shared governance (e.g., substantially overlapping board membership of a hospital and comprehensive medical group), or explicit cobranding of physicians with the system. We did not consider physician-hospital organizations, by themselves, to represent tight joint management. The final list comprises 626 health systems.
Operationalizing the CHSP initiative’s definition of health systems highlights the challenges of determining the exact nature of the relationship between systems and their components. Our approach to constructing the Compendium relied on some level of expert judgment to confirm linkages across the data sources, linkages between systems and their components, and to identify systems that deliver comprehensive care and meet our definition of a health system. For example, hospital management companies often present much like systems that provide comprehensive care, and it is not always possible to assess systems’ business models based on publicly available information. Also, there can be a time lag in capturing changes to systems resulting from mergers and acquisitions.
Determining System Counts of Hospitals and Physicians
All of the contributing data sources include information on system components, namely, hospitals and physicians. However, even when two sources identified the same system, they did not always identify the same components. To identify a final system count of hospitals, we matched hospitals across data sources using available identifiers, including CMS Certification Number (CCN) and AHA identification number (AHA ID). We also conducted hospital name and location matches because not all hospitals in the contributing data source had identifiers. We then removed all hospitals that did not report at least a CCN or an AHA ID after we performed name and location matching.
We manually reviewed hospitals that were listed in more than one health system, and we assigned each hospital to a single system.3 In most cases, the multiple systems were in fact the same system with a different name or systems that were nested within one another (i.e., subsystems and parent systems). In the former case, we updated the list to indicate that these systems were a match and the hospital belonged to this system; in the latter case, we assigned the hospital to the parent system. The remaining cases were hospital-level joint ventures in which multiple systems have a formal relationship with at least one other hospital. In these cases, we assigned the hospital to a system based on three decision rules, in order of priority: (1) there is a clear majority owner or a system that runs the day-to-day operations of the hospital, (2) the hospital is investor owned and only one of the systems is investor owned, and (3) in the absence of other clarifying information, proximity between the hospital and the system headquarters.
Counts of the number of physicians affiliated with health systems varied substantially across the data sources. The highest counts were typically found in HCOS, partly because HCOS attempts to enumerate both hospital-based physicians and those working in office-based practices. We limited the HCOS counts to physicians with close affiliations with facilities in the system. These close affiliations are identified as attending physicians (for system hospitals), facility staff and treating physicians for long-term care facilities, and all physician affiliations for system medical groups and other system facility types. This approach excludes physicians with looser system affiliations, such as those with only admitting privileges at hospitals.4 SK&A enumerates office-based physicians and seeks information about each of those physician’s affiliations and thus undercounts some hospital-based physicians (DesRoches et al., 2015). The AHA data do not enumerate individual physicians, but the survey asks about the counts of physicians in various hospital-physician relationships; we summed the AHA physicians across integrated salary, equity, and foundation models. We reported the highest physician count value for a system found across the three data sources to err on the side of inclusion, given the physician count exclusion criteria.
The thresholds of primary care and specialist physicians we used to exclude systems that did not provide comprehensive care are by their very nature judgment calls. However, we conducted sensitivity tests around the thresholds we selected to identify which systems would be dropped or added. We then conducted web searches of these systems to assess whether the added systems were in fact providing a comprehensive range of services or whether the dropped systems were potentially important to their community and provided a wide range of services. This approach may result in the underrepresentation of systems serving patients in rural or frontier areas; systems using networking approaches (i.e., teleconsultation) to provide comprehensive care, which may require fewer physicians; and systems that rely more heavily on advanced practice clinicians.
Describing System Attributes and Calculating System Penetration
To describe system attributes, we merged hospital data from the Healthcare Cost Report Information System (HCRIS; for total beds, ratio of full-time equivalent [FTE] residents to beds, hospital ownership type, and Medicare disproportionate share hospital [DSH] patient percentage) and the AHA annual survey (for missing hospital ownership type), and we aggregated hospital data up to the system level. We defined safety net hospitals as hospitals in the top quintile of Medicare DSH patient percentage among all nonfederal general acute care hospitals and indicated whether or not the system included at least one safety net hospital. We calculated system ownership type by determining the most common ownership type among system beds. We also calculated system hospital presence by counting the number of states in which the system operates (defined by the locations of their member hospitals).
To calculate measures of system penetration, we identified the total number of nonfederal general acute care hospitals in the United States and the total number of physicians. We defined total hospitals as nonfederal general acute care hospitals with a CCN or AHA ID in one of the three data sources. We obtained total physician counts from the HCOS data. Whereas physicians could be reported in more than one system for the system-level physician counts in the Compendium, we deduplicated the counts of total physician and physicians in systems when calculating system penetration. System penetration was calculated using a numerator of the total number of unique physicians in systems from HCOS and a denominator of total number of unique physicians in the United States from HCOS.5
Results
The 626 health systems in the United States varied by key structural attributes, including size, ownership, system type, and hospital presence. For example, we found substantial variation in the distribution of system size among health systems (Table 2). A large proportion of health systems are relatively small, based on the number of participating hospitals and physicians. The median number of hospitals in health systems is 2, with a range from 1 to 175 hospitals per system. About one-third of systems (n = 223) have only one general acute care hospital. The median number of physicians in health systems is 245. Across systems, the number of physicians ranged from 50 to 20,300.
Table 2.
Distribution of System Size, by Number of Hospitals and Physicians.
| Health systems
(n = 626) |
|||||||
|---|---|---|---|---|---|---|---|
| M | SD | Lowest number | 25th percentile | Mdn | 75th percentile | Highest number | |
| Hospitals | 6 | 13.6 | 1 | 1 | 2 | 5 | 175 |
| Hospital beds | 965 | 2,207.8 | 24 | 247 | 433 | 885 | 34,532 |
| Physicians | 742 | 1,479.5 | 50 | 112 | 245 | 767 | 20,300 |
| Primary care physicians | 227 | 502.7 | 10 | 41 | 93 | 234 | 8,995 |
Note. Data come from the 2016 AHRQ Compendium of U.S. Health Systems. Hospital and hospital beds reflect general acute care hospitals.
A small number of relatively large systems account for a disproportionate share of providers. The 10 largest systems in terms of the number of physicians account for 21.0% of the physicians in systems. The 10 largest systems in terms of the number of hospital beds account for 24.5% of beds in systems.
Health systems also varied by ownership, system type, and geographic presence (Table 3). Roughly 80% of health systems have nonprofit ownership, including religiously affiliated systems. One in six systems (17.3%) have state/local government ownership; these vary in size, but approximately half (50.9%) are below the overall median size as measured by the number of hospital beds. We identified 19 systems (3.0%) with investor ownership; these also vary in size, with the bulk of these systems (77.8%) above the overall system median for number of hospital beds. Appendix Table A1 highlights the variation in system attributes by size by presenting the 10 largest, 10 medium-sized, and 10 smallest systems based on number of acute care hospitals and total physicians.
Table 3.
Number and Percentage of Systems, by Ownership, System Type, and Geographic Reach.
| System characteristics | Percent in system (number) |
|---|---|
| Ownership type: Investor ownership |
3.0 (19) |
| State/local government ownership | 17.3 (108) |
| Nonprofit ownership | 79.7 (499) |
| Teaching status: System includes at least one major teaching hospital | 37.2 (233) |
| Predominantly serves children | 5.0 (31) |
| Safety net status: System includes at least one safety net hospital | 30.8 (193) |
| Hospital presence: Hospital(s) located in only one state |
83.9 (525) |
| Hospitals located in exactly two states | 9.3 (58) |
| Hospitals located in three or more states | 6.9 (43) |
Note. Data come from the 2016 AHRQ Compendium of U.S. Health Systems. A major teaching hospital is defined as a full-time equivalent resident-to-bed ratio greater than or equal to 0.25. Safety net hospitals are defined as the top quintile of Medicare disproportionate share hospital patient percentage nationally.
In aggregate, 7 in 10 health systems include at least some hospitals with a teaching affiliation. Almost 40 percent of systems have at least one major teaching hospital (defined as an FTE resident-to-bed ratio greater than or equal to 0.25). We identified 31 systems (5.0%) that serve predominantly children. Approximately one third of health systems have one or more safety net hospitals (as measured by the top quintile of the DSH patient percentage).
Most health systems had a hospital presence in only one state (based on the address of the system hospitals). About one in six (16.2%) systems have hospitals located in multiple states. Across systems, the number of states ranged from 1 to 35 per system. The top 10 systems in terms of hospital presence each had locations in 14 or more states.
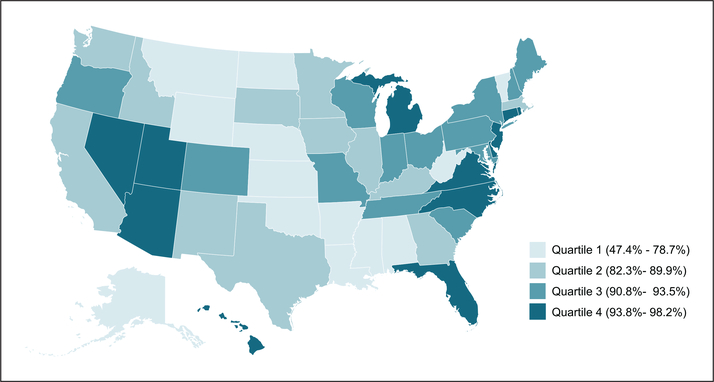
We found considerable system penetration among hospitals and physicians in 2016 (Table 4). A majority of all U.S. nonfederal general acute care hospitals (69.7%) are in health systems; they account for 88.2% of all hospital beds. More than 460,000 physicians, or 44.6% of all U.S. physicians, were in health systems, including 42.7% of primary care physicians. Among states, the percentage of hospital beds associated with health systems varies, ranging from 47.4% in Wyoming to 98.2% in Hawaii (Figure 2). Twenty-five states have more than 90% of all beds in nonfederal general acute care hospitals in health systems.
Table 4.
Number and Percentage of Hospitals, Hospital Beds, and Physicians in Health Systems.
| System members | Number in systems | Percent in systems |
|---|---|---|
| Hospitals | 3,513 | 69.7 |
| Hospital beds | 601,352 | 88.2 |
| All physicians | 464,505 | 44.6 |
| Primary care physicians | 142,000 | 42.7 |
Note. Data come from the 2016 AHRQ Compendium of U.S. Health Systems. Hospital statistics represent all U.S. nonfederal general acute care hospitals.
Figure 2.
Percentage of hospital beds belonging to health systems, by state.
Note. Data come from the 2016 AHRQ Compendium of U.S. Health Systems.
Hospitals that are part of a system differed from those not in a system (Appendix Table A2). Hospitals in systems were larger and varied by ownership and teaching status. Hospitals in systems were more likely to have religious or other nonprofit ownership and less likely to have state or local government ownership.
Discussion
Health systems are a pervasive presence in the United States. A majority of all hospitals and close to half of all physicians are in systems. This presence varies across geographic areas, with the top quartile of states having more than 94% of total beds in nonfederal general acute care hospitals in health systems. We also found substantial diversity among the 626 systems. For example, more than a third of health systems have only one nonfederal general acute care hospital, which is in stark contrast with the 10 largest systems (by number of hospital beds), which account for roughly a quarter of total beds in systems. These findings imply that policies to reform the delivery system must consider both the widespread influence of vertically integrated entities and the diversity in system characteristics. Payment and delivery reforms designed to encourage integration may need to account for this variation.
The debate on whether the growth of health systems is good or bad is ongoing. On the one hand, systems may be better positioned organizationally to invest in health information technology, implement care management processes, and participate in new value-based alternative payment models (Chukmaitov, Harless, Bazzoli, & Deng, 2017; Rodriguez et al., 2016). On the other hand, systems might gain greater market power, which could result in higher prices (Baker, Bundorf, & Kessler, 2014; Machta, Maurer, Jones, Furukawa, & Rich, 2018; Neprash, Chernew, Hicks, Gibson, & McWilliams, 2015). In addition, because value-based purchasing efforts are often aimed at reducing hospital use, the extent to which hospital-led systems will participate in such efforts remains to be seen. More research is needed on whether and to what extent systems, large and small, can achieve better quality and greater efficiencies.
The Compendium—the first national resource specifically developed to support research on health systems—will be a valuable tool for generating answers to questions about comparative health system performance. It can be used to study the characteristics of the U.S. health care system more broadly and policy issues related to provider organizations (Casalino, 2017). It can also be linked to other data sources to study the association of system attributes with cost and quality performance, as well as variation among systems in prices/contracted rates with physicians and hospitals’ and patients’ experience. Moreover, data on the internal structure of health systems might be used to develop taxonomies that describe the U.S. health care landscape (Bazzoli, Shortell, Dubbs, Chan, & Kralovec, 1999; Shortell et al., 2015; Wu, Shortell, Lewis, Colla, & Fisher, 2016).
A growing body of research on comparative health system performance is foundational to developing a high-value health care system. Given the diversity in systems, it is unwise for researchers to focus only on outcomes among system versus nonsystem providers. Instead, researchers should strive to differentiate systems by their form and function. Our data and analysis were limited in scope to vertical integration of hospitals and physicians, and we could not fully describe health systems that include vertical integration of other provider types (e.g., post–acute care). Future research might enumerate the configuration of health systems, such as the “hub and spoke” model, with academic medical centers surrounded by community hospitals (Cutler & Scott Morton, 2013). Future research might also explore other kinds of health systems that did not meet our narrow working definition (e.g., physician organizations that provide comprehensive management of their patient populations without ownership or tight management by a hospital).
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Agency for Healthcare Research and Quality under contract HHSA-290-2016-00001-C. Authors report support from grants 1U19HS024075 and 1U19HS024067. The views expressed herein are those of the authors and do not necessarily reflect those of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
Appendix
Table A1.
Example Health Systems by System Size.
| Health system name | System state (parent location) | Total hospitals | Total physicians | Total prlmary physicians | Total hospital beds | Total residents | Number of States the system operates In | System Includes a safety net hospital | System is predomlnately investor owned |
|---|---|---|---|---|---|---|---|---|---|
| Large systems (by number of acute care hospitals and total physicians) | |||||||||
| HCA | TN | 175 | 9,162 | 2,576 | 34,532 | 1,639 | 20 | Yes | Yes |
| Community Health Systems, Ine | TN | 156 | 4,283 | 1,594 | 20,882 | 419 | 22 | Yes | Yes |
| Ascension Health | MO | 122 | 10,502 | 3,931 | 1 8,097 | 2,062 | 19 | Yes | No |
| Cathollc Health 1 nitiatives | CO | 102 | 5,422 | 1,926 | 12,475 | 1,113 | 15 | Yes | No |
| Trinity Health | MI | 93 | 8,790 | 3,302 | 1 4,706 | 1,749 | 18 | Yes | No |
| Tenet Healthcare Corporation | TX | 82 | 6,297 | 1,587 | 16,315 | 2,123 | 14 | Yes | Yes |
| UfePoint Health | TN | 72 | 1,699 | 668 | 7,680 | 189 | 22 | Yes | Yes |
| Prime Healthcare Services, Ine | CA | 40 | 1,336 | 320 | 5,486 | 293 | 14 | Yes | Yes |
| Dignity Health | CA | 39 | 2,403 | 870 | 7,452 | 220 | 3 | Yes | No |
| Kaiser Permanente | CA | 37 | 20,300 | 8,995 | 8,800 | 855 | 3 | No | No |
| Medium-sized systems (with the median number of acute care hospitals) | |||||||||
| Vanderbilt University Medicai Center | TN | 2 | 1,852 | 366 | 895 | 701 | 1 | No | No |
| UW Health | Wl | 2 | 1,845 | 534 | 857 | 427 | 2 | No | No |
| UF Health | FL | 2 | 1,558 | 391 | 1,264 | 893 | 1 | Yes | No |
| The University of Chicago Medicine | IL | 2 | 1,270 | 344 | 896 | 593 | 1 | Yes | No |
| Cedars-SInai Health System | CA | 2 | 1,258 | 296 | 940 | 349 | 1 | No | No |
| University of Virginia Health System | VA | 2 | 1,247 | 203 | 623 | 660 | 1 | No | No |
| University of Kentucky Healthcare | KY | 2 | 1,230 | 269 | 829 | 485 | 1 | Yes | No |
| Augusta University Medicai Center | GA | 2 | 1,022 | 274 | 495 | 470 | 1 | Yes | No |
| John Muir Health | CA | 2 | 989 | 439 | 751 | 0 | 1 | No | No |
| SUNY Upstate Medicai University | NY | 2 | 895 | 168 | 641 | 335 | 1 | No | No |
| Small systems (by number of acute care hospitals and total physicians) | |||||||||
| Southeastern Health | NC | 1 | 55 | 21 | 256 | 5 | 1 | Yes | No |
| Klngs Daughters Health | IN | 1 | 55 | 24 | 89 | 0 | 1 | No | No |
| Campbell County Memorial Hospital | WY | 1 | 54 | 18 | 66 | 0 | 1 | No | No |
| West Jefferson Medicai Center | LA | 1 | 54 | 29 | 405 | 21 | 1 | No | No |
| South Central Regional Medicai Center | MS | 1 | 53 | 23 | 268 | 0 | 1 | No | No |
| Hendricks Regional Health | IN | 1 | 52 | 16 | 127 | 0 | 1 | No | No |
| Mld-Columbia Medicai Center | OR | 1 | 52 | 22 | 43 | 0 | 1 | No | No |
| Doctors Hospital at Renaissance | TX | 1 | 51 | 23 | 449 | 8 | 1 | Yes | Yes |
| Union Hospital | MD | 1 | 51 | 19 | 1 10 | 0 | 1 | No | No |
| Wyoming Medicai Center | WY | 1 | 51 | 18 | 158 | 0 | 1 | No | No |
Note. Data come from the 2016 AHRQ Compendium of U.S. Health Systems. We sorted Compendium systems by the number of general acute care hospitals and then by the number of total physicians. We then selected the 10 largest systems, the 10 smallest systems, and 10 systems with the median number of hospitals in systems nationally. Hospitals refer to nonfederal general acute care hospitals.
Table A2.
Comparison of Hospitals in Systems and Those Not in Systems.
| Hospitals in systems
(n = 3,513) |
Hospitals not in systems
(n = 1,528) |
|||
|---|---|---|---|---|
| Percent of hospitals | Number of hospitals | Percent of hospitals | Number of hospitals | |
| Hospital beds, M (SD) | 190 (200) | 55 (67) | ||
| Ownership type: | ||||
| Investor ownership | 21 | 676 | 19 | 273 |
| State/local government ownership | 12 | 373 | 44 | 643 |
| Nonprofit ownership | 67 | 2,148 | 37 | 551 |
| Major teaching hospital | 12 | 376 | 2 | 30 |
| Children’s hospital | 2 | 65 | 2 | 13 |
| Safety net hospital | 14 | 448 | 10 | 151 |
Note. Hospitals refer to nonfederal general acute care hospitals. Data come from the Healthcare Provider Cost Reporting Information System. A major teaching hospital is defined as a full-time equivalent resident-to-bed ratio greater than or equal to 0.25. Safety net hospitals are defined as the top quintile of Medicare disproportionate share hospital patient percentage nationally. Some hospitals have missing information for the results presented in this table (406 hospitals for beds and residents, 370 hospitals for ownership and facility type). These hospitals are not included in the calculations.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The Compendium is publicly available for download on the AHRQ website at https://www.ahrq.gov/chsp/compendium/index.html
After completing the unmatched health system to hospital matching, we manually reviewed each of the matches to identify possible parent-subsystem relationships. Manual review included visual review of the system and hospital names and locations, web searching, and expert judgment. A step-by-step example of the review process and a complete list of regional subsystems are published in the Compendium technical documentation.
A Compendium system-hospital linkage file and technical documentation is publicly available for download on the AHRQ website at https://www.ahrq.gov/chsp/compendium/technical-documentation.html
HCOS designates physician affiliations as attending, IDN affiliated, or admitting. Attending includes physicians whose primary practice location is physically located in the hospital. IDN affiliated includes physicians who practice at an outpatient location that is part of an IDN campus and admit to one or more IDN hospitals. Admitting includes physicians who admit to the hospital but are not designated as attending or IDN affiliated.
Our estimate of the total number of physicians from HCOS was consistent with the total active physicians reported by the Association of American Medical Colleges using the American Medical Association Master File (December 2015).
References
- Agency for Healthcare Research and Quality. (2017a). Compendium of U.S. health systems, 2016. Retrieved from http://www.ahrq.gov/chsp/compendium/index.html
- Agency for Healthcare Research and Quality. (2017b). Compendium of U.S. health systems, 2016: Technical documentation. Retrieved from https://www.ahrq.gov/chsp/compendium/technical-documentation.html
- Agency for Healthcare Research and Quality. (2017c). Defining health systems. Retrieved from https://www.ahrq.gov/chsp/chsp-reports/resources-for-understanding-health-systems/defining-health-systems.html
- Baker LC, Bundorf MK, Devlin AM, & Kessler DP (2018). Hospital ownership of physicians: Hospital versus physician perspectives. Medical Care Research and Review, 75, 88–99. [DOI] [PubMed] [Google Scholar]
- Baker LC, Bundorf MK, & Kessler DP (2014). Vertical integration: Hospital ownership of physician practices is associated with higher prices and spending. Health Affairs, 33, 756–763. [DOI] [PubMed] [Google Scholar]
- Bazzoli GJ, Shortell SM, Dubbs NL, Chan C, & Kralovec PD (1999). A taxonomy of health networks and systems: Bringing order out of chaos. Health Services Research, 33, 1683–1717. [PMC free article] [PubMed] [Google Scholar]
- Burns LR, Gimm G, Nicholson S, & Muller RW (2005). The financial performance of integrated health organizations/practitioner application. Journal of Healthcare Management, 50, 191–211. [PubMed] [Google Scholar]
- Burns LR, Goldsmith JC, & Sen A (2013). Horizontal and vertical integration of physicians: A tale of two tails In Goes J, Savage GT, & Friedman L (Eds.), Annual review of health care management: Revisiting the evolution of health systems organization (pp. 39–117). Bingley, England: Emerald Group. [DOI] [PubMed] [Google Scholar]
- Burns LR, & Pauly MV (2002). Integrated delivery networks: A detour on the road to integrated health care? Health Affairs, 21, 128–143. [DOI] [PubMed] [Google Scholar]
- Casalino LP (2014). Identifying key areas for delivery system research (AHRQ Publication No. 14–0024-EF). Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Casalino LP (2017). The Medicare Access and CHIP Reauthorization Act and the corporate transformation of American medicine. Health Affairs, 36, 865–869. [DOI] [PubMed] [Google Scholar]
- Chukmaitov AS, Harless DW, Bazzoli GJ, & Deng Y (2017). Factors associated with hospital participation in Centers for Medicare and Medicaid Services’ accountable care organization programs. Health Care Management Review. Advance online publication. doi: 10.1097/HMR.0000000000000182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen GR, Jones DJ, Heeringa J, Barrett K, Furukawa MF, Miller D, … & Fraze T (2017). Leveraging diverse data sources to identify and describe U.S. health care delivery systems. eGEMs: Journal for Electronic Health Data and Methods, 5(3), 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler DM, & Scott Morton F (2013). Hospitals, market share, and consolidation. JAMA Journal of the American Medical Association, 310, 1964–1970. [DOI] [PubMed] [Google Scholar]
- DesRoches CM, Barrett KA, Harvey BE, Kogan R, Reschovsky JD, Landon BE, … & Rich EC (2015). The results are only as good as the sample: Assessing three national physician sampling frames. Journal of General Internal Medicine, 30, 595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith J, Burns LR, Sen A, & Goldsmith T (2015). Integrated delivery networks: In search of benefits and market effects. Washington, DC: National Academy of Social Insurance. [Google Scholar]
- Kane CK (2017). Updated data on physician practice arrangements: Physician ownership drops below 50 percent. Washington, DC: American Medical Association; Retrieved from https://www.ama-assn.org/sites/default/files/media-browser/public/health-policy/PRP-2016-physician-benchmark-survey.pdf [Google Scholar]
- Machta RM, Maurer KA, Jones DJ, Furukawa MF, & Rich EC (2018). A systematic review of vertical integration and quality of care, efficiency, and patient-centered outcomes. Health Care Management Review. doi: 10.1097/HMR.0000000000000197 [DOI] [PubMed] [Google Scholar]
- Neprash HT, Chernew ME, Hicks AL, Gibson T, & McWilliams JM (2015). Association of financial integration between physicians and hospitals with commercial health care prices. JAMA Internal Medicine, 175, 1932–1939. [DOI] [PubMed] [Google Scholar]
- Post B, Buchmueller T, & Ryan AM (2018). Vertical integration of hospitals and physicians: Economic theory and empirical evidence on spending and quality. Medical Care Research and Review, 75, 399–433. doi: 10.1177/1077558717727834 [DOI] [PubMed] [Google Scholar]
- Rodriguez HP, McClellan SR, Bibi S, Casalino LP, Ramsay PP, & Shortell SM (2016). Increased use of care management processes and expanded health information technology functions by practice ownership and Medicaid revenue. Medical Care Research and Review, 73, 308–328. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell ER, & Ramsay P (2015). Accountable care organizations: The national landscape. Journal of Health Politics, Policy Law, 40, 637–688. doi: 10.1215/03616878-3149976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu FM, Shortell SM, Lewis VA, Colla CH, & Fisher ES (2016). Assessing differences between early and later adopters of accountable care organizations using taxonomic analysis. Health Services Research, 51, 2318–2329. [DOI] [PMC free article] [PubMed] [Google Scholar]