Abstract
A 78-year-old patient with acute respiratory distress was transferred to our hospital with ST segment elevation on electrocardiography. Coronary angiography revealed normal coronary arteries. Thorax computerized tomography showed ground glass opacification with consolidation in the lungs and mild pericardial effusion demonstrating myopericarditis associated with COVID-19.
Abbreviations: CT, computerized tomography; ECG, electrocardiography
Keywords: COVID-19, Myocarditis, Pericarditis
1. Introduction
An outbreak of pneumonia caused by a new coronavirus started in China in December 2019. Coronavirus disease (COVID-19) is caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). While affecting dominantly respiratory system, COVID-19 may also cause acute and chronic damage to the cardiovascular system. Cardiac conditions can be caused by SARS-CoV-2 or can be complications of any other pathology with higher cardio-metabolic demand. We present a 78-year-old man with acute respiratory distress and ST segment elevation on electrocardiography, who was subsequently diagnosed as COVID-19 related myocarditis.
2. Case report
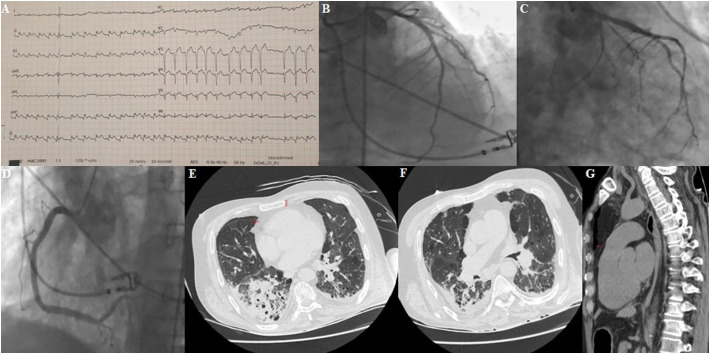
A 78-year-old hypertensive patient had admitted to another center with chest pain and shortness of breath. Upon developing acute respiratory distress in a short time, he was intubated and connected to the mechanical ventilator. No acute pathology or COVID-19 related findings were detected in the thorax computerized tomography (CT). Upon detecting ST segment elevation on electrocardiography (ECG), the patient was transferred to our emergency department. In our hospital, a 12-lead ECG showed atrial fibrillation with 150 beat/min and concave ST elevation except for aVR lead (Fig. 1A). Troponin T level was 998.1 (0–14) ng/L and CRP was 94.6 mg/L (<5). Hemogram analysis revealed leukocytosis and lymphopenia. Coronary angiography was performed after all safety precautions were taken due to COVID-19 Pandemic. No significant pathology was detected on the coronary arteries (Fig. 1B–D). Based on the clinical history and the COVID-19 outbreak, COVID-19 was deemed as likely and thorax CT was taken again. It showed ground glass opacification with consolidation (especially right lower lobe) in the lungs (Fig. 1E, F) associated with COVID-19. Bilateral lower lob subsegmental atelectasis and mild pericardial effusion were also detected (Fig. 1G). Furosemide, beta-blocker and angiotensin converting enzyme inhibitor was added to his COVID specific therapy. After performing coronary angiography and seeing that it was normal, patient was transferred to pandemic hospitalization center where he was hospitalized at first.
Fig. 1.
A. Electrocardiography shows atrial fibrillation and ST elevation; B, C, D. Coronary angiography indicating normal coronary arteries; E, F. Chest computerized tomography displaying ground glass opacification with consolidation (especially right lower lobe) in the lung; E, G. Tomography shows mild pericardial effusion (red arrows). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
This case image demonstrates the myopericarditis associated with COVID-19. COVID-19 should be kept in mind in the aetiology and pathogenesis of myopericarditis in today's conditions [1,2]. Myocarditis is generally suspected in patients with clinical evidence suggesting an acute coronary syndrome on ECG or laboratory testing and/or evidence of wall motion abnormalities with nonobstructive coronary arteries on coronary angiography. Patient, in our case, presented with sudden onset of cardiorespiratory distress, symptoms of viral infection, ST elevation on ECG, elevation of cardiac biomarkers and normal coronary artery indicating myocardial injury. The pericardial effusion on CT supported the diagnosis of pericarditis component. Not being able to perform echocardiography and magnetic resonance imaging (MRI) due to precautions taken for COVID-19 is limitation of our case.
Fever and cough, followed by headache, fatigue, shortness of breath were most common symptoms in patients with COVID-19. Cardiac complications, including heart failure, myocardial infarction, myocarditis and arrhythmia can be accompanied to COVID-19 as previously reported studies [3,4]. The mechanisms responsible for CV complications in COVID-19 are; direct myocardial injury, systemic inflammation, immune response, altered myocardial demand-supply ratio, plaque rupture and coronary thrombosis, adverse effects of therapies or electrolyte imbalances [5].
As troponin can be elevated in severe and critical pneumonia; it rarely indicates myocardial damage in COVID-19 patients. Echocardiography or cardiac MRI is helpful to differentiate heart damage. Among people who died from COVID-19, 11.8% of patients without underlying cardiovascular disease, had considerable heart damage, with elevated levels of troponin or cardiac arrest reported by the National Health Commission of China. Besides that, patients with cardiovascular disease are more likely to develop severe symptoms if infected with SARS-CoV-2.
As a conclusion, COVID-19 patients may present with severe cardiac complications. Myopericarditis should be kept in mind in patients with ST elevation on ECG without reciprocal changes and normal coronary arteries.
Author contributions
Conception and design of the study: Hicaz Zencirkiran Agus, Mustafa Yildiz.
Data collection: Ahmet Yasar Cizgici.
Literature review and writing: Mustafa Yildiz, Hicaz Zencirkiran Agus
Final review: Hicaz Zencirkiran Agus.
Declaration of competing interest
Authors state that there are no conflicts of interest.
References
- 1.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. Mar 27, 2020 doi: 10.1001/jamacardio.2020.1096. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen C., Zhou Y., Wang D.W. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz. Mar 5, 2020 doi: 10.1007/s00059-020-04909-z. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng Jia-Hui, Liu Ying-Xia, Yuan Jing, Wang Fu-Xiang, Wu Wei-Bo, Li Jin-Xiu. Apr 10, 2020. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y.Y., Ma Y.T., Zhang J.Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. Mar 5, 2020 doi: 10.1038/s41569-020-0360-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiong T.Y., Redwood S., Prendergast B., Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020 Mar 18 doi: 10.1093/eurheartj/ehaa231. pii: ehaa231 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]